Abstract
Purpose of Review
Arsenic is associated with cancer, heart disease, diabetes, and other outcomes that are also related to obesity. These similar effects raise the possibility that arsenic plays a role in obesity causation. They also raise the possibility that obesity may be an important effect modifier of arsenic-caused disease. This review summarizes the complex relationship between arsenic and obesity, with an emphasis on current research from human studies.
Recent Findings
Experimental studies provide some evidence that arsenic could play a role in obesity pathogenesis. To date, however, these associations have not been confirmed in human studies. In contrast, several epidemiologic studies have shown that the risks of arsenic-caused disease are markedly higher in obese individuals, highlighting obesity as an important susceptibility factor.
Summary
Arsenic exposure and obesity are prevalent and widespread. Research identifying vulnerable populations, including obese individuals, could lead to new interventions having broad public health effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tens of millions of people worldwide have been exposed to arsenic in drinking water, including an estimated 50 million in Bangladesh, 30 million in India, 15 million in China, and tens of millions more in Europe, South and Central America, and elsewhere [1]. Most of these exposures are a result of naturally occurring inorganic arsenic, although industrial contamination can also occur. In the USA, an estimated 12% of public water systems (5252 out of 43443 public water systems) have had arsenic concentrations near 10 μg/L [2], the current World Health Organization (WHO) recommended standard and US regulatory standard for public water supplies. An estimated 2.1 million people are exposed to higher levels from private wells [3], which are not regulated. Inorganic arsenic also occurs in a variety of foods including apple juice, chicken, wine, beer, and rice [4,5,6,7]. In 2012, the US Food and Drug Administration (FDA) found arsenic in almost all of the 193 brands of rice, rice baby foods, and rice cereals it tested [8]. Overall, through food, water, and other sources, millions of people, including young children, in the USA and worldwide are exposed to elevated levels of arsenic [9].
Ingested inorganic arsenic has been linked to a myriad of health effects, many of which have also been linked to obesity. These included diabetes, cardiovascular disease, hypertension, respiratory effects, altered immune function, and cancer (e.g., kidney, esophageal, and liver) [10]. Although the exact mechanisms by which arsenic causes this panoply of diseases in humans have not been fully elucidated, a number of the pathological processes that have been linked to arsenic also occur with obesity. For example, arsenic and obesity have both been linked to inflammation, oxidative stress, adipokine expression, and insulin resistance, and these pathologic processes are thought to play a role in the diseases caused by each [11]. Overall, the similar pathologic and mechanistic processes linked to arsenic and obesity as well as the similarity in illnesses caused each highlight the potential relationship between these two important disease risk factors.
In this paper, we review the current evidence suggesting that arsenic could be a cause of obesity, as well as the evidence that obesity or increased body mass index (BMI) may act as an effect modifier of arsenic-related disease. The pharmacokinetics and toxicity of inorganic arsenic varies greatly from species to species [12, 13]. In addition, the major mechanism by which inorganic arsenic causes most of its related diseases is unknown. Because of these factors, our focus is on overt health conditions and diseases seen in human studies. However, since the hypothesis that arsenic may cause or interact with obesity is somewhat novel and may not be completely intuitive, we also present data that supports the biologic plausibility of these hypotheses. This includes some laboratory animal and in vitro data, as well as information showing that arsenic and obesity are strongly related to some of the same diseases. Citations for comprehensive reviews of these experimental and other supportive data are provided when available. Reviews of the potential specific mechanisms of arsenic-related disease can also be found elsewhere [14•, 15•].
Arsenic as a Potential Cause of Obesity
Evidence From Animal Studies
The results of a number of studies in laboratory animals support the hypothesis that inorganic arsenic may cause or contribute to obesity or increased body weight. With regard to post-natal exposure, an experimental study of male mice observed a synergistic effect between arsenic and a high-fat diet (58% fat) on body weight [16]. In that study, mice exposed to both a high-fat diet and 25 or 50 ppm arsenic had higher body weights at 5 months relative to mice who were either fed a low-fat diet and exposed to arsenic and control mice that were fed a low fat diet and not exposed to arsenic [16]. A study exposed 5–6-week-old mice to 100 μg/L of As(III) via drinking water for 5 weeks. Relative to those not exposed to arsenic, mice exposed to arsenic experienced adipocyte hypertrophy, decreased adipose tissue expression of perilipin, and increased perivascular ectopic fat deposition in skeletal muscle [17]. Similarly, in a separate study, mice exposed to 100 μg/L of As(III) had increased perivascular ectopic fat deposition in skeletal muscle and marginally increased muscle weight after 5 weeks relative to unexposed control mice [17, 18]. Associations between in utero arsenic exposure and obesity in offspring have also been observed. For example, in male mice fed a Western-style diet (consisting of 15.5% protein, 40.1% fat, 44.4% carbohydrate by kilocalorie), 100 ppb of trivalent arsenic (NaAsO2) in drinking water administered in utero and continuously after birth was associated with increased liver weight as a proportion of body weight, elevated cholesterol, and increased body weight compared to control mice not exposed to arsenic [19].
Other experimental studies have provided evidence that inorganic arsenic may not be a causative agent for obesity. For example, an experimental study exposed C57BL6/J mice to sodium arsenite (NaAsO2) and either a purified normal (17% fat) or high-fat diet (60% fat). In that study, no changes were observed between the two dietary groups and inorganic arsenic exposure was associated with decreased adiposity among those fed a high-fat diet [20]. Similarly, arsenite exposure suppressed adipogenesis in brown adipose tissue [21].
Overall, although several studies in experimental animals have linked inorganic arsenic to increases in body weight, changes in fat metabolism and deposition, or other related outcomes, the evidence from laboratory animal studies that arsenic is a cause of obesity is mixed. Importantly though, arsenic toxicity, metabolism, and other pharmacokinetic factors vary greatly between humans and other species [12, 13], highlighting the importance of confirming findings from animal studies in human populations whenever possible.
Evidence From Human Studies
Human epidemiologic studies have not provided consistent evidence linking inorganic arsenic to increases in body weight or BMI, although most of these studies are cross-sectional and several did not distinguish inorganic and organic arsenic forms. Among 107 women of childbearing age in Santiago, Chile, the median total urinary arsenic level (combined organic and inorganic arsenic) was higher in overweight women than in normal weight women but this difference was small (mean levels of 12.3 μg/g creatinine (95% confidence interval (CI) = 6.9, 16.5) vs. 11.9 (95% CI = 6.2, 16.1), respectively) [22]. A study conducted among 74 welders in Massachusetts found that increasing toenail arsenic concentrations were associated with decreases in BMI [23]. These associations persisted after adjusting for dietary factors [23]. Similarly, a cross-sectional study of 150 blood samples obtained from 30 study sites in Ghana, South Africa, Seychelles, Jamaica, and the USA observed that the geometric mean of total arsenic in blood (μg/L) was lower among obese (geometric mean = 6.77, 95% CI = 5.66, 8.10) compared to non-obese individuals (geometric mean = 8.92, 95% CI = 8.03, 9.90) [24]. In that study, high arsenic (dichotomized at the median level) was not associated with increased odds of obesity after controlling for covariates, including age, sex, and fish intake [24]. An inverse association between inorganic arsenic and BMI was observed among Taiwanese adolescents, where urinary inorganic arsenic concentrations (defined as the sum of urinary inorganic arsenic and its major metabolites) were lower among obese compared to non-obese individuals [25, 26]. Study authors suggested that these associations might be due to obese children retaining higher levels of inorganic arsenic in their bodies as compared to normal weight children [26].
Other studies have observed no association between increasing arsenic exposure and obesity. Bulka et al. used data from the National Health and Nutrition Examination Survey (NHANES), years 2009 to 2012, to examine the association between urinary arsenic exposure and BMI. They found that urinary inorganic arsenic exposure (estimated by subtracting several organic arsenic species from levels of total arsenic) was not associated with obesity after adjusting or standardizing for urinary flow or other covariates [27]. Additionally, pre-pregnancy BMI was not associated with total arsenic or inorganic arsenic in the National Birth Defects Prevention Study [28]. Here, study participants completed a food frequency questionnaire (FFQ) and total and inorganic arsenic intakes were assessed by linking arsenic concentrations to each FFQ item. In other studies, urinary markers of arsenic exposure were not associated with BMI among adults in Korea [29], rural India [30], or children in Mexico City [31].
Our research group has been performing studies on the health effects of arsenic in Northern Chile, an area with a wide range of historical arsenic exposure levels resulting from naturally contaminated drinking water supplies. Here, we found no significant differences in the concentrations of total urinary inorganic arsenic or the individual inorganic arsenic metabolites between people with higher versus lower BMIs [32]. This finding remained when findings were adjusted for age, gender, diet, and the presence of chronic disease. We also found no relationship between past levels of inorganic arsenic in drinking water, including levels up to 860 μg/L, and being either overweight or obese (Table 1). Again, these findings were adjusted or otherwise controlled for age, gender, socioeconomic status, and chronic disease.
Overall, consistent associations between exposure to inorganic arsenic and increasing BMI have not been seen in the current research in humans. Importantly, a number of these studies have only assessed total arsenic and did not distinguish inorganic arsenic from the generally less toxic organic arsenic forms. The addition of organic arsenic and its major sources, primarily seafood, in these studies could mask or confound any potential effects caused by inorganic arsenic. In addition, the large majority of these studies have involved cross-sectional designs, where the potential for reverse causality can complicate their interpretation. Cross-sectional studies could also miss real effects if latency periods are long, information that is currently unknown. In summary, more research is needed to determine if arsenic exposure is on the causal pathway to obesity, and the use of prospective or retrospective designs could help rule out reverse causality and help identify appropriate latency periods.
Arsenic as a Cause of Obesity-Related Disease
Type 2 Diabetes
Although the human epidemiologic evidence linking arsenic directly to obesity is weak and inconsistent, there is convincing evidence that arsenic is a cause of several diseases that are also strongly linked to obesity. Perhaps the clearest example of this is type 2 diabetes, a major downstream consequence of obesity. As reviewed by Farkhondeh et al., arsenic, obesity, and type 2 diabetes may share several common mechanisms or pathological processes, such as apoptosis, elevated inflammation, and oxidative stress [15•]. In our Northern Chile study, we found that the highest tertile of cumulative arsenic exposure in drinking water (> 8665 μg/L-year) was associated with a 50% increase in the odds of type 2 diabetes compared to those in the lowest tertile (< 2416 μg/L-year; OR = 1.50, 95% CI = 1.03, 2.19) [34••]. We also found that this association was strongest among individuals of lower, compared to higher, socioeconomic status [35]. Most of those in the highest tertile of cumulative exposure were drinking water with fairly high arsenic concentrations (e.g., > 500 μg/L). A study in Bangladesh also observed that increasing concentrations of drinking water arsenic, as well as toenail arsenic, were associated with increased odds of type 2 diabetes [36]. This study also involved fairly high exposures, with median drinking water arsenic concentrations of 71.5 μg/L in those with diabetes. In the Zimapán and Lagunera regions of Mexico, researchers reported that a 10 ppb increase in inorganic arsenic concentration was associated with increased odds of type 2 diabetes [37]. Additionally, positive associations between arsenic exposure and type 2 diabetes have been observed in arseniasis-hyperendemic villages in Taiwan [38] and other areas with relatively high exposure levels [36]. Overall, the studies mentioned above are a sample of the wealth of human evidence that arsenic is a likely cause of type 2 diabetes. A meta-analysis on arsenic and diabetes that included 38 human studies reported an overall summary relative risk of 1.57 (95% CI = 1.27, 1.93), with 32 of the 38 studies reporting statistically significant positive associations [39]. Additional comprehensive reviews of the evidence linking arsenic to diabetes have been published [15•, 39,40,41]. There is also a wealth of in vivo and in vitro evidence linking arsenic to glucose intolerance, insulin resistance, and other pathologic or mechanistic features of diabetes, and comprehensive reviews of this evidence have also been previously published [15•, 39,40,41].
Gestational Diabetes
Arsenic exposure has also been linked to an increased risk of developing gestational diabetes mellitus (GDM), which may be a risk factor for type 2 diabetes after pregnancy. Among 1151 women without pre-existing diabetes in the New Hampshire Birth Cohort, a 100% increase in toenail arsenic and each 5 μg/L increase in tap water arsenic concentrations were associated with a 1.1 (95% CI = 1.0, 1.2) and 4.5 (95% CI = 1.2, 16.6) increase in odds of GDM, respectively [42]. Similar results were observed in a Canadian cohort, where pregnant women in the highest (> 1.3 μg/L) compared to lowest quartile of arsenic exposure (< 0.5 μg/L) in 1st trimester blood samples also had increased odds of GDM (OR = 3.7, 95% CI = 1.4, 9.6) with evidence of a dose-response relationship (p trend < 0.01) [43]. However, arsenic exposure was not associated with glucose intolerance in either study [42, 43]. Lastly, a prospective pregnancy cohort in China measured serum arsenic levels during each trimester and found that the highest compared to lowest quartile of arsenic was associated increased odds of GDM when measured during the 1st (OR = 1.71, 95% CI = 1.23, 2.38) and 3rd (OR = 1.39, 95% CI = 0.99, 1.93) trimesters only [44]. Overall, arsenic exposure in early pregnancy appears to be a risk factor for GDM.
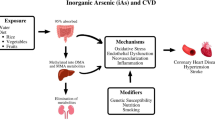
Cardiovascular Disease
In addition to diabetes, arsenic has also been clearly linked to an increased risk of other obesity-related diseases, including several cardiovascular diseases. These associations have been seen in multiple countries and in regions with varying arsenic exposure levels. For example, a population-based study of 11,746 individuals in Bangladesh found that a one standard deviation increase (115 μg/L) in well water arsenic concentrations was associated with an increased hazard of death from ischemic and other forms of heart disease with evidence of trend (hazard ratio [HR] = 1.92, 95% CI = 1.07, 3.43; p trend < 0.01) [45]. Increasing urinary arsenic exposure levels were also associated with death from ischemic and other forms of heart disease in that study [45]. Exposure to arsenic via contaminated well water was also associated with ischemic heart disease in among individuals in Taiwan [46]. Overall, the evidence linking inorganic arsenic to cardiovascular disease is fairly strong and several comprehensive reviews discussing this evidence have been published [47,48,49].
In addition to heart disease, arsenic has also been linked to hypertension. For example, increased odds of hypertension in relation to multiple drinking water arsenic exposure metrics have been observed among individuals in Northern Chile [50]. These findings are supported by a study conducted in villages in Taiwan where arseniasis is hyperendemic [51]. In that study, a dose-response relationship was observed and increasing cumulative arsenic exposure was associated with increased prevalence of hypertension [51]. Importantly, not all studies of arsenic and hypertension have reported positive associations [52], and a comprehensive review of this particular issue can be found elsewhere [53].
Obesity as an Effect Modifier
Overall, the similar diseases and similar pathologic or toxicological mechanisms linked to both arsenic and obesity in some studies have led our research group and others to hypothesize that while arsenic may not be a direct cause of obesity or increased body weight, arsenic and obesity might interact to increase the risks of their common adverse effects. Evidence for this type of synergy has been seen for other environmental exposures. For example, a number of studies suggest that the impacts of air pollution on cardiovascular disease and lung function are markedly worse in people who are obese or overweight compared to those with healthier weights [33, 54, 55]. A number of studies in laboratory animals support the hypothesis that elevated body weight could worsen arsenic-related toxicity. In wild-type mice, exposure to inorganic arsenic in drinking water resulted in insulin resistance only when combined with a high-fat diet and low folate intake [56•]. Similarly, mice doubly exposed to inorganic arsenic in drinking and high-fat diet were more likely to develop glucose intolerance compared to control mice, which may indicate that arsenic exposure acts synergistically with diet to influence obesity [57]. Arsenic exposure also significantly increased liver damage caused by a high fat diet in a mouse model of non-alcoholic fatty liver disease [58]. Arsenic exposure did not influence liver damage among those fed a low-fat diet in that study [58]. Lastly, arsenic exposure also increased oxidative stress, glomerular area expansion, mesangial matrix accumulation, and fibrosis among mice fed a high-fat diet relative to controls who received a low-fat diet [59]. Overall, these animal studies highlight the potential for interactions between arsenic and excess body adiposity. As we review below, several studies in humans have shown similar effects.
Findings From Northern Chile
In our studies from Northern Chile, we found that people with elevated BMIs were at greater risks of several arsenic diseases compared to people with more healthy BMIs. For example, while we found that high exposures to arsenic (> 5280 cumulative arsenic water concentration [μg/L] lagged 40 years) were associated with about a 50% increase in the risk of type 2 diabetes in all participants combined, this increase in risk was over 200% in people who were obese [34••] (Fig. 1). In addition, arsenic is an established cause of lung and bladder cancer, and we found that the odds of developing arsenic-related lung and bladder cancer were substantially elevated among individuals with high BMIs compared to those with lower BMIs [32]. Rothman synergy index values were 4.08 (95% CI = 1.01, 16.46) and 4.06 (95% CI = 1.23, 13.41) for the combined effect of high arsenic exposure and high BMI on the odds of lung and bladder cancer, respectively [32]. Finally, a number of studies have shown that arsenic causes non-malignant lung disease, and we found that individuals with an elevated BMI had increased odds of arsenic-related respiratory symptoms, including cough (OR = 10.7, 95% CI = 3.03, 50.1), shortness of breath (OR = 14.2, 95% CI 4.79, 52.4), and wheeze (OR = 14.4, 95% CI = 4.80, 53.7) [60]. ORs for these arsenic-related symptoms in people who had healthy BMIs were approximately 2–5 times lower.
Summary of findings from Northern Chile illustrating the combined effect of arsenic and obesity on disease risk. Note: Numbers below error bars indicate number of cases/non-cases in each group. Information on how wheeze, cough, and shortness of breath were defined is provided in Nardone et al. [60]. Information on how diabetes was defined is provided in Castriota et al. [34••]. Information on how lung and bladder cancer cases were ascertained is provided in Steinmaus et al. [32]. High BMI was defined as > 30 kg/m2 for diabetes, > 90th percentile (33.9 kg/m2) for wheeze, cough, and shortness of breath, and > 90th percentile at age 20 (27.7 kg/m2 in men and 28.6 kg/m2) for lung cancer and bladder cancer. High arsenic defined as the single year lifetime highest drinking water arsenic concentration ≥ 11 μg/L for wheeze, cough, and shortness of breath, cumulative arsenic water concentration lagged 40 years > 5280 μg/L for diabetes, and high arsenic exposure defined as water arsenic concentration > 800 μg/L for lung cancer and bladder cancer
Findings From Other Studies
Diabetes
Few other studies have examined the role of elevated BMI or obesity on the risks of arsenic-caused disease, and most of these have examined diabetes or insulin resistance. In a study of 933 individuals in a region of Bangladesh with high drinking water arsenic concentrations, the odds of arsenic-related diabetes were markedly increased among individuals with BMIs > 25 kg/m2 (OR = 14.4, 95% CI = 6.07, 34.1) [36]. In comparison, the odds of arsenic-related diabetes was 1.89 (95% CI = 1.07, 3.35) among individuals with BMI < 25 kg/m2. In the New Hampshire Birth Cohort, the role of arsenic on gestational diabetes was examined in 1151 pregnant women [42]. Here, arsenic exposure was assessed using measurements in home well water as well as urine and toenails. In all participants combined, each 5 μg/L increase in arsenic concentration in home well water was associated with about a 10% increased odds of GDM (OR = 1.1, 95% CI = 1.0, 1.2). Clear associations were not seen for urinary arsenic. In analyses stratified by BMI, the association between water arsenic levels and GDM was found to be primarily limited to obese women, with ORs of 0.9 (95% CI = 0.8, 1.2), 1.0 (95% CI = 0.8, 1.2), and 1.7, (95% CI = 1.0, 2.8) in normal weight (< 25 kg/m2), overweight (25–29.9 kg/m2), and obese women (> 30 kg/m2), respectively.
In another study, the impact of weight and arsenic on insulin resistance was assessed in Taiwanese school children [25]. Insulin resistance was assessed using the homeostasis model assessment of insulin resistance (HOMA-IR). Children with BMIs above and below normal levels were combined into one group (defined as “abnormal weight”) although the large majority in this group were overweight or obese. Compared to children with “normal” weight and urinary inorganic arsenic levels ≤ 19.54 μg/L, the increases in HOMA-IR values in children with abnormal weight and higher urinary arsenic levels, children with abnormal weight and arsenic concentrations ≤ 19.54 μg/L, and children with both abnormal weight and higher urinary arsenic concentrations were 0.366 (95% CI = −0.631, 1.326), 1.605 (95% CI = 0.674, 2.536), and 2.146 (95% CI = 1.192, 3.100), respectively, suggesting at least an additive effect.
Other Outcomes
A cross-sectional study conducted within the Health Effects of Arsenic Longitudinal Study (HEALS) cohort in Bangladesh examined the combined effect of arsenic exposure and BMI on cardiovascular disease markers [61]. In that study, individuals with urinary inorganic arsenic concentrations > 275.64 μg/g creatinine and well water arsenic concentrations > 73.5 μg/L had slightly elevated levels of soluble vascular cell adhesion molecule-1 (VCAM-1), a biomarker of inflammatory processes, relative to lower exposure groups. When stratifying by BMI (dichotomized at 19.1 kg/m2), the positive relationship between urinary and well water arsenic exposure and soluble VCAM-1 persisted only in the high BMI group [61]. Finally, in the New England Bladder Cancer Study, overweight individuals had an odds ratio of arsenic-related bladder cancer that was higher than that reported for normal weight individuals (ORs of 1.3 (95% CI = 0.89, 2.0) and 1.6 (95% CI = 1.1, 2.4) in normal weight and overweight participants, respectively, for cumulative arsenic intakes > 77.04 mg) [62]. No association between arsenic exposure and bladder cancer was observed in obese participants; however, the elevated relative risks for increased drinking water intake alone and other features of this study limit its interpretability.
Overall, although not entirely consistent across all studies, a variety of data suggests that arsenic-related disease risks may be higher in people with higher body weights or BMIs. To date, most of this evidence relates to diabetes. Evidence exists for other outcomes such as cancer or cardiovascular disease risk factors, but most of this has yet to be confirmed, highlighting the need for new research in this area.
Conclusions and Future Directions
Overall, our review of the current literature provides little conclusive evidence that arsenic directly causes increased BMI or obesity in humans. However, we identified a number of human and animal studies that showed that obesity or increased BMI could be important susceptibility factors for diseases caused by arsenic. Currently however, the role of obesity as an effect modifier of arsenic-induced disease remains understudied and is an important area of future research. Currently, the US regulatory and WHO recommended standards for arsenic in drinking water are 10 μg/L [63, 64]. These standards are primarily based on epidemiologic studies from highly exposed areas in Taiwan, which involved mostly healthy adults [63]. In addition, they are based only on the risks of cancer and not the other adverse outcomes like diabetes or cardiovascular that are likely caused by arsenic. Because these standards do not specifically incorporate data from potentially susceptible subpopulations, such as those who are obese, and do not include all relevant outcomes, they may be based on analyses that underestimate the true risks in many people.
The WHO estimated that in 2016, more than 1.9 billion adults worldwide were overweight, and of these over 650 million were obese [65]. In the USA, it has been estimated that by 2030, nearly 1 in 2 adults in the USA will be obese [66]. Overall, these large numbers, combined with the large numbers of people who are also exposed to arsenic, highlight the important role that a synergistic relationship between arsenic and obesity could play in public health. Clearly the best approach to improving public health is to focus on interventions aimed at decreasing exposure to arsenic as well as obesity. However, given that obesity rates are increasing worldwide, our review suggests that further research and further consideration of obesity in arsenic regulation might have a major impact in reducing arsenic-related disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ravenscroft P. Predicting the global distribution of natural arsenic contamination of groundwater. Symposium on arsenic: the geography of a global problem. London: Royal Geographical Society; 2007. http://www.geog.cam.ac.uk/research/projects/arsenic/symposium/S1.2_P_Ravenscroft.pdf. Accessed 03/16/12]
U.S. EPA. Arsenic occurrence in public drinking water supplies. Washington, DC: U.S. Environmental Protection Agency. EPA-815-R-00-232000. Report No.: EPA-815-R-00-23.
Ayotte JD, Medalie L, Qi SL, Backer LC, Nolan BT. Estimating the high-arsenic domestic-well population in the conterminous United States. Environ Sci Technol. 2017;51(21):12443–54. https://doi.org/10.1021/acs.est.7b02881.
Wilson D, Hooper C, Shi X. Arsenic and lead in juice: apple, citrus, and apple-base. J Environ Health. 2012;75(5):14–20.
Schute N. Arsenic in beer may come from widely used filtering process. National Public Radio. 2013.
Marshall T. Arsenic in apple juice: how much is too much? Tampa Bay Times. 2012.
Nachman KE, Baron PA, Raber G, Francesconi KA, Navas-Acien A, Love DC. Roxarsone, inorganic arsenic, and other arsenic species in chicken: a U.S.-based market basket sample. Environ Health Perspect. 2013;121(7):818–24. https://doi.org/10.1289/ehp.1206245.
U.S. FDA. Arsenic in rice: full analytical results from rice/rice product sampling—September 2012. U.S. Food and Drug Administration. 2012. http://www.fda.gov/Food/FoodborneIllnessContaminants/Metals/ucm319916.htm. Accessed 11/29/12.
Chung JY, Yu SD, Hong YS. Environmental source of arsenic exposure. J Prev Med Public Health. 2014;47(5):253–7. https://doi.org/10.3961/jpmph.14.036.
National Research Council. Critical aspects of EPA’s IRIS assessment of inorganic arsenic: interim report. Washington, DC: The National Academies Press; 2013.
Arcidiacono B, Iiritano S, Nocera A, Possidente K, Nevolo MT, Ventura V, et al. Insulin resistance and cancer risk: an overview of the pathogenetic mechanisms. Exp Diabetes Res. 2012;2012:789174–12. https://doi.org/10.1155/2012/789174.
Vahter M. Methylation of inorganic arsenic in different mammalian species and population groups. Sci Prog. 1999;82(Pt 1):69–88. https://doi.org/10.1177/003685049908200104.
Drobná Z, Walton FS, Harmon AW, Thomas DJ, Stýblo M. Interspecies differences in metabolism of arsenic by cultured primary hepatocytes. Toxicol Appl Pharmacol. 2010;245(1):47–56. https://doi.org/10.1016/j.taap.2010.01.015.
• Castriota F, Rieswijk L, Dahlberg S, La Merrill MA, Steinmaus C, Smith MT, et al. A state-of-the-science review of arsenic’s effects on glucose homeostasis in experimental models. Environ Health Perspect. 2020;128(1):16001. https://doi.org/10.1289/ehp4517This manuscript is a review article summarizing possible mechanism linking arsenite exposure and diabetes development in in vivo and in vitro studies.
• Farkhondeh T, Samarghandian S, Azimi-Nezhad M. The role of arsenic in obesity and diabetes. J Cell Physiol. 2019;234(8):12516–29. https://doi.org/10.1002/jcp.28112This manuscript is a review article summarizing the effect of arsenic exposure on obesity and disease risk with a focus on potential etiologic mechanisms.
Ahangarpour A, Zeidooni L, Samimi A, Alboghobeish S, Khorsandi LS, Moradi M. Chronic exposure to arsenic and high fat diet additively induced cardiotoxicity in male mice. Res Pharm Sci. 2018;13(1):47–56. https://doi.org/10.4103/1735-5362.220967.
Garciafigueroa DY, Klei LR, Ambrosio F, Barchowsky A. Arsenic-stimulated lipolysis and adipose remodeling is mediated by G-protein-coupled receptors. Toxicol Sci. 2013;134(2):335–44. https://doi.org/10.1093/toxsci/kft108.
Ambrosio F, Brown E, Stolz D, Ferrari R, Goodpaster B, Deasy B, et al. Arsenic induces sustained impairment of skeletal muscle and muscle progenitor cell ultrastructure and bioenergetics. Free Radic Biol Med. 2014;74:64–73. https://doi.org/10.1016/j.freeradbiomed.2014.06.012.
Ditzel EJ, Nguyen T, Parker P, Camenisch TD. Effects of arsenite exposure during fetal development on energy metabolism and susceptibility to diet-induced fatty liver disease in male mice. Environ Health Perspect. 2016;124(2):201–9. https://doi.org/10.1289/ehp.1409501.
Carmean CM, Kirkley AG, Landeche M, Ye H, Chellan B, Aldirawi H, et al. Arsenic exposure decreases adiposity during high-fat feeding. Obesity (Silver Spring). 2020;28(5):932–41. https://doi.org/10.1002/oby.22770.
Bae J, Jang Y, Kim H, Mahato K, Schaecher C, Kim IM, et al. Arsenite exposure suppresses adipogenesis, mitochondrial biogenesis and thermogenesis via autophagy inhibition in brown adipose tissue. Sci Rep. 2019;9(1):14464. https://doi.org/10.1038/s41598-019-50965-9.
Ronco AM, Gutierrez Y, Gras N, Munoz L, Salazar G, Llanos MN. Lead and arsenic levels in women with different body mass composition. Biol Trace Elem Res. 2010;136(3):269–78. https://doi.org/10.1007/s12011-009-8546-z.
Grashow R, Zhang J, Fang SC, Weisskopf MG, Christiani DC, Kile ML, et al. Inverse association between toenail arsenic and body mass index in a population of welders. Environ Res. 2014;131:131–3. https://doi.org/10.1016/j.envres.2014.03.010.
Ettinger AS, Bovet P, Plange-Rhule J, Forrester TE, Lambert EV, Lupoli N, et al. Distribution of metals exposure and associations with cardiometabolic risk factors in the “Modeling the Epidemiologic Transition Study”. Environ Health. 2014;13:90. https://doi.org/10.1186/1476-069x-13-90.
Lin HC, Huang YK, Shiue HS, Chen LS, Choy CS, Huang SR, et al. Arsenic methylation capacity and obesity are associated with insulin resistance in obese children and adolescents. Food Chem Toxicol. 2014;74:60–7. https://doi.org/10.1016/j.fct.2014.08.018.
Su CT, Lin HC, Choy CS, Huang YK, Huang SR, Hsueh YM. The relationship between obesity, insulin and arsenic methylation capability in Taiwan adolescents. Sci Total Environ. 2012;414:152–8. https://doi.org/10.1016/j.scitotenv.2011.10.023.
Bulka CM, Mabila SL, Lash JP, Turyk ME, Argos M. Arsenic and obesity: a comparison of urine dilution adjustment methods. Environ Health Perspect. 2017;125(8):087020. https://doi.org/10.1289/ehp1202.
Suhl J, Conway KM, Rhoads A, Langlois PH, Feldkamp ML, Michalski A, et al. Pre-pregnancy dietary arsenic consumption among women in the United States. Birth Defects Res. 2019;112:270–7. https://doi.org/10.1002/bdr2.1634.
Bae HS, Ryu DY, Choi BS, Park JD. Urinary arsenic concentrations and their associated factors in Korean adults. Toxicol Res. 2013;29(2):137–42. https://doi.org/10.5487/tr.2013.29.2.137.
Velmurugan G, Swaminathan K, Veerasekar G, Purnell JQ, Mohanraj S, Dhivakar M, et al. Metals in urine in relation to the prevalence of pre-diabetes, diabetes and atherosclerosis in rural India. Occup Environ Med. 2018;75(9):661–7. https://doi.org/10.1136/oemed-2018-104996.
Lewis RC, Meeker JD, Basu N, Gauthier AM, Cantoral A, Mercado-García A, et al. Urinary metal concentrations among mothers and children in a Mexico City birth cohort study. Int J Hyg Environ Health. 2018;221(4):609–15. https://doi.org/10.1016/j.ijheh.2018.04.005.
Steinmaus C, Castriota F, Ferreccio C, Smith AH, Yuan Y, Liaw J, et al. Obesity and excess weight in early adulthood and high risks of arsenic-related cancer in later life. Environ Res. 2015;142:594–601. https://doi.org/10.1016/j.envres.2015.07.021.
Dong G-H, Wang J, Zeng X-W, Chen L, Qin X-D, Zhou Y, et al. Interactions between air pollution and obesity on blood pressure and hypertension in chinese children. Epidemiology. 2015;26(5):740–7. https://doi.org/10.1097/EDE.0000000000000336.
•• Castriota F, Acevedo J, Ferreccio C, Smith AH, Liaw J, Smith MT, et al. Obesity and increased susceptibility to arsenic-related type 2 diabetes in Northern Chile. Environ Res. 2018;167:248–54. https://doi.org/10.1016/j.envres.2018.07.022This article found that arsenic exposure was associated with increased odds of type 2 diabetes. Associations were signficantly increased among obese individuals.
Eick SM, Ferreccio C, Acevedo J, Castriota F, Cordero JF, Roh T, et al. Socioeconomic status and the association between arsenic exposure and type 2 diabetes. Environ Res. 2019;172:578–85. https://doi.org/10.1016/j.envres.2019.03.013.
Pan WC, Seow WJ, Kile ML, Hoffman EB, Quamruzzaman Q, Rahman M, et al. Association of low to moderate levels of arsenic exposure with risk of type 2 diabetes in Bangladesh. Am J Epidemiol. 2013;178(10):1563–70. https://doi.org/10.1093/aje/kwt195.
Del Razo LM, García-Vargas GG, Valenzuela OL, Castellanos EH, Sánchez-Peña LC, Currier JM, et al. Exposure to arsenic in drinking water is associated with increased prevalence of diabetes: a cross-sectional study in the Zimapán and Lagunera regions in Mexico. Environ Health. 2011;10(1):73. https://doi.org/10.1186/1476-069X-10-73.
Tseng CH, Tai TY, Chong CK, Tseng CP, Lai MS, Lin BJ, et al. Long-term arsenic exposure and incidence of non-insulin-dependent diabetes mellitus: a cohort study in arseniasis-hyperendemic villages in Taiwan. Environ Health Perspect. 2000;108(9):847–51. https://doi.org/10.1289/ehp.00108847.
Sung T-C, Huang J-W, Guo H-R. Association between arsenic exposure and diabetes: a meta-analysis. Biomed Res Int. 2015;2015:368087–10. https://doi.org/10.1155/2015/368087.
Navas-Acien A, Silbergeld EK, Streeter RA, Clark JM, Burke TA, Guallar E. Arsenic exposure and type 2 diabetes: a systematic review of the experimental and epidemiological evidence. Environ Health Perspect. 2006;114(5):641–8. https://doi.org/10.1289/ehp.8551.
Chen CJ, Wang SL, Chiou JM, Tseng CH, Chiou HY, Hsueh YM, et al. Arsenic and diabetes and hypertension in human populations: a review. Toxicol Appl Pharmacol. 2007;222(3):298–304. https://doi.org/10.1016/j.taap.2006.12.032.
Farzan SF, Gossai A, Chen Y, Chasan-Taber L, Baker E, Karagas M. Maternal arsenic exposure and gestational diabetes and glucose intolerance in the New Hampshire birth cohort study. Environ Health. 2016;15(1):106. https://doi.org/10.1186/s12940-016-0194-0.
Shapiro GD, Dodds L, Arbuckle TE, Ashley-Martin J, Fraser W, Fisher M, et al. Exposure to phthalates, bisphenol A and metals in pregnancy and the association with impaired glucose tolerance and gestational diabetes mellitus: the MIREC study. Environ Int. 2015;83:63–71. https://doi.org/10.1016/j.envint.2015.05.016.
Xia X, Liang C, Sheng J, Yan S, Huang K, Li Z, et al. Association between serum arsenic levels and gestational diabetes mellitus: a population-based birth cohort study. Environ Pollut. 2018;235:850–6. https://doi.org/10.1016/j.envpol.2018.01.016.
Chen Y, Graziano JH, Parvez F, Liu M, Slavkovich V, Kalra T, et al. Arsenic exposure from drinking water and mortality from cardiovascular disease in Bangladesh: prospective cohort study. BMJ. 2011;342:d2431. https://doi.org/10.1136/bmj.d2431.
Hsueh YM, Wu WL, Huang YL, Chiou HY, Tseng CH, Chen CJ. Low serum carotene level and increased risk of ischemic heart disease related to long-term arsenic exposure. Atherosclerosis. 1998;141(2):249–57. https://doi.org/10.1016/s0021-9150(98)00178-6.
Navas-Acien A, Sharrett AR, Silbergeld EK, Schwartz BS, Nachman KE, Burke TA, et al. Arsenic exposure and cardiovascular disease: a systematic review of the epidemiologic evidence. Am J Epidemiol. 2005;162(11):1037–49. https://doi.org/10.1093/aje/kwi330.
Moon K, Guallar E, Navas-Acien A. Arsenic exposure and cardiovascular disease: an updated systematic review. Curr Atheroscler Rep. 2012;14(6):542–55. https://doi.org/10.1007/s11883-012-0280-x.
Tsuji JS, Perez V, Garry MR, Alexander DD. Association of low-level arsenic exposure in drinking water with cardiovascular disease: a systematic review and risk assessment. Toxicology. 2014;323:78–94. https://doi.org/10.1016/j.tox.2014.06.008.
Hall EM, Acevedo J, Lopez FG, Cortes S, Ferreccio C, Smith AH, et al. Hypertension among adults exposed to drinking water arsenic in Northern Chile. Environ Res. 2017;153:99–105. https://doi.org/10.1016/j.envres.2016.11.016.
Chen CJ, Hsueh YM, Lai MS, Shyu MP, Chen SY, Wu MM, et al. Increased prevalence of hypertension and long-term arsenic exposure. Hypertension. 1995;25(1):53–60.
Jones MR, Tellez-Plaza M, Sharrett AR, Guallar E, Navas-Acien A. Urine arsenic and hypertension in US adults: the 2003-2008 National Health and Nutrition Examination Survey. Epidemiology. 2011;22(2):153–61. https://doi.org/10.1097/EDE.0b013e318207fdf2.
Abhyankar LN, Jones MR, Guallar E, Navas-Acien A. Arsenic exposure and hypertension: a systematic review. Environ Health Perspect. 2012;120(4):494–500. https://doi.org/10.1289/ehp.1103988.
Weichenthal S, Hoppin JA, Reeves F. Obesity and the cardiovascular health effects of fine particulate air pollution. Obesity (Silver Spring). 2014;22(7):1580–9. https://doi.org/10.1002/oby.20748.
Xing X, Hu L, Guo Y, Bloom MS, Li S, Chen G, et al. Interactions between ambient air pollution and obesity on lung function in children: the Seven Northeastern Chinese Cities (SNEC) Study. Sci Total Environ. 2020;699:134397. https://doi.org/10.1016/j.scitotenv.2019.134397.
• Huang MC, Douillet C, Dover EN, Zhang C, Beck R, Tejan-Sie A, et al. Metabolic phenotype of wild-type and As3mt-knockout C57BL/6J mice exposed to inorganic arsenic: the role of dietary fat and folate intake. Environ Health Perspect. 2018;126(12):127003. https://doi.org/10.1289/ehp3951This article showed that mice exposed to inorganic arsenic developed insulin resistance only when they were also fed a high-fat diet.
Paul DS, Walton FS, Saunders RJ, Stýblo M. Characterization of the impaired glucose homeostasis produced in C57BL/6 mice by chronic exposure to arsenic and high-fat diet. Environ Health Perspect. 2011;119(8):1104–9. https://doi.org/10.1289/ehp.1003324.
Tan M, Schmidt RH, Beier JI, Watson WH, Zhong H, States JC, et al. Chronic subhepatotoxic exposure to arsenic enhances hepatic injury caused by high fat diet in mice. Toxicol Appl Pharmacol. 2011;257(3):356–64. https://doi.org/10.1016/j.taap.2011.09.019.
Zhang Y, Young JL, Cai L, Tong YG, Miao L, Freedman JH. Chronic exposure to arsenic and high fat diet induces sex-dependent pathogenic effects on the kidney. Chem Biol Interact. 2019;310:108719. https://doi.org/10.1016/j.cbi.2019.06.032.
Nardone A, Ferreccio C, Acevedo J, Enanoria W, Blair A, Smith AH, et al. The impact of BMI on non-malignant respiratory symptoms and lung function in arsenic exposed adults of Northern Chile. Environ Res. 2017;158:710–9. https://doi.org/10.1016/j.envres.2017.06.024.
Wu F, Jasmine F, Kibriya MG, Liu M, Wojcik O, Parvez F, et al. Association between arsenic exposure from drinking water and plasma levels of cardiovascular markers. Am J Epidemiol. 2012;175(12):1252–61. https://doi.org/10.1093/aje/kwr464.
Koutros S, Baris D, Waddell R, Beane Freeman LE, Colt JS, Schwenn M, et al. Potential effect modifiers of the arsenic-bladder cancer risk relationship. Int J Cancer. 2018;143(11):2640–6. https://doi.org/10.1002/ijc.31720.
U.S. EPA. National primary drinking water regulations: arsenic and clarifications to compliance and new source contaminants monitoring; final rule. Fed Reg 40 CFR Parts 141 and 1422001 January 22, 2001.
WHO. Arsenic in drinking water. Background document for development of WHO guidelines for drinking water quality; 2011. http://www.who.int/water_sanitation_health/dwq/chemicals/arsenic.pdf.
World Health Organization. Obesity and overweight factsheet; 2020. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed March 5 2020.
Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440–50. https://doi.org/10.1056/NEJMsa1909301.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Metals and Health
Rights and permissions
About this article
Cite this article
Eick, S.M., Steinmaus, C. Arsenic and Obesity: a Review of Causation and Interaction. Curr Envir Health Rpt 7, 343–351 (2020). https://doi.org/10.1007/s40572-020-00288-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-020-00288-z