Abstract
Objective
To devise an Italian version of the quick mild cognitive impairment screen (Qmci) and to obtain normative data.
Methods
An Italian version of the Qmci screen (Qmci-I) was administered to 307 subjects free from cognitive impairment. The normative sample was divided into three age levels (50–59; 60–69 and 70–80 years) and four education levels (3–5; 6–8; 9–13; >13 years of school attendance). Multiple regression analyses were used to evaluate the effect of age, sex and schooling on Qmci-I scores (overall and by domains) and to calculate cut-off values, with reference to the confidence interval on the fifth centile.
Results
The mean Qmci-I score was 64/100 (SD = 11). The age variable showed a significant negative effect on the overall Qmci-I score, with older people performing worse than younger ones. Conversely, education was associated with higher scores. Significant effects of age and education affected logical memory alone. For the other domains, the following effects were found: (1) higher age associated with lower scores on delayed recall; (2) higher education levels associated with higher scores on immediate recall, clock drawing and word fluency. The adjusted cut-off score for the Qmci-I screen in this sample was 49.4. Qmci-I scores were weakly correlated with those of MMSE (rho = 0.20).
Conclusions
The Qmci-I is a rapid and multi-domain short cognitive screening instrument useful for evaluating cognitive functions. However, like other screening tools, it is significantly influenced by age and education, requiring normative data and correction of values when used in the clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Older adults may experience subjective cognitive impairment, often described as ‘forgetfulness’. In most cases this relates to “physiological” age-related cognitive decline, since standard neuropsychological assessment, with scores referenced against normative data, does not detect significant deficits in specific cognitive domains. In other cases, individuals clearly show objective impairment below the expected levels, i.e., 1.5 standard deviation (SD) below the mean normal performance, mainly in memory, as confirmed by an informant, that can be classified as mild cognitive impairment (MCI) if no associated functional decline can be demonstrated [1,2,3,4]. It is important to detect MCI, as it is considered a risk factor for dementia: in fact, approximately 5–20% of patients per year—depending on the setting (e.g., community versus clinic)—show a decline after diagnosis [1,2,3,4,5,6], especially for those with the amnestic subtype of MCI (aMCI) who converted to Alzheimer’s disease (AD) [7, 8]. Prognosis, management and pharmacological treatment options differ between MCI and dementia [9, 10].
Given the arguable importance of the early detection of dementia to identify modifiable risk factors before the onset of functional impairment [11], a great deal of attention has been devoted to devising a rapid, accurate and reliable tools to improve detection of MCI (e.g., in memory clinics, general practice, etc.). Despite this, few instruments to detect MCI are currently available [12], with few studies comparing specific MCI instruments [13]. To address this, a short cognitive screening instrument, specifically designed to detect MCI—called the quick mild cognitive impairment (Qmci) screen [14]—has been recently proposed. The Qmci screen is composed of six subtests, i.e., orientation, clock drawing, verbal fluency and three tests of memory (five-word immediate and delayed recall and logical memory-immediate verbal recall of a short story) with scores from 0 (indicating severe impairment) to 100 (indicating higher levels of normal cognition) [15]. The Qmci screen has shown good psychometric properties and is suitable to distinguish normal people from subjects with MCI, as well as from patients suffering from dementia, as compared to the Montreal cognitive assessment (MoCA) [13], the ADAS-cog and CDR [16]. These properties have been confirmed in several external validation studies performed in other countries [17,18,19,20]. However, like with other instruments such as the mini-mental state examination (MMSE) [21] and MoCA [22], there is evidence that cut-off scores for the Qmci screen should be adjusted for the effects of age and education [23]. To date, no normative data are available for the Qmci screen in those without cognitive impairment.
Different from MMSE and MoCA: The Qmci has a score range more than threefold wider. This can avoid the ceiling effect in the very early stages of MCI, making the tool suitable to detect a larger number of subjects with subtle cognitive disorders. Furthermore, administration time is only five minutes, i.e., two–threefold shorter than that required for either MMSE and MoCA.
The aims of the present study were to (1) validate the Italian version of the Qmci screen (Qmci-I) against the MMSE and to (2) obtain normative data by administering the screen to a sample of healthy Italian people, representative in terms of age and education of subjects presenting to memory clinics or general practice for assessment.
Methods
Translation and back-translation; pre-test
The original version of the Qmci screen was translated into Italian by a Neurologist and a Psychologist fluent in English. Furthermore, a native English language-speaking translator, blind to the aims of the study, performed the back-translation. Finally, the developers of the Qmci were asked to approve the final version. The personnel involved in the collection of the normative sample was trained by testing the Qmci-I on a small group of healthy participants free from cognitive impairment (n. 22 volunteers). The Qmci-I is presented in Appendix 1.
Subjects and procedures
Healthy subjects (HS) were recruited among clients (and/or their relatives) attending the General Practitioners (GP) or memory clinics in Campania (Italy) by convenience sampling. A “mirror-wise” pre-selection criterion [1,2,3,4] was applied to the subjects to be included. Only those without symptoms or evidence of cognitive decline were included. According to these criteria: (1) the subject did not complain of symptoms of memory loss or another cognitive deficit; (2) this was confirmed by an informant (a relative or the GP); (3) the subject and informant did not report impairment in daily living activities; (4) no dementia could be suspected on the basis of the history.
Inclusion criteria were: subjects’ ages between 50 and 80 years; at least 3 years of school education, and a MMSE score ≥ 25/30. Exclusion criteria were: presence of significant neurological and/or psychiatric disorders (epilepsy, Parkinson’s disease, stroke, psychosis, bipolar disorder, major depressive disorder, etc.); significant general medical diseases interfering with cognition; history of alcohol or substance abuse; use of medications with known significant effects on cognition (e.g., anti-psychotics). To avoid a “hyper-normality bias”, disorders usually observed in older adults (hypertension, diabetes, hyperlipidemia), if well controlled by treatment were not considered as exclusion criteria. To avoid false-negative results, subjects with a ‘normal’ MMSE score (i.e., ≥ 25/30) who showed an absolute memory decay (i.e., a score 0/3 at the three-words delayed recall) were not included in the final sample.
Statistics
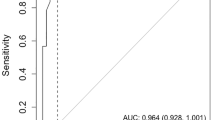
Descriptive statistics were used to summarize data. The effect of demographic variables on Qmci-I scores (overall and by subtests) was examined using multiple regression analysis taking Qmci-I scores as dependent variable and age, sex and education (years of schooling) as the independent one(s). Simultaneous regression models were then constructed to correct raw scores with reference to the independent variables. The level of significance at which to include terms in the model was fixed at p = 0.0167, based on an overall p value of 0.05 divided by the number of independent variables on a Bonferroni basis. The corrected scores were ranked and the non-parametric tolerance limits for the lowest 5% of the values were calculated with 95% confidence intervals. The cut-off scores of the Qmci-I were fixed at the inner tolerance limit on the 5th centile, according to the procedure used by Measso et al. [24] for the MMSE. This means that 95% of HS have an adjusted overall Qmci-I score equal to or greater than the cut-off value, with a 95% probability of this being true. According to the approaches followed by Spinnler and Tognoni [25] and Capitani and Lajacona [26], non-parametric equivalent scores (ES) were described on a 0–4 point interval: 0 equates to scores equal to below or lower the tolerance limit on the 5° centile; 4 corresponding to scores equal to or above the median value (50° centile); the remaining values indicating the non-parametric intermediate parts of the left area of distribution. Concurrent validity was evaluated by correlating the overall Qmci-I scores with those of the MMSE by means of the non-parametric Spearman rank test.
Results
All subjects were screened with the Qmci-I and the MMSE, if possible on two separate occasions.
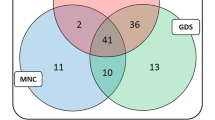
The normative sample consisted of 307 subjects, with almost equal numbers of men and women (Men = 155; women = 152). The mean age of subjects was 63 years (SD = 8.6) with a mean number of years of school attendance of 11.73 (SD = 4.34). There were no differences between men and women according to age and education, albeit this was of borderline significance. According to previous normative studies of cognitive screening tools [24] the normative sample was divided into three age levels (50–59; 60–69 and 70–80 years) and four education levels (3–5; 6–8; 9–13; >13 years of school attendance). Table 1 showsthe distribution of the sample according to age and education.
The mean MMSE score of HS was 26/30 (SD = 1.52). Table 2 reports the mean, SD and range of raw scores of the Qmci-I (overall and separated by domains). A trend towards a ceiling effect was observed on the orientation domain and, to a lesser extent, at immediate recall (five-word registration task), since subjects tended to give the maximum score, with a consequent collapse of the variance. Table 3 shows the mean and SD of the raw overall Qmci-I scores separated by levels of age and education. Lower mean scores were observed in older subjects with lower education level.
Table 4 shows the results of the multiple regression analyses, taking the Qmci-I scores (overall and single domains) as dependent variables and demographic variables as the independent(s) ones. In all cases no gender effect was observed. Age was associated with significantly lower overall Qmci-I scores with older adults performing worse than younger ones. Conversely, education was associated with higher scores. Examining individual subdomain scores, a significant effect of both age and education was observed only for logical memory. For the remaining subdomains, the regression analysis showed only a negative effect of age on delayed recall and a positive effect of education on immediate recall (registration), clock drawing and verbal fluency sub-domains. Using regression analysis, the best fitting simultaneous linear regression model was constructed to correct the Qmci-I raw scores by adding or subtracting the effect of the concomitant variables. After correction, the scores were ranked and the non-parametric tolerance limits for the lowest 5% of values were calculated with 95% confidence intervals as described above. The optimal Qmci-I score was found to be 49.4, i.e., 95% of HS having an adjusted Qmci-I score equal to or greater than 49.4, with a 95% probability of this being true.
Table 5 shows the best simultaneous correction model of Qmci-I scores (overall and by sub-domains). ES, and the corresponding scores intervals, are reported in Table 6.
The correlation between Qmci-I total scores and those of MMSE was considered weak, since it approached significance (p < 0.0005), but showing a low correlation coefficient value (rho = 0.201).
Discussion
This paper presents the development of the Italian version of the Qmci screening tool, with normative data from a sample of age, sex and education stratified HS. It is also the first validation of the Qmci-I. The study shows that healthy Italians scored lower at Qmci screening than English-speaking individuals, from Ireland [13], Canada [14] and Australia [18], but similar to those reported in healthy Dutch [17] or in an older Turkish individuals with low education levels [19]. Several factors may account for these discrepancies, namely, the size and the characteristics of the sample, the settings, etc. In particular, the studies with English-speaking participants included those with higher mean MMSE scores, thus probably starting from a better level of global cognitive functioning. Another result is that at least one Qmci-I subtest (i.e., Orientation) was unaffected by the effects of age and education, with similar scores found for those at all levels. Although this did not invalidate the psychometric properties of the whole tool, it should alert clinicians to take into account this effect when using the Qmci-I in subjects with cognitive impairment. Similar ceiling effects for this subdomain were seen in other studies validating the Qmci screening tool [15]. Data on the Qmci-I in Italian patients with cognitive impairment have not yet been published, but we hypothesize that low scores on the orientation subtest could clearly discriminate HS from patients with dementia, but not HS and MCI. This study also correlated the Qmci-I with the much-used MMSE showing that the two instruments are poorly correlated in healthy Italians. This result was expected given the poor accuracy of the MMSE in detecting MCI compared to the Qmci screen and its subtests, which were selected specifically to detect early cognitive impairment [14, 15].
Of the demographic variables included in the multiple regression analysis, gender was not significant suggesting that this has no effect on the cut-offs used for the Qmci-I. This result replicates findings reported from all studies on Qmci [14, 17,18,19] and from those of the Italian versions of other screening tools for cognitive impairment [24, 27]. On the other hand, a strong negative effect of age was observed for Qmci-I total scores, with older HS attaining lower scores than younger ones. Although expected, based on the results of other instruments [24, 27], such effects were not found for all subtests. In fact, only tasks exploring episodic memory (i.e., delayed recall and logical memory) were significantly influenced by age, scores being lower for older participants. Age and education had effects similar to those found in a validation of the Qmci screening tool in Irish subjects, although a previous paper included people referred for cognitive impairment and did not look at the subtests [23].The results of the normative data in an healthy Italian cohort supports the view that “physiological” cognitive decline does not affect all cognitive domains to the same extent, with episodic memory showing more susceptibility to normal ageing [28, 29].
Similarly, education also affected total Qmci-I scores, higher scores being associated with more school years, replicating previous Qmci screen data in other samples [14, 17,18,19, 30] as well as other screening tools [24, 27]. Such effects involved almost all cognitive sub-domains of the Qmci-I; consistent with the view that education exerts a protective effect on “normal” age-related cognitive decline [31]. Interestingly, only delayed recall has been shown to be an “education-free” task, being less affected by the effects of education [31]. Previous studies using the Qmci screen in patients with MCI and dementia [15] already pointed to the different sensitivity of the tasks in assessing cognitive impairment, confirming that delayed recall is particularly accurate in detecting MCI, in particular aMCI. Although our study did not include cognitively impaired subjects, it supports the crucial role of adjusting for age and education when interpreting the results of short cognitive screening instruments [21, 23, 32]. In this sense, sub domains with minimal effects on education—such as delayed recall that unmask episodic memory impairment—are particularly useful in individuals with early cognitive decline.
This study has a number of limitations. The sampling and recruitment methods may have meant that some participants with early cognitive impairment could have been included. Non-consecutive sampling may have reduced the externalise ability of the data. Similarly, while attempts were made to find those without cognitive symptoms, no established criteria for subjective cognitive decline (SCD) were used, meaning that some subjects with asymptomatic prodromal disease could have been included. That said, the lack of subjective or corroborated symptoms suggests that none of the subjects would have met existing criteria for SCD [33].
Another limitation could be represented by the procedures adopted to obtain corrected scores. Although widely used in the Neuropsychological literature [25, 26] the linear regression model may have biased by the not-normally distribution at some subtests showing a trend toward a ceiling effect (i.e., orientation and immediate recall). Further studies will assess the usefulness of including a revised version of the Qmci only tasks showing better discriminating properties, thus increasing the sensitivity and specificity of the overall score.
Innovative, cross-sectorial strategies examining key areas at population level may contribute directly or indirectly to improve the quality of life of older people making our health and social care systems more efficient and sustainable [34]. Cognitive screening, despite the lack of certainty over its use at population level [11] is one such area and establishing normative data is an important step in this direction.
Conclusions
This study presents normative data for the Qmci-I, correlating it with the MMSE in healthy subjects. The study shows the effects of age and education on the total Qmci-I screen score and its subtests reaffirming that—like other short cognitive screens—it is also affected by age and education.
Like any screening tool, normative data are important and this is the first study providing it for this new instrument. Our results show that the cut-off value is lower that what reported in other studies. This again points to the need for normative data for each population to avoid false-positive and false-negative detection. In this perspective, further studies in Italian patients with MCI and early dementia will better clarify the psychometric properties of the Qmci-I. They will also help address the question of whether the multi-domain structure of the tool could be useful to classify the several subtypes of MCI.
References
Petersen RC, Smith GE, Waring SC et al (1999) Mild cognitive impairment: clinical characterization an outcome. Arch Neurol 56:303–308
Petersen RC, Lopez O, Armstrong MJ et al (2018) Practice guideline update summary: mild cognitive impairment: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology 90:126–135
Jak AJ, Preis SR, Beiser AS et al (2016) Neuropsychological criteria for mild cognitive impairment and dementia risk in the Framingham Heart Study. J Int Neuropsychol Soc 22:937–943
Petersen RC, Aisen P, Boeve BF et al (2013) Mild cognitive impairment due to Alzheimer disease in the community. Ann Neurol 74:199–208
Bozoki A, Giordani B, Heidebrink J et al (2001) Mild cognitive impairments predict dementia in nondemented elderly patients with memory loss. Arch Neurol 58:411–416
Farias ST, Mungas D, Reed BR et al (2009) Progression of mild cognitive impairment to dementia in clinic-vs community-based cohorts. Arch Neurol 66:1151–1157
Albert MS, DeKosky ST, Dickson D et al (2011) The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:270–279
Michaud TL, Su D, Siahpush M et al (2017) The Risk of incident mild cognitive impairment and progression to dementia considering mild cognitive impairment subtypes. Dement Geriatr Cogn Dis 7:15–29
Tricco AC, Soobiah C, Berliner S et al (2013) Efficacy and safety of cognitive enhancers for patients with mild cognitive impairment: a systematic review and meta-analysis. Can Med Ass J 185:1393–1401
Panegyres PK, Berry R, Burchell J (2016) Early dementia screening. Diagnostics 6:6–12
Fox C, Lafortune L, Boustani M et al (2013) The pros and cons of early diagnosis in dementia. Br J Gen Pract 63:e510–e512
Lonie JA, Tierney KM, Ebmeier KP (2009) Screening for mild cognitive impairment: a systematic review. Int Geriatr Psychiatry 24:902–915
O’Caoimh R, Timmons S, Molloy DW (2016) Screening for mild cognitive impairment: comparison of “MCI specific” screening instruments. J Alzheimer’s Dis 51:619–629
O’Caoimh R, Gao Y, McGlade C et al (2012) Comparison of the quick mild cognitive impairment (Qmci) screen and the SMMSE in screening for mild cognitive impairment. Age Ageing 41:624–629
O’Caoimh R, Gao Y, Gallagher PF et al (2013) Which part of the quickmild cognitive impairment screen (Qmci) discriminates between normal cognition, mild cognitive impairment and dementia? Age Ageing 42:324–330
O’Caoimh R, Svendrovski B, Johnston BC et al (2014) The quick mild cognitive impairment screen correlated with the Standardized Alzheimer’s Disease Assessment Scale-cognitive section in clinical trials. J Clin Epidem 67:87–92
Bunt S, O’Caoimh R, Krijnen WP et al (2015) Validation of the Dutch version of the quick mild cognitive impairment screen (Qmci-D). BMC Geriatr 15:115. https://doi.org/10.1186/s12877-015-0113-1
Clarnette R, O’Caoimh R, Antony DN et al (2016) Comparison of the quick mild cognitive impairment (Qmci) screen to the Montreal cognitive assessment (MoCA) in an Australian geriatrics clinic. Int J Geriatr Psychiatry 32:643–649
Yavuz BB, Varan HD, O’Caoimh R et al (2017) Validation of the Turkish version of the quick mild cognitive impairment screen. Am J Alzheimer’s Dis Other Dement 32:145–156
Xu Y, Yu Y, Li X et al (2017) Development of the Chinese version of the quick mild cognitive impairment (Qmci-CN). Age Ageing 46(S3):57
Crum RM, Anthony JC, Bassett SS et al (1993) Population-based norms for the mini-mental state examination by age and educational level. Jama 269:2386–2391
Rossetti HC, Lacritz LH, Cullum CM et al (2011) Normative data for the Montreal cognitive assessment (MoCA) in a population-based sample. Neurology 77:1272–1275
O’Caoimh R, Gao Y, Svendovski A et al (2017) Comparing approaches to optimize cut-off scores for short cognitive screening instruments in mild cognitive impairment and dementia. J Alzheimer’s Dis 57:123–133
Measso G, Cavarzeran F, Zappalà G et al (1993) The mini-mental state examination: normative study of an Italian random sample. Dev Neuropsychol 9:77–85
Spinnler H, Tognoni G (1987) Standardizzazione e taratura italiana di test neuropsicologici. Ital J Neurol Sci 6:8–120
Capitani E, Laiacona M (1988) Aging and psychometric diagnosis of intellectual impairment: some considerations on test scores and their use. Dev Neuropsychol 4:325–330
Santangelo G, Siciliano M, Pedone R et al (2015) Normative data for the Montreal cognitive assessment in an Italian population sample. Neurol Sci 36:585–591
Tromp D, Dufour A, Lithfous S et al (2015) Episodic memory in normal aging and Alzheimer disease: insights from imaging and behavioral studies. Ageing Res Rev 24:232–262
Fjell AM, Sneve MH, Grydeland H et al (2015) Functional connectivity change across multiple cortical networks relates to episodic memory changes in aging. Neurobiol Aging 36:3255–3268
Clarnette R, Goh M, Bharadwaj S et al (2018) Screening for cognitive impairment in an australian aged care assessment team as part of comprehensive geriatric assessment. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn 15:1–12
Roldán-Tapia MD, Cánovas R, León I et al (2017) Cognitive vulnerability in aging may be modulated by education and reserve in healthy people. Front Aging Neurosci 9:340. https://doi.org/10.3389/fnagi.2017.00340
Malek-Ahmadi M, Powell JJ, Belden CM et al (2015) Age-and education-adjusted normative data for the Montreal cognitive assessment (MoCA) in older adults age 70–99. Aging Neuropsychol Cogn 22:755–761
Eckerström M, Göthlin M, Rolstad S et al (2017) Longitudinal evaluation of criteria for subjective cognitive decline and preclinical Alzheimer’s disease in a memory clinic sample. Alzheimer’s Dement Diagn Assess Dis Monit 8:96–107
Illario M, Vollenbroek-Hutten M, Molloy DW et al (2015) Active and healthy ageing and independent living. J Aging Res 2015:542183
Acknowledgements
Michele Arcopinto (Department of Clinical Medicine & Surgery, University of Naples “Federico II”, Naples, Italy), Patrizia Cuccaro (Research and Development Unit, Azienda Ospedaliera Universitaria Federico II, Naples, Italy), Simona De Chiara (G.P. office, Napoli, Italia), Natascia De Lucia (Department of Neurological, Reproductive and Odontostomatological Sciences, University of Naples “Federico II”, Italia), Carmine Del Giudice (Research and Development Unit, Azienda Ospedaliera Universitaria Federico II, Naples, Italy), Nicola Ferrara (Department of Translational Medical Sciences, University of Naples “Federico II”, Naples, Italy), Vincenzo Girardi (G.P. office, Napoli, Italia), Iolanda Grimaldi(Research and Development Unit, Azienda Ospedaliera Universitaria Federico II, Naples, Italy), Ilaria Liguori (Department of Translational Medical Sciences, University of Naples “Federico II”, Naples, Italy), Francesco Orfila Pernas (Institut Universitari d’Investigació en Atenció Primària Jordi Gol, Barcelona, Spagna), Constança Paúl (Instituto de Ciências Biomédicas Abel Salazar, Universidade do Porto, Porto, Portugal), Giovanni Tramontano (Research and Development Unit, Azienda Ospedaliera Universitaria Federico II, Naples, Italy),Francesca Saveria Tripodi (Frullone Geriatric Center, ASL Napoli 1 Centro, Naples, Italy).
Funding
None of the authors received any funding for this work.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Human and animal rights
This study was approved by the local ethics committee and carried out according to the Declaration of Helsinki.
Informed consent
All subjects gave informed consent to the study.
Additional information
The members of the Working Group are provided in the Acknowledgements section.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Iavarone, A., Carpinelli Mazzi, M., Russo, G. et al. The Italian version of the quick mild cognitive impairment (Qmci-I) screen: normative study on 307 healthy subjects. Aging Clin Exp Res 31, 353–360 (2019). https://doi.org/10.1007/s40520-018-0981-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-018-0981-2