Abstract
Background and aims
Loss of both muscle and bone mass results in fragility fractures with increased risk of disability, poor quality of life, and death. Our aim was to assess the association between low appendicular lean mass (aLM) defined according to different criteria and low bone mineral density (BMD) in hip-fracture women.
Methods
Six hundred fifty-three women admitted to our rehabilitation hospital underwent dual energy X-ray absorptiometry 19.1 ± 4.1 (mean ± SD) days after hip-fracture occurrence. Low aLM was identified according to either Baumgartner’s definition (aLM/height2 less than two standard deviations below the mean of the young reference group) or FNIH criteria: aLM <15.02 kg, or aLM adjusted for body mass index (BMI) <0.512. Low BMD was diagnosed with a T-score <−2.5 at the unfractured femoral neck.
Results
Using Baumgartner’s definition, the association between low aLM/height2 and low BMD was significant: χ 2(1, n = 653) = 8.52 (p = 0.004), but it was erased by adjustments for age and fat mass. Using the FNIH definition the association between low aLM and low BMD was significant: χ 2(1, n = 653) = 42.5 (p < 0.001), and it was confirmed after adjustment for age and fat mass (p < 0.001). With the FNIH definition based on aLM/BMI ratio the association between low aLM/BMI ratio and low BMD was nonsignificant: χ 2(1, n = 653) = 0.003 (p = 0.957).
Conclusions
The association between low aLM and low BMD in women with hip fracture dramatically depends on the adopted definition of low aLM. FNIH threshold for aLM (<15.02 kg) emerges as a useful tool to capture women with damage of the muscle-bone unit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aging process of both bones and skeletal muscles is characterized by the progressive loss of mass and by qualitative deterioration [1, 2]. Abnormally high bone wasting resulting in increased risk of fragility fractures characterizes osteoporosis [3, 4]. Abnormally elevated muscle wasting, resulting in impaired strength, limited function, and propensity to falls, depicts sarcopenia [5–8]. Both osteoporosis and sarcopenia with their complications contribute to limit activity and participation in older people, impose a relevant economic burden on healthcare services, and are associated with a reduced life span [3–8]. Notably, a positive association between osteoporosis and sarcopenia, the so-called “hazardous duet” [9], has been shown in survey studies [10–12]. The rationale for the observed association rests on the presence of several causal factors that are thought to contribute to both the conditions. These include a decreased level of physical activity, hormonal changes (mainly low levels of sex steroids, growth hormone and insulin-like growth factor-I), a reduction in dietary protein, catabolic stimuli from chronic inflammation, and vitamin D deficiency [13, 14]. Furthermore, genetic factors contribute to the tight linkages between muscles and bones [15], and the two tissues affect each other by a complex cross-talk which involves a number of secreted molecules [16].
Both sarcopenia and osteoporosis are expected to be highly prevalent in older people who sustain hip fractures, because a fall in individuals with reduced bone strength usually underlies a fracture of the hip [3, 4]. Although qualitative changes play a relevant role in the genesis of both osteoporosis and sarcopenia, low skeletal muscle mass is considered a basic component of the sarcopenia composite definition [5–8], and osteoporosis is diagnosed when low BMD values are found [3, 4]. Indeed, the high prevalence of reduced BMD and reduced appendicular lean mass (aLM) and a significant positive association between the two conditions has actually been shown after hip fracture [17–19]. The threshold for low bone mass (a BMD at least 2.5 standard deviations below the mean BMD found in the reference population of young adults) is largely agreed on and universally used in epidemiological studies [3, 4]. Conversely, there is still debate on the optimal definition of low aLM. According to the original definition by Baumgartner et al. sarcopenia was defined as skeletal muscle mass in the limbs, as measured by dual energy X-ray absorptiometry (DXA), divided by height squared, two standard deviations below the mean in healthy young people under 30 years of age participating in the Rosetta study [20]. In 2014, the Foundation for the National Institutes of Health (FNIH) released operational thresholds [8] for clinically relevant low lean mass (LM). The thresholds were derived from the analysis of multiple existing data sources from large longitudinal studies and were chosen to discriminate relevant outcomes. In women [21], the suggested threshold for low aLM assessed by DXA was an aLM-to-BMI ratio less than 0.512 (or aLM <15.02 kg).
It is noteworthy that the definition of low aLM can capture people with low BMD besides low muscle mass, to facilitate interventions on the bone-muscle unit in people at high risk for fractures [22, 23]. Our aim was to assess the association between low aLM defined according to different criteria and low BMD in hip-fracture women.
Methods
Patients and setting
The study was performed in a city with about one-million inhabitants. We evaluated 720 white women consecutively admitted to our physical medicine and rehabilitation division because of their first hip fracture during a 48-month period. The women came from several orthopedic wards from various hospitals and were referred for acute inpatient rehabilitation by the consultant physiatrists of the orthopedic wards. Thirty-five of the 720 women we evaluated were excluded from our study because their hip fractures resulted from either major trauma or cancer affecting bone. The remaining 685 women sustained fractures that either were spontaneous or resulted from minimal trauma (trauma equal to or less than a fall from a standing position). Eleven of these 685 women were excluded from our study because they had previous arthroplasties that could alter DXA assessment. The remaining 674 women were asked to undergo a DXA scan and to participate in the study. Twenty-one of these 674 women refused to undergo DXA assessment and/or to participate in the study. The final study sample included 653 women who gave their informed consent to participate in the study. Institutional Review Board approval was obtained for the study protocol.
Outcome measures
DXA (Discovery Wi, Hologic Inch.) was used to measure whole and regional body composition. We calculated aLM as the sum of lean mass (LM) in arms and legs. Because metal implants (prostheses, plates, screws, and nails) and postoperative edema can affect the regional assessment of body composition, we corrected aLM by substituting LM in unfractured leg for LM in fractured leg, as previously described: corrected aLM = (LM in unfractured leg × 2) + LM in arms [17, 18].
Low aLM was identified according to different definitions. Taking into account the normative data from the New Mexico Elder Health Study, Baumgartner’s definition identified the women whose aLM/height2 was less than two standard deviations below the mean of the young reference group [20]. FNIH criteria [21] identified the women whose aLM was lower than 15.02 kg (or whose aLM adjusted for body mass index was <0.512).
We evaluated bone mineral density by DXA scan at the non-fractured hip. Two regions of interest were considered: femoral neck and total hip. Osteoporosis was diagnosed when a T-score <−2.5 was found at either femoral neck or total hip. The reference population for T-score calculation was from the Third National Health and Nutrition Examination Survey (NHANES III).
Statistical analyses
We evaluated the linear correlation between measures of LM (aLM, aLM/BMI, aLM/height2) and BMD assessed at either femoral neck or total hip using a Pearson’s test, after checking for normality each of the tested variables using a Shapiro–Wilk test. The association between low levels of aLM (or low levels of either aLM/height2 or aLM/BMI ratio) and BMD was investigated by a Chi-square test for independence. A binary logistic regression test was used to adjust the association between low levels of aLM (or aLM/BMI ratio, or aLM/height2) and low levels of BMD (dependent variable) for age and fat mass (FM). In the regression models, multicollinearity was checked by calculating variance inflation factors which were always lower than 1.3.
The statistical package used was SPSS, version 14.
Results
Descriptive statistics for the 653 women are shown in Table 1.
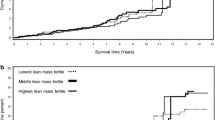
We found a significant positive correlation between aLM and BMD assessed at either femoral neck (r = 0.34; p < 0.001) as shown in Fig. 1, or total hip (r = 0.34; p < 0.001). The age-adjusted correlations between each of the three measures of lean body mass (aLM, aLM/BMI, and aLM/height2) and BMD assessed at either femoral neck or total hip are shown in Table 2.
Using the definition from the New Mexico Elder Health Study, 432 of the 653 women (i.e., 66%; 95% CI 63–70%) had low aLM/height2, whereas using the definition from the FNIH the women with low aLM were 548 of the 653 (i.e., 84%, 95% CI 81–87%). The number of women with low aLM dropped to 224 of the 653 (i.e., 34%, 95% CI 31–38%) when we adopted the FNIH definition based on aLM/BMI ratio.
Low BMD at femoral neck was diagnosed in 432 of the 653 women (i.e., 66%; 95% CI 63–70%), whereas low BMD at total hip was found in 379 women (i.e., 58; 95% CI 54–62%).
After categorization according to the New Mexico Elder Health Study, we found a significant association between low aLM/height2 and low BMD assessed at either femoral neck or total hip: χ 2(1, n = 653) = 8.52 (p = 0.004) and χ 2(1, n = 653) = 16.5 (p < 0.001), respectively. After categorization according to the FNIH threshold for aLM, we found a significant association between low aLM and low BMD assessed at either femoral neck or total hip: χ 2(1, n = 653) = 42.5 (p < 0.001) and χ 2 (1, n = 653) = 50.0 (p < 0.001), respectively. After categorization according to the FNIH threshold for aLM/BMI ratio, the association between low aLM/BMI was significant with BMD assessed at total hip, but not at femoral neck: χ 2 (1, n = 653) = 17.4 (p < 0.001) and χ 2(1, n = 653) = 0.003 (p = 0.957), respectively. The significant association between low aLM defined according to the FNIH threshold and low BMD assessed at either femoral neck or total hip was confirmed after adjustments for age and FM as shown in Table 3. Conversely, the significant association between low aLM/height2 defined according to the New Mexico Elder Health Study and low BMD disappeared after adjustments for age and FM (Table 4). Finally, the association between low aLM/BMI and low BMD assessed at total hip was erased after adjustment for age and fat mass (p = 0.577, data not shown in detail).
Discussion
In women with hip fracture, we show that the association between low BMD and low aLM dramatically depended on the adopted definition of low aLM: the association was significant but it was erased by adjustments with Baumgartner’s definition, significant even after adjustments with the FNIH definition based on aLM alone, whereas with the FNIH definition based on aLM/BMI ratio the association was nonsignificant at all with BMD assessed at femoral neck, and significant but erased by adjustments with BMD assessed at total hip.
To interpret our results, differences in the genesis of the various definitions of low aLM must be taken into account. Baumgartner’s definition was based on distributional characteristics in a reference population and indexing to body size was obtained by calculating the aLM/height2 ratio [20]. Conversely, the recently released FNIH thresholds were based on an operational concept: they were aimed at discriminating values of aLM associated with clinically relevant changes of muscle strength and function [8, 21].
The 66% prevalence of low aLM we find with Baumgartner’s definition is consistent with three previous reports in Caucasian women with hip fracture assessed by either DXA [17, 18] or bioelectrical impedance analysis (BIA) [24]. Conversely, in 304 Japanese women with hip fracture, Hida et al. [19] found a relatively small proportion of women with low aLM/height2 (45%) and an even lower proportion (18%) was found by Gonzales-Montalvo et al. in 479 hip-fracture patients (80% women) assessed by BIA in Spain [25]. The reasons underlying the discrepancies in the reported prevalence of low aLM after hip-fracture are not obvious. A major role may be played by differences in the modest-sized reference populations which result in different thresholds for diagnosing low aLM [20, 26–28]. Alternatively, time between fracture occurrence and aLM assessment has been emphasized [25]. Indeed, changes in body composition, including a decrease in LM, occur after hip fracture and may contribute to increase the prevalence of low aLM found in subacute patients [17, 18, 24] versus acute patients [19, 25]. However, the decrease in LM is modest in the weeks following the hip fracture: no significant changes were reported ten days later [29] and a mean percentage reduction of either 3.4% [29] or 6.2% [30] was shown at a two-month follow-up. Given the modest decrease in aLM, it is unlikely that a 2–3 weeks delay in its assessment [17, 18, 24] may generate major changes in the proportion of women with low values.
The high prevalence of low aLM we find after hip fracture is consistent with the reported association between low muscle mass and fragility fractures [12, 19], but we have no data on unfractured controls to further support the association.
The 84% prevalence of low aLM we find with the FNIH definition is consistent with a previous report in a smaller sample of 138 Caucasian women with hip fracture [31] and it looks higher than the one (38%) found in the 1869 women included in the FNIH project [32]. This is not surprising, because the women included in our sample had a mean age of 79.6 years and sustained a hip fracture, whereas the women included in the FNIH project had a mean age of 76.5 years (SD 4.5 years) and were selected on the basis of “normal” gait speed (>0.8 m/s). Notably, we found a major change in the prevalence of low aLM with indexing to BMI: from 84 to 34% with a 60% relative reduction. A smaller absolute reduction with a similar relative reduction (from 38 to 15% = 61% relative reduction) was observed in the 1869 women of the FNIH project [32]. We conclude that indexing to BMI has major consequences on the prevalence of low aLM, with a similar relative reduction in older women with hip fracture or with normal gait speed.
In agreement with previous reports, we found a high prevalence of osteoporosis in our sample [33, 34], and a positive association between aLM and BMD [17, 19]. The women with low aLM according to the FNIH definition had a higher risk of osteoporosis than those with non-low aLM (odds ratio adjusted for age and fat mass = 2.65 with BMD assessed at femoral neck and 2.48 with BMD assessed at total hip). We support the view of a tight link between skeletal muscle and bone tissue.
Indexing aLM to body size by either height2 or BMI resulted in loss of significant associations with osteoporosis, despite the significant association between low aLM and BMD which persisted after adjustment for age and FM. Indeed, indexing aLM but not BMD to body size can mask the association between muscle and bone mass, at least in postmenopausal women [9, 10]. This is a key point, because various recommended definitions of low aLM include indexing to body size, whereas the current definition of low BMD does not. This discrepancy can result in relevant consequences when either epidemiological or clinical data are considered using aLM as a measure of muscle mass avoids discrepancies due to indexing to body size. Furthermore, assessing aLM is easy to apply because it does not need height assessment, which is often difficult in older women, particularly after a fracture of the hip.
Our study has limitations. We investigated white women admitted to a single rehabilitation hospital in Italy, who agreed to be studied and who could be evaluated by DXA. As a consequence, our data cannot be generalized to the overall population of hip-fracture patients. We did not evaluate muscle function (strength and/or performance), which is included in all the recent definitions of sarcopenia together with low aLM [5–8]. Indeed, several changes in muscle composition that occur with aging may play a pivotal role in impairing muscle function irrespectively of DXA-assessed muscle mass [35]. However, low aLM is a basic component of every sarcopenia composite definition [5–8]. Furthermore, assessments of lower limb strength or performance after hip fracture are often non-feasible or they are altered by the fracture and its surgical treatment. The study design is cross sectional, and data does not prove causal inference. Finally, caution is needed when FM and LM are included into a regression model, because they are primary components of body weight, and they are highly correlated with one another.
In conclusion, we show that the association between low aLM and low BMD dramatically depended on the adopted definition of low aLM in a large sample of women with subacute hip fracture. Major diagnostic changes at both individual and epidemiological levels are expected to be associated with changes in the reference definition. FNIH threshold for aLM (<15.02 kg) emerges as a useful tool to capture women with damage of both the tissue components of the muscle-bone unit.
References
Shimokata H, Ando F, Yuki A, Otsuka R (2014) Age-related changes in skeletal muscle mass among community-dwelling Japanese: a 12-year longitudinal study. Geriatr Gerontol Int 14(S1):85–92
Johnell O, Kanis JA, Oden A et al (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF) (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Physician’s Guide to Prevention and Treatment of Osteoporosis. Washington, DC: The National Osteoporosis Foundation, 2013
Fielding RA, Vellas B, Evans WJ et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12:249–256
Muscaritoli M, Anker SD, Argilés J et al (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr 29:154–159
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al; European Working Group on Sarcopenia in Older People (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39: 412–423
Studenski SA, Peters KW, Alley DE et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 69:547–558
Crepaldi G, Maggi S (2005) Sarcopenia and osteoporosis: a hazardous duet. J Endocrinol Invest 28(S10):66–68
He H, Liu Y, Tian Q, Papasian CJ, Hu T, Deng HW (2016) Relationship of sarcopenia and body composition with osteoporosis. Osteoporos Int 27:473–482
Sjoblom S, Suuronen J, Rikkonen T, Honkanen R, Kroger H, Sirola J (2013) Relationship between postmenopausal osteoporosis and the components of clinical sarcopenia. Maturitas 275:175–180
Verschueren S, Gielen E, O’Neill TW et al (2013) Sarcopenia and its relationship with bone mineral density in middle-aged and elderly European men. Osteoporos Int 24:87–98
Tarantino U, Baldi J, Celi M et al (2013) Osteoporosis and sarcopenia: the connections. Aging Clin Exp Res 25(S1):S93–S95
Girgis CM, Mokbel N, Digirolamo DJ (2014) Therapies for musculoskeletal disease: can we treat two birds with one stone? Curr Osteoporos Rep 12:142–153
Urano T, Inoue S (2015) Recent genetic discoveries in osteoporosis, sarcopenia and obesity. Endocr J 62:475–484
Tagliaferri C, Wittrant Y, Davicco MJ, Walrand S, Coxam V (2015) Muscle and bone, two interconnected tissues. Ageing Res Rev 21:55–70
Di Monaco M, Vallero F, Di Monaco R, Tappero R (2011) Prevalence of sarcopenia and its association with osteoporosis in 313 older women following a hip fracture. Arch Gerontol Geriatr 52:71–74
Di Monaco M, Castiglioni C, De Toma E et al (2015) Presarcopenia and sarcopenia in hip-fracture women: prevalence and association with ability to function in activities of daily living. Aging Clin Exp Res 27:465–472
Hida T, Ishiguro N, Shimokata H et al (2013) High prevalence of sarcopenia and reduced leg muscle mass in Japanese patients immediately after a hip fracture. Geriatr Gerontol Int 13:413–420
Baumgartner RN, Koehler KM, Gallagher D et al (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Cawthon PM, Peters KW, Shardell MD et al (2014) Cutpoints for low appendicular lean mass that identify older adults with clinically significant weakness. J Gerontol A Biol Sci Med Sci 69:567–575
Drey M, Sieber CC, Bertsch T, Bauer JM, Schmidmaier R, FiAT intervention group (2016) Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin Exp Res doi:10.1007/s40520-015-0494-1
Cederholm T, Cruz-Jentoft AJ, Maggi S (2013) Sarcopenia and fragility fractures. Eur J Phys Rehabil Med 49:111–117
Fiatarone Singh MA, Singh NA, Hansen RD et al (2009) Methodology and baseline characteristics for the sarcopenia and hip fracture study: a 5-year prospective study. J Gerontol A Biol Sci Med Sci 64:568–574
González-Montalvo JI, Alarcon T, Gotor P et al (2015) Prevalence of sarcopenia in acute hip fracture patients and its influence on short-term clinical outcome. Geriatr Gerontol Int. doi:10.1111/ggi.12590
Sanada K, Miyachi M, Tanimoto M et al (2010) A cross-sectional study of sarcopenia in Japanese men and women: reference values and association with cardiovascular risk factors. Eur J Appl Physiol 110:57–65
Masanes F, Culla A, Navarro-Gonzalez M et al (2012) Prevalence of sarcopenia in healthy community-dwelling elderly in an urban area of Barcelona (Spain). J Nutr Health Aging 16:184–187
Castaneda C, Janssen I, Castaneda C, Janssen I (2005) Ethnic comparisons of sarcopenia and obesity in diabetes. Ethn Dis 15:664–670
D’Adamo CR, Hawkes WG, Miller RR et al (2014) Short-term changes in body composition after surgical repair of hip fracture. Age Ageing 43:275–280
Fox KM, Magaziner J, Hawkes WG et al (2000) Loss of bone density and lean body mass after hip fracture. Osteoporos Int 11:31–35
Di Monaco M, Castiglioni C (2016) Weakness and low lean mass in women with hip fracture: prevalence according to the FNIH criteria and association with the short-term functional recovery. J Geriatr Phys Ther. doi:10.1519/JPT.0000000000000075
McLean RR, Shardell MD, Alley DE et al (2014) Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the foundation for the National Institutes of Health (FNIH) sarcopenia project. J Gerontol A Biol Sci Med Sci 69:576–583
Di Monaco M, Castiglioni C, Di Monaco R, Tappero R (2015) Prevalence and burden of vertebral fractures in older men and women with hip fracture: a cross-sectional study. Geriatr Gerontol Int. doi:10.1111/ggi.12479
Ha YC, Baek JH, Ko YB, Park SM, Song SH (2015) High mortality and poor morbidity after hip fracture in patients with previous vertebral fractures. J Bone Miner Metab 33:547–552
Degens H, Korhonen MT (2012) Factors contributing to the variability in muscle ageing. Maturitas 73:197–201
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Di Monaco, M., Castiglioni, C., Di Monaco, R. et al. Association between low lean mass and low bone mineral density in 653 women with hip fracture: does the definition of low lean mass matter?. Aging Clin Exp Res 29, 1271–1276 (2017). https://doi.org/10.1007/s40520-017-0724-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0724-9