Abstract
Objectives
To evaluate patients’ participation during physical therapy sessions as assessed with the Pittsburgh rehabilitation participation scale (PRPS) as a possible predictor of functional gain after rehabilitation training.
Methods
All patients aged 65 years or older consecutively admitted to a Department of Rehabilitation and Aged Care (DRAC) were evaluated on admission regarding their health, nutritional, functional and cognitive status. Functional status was assessed with the functional independence measure (FIM) on admission and at discharge. Participation during rehabilitation sessions was measured with the PRPS. Functional gain was evaluated using the Montebello rehabilitation factor score (MRFS efficacy), and patients stratified in two groups according to their level of functional gain and their sociodemographic, clinical and functional characteristics were compared. Predictors of poor functional gain were evaluated using a multivariable logistic regression model adjusted for confounding factors.
Result
A total of 556 subjects were included in this study. Patients with poor functional gain at discharge demonstrated lower participation during physical therapy sessions were significantly older, more cognitively and functionally impaired on admission, more depressed, more comorbid, and more frequently admitted for cardiac disease or immobility syndrome than their counterparts. There was a significant linear association between PRPS scores and MRFS efficacy. In a multivariable logistic regression model, participation was independently associated with functional gain at discharge (odds ratio 1.51, 95 % confidence interval 1.19–1.91).
Conclusion
This study showed that participation during physical therapy affects the extent of functional gain at discharge in a large population of older patients with multiple diseases receiving in-hospital rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rehabilitation is a process of care aimed at reducing patient’s functional deficits without necessarily reversing the underlying biology of the disease [1]. Currently, rehabilitation is recognized as a core element of the practice of medicine, especially when provided with multidisciplinary team and specific approaches [2]. Within this context, it is commonly accepted that a crucial role is played by physiotherapists and by their ability to engage the patient in the activities essentials for the outcome [3, 4]. Because of its possible implications on functional outcomes, patients’ participation in the rehabilitative process has been proposed as an important component of a comprehensive assessment [4]. Indeed, participation can be viewed as an emotional and motivational engagement to be active in a problem-solving process, and rehabilitation may be viewed as a problem-solving process [5]. However, a clear and operational definition of patients’ participation in the context of rehabilitation is currently lacking [6].
Lenze and colleagues proposed that patient participation should be assessed as an observable behavior—quantifiable and measurable—to pursue and adhere to physical therapy [7]. Based on this conceptualization, they developed and validated the Pittsburgh rehabilitation participation scale (PRPS), which standardized measure of patient participation in rehabilitation [7].
To date, only a few studies have assessed the contribution of participation during physical therapy to the recovery process. The role of participation has been evaluated in patients with hip fracture and in patients with other clinical conditions. Study findings noted that participation was not only a predictor of outcomes at discharge, including poor functional gain and prolonged hospital length of stay, but also a mediator of the contributions of depression and cognitive impairment to these negative outcomes [8, 9]. Recently, Paolucci and colleagues confirmed the impact of participation on functional outcomes for patients with stroke or orthopedic diseases in a large sample of relatively young patients (mean age 59.4 ± 12.8 years) [10].
To the best of our knowledge, no other studies have been conducted to assess whether participation predicts functional outcomes in patients undergoing rehabilitation. Additionally, previous studies have not assessed participation as a predictor of recovery in a population of exclusively geriatric patients with high levels of comorbidity. Therefore, we undertook this study to assess the predictive role of participation, measured with the PRPS, on functional recovery in a large population of older and comorbid patients admitted to a rehabilitation unit. We hypothesized that participation could be a predictor of functional gain, independently of age and other variables, which have been found to affect rehabilitation in various studies [7, 11–14].
Methods
This was a retrospective cohort study including all patients aged 65 years and older, consecutively admitted for the first time between June 1, 2009 and December 31, 2011, to our 80-bed Department of Rehabilitation and Aged Care (DRAC). All data were obtained from clinical medical charts and included information and screening measures routinely collected during hospitalization.
The local ethics committee approved the study and the waiver of informed consent given the retrospective nature of the study.
All data were collected by SM, AM, FG, from review of clinical medical charts, including demographics (age, gender, and living arrangement), health, functional, and cognitive status. We also collected the body mass index (BMI) [15]. Cognitive assessment was performed with the mini-mental state examination (MMSE) [16], a commonly used tool in geriatric rehabilitation practice (score range 0–30), while affective status was assessed using the 15-item geriatric depression scale (GDS) (score range 0–15) [17]. The GDS is a tool frequently used in rehabilitation setting to assess depressive symptoms, and it has been shown to predict functional outcomes [13]. Patients were evaluated with the GDS only if they had a MMSE score ≥15/30, since the tool lacks reliability in subjects with moderate to advanced dementia [13, 18].
Comorbidity was defined according to the cumulative illness rating score (CIRS) [19]. CIRS assesses chronic medical illness burden while taking into account the severity of chronic diseases; the score for each of the 14 conditions can range from 1 (absence of pathology) to 5 (maximum level of severity of the disease). The CIRS severity index is the average score of the first 13 items.
Functional status was assessed with the functional independence measure (FIM) [20, 21], a validated tool for clinical assessment of disability in the inpatient rehabilitation setting, showing high inter-rater reliability (ICC = .96) and good predictive validity [22, 23]. The FIM comprises 18 items, each of which is assessed against a seven-point ordinal scale, where the higher the score for an item, the more independently the patient is able to perform the tasks assessed by that item. Total scores range from 18 (functional dependence) to 126 (functional independence). The items are divided into two major groups, the motor and the cognitive items; the motor items include self-care (eating, grooming, bathing, dressing-upper body, dressing-lower body, toileting), sphincter control (bladder and bowel management), transfers (bed/chair/wheelchair, toilet, tub/shower), locomotion (walk/wheelchair, stairs), while the cognitive items include communication (comprehension, expression) and social cognition (social interaction, problem solving, memory). The rating scale designates major graduations in behavior from dependence to independence. FIM scores were collected both on admission and at discharge by two trained physiotherapists [24].
The pre-admission functional status was assessed by asking proxies about patient’s independence in walking without aids or assistance one month before DRAC admission.
Participation was assessed with the PRPS [7] by four physiotherapists trained in its use. The PRPS is a six-point Likert Scale developed to evaluate patient’s participation during physical therapy sessions. According to the authors who developed the PRPS, the scale is scored as follows: (1) refusal or no participation in a session; (2) no participation in at least half of the session; (3) good participation in most or all exercises, but without maximal effort or not finishing most exercises; (4) good participation in all exercises with good effort and finishing most but not all exercises; (5) very good participation in all exercises with maximal effort and finishing all exercises; (6) excellent participation in all exercises, and taking an active interest in exercises and/or future therapy sessions. In a study using actigraphy as an objective measure, this tool was found to be a reliable and accurate measure of participation during physical therapy sessions [25]. The PRPS has high inter-rater reliability (interclass correlation coefficient [ICC] to rehabilitative process = .96 for physical therapists) and good predictive validity (correlation with FIM change: r = .32, F = 26.3, p < .0001) [7]. A native English speaker directly translated the PRPS from English into Italian language. At discharge, a PRPS summary score was calculated for each patient by four physiotherapists as the average value of all PRPS scores obtained weekly during the whole course of inpatient rehabilitation. The weekly average score was calculated using the daily PRPS evaluation during each rehabilitation session.
Patients received two sessions of physical therapy from Monday to Friday and one session on Saturday, either individually or in small groups. Each session of rehabilitation started with a 10-min warm-up and included exercises of strengthening, range of motion, flexibility, transfer training, gait training, and self-care.
Exclusion criteria
The flowchart of the study is shown in Fig. 1. We reviewed all medical charts of patients admitted to the DRAC during the period of interest, and we excluded those who had the following conditions: age ≤65 years; coma, vigilance disorders, delirium, aphasia, and neglect (i.e., clinical conditions that could have interfered with the administration of the PRPS); serious infections and/or non-infection vs adverse clinical events during in-hospital rehabilitation (i.e., clinical conditions that could have affected the patient’s capability to be engaged in physical therapy); transfer to an acute medical ward or death; or refusal to sign informed consent on admission to the DRAC. Additionally, we excluded the medical charts of patients with at least one missing variable, including those with a MMSE score lower that 16/30 since they did not receive GDS assessment (see above).
Outcome measures
The outcome measures selected in this study were part of the standard medical evaluation provided by our DRAC. In accordance with a previous study [26], two parameters derived from the FIM were created: FIM efficacy (FIM efficacy = discharge FIM minus admission FIM) and the Montebello rehabilitation factor score (MRFS) efficacy. FIM efficacy represented the absolute functional gain. MRFS efficacy was the ratio between the absolute functional gain and the difference between the maximum possible FIM and the FIM admission (MRFS efficacy = FIM efficacy/(maximum possible FIM minus admission FIM). We used MRFS efficacy as our outcome measure to solve the problem arising from the fact that patient with high admission scores can achieve only limited gain compared with those who started with lower admission scores [26]. Indeed, the MRFS efficacy is a widely adopted measure of rehabilitation because it overcomes this ceiling effect. Scores are measured in relation to the patient’s specific potential for improvement and reflect a relative functional gain.
Statistical analysis
Comparison groups were obtained using a median-split methodology, a commonly used modality in research studies [27, 28]. MRFS efficacy was calculated for all patients, and two groups of patients were identified: Patients with “good functional gain” were those with MRFS efficacy above the median value of the whole sample (.037), while patients with “poor functional gain” were those with MRFS efficacy under the median value.
Continuous variables are presented as mean ± standard deviation, while categorical data as number and proportions. Normal distribution was evaluated for each variable with a pretest for homogeneity of variances. If abnormal distribution was present, a nonparametric test was used (Mann–Whitney). Otherwise, the Student’s t test for pair comparison was used to examine differences for continuous variables, while the Chi-square test (Fisher’s Test) for categorical variables. Correlations between each variable introduced in the univariate analysis and the MRFS efficacy were evaluated with the Pearson’s correlation coefficient, including the PRPS.
We then conducted a multivariable logistic regression model adjusted for confounding factors. In this model, we included variables showing a significant correlation with the MRFS efficacy score based on the Pearson’s correlation coefficient, and others that were judged to have clinical relevance according to previous studies [8, 11]. We did not perform a priori calculations to guide sample size. Instead, the maximum degrees of freedom we were allowed in the logistic regression model was obtained, as per convention [29], by dividing the minimum number of events (i.e., good functional gain at discharge; N = 272) by 15 to obtain a total of 18 degrees of freedom. All statistical analyses were performed using SPSS (Statistical Package for Social Sciences) version 14, with alpha level set at .05.
Results
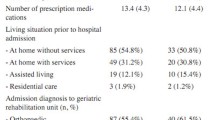
A total of 556 subjects were included in this study. Characteristics of the whole sample, stratified into ‘good functional’ and ‘poor functional,’ are summarized in Table 1. Groups did not differ by gender, BMI, number of drugs, length of stay, and proportion of patients admitted for neurologic reasons. However, patients with poor functional gain at discharge were significantly older, more cognitively impaired and more comorbid, had worse functional status on admission, more depressive symptoms, were more likely to undergo rehabilitation for cardiac diseases or immobility syndrome, and were less likely to be able to walk independently before admission. This group of patients also showed a lower PRPS average score during physical therapy sessions in comparison with those with high functional recovery. A minority of patients showed an excellent participation, that is an average score of 6 (55 patients, 9.9 %). The majority of patients had an average PRPS score of 4 (192 patients, 34.5 %) or 5 (237 patients, 42.6 %), while 11.4 % of patients a score of 3 (63 patients). Only few patients had a score of 1 or 2 (9 patients, 1.6 %) (data not shown).
We examined Pearson’s correlations between MRFS efficacy and all other variables. Higher MRFS efficacy was significantly correlated with lower age (r = −.19), higher MMSE (r = .22), ability to walk before admission (r = .24), lower depressive symptoms (GDS, r = −.14), lower comorbidity (CIRS severity, r = −.13), higher participation (PRPS, r = .21), being admitted for orthopedic disease (r = .18) or pulmonary disease (r = .11), and not having immobility syndrome (r = −.24). Sex, BMI, number of drugs, living alone before admission, and being admitted for neurologic or cardiac diseases did not correlate with the MRFS efficacy. Figure 2 shows variables significantly correlated with the MRFS.
The possible effect of participation on functional recovery at discharge was tested in a multivariate regression model, including all variables that were significantly associated with MRFS, plus gender. Table 2 shows the results of the multivariable logistic regression. PRPS score—indicative of participation level—was significantly associated with functional status at discharge (odds ratio [OR] = 1.51, 95 % confidence interval [CI] 1.19–1.91; p = .001). Other predictors of the functional outcomes were the independence in walking before admission (OR = 2.05; 95 % CI 1.36–3.11; p = .001) and an admission to the DRAC after orthopedic surgery (OR 1.79; 95 % CI 1.01–3.19; p = .046).
Discussion
This study was carried out in a large population of elderly patients with multiple diseases, with the aim to assess whether the patients’ participation to physical therapy sessions affects the extent of functional gain at discharge. We found a linear and significant association between the mean level of patients’ participation and functional gain (as measured with the MRFS efficacy) and also that participation was an independent predictor of this outcome, after adjusting for several covariates.
The efficacy of therapeutic exercises strongly relies on patient’s engagement in and cooperation with the exercise regimen. Multiple factors can modulate engagement and motivation in such activities. Previous studies reported that depressive symptoms and cognitive impairment, especially executive dysfunctions, have a negative effect on a patient’s participation in rehabilitation [30]. Other studies reported that patient’s beliefs about illness, self-efficacy in performing specific activities, perception about the utility of the exercises in relation to the expected outcome, involvement in goal-formulation, and attitudes about therapeutic targets may also affect the degree of participation in rehabilitation activities [31–33]. Other factors that have been hypothesized to play a role are pain, fear of falling, and the manner of approaching the patient during physical therapy sessions [34, 35]. Therefore, we can hypothesize that there is a strong relationship between the level of patient’s participation during physiotherapy and a number of factors that are known to predict the rehabilitation outcome at discharge.
By demonstrating that PRPS score predicts the efficacy of rehabilitation, while other variables that are traditionally considered as predictors (such as age, comorbidity, cognitive status and depression) did not, our findings suggest that participation is an important variable that could be a possible mediator of the association between a patient’s clinical condition and the functional outcome of rehabilitation. This hypothesis for a future study is in line with the results of a study by Lenze, demonstrating that participation modulates the association between depression and, to a lesser extent, cognitive impairment and functional outcome [8].
The other two predictors of functional gain in our study were the ability to walk independently before admission and an admission to the DRAC after orthopedic surgery. The finding that the ability to walk independently before admission predicts functional gain is in line with previous studies finding that the pre-admission functional status is a predictor of functional outcome among elderly patients [36–38]. A possible explanation of the association between the admission after orthopedic surgery and functional outcomes is related to the type of orthopedic surgery. Indeed, most of the patients underwent an elective arthroplasty, a procedure that implies a sudden decline of walking abilities soon after surgery but a likewise rapid improvement in functional performances after few days of rehabilitation. Therefore, it could be hypothesized that, in comparison with the others, these patients had the highest likelihood to improve in functional status at discharge.
Implications of the study are several. Firstly, our data suggest that participation should be routinely assessed during the course of rehabilitation of geriatric patients. Secondly, since previous studies have demonstrated that participation can improve throughout the course of rehabilitation [7], it follows that it should be actively evaluated in patients undergoing rehabilitation in light of their different clinical and psychological needs. For example, participation of cognitively impaired patients would be encouraged using different approaches and techniques than would be used with patients without cognitive impairment. Thirdly, because among all the variables that have been identified as predictors of successful rehabilitation, participation is one of the few factors which are potentially modifiable, physical therapists should sharply focus on this issue in their everyday clinical practice. The relevance of participation as a determinant of rehabilitation outcome should also be taught to students in medical and physiotherapy schools.
Strengths of this study are the inclusion of a large number of patients and of a population of geriatric patients with multiple comorbid diseases. Another strength is that we excluded patients with clinical conditions that may affect per se the administration of PRPS, such as coma, delirium and adverse clinical events. By excluding patients with these conditions, we believe to have reduced the risk of biasing the PRPS assessment with reasons unrelated to patient’s willingness and/or physiotherapist’s approach.
Some limitations should also be highlighted. This was a single-center retrospective cohort study, and the results may not be generalizable to other settings. We also did not collect the PRPS score for each session, but only the average PRPS scores of the whole length of stay, and thus we cannot assess how participation has changed throughout the period of rehabilitation. This would have allowed us to make some additional inferences. In fact, it is not uncommon that participation increases for many patients as they begin to see the effects of rehabilitation. So even a patient who starts off with a low participation score may in fact increase participation as the value of therapy becomes more evident. It might be therefore interesting to compare the outcome of three distinct patient groups: high participation throughout, low participation throughout, and those whose participation increased over time. A future study can explore this issue. A third limitation is that we did not collect data about the global pre-admission functional status of our patients. However, we did have information about pre-admission walking independence, which was obtained by asking patients or proxies. In previous studies, this notion was found to be a good predictor of overall functional mobility in older adults [39]. Also, this study investigated the immediate effect of participation only on short-term outcomes, but it was not possible to test the relationship in the medium and long term. Another limitation was that we did not assess predictors of participation; however, this was not the primary aim of our study, and currently there are no validated instruments to measure motivation in rehabilitation. Finally, a limitation is that we used a median-split methodology to stratify patients into those who regained functions and those who did not. This approach is quite arbitrary, since it assumes an ideal distribution of the scores above and below a certain cutoff. Therefore, we cannot exclude that using this method we may have contributed to obscuring some meaning encoded in the original data. However, it should be observed that this approach has a long tradition in statistics and, taking into account the large sample size of our study, we believe that it would not have determined a significant variation of the final study’s results. Furthermore, we consider that a dichotomous outcome (i.e., good or poor functional gain) would be more informative for the clinical practice rather than the using the total MRFS as a continuous variable.
Future studies should evaluate reasons for and possible predictors of poor participation in order to discover targets of intervention during rehabilitation, thus optimizing the potential patients’ recovery process. Additionally, they will measure both the association of the everyday PRPS score with functional recovery and the outcome at discharge with different statistical approaches.
Conclusions
The study highlights the needs to routinely assess the patients’ participation in physiotherapy sessions and indirectly suggests the importance of fostering active engagement of older adult patients during rehabilitation.
References
Tallis R (1992) Rehabilitation of the elderly in the 21st century. The F. E. Williams Lecture 1992. J R Coll Physicians Lond 26:413–422
Bachmann S, Finger C, Huss A et al (2010) Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ 340:c1718
Ashworth PD, Longmate MA, Morrison P (1992) Patient participation: its meaning and significance in the context of caring. J Adv Nurs 17:1430–1439
Wade DT, de Jong BA (2000) Recent advances in rehabilitation. BMJ 320:1385–1388
Wressle E (2002) Client participation in the rehabilitation process. In: Division of occupational therapy, DoNaL. Faculty of Health Sciences, Linköpings Universitet, pp 1–67
Maclean N, Pound P (2000) A critical review of the concept of patient motivation in the literature on physical rehabilitation. Soc Sci Med 50:495–506
Lenze EJ, Munin MC, Quear T et al (2004) The Pittsburgh rehabilitation participation scale: reliability and validity of a clinician-rated measure of participation in acute rehabilitation. Arch Phys Med Rehabil 85:380–384
Lenze EJ, Munin MC, Dew MA et al (2004) Adverse effects of depression and cognitive impairment on rehabilitation participation and recovery from hip fracture. Int J Geriatr Psychiatry 19:472–478
Lenze EJ, Munin MC, Quear T et al (2004) Significance of poor patient participation in physical and occupational therapy for functional outcome and length of stay. Arch Phys Med Rehabil 85:1599–1601
Paolucci S, Di Vita A, Massicci R et al (2012) Impact of participation on rehabilitation results: a multivariate study. Eur J Phys Rehabil Med 48:455–466
Cameron ID, Schaafsma FG, Wilson S et al (2012) Outcomes of rehabilitation in older people-functioning and cognition are the most important predictors: an inception cohort study. J Rehabil Med 44:24–30
Fusco D, Bochicchio GB, Onder G et al (2009) Predictors of rehabilitation outcome among frail elderly patients living in the community. J Am Med Dir Assoc 10:335–341
Morghen S, Bellelli G, Manuele S et al (2011) Moderate to severe depressive symptoms and rehabilitation outcome in older adults with hip fracture. Int J Geriatr Psychiatry 26:1136–1143
Hershkovitz A, Kalandariov Z, Hermush V et al (2007) Factors affecting short-term rehabilitation outcomes of disabled elderly patients with proximal hip fracture. Arch Phys Med Rehabil 88:916–921
Keys A, Fidanza F, Karvonen MJ et al (1972) Indices of relative weight and obesity. J Chronic Dis 25:329–343
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Yesavage JA, Brink TL, Rose TL et al (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
McGivney SA, Mulvihill M, Taylor B (1994) Validating the GDS depression screen in the nursing home. J Am Geriatr Soc 42:490–492
Parmelee PA, Thuras PD, Katz IR et al (1995) Validation of the cumulative illness rating scale in a geriatric residential population. J Am Geriatr Soc 43:130–137
Keith RA, Granger CV, Hamilton BB et al (1987) The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil 1:6–18
Granger CV, Hamilton BB, Linacre JM et al (1993) Performance profiles of the functional independence measure. Am J Phys Med Rehabil 72:84–89
Corrigan JD, Smith-Knapp K, Granger CV (1997) Validity of the functional independence measure for persons with traumatic brain injury. Arch Phys Med Rehabil 78:828–834
Stineman MG, Shea JA, Jette A et al (1996) The functional independence measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil 77:1101–1108
Kidd D, Stewart G, Baldry J et al (1995) The functional independence measure: a comparative validity and reliability study. Disabil Rehabil 17:10–14
Talkowski JB, Lenze EJ, Munin MC et al (2009) Patient participation and physical activity during rehabilitation and future functional outcomes in patients after hip fracture. Arch Phys Med Rehabil 90:618–622
Rolland Y, Pillard F, Lauwers-Cances V et al (2004) Rehabilitation outcome of elderly patients with hip fracture and cognitive impairment. Disabil Rehabil 26:425–431
Dong Y, Slavin MJ, Chan BP et al (2013) Cognitive screening improves the predictive value of stroke severity scores for functional outcome 3-6 months after mild stroke and transient ischaemic attack: an observational study. BMJ Open 3:e003105
Andreescu C, Lenze EJ, Dew MA et al (2007) Effect of comorbid anxiety on treatment response and relapse risk in late-life depression: controlled study. Br J Psychiatry 190:344–349
Peduzzi P, Concato J, Kemper E et al (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49:1373–1379
Skidmore ER, Whyte EM, Holm MB et al (2010) Cognitive and affective predictors of rehabilitation participation after stroke. Arch Phys Med Rehabil 91:203–207
Wressle E, Eeg-Olofsson AM, Marcusson J et al (2002) Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J Rehabil Med 34:5–11
Resnick B (2002) Geriatric rehabilitation: the influence of efficacy beliefs and motivation. Rehabil Nurs 27:152–159
Sluijs EM, Kok GJ, van der Zee J (1993) Correlates of exercise compliance in physical therapy. Phys Ther 73:771–782
Lequerica AH, Donnell CS, Tate DG (2009) Patient engagement in rehabilitation therapy: physical and occupational therapist impressions. Disabil Rehabil 31:753–760
Bellelli G, Bernardini B, Trabucchi M (2012) The specificity of geriatric rehabilitation: myth or reality? A debate from an Italian perspective. J Am Med Dir Assoc 13:94–95
Torpilliesi T, Bellelli G, Morghen S et al (2012) Outcomes of nonagenarian patients after rehabilitation following hip fracture surgery. J Am Med Dir Assoc 13:81-e1–81-e5
Bellelli G, Noale M, Guerini F et al (2012) A prognostic model predicting recovery of walking independence of elderly patients after hip-fracture surgery. An experiment in a rehabilitation unit in Northern Italy. Osteoporos Int 23:2189–2200
Valderrama-Gama E, Damian J, Guallar E et al (1998) Previous disability as a predictor of outcome in a geriatric rehabilitation unit. J Gerontol A Biol Sci Med Sci 53:M405–M409
Alexander NB, Guire KE, Thelen DG et al (2000) Self-reported walking ability predicts functional mobility performance in frail older adults. J Am Geriatr Soc 48:1408–1413
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
All procedures performed were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The local ethics committee approved the study and the waiver of informed consent given the retrospective nature of the study.
Rights and permissions
About this article
Cite this article
Morghen, S., Morandi, A., Guccione, A.A. et al. The association between patient participation and functional gain following inpatient rehabilitation. Aging Clin Exp Res 29, 729–736 (2017). https://doi.org/10.1007/s40520-016-0625-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0625-3