Abstract
Summary
A score for identifying post-hip-fracture surgery patients at various levels (high, medium, and low) of risk for unsuccessful recovery of pre-fracture walking ability was developed. Three hundred ninety-eight HF patients were enrolled in the study. The score significantly and independently predicted failure to walk independently at discharge, failure to walk independently after 12 months, and death after 12 months. The score may be useful for clinicians and healthcare administrators to target populations for rehabilitative programs.
Introduction
To develop a model predicting at the time that elderly hip-fracture (HF) patients undergo rehabilitation if they will have recovered walking independence at discharge.
Methods
Data from all patients admitted to a Department of Rehabilitation in Italy between January 2001 and June 2008 after HF surgery were used. Variables concerning cognitive, clinical, functional, and social parameters were evaluated. Predominant measures were identified through correspondence analysis, and a variable score was defined. Three risk classes (minimum, moderate, and high) were identified and univariate and multivariate logistic regressions were used to assess the model's predictivity and risk classes for the various outcomes.
Results
Three hundred ninety-eight HF patients were enrolled. The variables selected to construct the score were age, gender, body mass index, number of drugs being taken, the Mini Mental State Examination, the Instrumental Activity of Daily Living, and the pre-fracture Barthel index. According to univariate analysis, the score was not better than the pre-fracture Barthel's index, but, according to multivariate analysis, it was an independent predictor for all the outcomes, while the pre-fracture Barthel index predicted only outcomes at discharge. In particular, the score significantly predicted failure to walk independently at discharge, failure to walk independently after 12 months, and death after 12 months.
Conclusions
A method of identifying post-HF surgery patients at various levels (high-, medium-, and low-) of risk for unsuccessful recovery of pre-fracture walking ability has been designed. The method may be useful for clinicians and healthcare administrators to target populations for rehabilitative programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture (HF) and the resulting postsurgical outcomes continue to be a major public health concern in most Western countries [1]. Despite recent literature indicating that the HF incidence may be stabilizing or decreasing, [2–4] concern still exists that because of the aging of the population, the absolute number of HF will further increase. In this respect, a recent study [5] estimated that approximately 45% of fractures will occur in those aged 85 years and above, compared to 34% in 2004. Even following successful surgery, in fact, patients who undergo rehabilitation after HF surgery frequently do not recover their pre-fracture walking ability and can develop permanent disabilities with deterioration in their quality of life [6–8].
Although identifying and quantifying factors predicting recovery of walking independence at discharge after HF surgery rehabilitation are considered a public health priority [9] and numerous variables have been found to predict a lack of recovery at discharge [10], to our knowledge, a model stratifying HF patients according to their likelihood of walking independently after rehabilitation is not yet available. In the light of these considerations, the aim of the present study was to develop an efficient method identifying patients likely to recover their pre-fracture walking ability from those who are not. Data from a population of elderly adults consecutively admitted to a rehabilitation unit after HF surgery were used to formulate a prognostic model.
Patients and methods
Study population
Three hundred ninety-eight consecutive HF patients who were transferred to a 60-bed Rehabilitation and Aged Care Unit [11] from three local hospitals (Cremona, Manerbio, and Brescia) between January 2001 and June 2008 were considered potential study participants. Inclusion in the study was limited to patients without other fractures, who had no restrictions regarding weight bearing after surgery and who did not have life-threatening conditions such as acute myocardial infarction, coma, or terminal cancer at the time of admission. Informed consent was obtained from all participants or from their legal guardians. The study was approved by the Ethics Committee of the Gerontological Sciences of the Geriatric Research Group, Brescia, Italy.
The patients were generally assigned to a standardized care plan during their hospital stay and followed a multimodal fast-track rehabilitation program including: early surgery within 24–48 h of admission, epidural anesthesia and analgesia continued for 96 h postoperatively, prophylactic intraoperative antibiotics, a standardized transfusion protocol if hemoglobin was lower than 6 mmol/L, supplementary oxygen if patients were supine during the perioperative period, and low molecular weight heparin was administered during the perioperative period. The patients were mobilized on the same day of surgery if possible, and physiotherapy was generally begun the day after.
During the rehabilitation period, on the average, each patient received two daily rehabilitative sessions (40 min in the morning and 40 in the afternoon) from Monday to Friday and a single session (40 min in the morning) on Saturday. Patients were discharged when they regained their pre-fracture functional level or when all the members of the rehabilitative staff agreed that they did not foresee any further improvement in the subject's functional performance.
Predictive variables
The data recorded included: the patients' socio-demographic characteristics (age, gender, living arrangements before HF), markers of nutritional and health status (body mass index (BMI) [12], Charlson comorbidity index (CCI) [13], the number of drugs being taken when the patient was admitted), functional independence (the Barthel index [14] referring to the patient's status 1 month prior to HF and at admission, the functional independence measure (FIM) tm [15] on admission; the Tinetti scale on admission, [16] the Trunk Control (TCT) test [17] on admission, the Instrumental Activities of Daily Living (IADL) [18] prior to HF), cognitive state (the Mini Mental State Examination (MMSE)) on admission [19] and affective status (15-items on the Geriatric Depression Scale [20]. The type of fracture (i.e., cervical, intertrochanteric, or subtrochanteric), the type of surgical procedure performed (i.e., endoprothesis or internal fixation), and the length of time between surgery and admission to the rehabilitation unit (in days) were also recorded.
Outcome variables
The ability to walk independently in patients who had undergone rehabilitation after HF surgery was evaluated considering:
-
1.
at discharge
-
a.
The Barthel index ambulation subscore
-
b.
The total Barthel index
-
a.
-
2.
12 months after discharge, a clinical evaluation was carried out during which walking ability was assessed and defined as (unable to walk; needs constant help of one or more persons during deambulation; needs minimal help to reach for walking aids and to use them; walks independently but only for short walks and needs supervision for greater confidence or safety; walks independently without help or supervision).
A secondary outcome was 12-month survival after discharge.
Statistical analysis
The study's objective was to identify the best combination of variables predicting subjects who would recover walking independence by the time of their discharge or 12 months later. The following statistical analyses were developed: (1) correspondence analysis to identify the predominant factors among original variables; (2) construction of a weighted score defined considering the most important factors identified by correspondence analysis (Fig. 1); (3) univariate analysis of the predictive ability of the defined weighted score with respect to its single components; (4) multivariate analysis of the predictive ability of the score considering its components as competing predictors; (5) definition of optimal cut-offs for the score.
-
1.
Correspondence analysis [21] is a multivariate statistical technique used to summarize high dimensional data by reducing them to a limited number of factors. Original variables, too complex to be displayed in a contingency table, can be viewed graphically in a map where each row and column is represented as a point (profile), and the distance between profiles is calculated as chi-squared distance. Inertia is a geometric measure of the dispersion of profiles in the multidimensional space; it can be decomposed along the principal dimensions, and a map based on the selection of the principal dimensions in a low-dimensional space (usually two or three dimensions) can be constructed. The inertia is the variance of the solutions and the eigenvalues are the percentage of inertia explained by a dimension. Original variables considered in the correspondence analysis were: age, gender, living arrangements before HF, BMI, CCI, the number of drugs being taken at the time of admission, the type of fracture, the type of surgical procedure performed, the length of time between surgery and admission, the Barthel index 1 month prior to HF, the Barthel index at admission, the FIM tm at admission, the Tinetti at admission, the TCT at admission, the IADL, and the MMSE. The Geriatric Depression Scale was not considered in the analysis due to the high number of missing values.
-
2.
Variables most contributing to the inertia of the two dimensions highlighted by the correspondence analysis were identified. Each variable was re-defined according to a hierarchical classification into three classes (0 = no problems, 0.5 = minor problems, 1 = major problems) considering traditional cut-offs and frequency distribution (Table 1). For each subject in the database, the value of each variable redefined according to the hierarchical classification was then weighted according to the contribution of the variable to the inertia of each dimension. A score for each of the two dimensions identified was defined by adding the reweighted variables.
Table 1 Weight assigned to each variable identified considering correspondence analysis dimensions, based on the severity of the problem The total score was then calculated as sum of the scores for each of the two dimensions, weighted by the percentage of inertia of each dimension. As it was defined, the total score included information about a first dimension (in our case, concerning cognitive and functional dependence), the most important in terms of variability and a second dimension. The total score gives a measure of the risk of unsuccessful recovery of pre-fracture walking ability, and its possible values ranges from 0 (minimum risk of non-recovery walking independence) to 100 (highest risk of non-recovery walking independence). An example of the score's use in everyday clinical practice is outlined in Fig. 2.
The total score of the groups was compared using a Generalized Linear Model; the homoschedasticity of variance between groups was assessed by Levene's test, and if there was heteroschedasticity, Welch's ANOVA was used.
-
3.
To test the hypothesis that the predictive ability of the total score was superior to that of its single components considered individually (the BMI, the number of drugs being taken at the time of admission, the Barthel index at admission, the IADL, and the MMSE), univariate logistic model was applied on individual parameters. The ROC curve for each model provides a measure of the model's ability to discriminate those subjects who experienced the outcomes of interest vs. those who did not. Accuracies of models were compared considering the corresponding area under the ROC curve, using a Z test for dependent ROC (because the models were based on the same subjects).
-
4.
Multivariate logistic regression models were defined using the score as a possible predictor “competing” with its own components, using a stepwise selection procedure.
-
5.
Two cut-offs for the total score were defined to identify subjects with a minimum, medium, or high risk of disability. The optimal cut-offs for each outcome were identified considering the ROC curves for the score variable and the Youden criteria. The cut-offs identified were 29 and 41, and the three risk classes were then: minimal (score = 0–28), medium (score = 29–40), and high (score = 41–100). Logistic regression models were defined, with risk classes and other individual scales as predictors, considering a stepwise selection procedure.
All analyses were performed using SAS 9.2 software.
Results
The general characteristics of the study population are presented in Table 2. Approximately 84% of the sample were females, and the subjects' mean age was 82.5 ± 7.2 years. Almost 66% lived with a spouse and/or others, and 5.3% were residents in NH before HF. The average number of comorbidities was 1.7, and the average number of drugs being taken at admission was 5.4. With reference to functional status, the mean Barthel index value 1 month before HF was 84.1 ± 19.5, while it was 29.7 ± 15.8 at admission. The mean values for the FIM, the Tinetti, and the TCT scales were, respectively, 55.3 ± 20.5 (range 18–112), 4.2 ± 4.8 (range 0–22), and 13.3 ± 12.0 (range 0–48). With reference to the IADL tasks, an average of nearly 4 were impaired.
In order to construct the final score, we considered all the variables except two. The FIM tm was not considered because, at least in Italy, raters need to take a special course and to have a permit licensed by the Uniform Data System for Medical Rehabilitation (UDSmr) (www.udsmr.org). It is not easily accessible to a large part of health workers in rehabilitation facilities and much of it overlaps with the Barthel index, thus increasing the risk of collinearity in the statistical analyses. The Tinetti scale was not considered in the final score since it assesses a dimension which is strongly related and overlaps with the Barthel index. Correspondence analysis and the study of eigenvalues and variance revealed that there were two factors with an ellipsoid configuration. The most important factor was linked to “cognitive and functional dependence” and the most important variables in terms of inertia of the first factor were: MMSE, the Barthel index 1 month prior to the HF, and the IADL. The variables contributing the most to the inertia of the second factor were related to the “health status and surgical procedure”: BMI, the number of drugs being taken, age, gender, and type of surgery.
The total score was constructed as a measure of the risk of unsuccessful recovery of pre-fracture walking ability, and its values ranged from 0 (minimum risk of non-recovery walking independence) to 100 (highest risk of non-recovery walking independence). The mean score of the total sample was 40.4 ± 20.8, with a median value of 39.2. Significant differences were found for sex (47.5 ± 22.5 vs. 39.1 ± 20.3, for males and females, respectively; p = 0.0031) and age groups (32.7 ± 20.7 vs. 36.9 ± 19.6 vs. 47.0 ± 20.4, for subjects aged 65–74, 75–84, and 85 or more years, respectively; p < 0.0001).
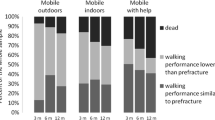
With reference to the Barthel index ambulation subscore at discharge, 8.4% of the sample were dependent on assistance for ambulation, 12.4% required the constant presence of one or more assistants during ambulation, 21% required assistance in reaching walking aids, 33.4% were independent in ambulation but were unable to walk 50 m without help, and 24.8% were able to walk 50 m without help. Of the subjects, 25.8% had severe or complete disability, 26.3% had moderate disability, while 47.9% had mild or minimum disability on the total Barthel index at discharge. The distribution of the walking ability item 12 months after discharge was 12.1% (unable to walk), 8.4% (needs constant help), 25% (needs minimal help), 15.1% (walks independently only for short walks), and 39.5% (walks independently without help or supervision).
Figures 3, 4, and 5 show the ROC curves for each outcome. Considering the Barthel index subscore on ambulation at discharge (Fig. 3), the area under the ROC curve (AUC) for our score was 0.82 (“good predictor”), and it was significantly different from the AUC for each of the other predictors (p < 0.05) with the exception of the Barthel index 1 month prior to HF (p = 0.6367) and IADL score (p = 0.1587). In relation to the total Barthel index score at discharge (Fig. 4), the AUC for our score was 0.86 (“good predictor”); it was significantly different from the AUC of the other predictors (p < 0.05) with the exception of the Barthel index 1 month prior to HF (p = 0.5722) and the IADL score (p = 0.8801). Finally, considering the walking ability outcome 12 months after discharge, the AUC for the prognostic score was 0.75 (“fairly good predictor”), significantly different from the AUC for BMI (p < 0.0001) and the number of drugs being taken at admission (p < 0.0001).
Table 3 presents the results of logistic regression models defined to study the prediction of the score in relation to defined outcomes. In particular, the Barthel index ambulation subscore at discharge was dichotomized into 0 = “independent in ambulation for less than 50 m or for more than 50 m” vs. 1 = “dependent or requiring assistance in ambulation”. The outcome on the total Barthel index score at discharge was dichotomized into 0 = “minimum or mild disability” vs. 1 = “moderate, severe, or complete disability”. The walking ability outcome 12 months after discharge was dichotomized into 0 = “walks independently but only for short walks and needs supervision for greater confidence or walks independently without help or supervision” vs. 1 = “unable to walk, needs constant help, or needs minimal help”.
The model score variable was a significant predictor of each outcome considered; in particular, a risk of dependence in ambulation at discharge of 7%, a risk of moderate, severe, or complete disability in the Barthel index at discharge of 9%, and a risk of dependence in walking at 12 months of 5% corresponded to an increase of one point in the model score variable. In addition, an increase of one point in the total model score corresponded to a 4% increase in the risk of death 12 months after discharge.
Risk classes resulting from the total score were: minimum risk (score 0–28; 32.4%); medium risk (score 29–40; 21.4%); high risk (score 41–100; 46.2%). High risk was a significant predictor for dependency on the Barthel index ambulation subscore at discharge (OR = 7.49, 95% CI 3.53–15.9), on the Barthel index at discharge (OR = 3.27, 95% CI 1.25–8.56) and for the walking ability item 12 months after discharge (OR = 5.72, 95% CI 2.88–11.37); a medium risk was a significant predictor for walking dependency at discharge (OR = 3.60, 95% CI 1.62–8.00) and at 12 months after discharge (OR = 4.78, 95% CI 2.47–9.26).
Discussion
This study proposes a method to stratify elderly HF patients into three (high, medium, and low) risk groups for two outcomes: recovery of functional status and walking ability by the time of discharge from a rehabilitation center and 12 months later.
Several studies have assessed predictors of functional recovery in patients following HF surgery and rehabilitation, finding that many factors, including age [22], gender [23], health status [24], fracture type and procedures [25], post-operative pain [26], anemia [27], cognitive impairment [28], pre-fracture functional status [8, 10, 29, 30], post-operative immobilization [31], and functional status at discharge [7, 29, 32], affect the short- and long-term prognosis. However, only a few have attempted to assemble these data to formulate a model predicting various risk levels of unsuccessful recovery of walking independence at discharge from rehabilitation units. Hagino et al. [33] developed a scoring system to predict ambulation status based on data from a population of 186 elderly patients, all ambulant prior to HF. The predictor variables examined in that study were: age, gender, cognitive level, fracture type, anemia, liver function, renal function, electrolyte abnormality, inflammatory status, urinary glucose, lung function, cardiac function, and chronic systemic comorbidity at admission. After univariate and multivariate analyses, three factors (anemia, dementia, and abnormal lung function) found to predict ambulation were used to develop a scoring system. Masuda et al. [34] developed a method of evaluating patients' prognosis based on pulmonary, heart, renal, and hepatic function, and on the presence of hypertension, glucose tolerance impairment, anemia, and hypoproteinemia. Three evaluation grades were established for each item, and the score was based on the preoperative status classification system of the American Society of Anesthesiologists (ASA). Wallace et al. [35] had earlier assessed 322 elderly HF patients with reference to their social circumstances and medical state. Those who were totally independent received one point; those living alone with help received two points, and those living in an institution received three points. With regard to medical state, those in good general health received one point, those with satisfactory general health but a history of previous serious illness received two points, and those with poor health received three points. The scores from both categories were summed giving each patient a possible combined score of two to six. The authors concluded that those patients with scores of 3 or less could be expected to make satisfactory progress during rehabilitation, while those with scores of 5 or 6 were unlikely to return to their pre-fracture status. Another study [36] on only 63 patients developed a prognostic score based on the patients' pre-injury level of independence in activities of daily living, medical comorbidities, and Pfeiffer's mental scoring system.
To our knowledge, this is the first description of a model predicting recovery of walking ability and functional status on the basis of data gleaned from a structured, comprehensive, multidimensional assessment of old HF patients. Of note, to construct this score, we used parameters that particularly characterize aged patients and are frequently used in rehabilitation settings. Indeed, the score included demographic and social factors (age and gender), the evaluation of nutritional (body mass index) and health status (number of drugs), while functional and cognitive parameters were derived from the Barthel index (referred to pre-fracture status), IADL, and the MMSE. These sensitive tools have been validated in several settings [12, 14, 18, 19], are widely available, and are used in the majority of facilities specialized in the rehabilitation and long-term care of elderly patients. The finding that the prognostic value of the summed score was superior to that of the individual components considered singularly indirectly suggests that it has a greater potential to predict patient recovery with respect to single components. In fact, although the univariate analysis and the ROC curves seem to suggest that there is no difference between the score and the Barthel index in terms of sensitivity and specificity, the multivariate logistic regressions demonstrate that the new score, after adjustment for all potential predictors, maintained its significant, independent power with regard to all the outcomes (i.e., “walking ability at discharge”, “walking ability 12 months after discharge”, and “death 12 months after discharge”), while the pre-fracture Barthel index predicted only selective outcomes (i.e., “walking ability at discharge”, “walking ability 12 months after discharge”). Moreover, the Barthel index is a self-reported tool (and therefore quite subjective) and, in this study, its predictive power was partially limited by a collinearity between the predicting variable (i.e., the pre-fracture Barthel index assessed on admission) and the outcome measures (i.e., the subscore walking ability and the total score of the Barthel index assessed at discharge). The score being proposed instead also depends on several “objectively based” tools of assessment (such as the BMI and the MMSE).
This model has several potential uses in clinical in healthcare and research settings.
The aim of HF rehabilitation following HF surgery is to restore the patient's walking independence and functional status to pre-fracture levels, but many do not recover their independence despite intensive rehabilitation programs [37–39]. Our model could be used to identify, already at the time of admission, patients with different risk levels of unsuccessful recovery so that specific, personalized interventions can be targeted. This method could, for example, be useful in identifying high-risk patients who would probably benefit from advanced care assistance programs and not traditional rehabilitation. The method could also be utilized by healthcare administrators to promote development of post-acute care settings adapted to patients' needs. Patients with a higher risk of unsuccessful recovery would probably do better in settings where the approach is predominantly clinical, while those at lower risk may benefit from facilities with a predominantly physiotherapic approach.
The method could also be used by researchers designing epidemiological studies assessing procedures, treatments, and interventions geared towards patients with similar risk levels and benchmarking studies comparing costs and outcomes in facilities caring for patients with similar risk profiles.
It is evident that our findings cannot be extrapolated to younger populations, and that further studies are needed to validate a similar risk score in non-geriatric as well as in non-selected geriatric populations. The fact that we did not assess variables with possible implications on recovery, such as the degree of preoperative risk, the type of anaesthesia utilized, and vitamin D levels should be considered one of the study's limitations.
The problem of identifying patients at high risk of not recovering their pre-fracture walking independence following HF surgery continues to be an important problem in clinical practice [38] since the absolute number of HF in frail, elderly subjects is expected to grow [5]. The prognostic model explicated here may have direct applicability in aiding clinicians and health care administrators in identifying patients at low, medium, and high risk for unsuccessful rehabilitation following HF surgery. Stratifying these patients according to their risk level is an important step in developing targeted programs and interventions in the most efficacious, cost-effective ways to enhance their well-being and quality of care. Further studies are, of course, warranted to validate this tool in different populations and settings.
References
Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB (2009) Incidence and mortality of hip fractures in the United States. JAMA 302:1573–1579
Giversen IM (2006) Time trends of age-adjusted incidence rates of first hip fractures: a register-based study among older people in Viborg County, Denmark, 1987–1997. Osteoporos Int 17:552–564
Melton LJ III, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM, Therneau TM, Leibson CL (2009) Secular trends in hip fracture incidence and recurrence. Osteoporos Int 20:687–694
White SM, Griffiths R (2010) Projected incidence of proximal femoral fracture in England: A report from the NHS Hip Fracture Anaesthesia Network (HIPFAN). Injury (in press)
Holt G, Smith R, Duncan K, Hutchison JD, Reid D (2009) Changes in population demographics and the future incidence of hip fracture. Injury 40:722–726
Boonen S, Autier P, Barette M, Vanderschueren D, Lips P, Haentjens P (2004) Functional outcome and quality of life following hip fracture in elderly women: a prospective controlled study. Osteoporos Int 15:87–94
Holt G, Smith R, Duncan K, Hutchison JD, Gregori A (2008) Outcome after surgery for the treatment of hip fracture in the extremely elderly. J Bone Joint Surg Am 90:1899–1905
Maggi S, Siviero P, Wetle T, Besdine RW, Saugo M, Crepaldi G (2010) A multicenter survey on profile of care for hip fracture: predictors of mortality and disability. Osteoporos Int 21:223–231
Young Y, Fried LP, Kuo YH (2010) Hip fractures among elderly women: longitudinal comparison of physiological function changes and health care utilization. J Am Med Dir Assoc 11:100–105
Kristensen MT (2011) Factors affecting functional prognosis of patients with hip fracture. Eur J Phys Rehabil Med 47:257–264
Bellelli G, Magnifico F, Trabucchi M (2008) Outcomes at 12 months in a population of elderly patients discharged from a rehabilitation unit. J Am Med Dir Assoc 9:55–64
Matthews LE (1985) Using anthropometric parameters to evaluate nutritional status. J Nutr Elderly 5(2):67–71
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Shah S, Vanclay F, Cooper B (1989) Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol 42:703–709
Granger CV, Cotter AC, Hamilton BB, Fiedler RC (1993) Functional assessment scales: a study of persons after stroke. Arch Phys Med Rehabil 74:133–138
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34:119–126
Franchignoni FP, Tesio L, Ricupero C, Martino MT (1997) Trunk control test as an early predictor of stroke rehabilitation outcome. Stroke 28:1382–1385
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Sheikh JI, Yesavage JA (1986) Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clinical gerontology: a guide to assessment and intervention. The Haworth Press, NY, pp 165–173
Sourial N, Wolfson C, Zhu B, Quail J, Fletcher J, Karunananthan S, Bandeen-Roche K, Beland F, Bergman H (2010) Correspondence analysis is a useful tool to uncover the relationships among categorical variables. J Clin Epidemiol 63:638–646
Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD (1995) Ambulatory ability after hip fracture. A prospective study in geriatric patients Clin Orthop Relat Res 310:150–159
Lieberman D, Fried V, Castel H, Weitzmann S, Lowenthal MN, Galinsky D (1996) Factors related to successful rehabilitation after hip fracture: a case–control study. Disabil Rehabil 18:224–230
Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM (2009) Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br 91:922–927
Haentjens P, Autier P, Barette M, Venken K, Vanderschueren D, Boonen S (2007) Survival and functional outcome according to hip fracture type: a one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone 41:958–964
Morrison RS, Magaziner J, McLaughlin MA, Orosz G, Silberzweig SB, Koval KJ, Siu AL (2003) The impact of post-operative pain on outcomes following hip fracture. Pain 103:303–311
Carson JL, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, Noveck H, Strom BL (1996) Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet 348:1055–1060
Young Y, Xiong K, Pruzek RM (2011) Longitudinal functional recovery after post-acute rehabilitation in older hip fracture patients: the role of cognitive impairment and implications for long-term care. J Am Med Dir Assoc 12:431–438
Beloosesky Y, Weiss A, Grinblat J, Brill S, Hershkovitz A (2004) Can functional status, after rehabilitation, independently predict long-term mortality of hip-fractured elderly patients? Aging Clin Exp Res 16:44–48
Parker MJ, Palmer CR (1995) Prediction of rehabilitation after hip fracture. Age Ageing 24:96–98
Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison RS (2006) Early ambulation after hip fracture: effects on function and mortality. Arch Intern Med 166:766–771
Torpilliesi T, Bellelli G, Morghen S, Gentile S, Ricci E, Turco R, Trabucchi M (2011) Outcomes of nonagenarian patients after rehabilitation following hip fracture surgery. J Am Med Dir Assoc (in press)
Hagino T, Ochiai S, Wako M, Sato E, Maekawa S, Senga S, Sugiyama H, Hamada Y (2007) A simple scoring system to predict ambulation prognosis after hip fracture in the elderly. Arch Orthop Trauma Surg 127:603–606
Masuda T, Miura N, Ishii S, Hibino Y, Beppu M (2004) New preoperative evaluation system of the physical findings of aged patients with femoral neck fracture. J Orthop Sci 9:434–439
Wallace RG, Lowry JH, McLeod NW, Mollan RA (1986) A simple grading system to guide the prognosis after hip fracture in the elderly. Br Med J (Clin Res Ed) 293:665
Hashmi MA, Tellisi N, Rigby AS, Wahab KH (2004) The value of a prognostic scoring system in the rehabilitation of elderly patients with proximal femoral fractures. Int J Clin Pract 58:2–5
Marottoli RA, Berkman LF, Cooney LM Jr (1992) Decline in physical function following hip fracture. J Am Geriatr Soc 40:861–866
Osnes EK, Lofthus CM, Meyer HE, Falch JA, Nordsletten L, Cappelen I, Kristiansen IS (2004) Consequences of hip fracture on activities of daily life and residential needs. Osteoporos Int 15:567–574
Shyu YI, Chen MC, Liang J, Wu CC, Su JY (2004) Predictors of functional recovery for hip fractured elders during 12 months following hospital discharge: a prospective study on a Taiwanese sample. Osteoporos Int 15:475–482
Acknowledgments
The authors wish to thank Dr. Sara Morghen for the management of database and Drs. Tiziana Torpilliesi, Alessandra Marrè, Eleonora Ricci Elena Lucchi, and Salvatore Speciale for collecting data. Sincere appreciation is due to the team of physical therapists for their support in rehabilitation activities and to Linda Inverso Moretti for reviewing the English version of this manuscript.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bellelli, G., Noale, M., Guerini, F. et al. A prognostic model predicting recovery of walking independence of elderly patients after hip-fracture surgery. An experiment in a rehabilitation unit in Northern Italy. Osteoporos Int 23, 2189–2200 (2012). https://doi.org/10.1007/s00198-011-1849-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1849-x