Abstract
Objective
The aim of the present study was to compare decision-making and cognitive flexibility in patients with disordered eating and weight, ranging from anorexia nervosa to obesity, and a healthy group.
Method
Participants were 113 patients (86 with eating disorders and 27 with obesity), and a group of 39 healthy subjects; all completed the Iowa gambling task, the Wisconsin Card Sorting Test and several clinical self-report measures.
Results
Eating disordered and obese patients showed impaired performance on the decision-making task, and the obese group showed the worst performance on the set-shifting task. There were no associations between neuropsychological performance and eating or obsessive symptomatology, although significant associations were found with anxiety and depression measures.
Discussion
Considering the executive functions as a transdiagnostic process in ED and obesity could provide explanations for the inability to regulate food intake, present in both ED and obese patients. Implications of these executive impairments in the development and maintenance of ED and obesity are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eating behavior is a complex process. It provides the necessary input for the essential body functions and can be stimulated by hunger, cravings or hedonic sensations [1]. People have to choose when and how much to eat, but sometimes this process does not work in a healthy way, as in the case of eating disorders (ED) and obesity. ED are characterized by an altered eating pattern and the over-evaluation of figure and weight in one’s self-concept. In this category, the DSM-5 [2] includes anorexia nervosa (AN), bulimia nervosa (BN) and binge eating disorder (BED), with the high co-occurrence between the latter disorder and obesity being relevant [3]. Obesity is not a mental disorder; it is defined by an excessive accumulation of body fat, specifically a body mass index (BMI) greater than 30 kg/m2. Interest in this medical condition has increased in the past two decades because obesity has become a serious health problem causing extensive economic costs worldwide [4]. Losing weight and, especially, maintaining weight loss are not easy issues. Even with the help of professionals, weight regain typically occurs when professional management ends, and 3–5 years post-treatment, about 85 % of patients have regained the lost weight or even exceeded their pretreatment weight [5].
In recent years, it has become increasingly important to consider ED and obesity as two poles on the same continuum of problems related to eating and weight. Within these two conditions, a wide variety of types of disordered eating represent some anomalous functioning patterns, including body dissatisfaction, unhealthy behaviors to lose weight, or the inability to maintain the lost weight [6]. Obesity per se is a specific risk factor for BN and BED, and individuals with obesity often have an ED as well [7, 8]. Both ED and obesity are associated with maladaptive eating styles that may be relevant to their development and maintenance [9].
As mentioned above, eating is not an automatic process, and it is influenced by a complex interplay among physiological, psychological, social and genetic factors that influence meal timing, quantity of food intake and food preferences [10]. In eating behavior people are confronted with ongoing temptations motivating food intake within an environment characterized by an abundance of highly palatable food [11]. In this set of choices, the patients with anorexia nervosa seems to rigidly decide to give up eating, the decision to stop eating in the patients with bulimia nervosa is interrupted by the urge to binge eat, and in the case of the patients with obesity, the decision to go on a diet and lose weight is usually unstable. The regulatory process involved in response inhibition and decision-making is related to the executive functions [12].
The executive functions encompass a number of cognitive processes that allow the initiation, planning, regulation, inhibition, sequencing and achievement of goal-oriented behavior and complex thought, all of which may impact eating behavior [4]. Executive function studies in ED have found dysfunctions in decision-making, response inhibition and cognitive flexibility, independently of illness severity or BMI [13, 14]. Neuropsychological assessments in AN have revealed some consistent impairments in executive functions, specifically poor flexibility or set-shifting (the ability to switch tasks flexibly or the mental ability to change one’s behavior when the rules change), ineffective decision-making (poor capacity to make decisions about a course of action), and weak central coherence (the tendency to focus excessively on details, with problems integrating elements appropriately in their context) [15], although for BN the executive malfunctions are less clear [16]. Such findings are consistent with the clinical observation that these patients tend to be cognitively rigid and persistent.
In contrast with the development in the ED field, few reviews have specifically examined executive functioning in obesity; in these studies a poor executive functioning performance has also been described, such as reduced decision-making abilities or problems related to impulsivity [17–20].
As far as we know, only two studies have compared executive function performance over a broad ED and weight spectrum, that is, including AN, BN and obese patients [17], or AN and obese patients [14]. The results showed that patients with AN, BN and obesity performed significantly worse than healthy controls. Group differences were more marked in the cognitive flexibility and decision-making domains. Regarding the comparison of AN and obese patients, both showed a pattern of choices resulting in elevated immediate gains despite future losses, with similar levels of impairment, which is the expression of their deficit in planning everyday functioning [21].
The aim of the current study was to compare the performance on neuropsychological tasks, more specifically, decision-making and cognitive flexibility abilities, in patients with disordered eating and weight, covering a wide range from AN restrictive subtype to obesity, differentiating restrictive and purging symptoms, and comparing these patients to a healthy comparison group. To neutralize the influence of other variables in the performance differences, socio-demographic characteristics (age, and level of education) and clinical measures (BMI, depression, anxiety and obsessive symptoms) were controlled. In addition, possible relationships between executive function performance and eating and general psychopathology were analyzed.
Method
Participants
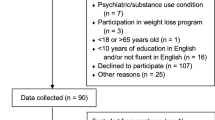
Both healthy and clinical individuals participated in this study. Socio-demographic characteristics of the groups are presented in Table 1. The clinical sample was composed of 113 patients. Twenty-seven (23 women) were obese patients (OB group) [age range 19–65; body mass index (BMI) range 31.48–67.16]. The inclusion criteria were having a BMI above 30 and not meeting diagnostic criteria for binge eating disorder according to the DSM-IV-TR [22]. The second group was composed of 86 ED patients [22]. Specifically, there were 18 women with AN restricting type (ANR) (age range 13–43, BMI range 13.18–17.11); 10 women with AN binge eating/purging type (ANP); 25 women with bulimia nervosa purging type (BNP); 21 patients (19 women) fulfilled the criteria for eating disorder not otherwise specified (AN type; ED.AN) (age range 13–47; BMI 17.77–23.54); and 12 patients (10 women) fulfilled the criteria for eating disorder not otherwise specified (BN type; EDNOS.BN). To simplify the composition of the analysis of the patient groups, and according to those studies interested in the difference between restrictive/binge-purge symptomatology in the neuropsychological profile [39, 43, 44, 52], those patients who presented bingeing/purging symptomatology (ANP, BNP, and EDNOS.BN) were grouped under the name “Bingeing/Purging group” (BP-G), consisting of 47 patients (45 women) (age range 17–44; BMI range 15.13–29.38). Thus, the clinical sample of this study was composed of ANR (18), ED.AN (21), BP-G (47) and OB (27) groups. The clinical sample was receiving their usual treatment (cognitive behavior therapy, diet therapy, or in some cases, psychopharmacological treatment, usually antidepressants, anxiolytics, or anticonvulsants).
Finally, the healthy comparison group (HCG) was composed of 39 participants (30 women; age range 19–56), recruited at the University of Valencia (undergraduate and postgraduate students). The inclusion criteria were not having any mental disorder and being normal weight (BMI 20–25). All the participants were white/caucasian.
The one-way ANOVA showed differences in age (the youngest group was the ANR group, and the oldest group was the OB group) and educational level, revealing that most of the obese participants had only finished primary education. As expected, significant differences were found in the BMI of the participants (lowest in ANR and highest in OB).
Measures
Self-report measures. Different questionnaires were administrated to participants to assess clinical variables to control their effects on performance on the neuropsychological assessment.
Eating attitudes test (EAT-26) [23]. This is a 26- items self-report questionnaire that assesses attitudes and behaviors related to ED on a 6-point Likert scale (never-always). It has three subscales (Dieting, Bulimia and Food Preoccupation, and Oral Control), and the total score measures symptom severity. The Spanish version used in this study [24] has shown good internal consistency in the present sample (α = . 92).
Clark-Beck Obsessive–Compulsive Inventory (CBOCI) [25, 26]. This is a 25-item self-report questionnaire that assesses the frequency of obsessive and compulsive symptoms on a 4-point scale (never-always). The Spanish version of this inventory [27] has shown good internal consistency in the present study (Total score α = .88; Obsessions scale α = .84; Compulsions scale α = .77).
Beck depression inventory (BDI) [28]. This is a 21-item self-report measure of the intensity or severity of depressive symptoms, with a 4-point scale ranging from 0: Symptom not present to 3: Symptom very intense. The Spanish version [29] was used, obtaining an internal consistency for the present study of .94.
Beck anxiety inventory (BAI) [30]. This self-report evaluates anxiety-related somatic symptoms across 21 items rated on a 4-point Likert-type scale from 0: Not at all to 3: Severely. In the present study, the Cronbach’s α value was .93.
Neuropsychological assessment. Decision-making ability was assessed by a computerized version of the Iowa gambling task (IGT) [31]. This instrument simulates the main components used in decision-making in real life, such as the evaluation of rewards and punishment in situations of risk and uncertainty. The computer presents participants with four identical decks of cards. Two decks (A&B) are disadvantage decks, or high-risk decks, which provide high immediate gain, but larger future losses. The other two decks (C&D) are advantageous decks, or low-risk decks, which provide lower immediate gain, but smaller future losses. Initially, the computer gives the participant $2000, and the subject’s task consists of choosing among the four decks in each trial, using a computer mouse, to try to win the maximum amount of money. After each choice, the participant receives immediate feedback from the computer about the losses or gains. To get more money at the end of the test, the participant should choose more cards from the advantageous decks.
The classic analysis of the IGT provides two types of results. It can analyze the global outcome score (net score), which give us information about whether the participants have the ability to sacrifice immediate rewards to achieve higher long-term gains. Moreover, the score by blocks is obtained by dividing the 100 trials into five blocks of 20 and analyzing a net score for each block, which provides information about the subjects’ learning throughout the trials. Lower scores represent worse performance; negative scores reflect a preference for disadvantageous choices.
Cognitive flexibility and control of impulsive responses were assessed with a computerized version of the Wisconsin Card Sorting Test (WSCT) [32]. Four stimulus cards with different symbols (which differ in color, number or shape) are presented on the computer screen. Participants are instructed to match a response card (which is also presented on the computer screen) with one of the four stimulus cards according to a criterion (which can be color, number or form). The computer does not reveal the classification criterion; however, it gives feedback after each trial, specifically telling the participant whether the match is right or wrong. When the participant makes 10 consecutive correct pairings, the computer changes the criterion for matching the cards. The test ends when all 128 response cards have been presented. Different scores can be calculated. In this study, the three most widely used indexes were calculated: “total categories completed”, “perseverative errors”; and “the total number of errors”.
Procedure
Clinical participants were recruited from the Research Unit for Obsessive–Compulsive and Eating Disorders of the University of Valencia (Spain) and outpatient mental-health clinics in the Spanish National Health System. Participants from the community were recruited from under/post-graduate courses at the University of Valencia. Before being included, all potential participants were individually screened with a semi-structured interview by the authors, who are all Ph.D. level Clinical Psychologists and have several years of experience conducting diagnostic evaluations in clinical settings. Information about basic demographic data (age, gender, educational level, socio-economic status) was also recorded. Current and lifetime ED diagnoses (inclusion and exclusion) were confirmed with the Structured Clinical Interview for DSM-IV-TR [33, 34].
After clinical and healthy participants had given his or her explicit informed consent to participate in the study, the neuropsychological assessment was completed individually in the presence of the experimenter. Next, each participant filled out the self-report questionnaires, and weight and height data were collected. The study received the approval of the ethics committees of the University of Valencia and the outpatient mental-health units of the National Health System.
Statistical analyses
We used Kolmogorov–Smirnov to check the normality of the variables under study. The homogeneity of variance assumption was tested with Levene’s test. The Q–Q plots were used to get an indication of the amount of non-normality, and data were screened for the presence of outliers. Outliers were removed if necessary. After all these measures, and given that the ANOVA and MANOVA models were quite robust [35–38] to the lack of normality, the use of flexible and more powerful parametric tests was preferred. First, a set of preliminary analyses were conducted to compare the groups on the socio-demographic variables. The Chi-squared test was used to compare them on educational level. Analyses of variance (ANOVA) were carried out to compare groups on the clinical variables; significance of F or Brown-Forsythe was observed.
For the IGT performance, the global score was calculated as the difference in the number of cards selected from the advantageous and disadvantageous decks (C + D)–(A + B), and the differences among groups were analyzed by applying one-way ANOVA. Then, the 100 trials were divided into five blocks, and the net scores in each block were calculated using the same procedure. The between-group comparisons were performed with repeated-measures ANOVA. Regarding the WCST, the performance on the three indexes (total categories completed, perseverative errors and total errors) was analyzed with a multivariate analysis of variance (MANOVA) among the groups. Post hoc analyses were conducted using the Bonferroni correction for multiple comparisons. On the socio-demographic and clinical variables that showed group differences, ANCOVA and MANCOVA were performed to control their influence on neuropsychological performance.
Pearson correlations were used to evaluate the relationships between the neuropsychological measures (IGT and WCST) and the clinical variables (mood, obsessive and eating symptomatology). Statistical analyses were performed using SPSS v.20 (SPSS Inc., Chicago, Illinois).
Results
Sample characteristics
Clinical characteristics of the groups are presented in Table 2. The analysis revealed that all the clinical groups had higher scores than the HCG on depression measures (BDI). There were also differences on the anxiety measures (BAI); specifically, ANR, ED.AN and BP-G had higher scores than HCG. Results for CBOCI showed that the OB group and the HCG obtained the lowest scores, and the ANR group had the highest scores on both the obsession and compulsion scales. Finally, on the eating psychopathology measures, there were significant differences between groups, with all the groups of ED patients scoring higher on these scales, as expected.
IGT performance
Table 3 shows the means for the total IGT net scores in each group. Differences among groups in total IGT net score have been shown with a one-way ANOVA. Post hoc comparisons indicated that all the clinical groups performed worse than the HCG group. Since BMI, age, level of education, depression, anxiety, obsessive symptoms and eating psychopathology showed differences among groups, these variables were considered as covariates in an ANCOVA. The analysis indicated that the differences in the total IGT net scores were maintained [F (1,98) = 4.097, p < .05; η 2 p = .143].
A repeated-measures ANOVA was carried out with the scores of each the five blocks. Mauchly’s test indicated that sphericity was not assumed (χ 2 (9) = .59; p = .0001), and we used Greenhouse-Geisser to correct the degrees of freedom (ε = .785). Results showed a significant main effect of Block [F (3.14, 461.45) = 6.495, p < .05; η 2 p = .042], a significant main effect of group [F (4, 147) = 6.851, p < .05; η 2 p = .157] and a significant Block × Group interaction [F (12.55, 461.45) = 2.703, p < .05; η 2 p = .069], indicating a different IGT performance between clinical groups and HCG (ANR vs HCG, p = .005; BP-G vs HCG, p = .0001; ED.AN vs HCG, p = .004; OB vs HCG, p = .002). Controlling for socio-demographic and clinical variables (age, BMI, level of education, depression and anxiety measures, obsessive symptoms and eating psychopathology) with a MANCOVA, the main effect for groups and the effect for the Block × Groups interaction remained significant. Trend analyses across IGT blocks within each group showed that clinical groups did not show learning during the task. Table 3 shows the means for each group in each bloc.
WCST performance
Table 3 provides groups’ mean scores on the WCST performance indexes used in this research. MANOVA showed significant differences among the subgroups on all the variables measured Pillai’s Trace (V = .388, F (12, 438) = 5.425, p < .001, η 2 p = .129). There was a significant difference in “total categories completed”. Post hoc analysis revealed that the obese group completed fewer categories than the other groups, showing significant differences with all of them, and the group of eating disorder not otherwise specified, anorexia type, presented significant differences when compared to the healthy comparison group. As differences among groups on clinical and socio-demographic variables could influence WCST performance, a MANCOVA was performed for each of the covariates to control them. This analysis indicated that the significant differences obtained previously were maintained. In addition, there were significant differences among groups on “number of perseverative errors”. Post hoc comparisons indicated that the OB and ED.AN groups made significantly more perseverative errors than the rest of the groups. MANCOVA indicated that the difference between groups remained significant. Finally, the results revealed significant differences among groups on “number of total errors”. Post hoc comparisons showed that the OB and ED.AN groups made significantly more errors than the rest of the groups. Group differences were maintained when we controlled the effect of the covariates.
Association between neuropsychological performance and clinical measures
The relationship between clinical variables and neuropsychological variables was analyzed using Pearson’s correlations. Results showed that there were no significant associations between the obsessive and compulsive CBOCI scales or the EAT scores and the IGT total net scores or the three WCST indexes (see Table 4). Mood variables were significantly related to some neuropsychological scores: a positive relationship was found between BDI and BAI and “number of total errors” on the WCST, respectively; and negative correlations were found between BAI and “total categories completed” on the WCST, and between BDI and BAI and IGT total net scores, respectively.
Discussion
The aim of the present study was to analyze the executive functions of ED and obese patients, specifically their decision-making and cognitive flexibility abilities, when compared to a healthy control group. Regarding the clinical variables analysis, as expected, both ED and obese patients scored higher on anxiety, depression and eating psychopathology measures. The association between eating symptomatology and general psychopathology has consistently been found in several studies, not only in ED but also in obesity [8]. However, the psychopathology most frequently found in obesity is related to mood symptoms, while in ED obsessive symptoms and rigid thinking styles are frequently present, especially in ANR [39].
On decision-making performance, results showed that the clinical participants preferred immediate gains but larger future losses, obtaining a negative net score on the IGT compared to the HGC. Moreover, trend analysis across IGT blocks within each group revealed that the clinical sample did not learn during the task. These data are similar to those obtained by others [14, 40], where ED and obese samples showed impaired performance on a decision-making task and failed to learn during the process. The IGT performance deficits in ED and obesity have been found regardless of age, gender, BMI [17, 40, 41] and years of education [17, 40, 42], and we can add level of education, mood and obsessive symptoms, and severity of eating symptoms. Together, these results provide some evidence that both types of patients shared a similar inability to modulate reward and punishment using a long-term perspective, with their behavior guided by immediate rewards (restrictive eating, binges, purges, or palatable food), despite the severe long-term effects on their bodies and weight [40]. In other words, this neuropsychological task can also reveal decision-making impairments in the inability to regulate food intake [41].
When the groups were compared on a set-shifting task (WCST), one group’s performance was clearly the worst: the obese patients. In neuropsychological studies of AN, poor flexibility is a consistent finding in different studies [15], and a recent meta-analysis on the spectrum of eating disorders, overweight and obesity [43] provides strong support that inefficient set-shifting is a salient neuropsychological phenomenon across ED subtypes and obesity. Another result of this meta-analysis was that this evidence was stronger in ANR than in AN purgative subtypes. In contrast, our study did not find differences among ANR, ED.AN (similar to ANR diagnosis) and the binge/purge group). A recent study [44] found that patients with binge eating disorder, some with obesity, were characterized by poorer decision-making and cognitive flexibility compared to AN restrictive-type patients. The communality in poor set-shifting ability supports the idea that EDs and obesity lie on a continuum and share several neurobiological and neurocognitive features [14, 43, 45].
Regarding the second objective, we found significant associations between neuropsychological and mood variables. Anxiety and depression measures have an influence on the quality of performance on decision-making and on different aspects of the set-shifting ability. This finding agrees with some studies [21, 46] that found relationships between mood symptoms and neuropsychological performance. One study [21] found associations with anxiety, but not with depression; however, the executive functions were assessed with different tasks from the IGT and WCST.
Executive dysfunctions have been found in several studies on ED, independently of illness severity or BMI. Obesity needs to be considered as a condition associated with decision-making deficits and poor set-shifting. These executive (dys-) functions influence performance on preferring immediate reward, without considering negative future outcomes, and having a rigid thinking style, and these functions could contribute to the inability to regulate food intake. In the case of obesity, this can be translated into becoming obese, but it can also reflect the difficulty of maintaining weight loss after weight reduction treatment [40]. Moreover, ED and obese patients show strong resistance to change. Along these lines, treatments for ED and obesity should consider these aspects. In recent years, cognitive remediation therapy (CRT), a therapeutic approach devoted to helping to improve patients’ mental flexibility, global thinking strategies, or decision-making, has been adapted for interventions in eating disorders [47] and obesity [48], showing promising results. This implementation of the treatment is intended to improve the executive function, helping patients to manage their eating behavior and use more effective weight loss maintenance strategies. Recent findings from neuroscience indicate that the brain, thinking, and the information processing style are capable of changing over the lifespan. Some specific functions such as cognitive flexibility, problem solving, impulsiveness, etc., need to be related to the modern neuroimaging studies on ED to clarify their role in the etiology of ED and their consequences for each ED type, and their relationship with obesity. The possibility of a dysfunction of the central nervous system in patients with ED has been explored by means of neuropsychological assessment; for example the WCST allows the measurement of cortical function during instrumental learning and reinforcement, essential processes for efficient flexible behavior [49]. These recent neuroimaging studies begin to offer insights into the etiology of ED and options for the direction of future treatments and therapeutic strategies. And finally, transdiagnostic perspectives and dimensional concepts have received increasing attention in recent years [50, 51]. Considering the executive functions as a transdiagnostic process in ED and obesity can play a role in explaining the diagnostic cross-over between ED categories and the co-morbidity between EDs and obesity.
This study has several limitations. The groups were composed mainly of women, so that the results cannot be analyzed from a gender perspective. Therefore, replication with a larger group, including males, would be desirable. Future research should consider factors that were not controlled for here, such as IQ or illness duration, which may impact IGT and WCST performance. Moreover, because the nature of the present data is cross-sectional, future studies should include longitudinal data. However, as far as we know, the present study is the only one that has compared executive function performance over a broad ED and weight spectrum, including obesity, but differentiating restrictive and purgative ED symptoms. The results revealed dysfunctional decision-making and poor flexibility (set-shifting) in ED and obese patients, with no differences among them, highlighting the worse performance of obese patients on set-shifting abilities. The study of neuropsychological abilities in ED and obesity may be important for improving our knowledge about eating and weight disorders, including a better understanding of ED categories [52] and how to optimize their therapeutic approach.
References
Ahima RS, Antwi DA (2008) Brain regulation of appetite and satiety. Endocrinol Metab Clin N Am 37(4):811–823. doi:10.1016/j.ecl.2008.08.005
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association, Arlington. doi:10.1176/appi.books.9780890425596
Villarejo C, Fernández-Aranda F, Jiménez-Murcia S, Peñas-Lledó E, Granero R, Penelo E, Tinahones FJ, Sancho C, Vilarrasa N, Montserrat-Gil de Bernabé M, Casanueva FF, Fernández-Real JM, Frübeck G, De la Torre R, Treasure J, Botella C, Menchón JM (2012) Lifetime obesity in patients with eating disorders: increasing prevalence, clinical and personality correlates. Eur Eat Disord Rev 20(3):250–254. doi:10.1002/erv.2166
Raman J, Smith E, Hay P (2013) The clinical obesity maintenance model: an integration of psychological constructs including mood, emotional regulation, disordered overeating, habitual cluster behaviours, health literacy and cognitive function. J Obes 2013:1–9. doi:10.1155/2013/240128
Cooper Z, Doll HA, Hawker DM, Birne S, Bonner G, Eeley E, O’Connor ME, Fairburn CG (2010) Testing a new cognitive behavioral treatment for obesity: a randomized controlled trial with three-year follow-up. Behav Res Ther 48(8):706–713. doi:10.1016/j.brat.2010.03.008
Perpiñá C, Roncero M, Fernández-Aranda F, Jiménez-Murcia S, Forcano L, Sánchez I (2013) Clinical validation of a virtual environment for normalizing eating patterns in eating disorders. Compr Psychiatry 54(6):680–686. doi:10.1016/j.comppsych.2013.01.007
Loth KA, MacLehose R, Bucchianeri M et al (2014) Predictors of dieting and disordered eating behaviors from adolescence to young adulthood. J Adolesc Health 55:705–712. doi:10.1016/j.jadohealth.2014.04.016
Villarejo C, Jiménez-Murcia S, Álvarez-Moya E, Granero R, Penelo E, Treasure J, Vilarrasa N, Gil-Montserrat de Bernabé M, Casanueva FF, Tinahones FJ, Fernández-Real JM, Frühbeck G, De la Torre R, Botella C, Agüera Z, Menchón JM, Fernández-Aranda F (2014) Loss of control over eating: a description of the eating disorder/obesity spectrum in women. Eur Eat Disord Rev 22(1):25–31. doi:10.1002/erv.2267
Krug I, Villarejo C, Jiménez-Murcia S, Perpiñá C, Vilarrasa N, Granero R, Cebolla A, Botella C, Montserrat-Gil de Bernabe M, Penelo E, Casella S, Islam MA, Orekhova E, Casanueva FF, Karwautz A, Menchón JM, Treasure J, Fernández-Aranda F (2013) Eating-related Environmental Factors in Underweight Eating Disorders and Obesity: Are there common vulnerabilities during childhood and early adolescence? Eur Eat Disord Rev 21(3):202–208. doi:10.1002/erv.2204
Grimm ER, Steinle NI (2011) Genetics of eating behavior: established and emerging concepts. Nutr Rev 69(1):52–60. doi:10.1111/j.1753-4887.2010.00361.x
Svaldi J, Schmitz F, Trentowska M, Tuschen-Caffier B, Berking M, Nauman E (2014) Cognitive interference and food related memory bias in binge eating disorder. Appetite 72:28–36. doi:10.1016/j.appet.2013.09.014
Hofmann W, Schmeichel BJ, Baddeley AD (2012) Executive functions and self-regulation. Trends Cogn Sci 16(3):74–180. doi:10.1016/j.tics.2012.01.006
Tchanturia K, Liao PC, Uher R, Lawrence N, Treasure J, Campbell IC (2007) An investigation of decision making in anorexia nervosa using the Iowa Gambling Task and skin conductance measurements. J Int Neuropsychol Soc 13(4):635–641. doi:10.1017/S1355617707070798
Fagundo AB, De la Torre R, Jiménez S, Agüera Z, Granero R, Tárrega S, Botella C, Baños R, Fernández-Real JM, Rodríguez R, Forcano L, Frübeck G, Gómez-Ambrosi J (2012) Executive function profile in extreme eating/weight conditions: from anorexia nervosa to obesity. PLoS One 7(8):e43382. doi:10.1371/journal.pone.0043382
Tchanturia K, Harrison A, Davies H, Roberts M, Oldershaw A, Nakazato M, Stahl D, Morris R (2011) Cognitive flexibility and clinical severity in eating disorders. PLoS One 6(6):e20462. doi:10.1371/journal.pone.0020462
Van den Eynde F, Guillaume S, Broadbent H, Campbell I, Schmidt U, Tchanturia K (2011) Neurocognition in bulimic eating disorders: a systematic review. Acta Psychiatr Scand 124(2):120–140. doi:10.1111/j.1600-0447.2011.01701.x
Brogan A, Hevey D, Pignatti R (2010) Anorexia, bulimia, and obesity: shared decision making deficits on the Iowa Gambling Task (IGT). J Int Neuropsychol Soc 16(4):711–715. doi:10.1017/S1355617710000354
Danner UN, Ouwehand C, van Haastert NL, Hornsveld H, de Ridder DT (2011) Decision-making impairments in women with binge eating disorder in comparison with obese and normal weight women. Eur Eat Disord Rev 20(1):56–62. doi:10.1002/erv.1098
Fitzpatrick S, Gilbert S, Serpell L (2013) Systematic review: are overweight and obese individuals impaired on behavioural tasks of executive functioning? Neuropsychol Rev 23(2):138–156. doi:10.1007/s11065-013-9224-7
Pignatti R, Bertella L, Albani G, Mauro A, Molinari E, Semenza C (2006) Decision making in obesity: a study using the Gambling Task. Eat Weight Disord 11(3):126–132. doi:10.1007/BF03327557
Billingsley-Marshall RL, Basso MR, Lund BC, Hernandez ER, Johnson CL, Drevets WC, McKee PA, Yates WR (2013) Executive function in eating disorders: the role of state anxiety. Int J Eat Disord 46(4):316–321. doi:10.1002/eat.22086
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders (4th ed, text revision). American Psychiatric Press, Washington. doi:10.1176/appi.books.9780890425596.744053
Garner DM, Garfinkel PE (1979) The eating attitudes test: an index of the symptoms of anorexia nervosa. J Psychol Med 9(2):273–279. doi:10.1017/S0033291700030762
Castro J, Toro J, Salamero M, Guimerá E (1991) The eating attitudes test: Validation of the Spanish version. Evaluación Psicológica 7(2):175–190
Clark DA, Beck AT (2002) Manual for the Clark-Beck obsessive compulsive inventory. Psychological Corporation, San Antonio
Clark DA, Antony MM, Beck AT, Swinson RP, Steer RA (2005) Screening for obsessive and compulsive symptoms: validation of the clark-beck Obsessive–Compulsive inventory. Psychol Assess 17:132–143. doi:10.1037/1040-3590.17.2.132
Belloch A, Reina N, García-Soriano G, Clark DA (2009) El Inventario Clark-Beck de Obsesión-Compulsión (C-BOCI): Validación para su uso en población española. Revista de Psicopatología y Psicología Clínica 14:95–105. doi:10.5944/rppc.vol.14.num.2.2009.4069
Beck AT, Steer RA, Ball R, Ranieri WF (1996) Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J Personal Assess 67(3):588–597. doi:10.1207/s15327752jpa6703_13
Sanz J, Vázquez C (1998) Fiabilidad, validez y datos normativos del inventario para la depresión de Beck. Psicothema 10(2):303–318
Beck AT, Steer RA (1993) Manual for the Beck Anxiety Inventory. Psychological Corporation, San Antonio
Bechara A, Damasio AR, Damasio H, Anderson SW (1994) Insensitivity to future consequences following damage to human prefrontal cortex. Cognition 50:7–15. doi:10.1016/0010-0277(94)90018-3
Berg EA (1948) A simple objective technique for measuring flexibility in thinking. J Gen Psychol 39:15–22. doi:10.1080/00221309.1948.9918159
First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS (1997) Structured clinical interview for DSM-IV axis II personality disorders, (SCID-II). American Psychiatric Press, Washington, DC
First MB, Spitzer RL, Gibbon M, Williams JBW (2002) Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). Biometrics Research, New York State Psychiatric Institute
Harwell MR, Rubinstein EN, Hayes WS, Olds CC (1992) Summarizing Monte Carlo results in methodological research: the one- and two-factor fixed effects ANOVA cases. J Educ Behav Stat 17(4):315–339. doi:10.3102/10769986017004315
Maxwell SE, Delaney HD (2004) Designing experiments and analyzing data: a model comparison perspective. Lawrence Erlbaum Associates, New Jersey
Stevens J (2002) Applied multivariate statistics for the social sciences. Lawrence Erlbaum Associates, New Jersey
Tabachniq B, Fidel LS (2012) Using multivariate statistics. Pearson, New York
Anderluh MB, Tchanturia K, Rabe-Hesketh S, Treasure J (2003) Childhood obsessive-compulsive personality traits in adult women with eating disorders: defining a broader eating disorder phenotype. Am J Psychiatry 160(2):242–247. doi:10.1176/appi.ajp.160.2.242
Brogan A, Hevey D, O’Callaghan G, Yoder R, O’She D (2011) Impaired decision making among morbidly obese adults. J Psychosom Res 70(2):189–196. doi:10.1016/j.jpsychores.2010.07.012
Verdejo A, Pérez M, Schmidt J, Fernández MJ, López G, Martín M, Martín JA, Marcos A, Campoy C (2010) Selective alterations within executive functions in adolescents with excess weight. Obesity 18:1572–1578. doi:10.1038/oby.2009.475
Koritzky G, Yechiam E, Bukay I, Milman U (2012) Obesity and risk taking: A male phenomenon. Appetite 59(2):289–297. doi:10.1016/j.appet.2012.05.020
Wu M, Brockmeyer T, Hatmann M, Skunde M, Herzog W, Friederich HC (2014) Set-shifting ability across the spectrum of eating disorders and in overweight and obesity: a systematic review and meta-analysis. Psychol Med 44(16):3365–3385. doi:10.1017/S0033291714000294
Aloi M, Rania M, Caroleo M, Bruni A, Palmieri A, Cauteruccio MA, Segura-García C (2015) Decision making, central coherence and set-shifting: a comparison between Binge Eating Disorder, Anorexia Nervosa and Healthy Controls. BMC Psychiatry 15(1):6. doi:10.1186/s12888-015-0395-z
Volkow ND, Wang GJ, Tomasi D, Baler RD (2013) Obesity and addiction: neurobiological overlaps. Obes Rev 14(1):2–18. doi:10.1111/j.1467-789X.2012.01031.x
Cserjésia R, Luminetb O, Ponceletb A, Lénárda L (2009) Altered executive function in obesity. Exploration of the role of affective states on cognitive abilities. Appetite 52:535–539. doi:10.1016/j.appet.2009.01.003
Tchanturia K, Lock J (2011) Cognitive Remediation Therapy (CRT) for eating disorders. Development, refinement and future directions. Curr Top Behav Neurosci 6:269–287. doi:10.1007/7854_2010_90
Raman J, Hay P, Smith E (2014) Manualised Cognitive Remediation Therapy for adult obesity: study protocol for a randomized controlled trial. Trials 15:426. doi:10.1186/1745-6215-15-426
Lao-Kaim NP, Fonville L, Giampietro VP, Williams SCR, Simmons A, Tchanturia K (2015) Aberrant function of learning and cognitive control networks underlie inefficient cognitive flexibility in anorexia nervosa: a cross-sectional fMRI study. PLoS One. doi:10.1371/journal.pone.0124027
Fairburn CG, Cooper Z, Shafran R (2003) Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behav Res Ther 41(5):509–528. doi:10.1016/S0005-7967(02)00088-8
García-Soriano G, Roncero M, Perpiñá C, Belloch A (2014) Intrusive Thoughts in Obsessive–Compulsive Disorder and Eating Disorder Patients: A Differential Analysis. Eur Eat Disord Rev 22(3):191–199. doi:10.1002/erv.2285
Van Autreve S, De Baene W, Baeken C, Heeringen C, Vervaet M (2013) Do restrictive and bingeing/purging subtypes of anorexia nervosa differ on central coherence and set shifting? Eur Eat Disord Rev 21(4):308–314. doi:10.1002/erv.2233
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The work has been performed according to ethical standards of the national ethics committee.
Informed consent
Written informed consent was obtained from all of the participants before participation in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding sources
This study is supported by the Spanish Ministerio de Ciencia y Tecnología (Grant PSI2009/10957); Ministerio de Economía y Competitividad (PSI2014-51920-R) and by the Conselleria d’ Educació, Cultura i Esport, Generalitat Valenciana (PROMETEO/2013/066). Centro de Investigación Biomédica en Red Fisiopatología de la Obesidad y Nutrición is an initiative of ISCIII.
Conxa Perpiñá, as member of University of Valencia, has received research grants.
Rights and permissions
About this article
Cite this article
Perpiñá, C., Segura, M. & Sánchez-Reales, S. Cognitive flexibility and decision-making in eating disorders and obesity. Eat Weight Disord 22, 435–444 (2017). https://doi.org/10.1007/s40519-016-0331-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-016-0331-3