Opinion statement
The major progress in the history of medicine represented by the discovery of antibiotics is nowadays compromised by the universal spread of antibiotic resistance. World Health Organization (WHO) lists third-generation cephalosporin-resistant Escherichia coli and Klebsiella pneumoniae and carbapenem-resistant K. pneumoniae in a group of seven bacteria of international concern, responsible for both healthcare-associated and community-acquired infections. Patients infected by these pathogens have limited therapeutic options, worse clinical outcomes, increased mortality rates, and a higher healthcare resources consumption. In infections caused by extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae, appropriate monotherapy is effective and carbapenems are the drugs of choice; however, β-lactams/β-lactamase inhibitors (BLBLIs) are regarded as an alternative mainly in patients without severe infections, with E. coli bacteremia with urinary source or with low minimum inhibitory concentrations (MICs). For infections caused by carbapenem-resistant Enterobacteriaceae (CRE), where the predicted mortality rate of patients is high, a combination antimicrobial treatment should be preferred. Many important variables in the treatment such as the role of high dosages and loading doses, the variable degrees of dosage reduction for impaired renal function, and the inclusion of carbapenems or tigecycline are a matter of debate. Despite the obscure vision provided by a notable number of meta-analyses, tigecycline is an effective and safe option for the treatment of MDR Enterobacteriaceae, as part of a combination regimen in case of infections caused by CRE, where a higher dosage (200 mg/daily) should be preferred. Colistin is the most active in vitro agent against CRE. Despite clinical data about the efficacy of fosfomycin against MDR Enterobacteriaceae are limited, this molecule represents an interesting option for the treatment of lower urinary tract and even systemic infections caused by difficult-to-treat Gram-negative pathogens. Based on in vitro studies, ceftolozane–tazobactam and ceftazidime–avibactam will represent very interesting new drugs for the treatment of ESBL-producing and CRE infections, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The report of successful treatment of life-threatening infections early in the 1940s opened the “antibiotic era.” Stimulated by a widespread use over the Second World War and by an impressive industrial effort to develop and produce antibiotics, this major progress in the history of medicine is nowadays compromised by the universal spread of antibiotic resistance which has largely escaped from hospitals to project the human being into the post-antibiotic era [1].
This review will focus on the epidemiology and treatment challenging of multi-drug resistant (MDR) Enterobacteriaceae.
Epidemiology of multi-drug resistant (MDR) Enterobacteriaceae worldwide and in Europe
Antibacterial resistance is a complex global health challenge. World Health Organization (WHO) lists third-generation cephalosporin-resistant Escherichia coli and Klebsiella pneumoniae and carbapenem-resistant K. pneumoniae in a group of seven bacteria of international concern, responsible for both healthcare-associated and community-acquired infections. Patients infected by these pathogens have limited therapeutic options, worse clinical outcomes, increased mortality rates, and a higher healthcare resources consumption. The rapid worldwide spreading of these isolates is threatening and the proportion of carbapenem-resistant strains in K. pneumoniae is reported to be up to 54 % in some regions (Tables 1 and 2) [2].
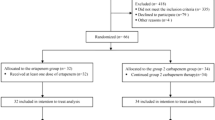
In the European Antimicrobial Resistance Surveillance Network (EARS-Net) study, a population-weighted mean percentage of third-generation cephalosporin-resistant E. coli of 11.9 % has been reported (Fig. 1); 70.5–100 % of these strains were extended-spectrum β-lactamase (ESBL) producers. The proportion of third-generation cephalosporin-resistant K. pneumoniae isolates was 25.6 %; of these, 62–100 % resulted as ESBL producers.
Proportion of third-generation cephalosporin-resistant (R+I) Escherichia coli isolates in EARS-NET participating countries in 2013. From the European Antimicrobial Resistance Surveillance Network (EARS-Net) Report 2014 (accessed July 28, 2015; http://ecdc.europa.eu/en/healthtopics/antimicrobial_resistance/database/Pages/map_reports.aspx#sthash.4qVyWAm5.dpuf).
Resistance to carbapenems remains very low (<0.1 %) in E. coli in Europe; otherwise, it is increasingly common in K. pneumoniae (0–60.5 %) (Fig. 2). Concerning, an increasing trend of combined resistance to multiple antibiotics in both E. coli and K. pneumoniae emerged in the last 4 years, mainly in three countries (Greece, Italy, and Malta) where an endemic spread of carbapenemase-producer strains was observed [3, 4].
Proportion of carbapenem-resistant (R+I) Klebsiella pneumoniae isolates in EARS-NET participating countries in 2013. From the European Antimicrobial Resistance Surveillance Network (EARS-Net) Report 2014 (accessed July 28, 2015; http://ecdc.europa.eu/en/healthtopics/antimicrobial_resistance/database/Pages/map_reports.aspx#sthash.U7TD809o.dpuf).
In USA, ESBLs and carbapenem-resistant Klebsiella spp. and E. coli cause 26,000 and 9300 hospital-acquired infections (HAI) per year, respectively, with approximately 1710 and 600 associated deaths [5]. Among pathogens causing HAI, as reported by the National Healthcare Safety Network (NHSN) in 2009–2010, up to 3.5 % of E. coli and 12.8 % of K. pneumoniae were found to be carbapenem resistant [6].
A meta-analysis describing the epidemiology of carbapenem-resistant Enterobacteriaceae (CRE) in Asia in 2000–2012 shows a very low prevalence, with average resistance rates of 1 % for meropenem with higher trend (up to 2.5 %) in Turkey and India. Klebsiella spp. accounts for the largest proportion (39.9 %) of carbapenem-resistant isolates [7].
It is difficult to know the real extent of ESBL-producing Enterobacteriaceae and CRE in Africa due to scarcity of surveillance systems and reports; anyway, available data show an increasing trend.
ESBL-producing Enterobacteriaceae have been described in South Africa, Kenya, Senegal, Cameroon, Tanzania, and Nigeria [8]. A recent study conducted in Gabon reported that 15.4 % of Enterobacteriaceae (and 49.4 % of all K. pneumoniae isolates) were ESBL producers [9]. Other available studies show a prevalence rate of ESBLs ranging from 4 % of Central African Republic [8] to 50 % of Tanzania [10, 11].
General concepts for the treatment: importance of appropriate treatment, pharmacokinetic/pharmacodynamic (PK/PD) data, susceptibility test, and combination therapy
There are a number of important issues for the reduction of mortality in patients with infections caused by MDR Enterobacteriaceae, including the underlying mechanism of resistance, the choice and timing of empiric or targeted treatment, dosing and infusion, duration of treatment, and monotherapy versus combination treatment [12]. In clinical practice, the main dilemma is the best use of carbapenems; these drugs are considered the treatment of choice for infections caused by ESBL-producing Enterobacteriaceae, but carbapenem-sparing strategies, based on the local epidemiology, must be adopted in order to avoid the threat of carbapanemase-producing Enterobacteriaceae. In addition, there are no large and robust studies on well-selected patient populations and most available data on clinical outcome come from retrospective analyses, with heterogeneity of drugs and dosages and often without any significant contribution of PK/PD data, even in the setting of severe sepsis and septic shock. Among clinical variables, the time to initiation of appropriate therapy is the strongest modifiable independent predictor for mortality in infections due to MDR Enterobacteriaceae [13, 14]; the delay with CRE may be as high as 120 ± 23 h, mainly due to current routine practices for identification in microbiology laboratories [15, 16].
Microbiological details and characterization of susceptibilities have greatly improved in the last 10 years but are still a matter of debate beyond CLSI and EUCAST breakpoints and related methodologies. Extended-spectrum β-lactamases (ESBL) hydrolyze penicillin, cephalosporins, and aztreonam with different degree of activity according to the ESBL type, thus ESBL-producing organisms may be susceptible in vitro to some of the above agents [17]. ESBL detection can be done with phenotypic tests usually used in clinical routine and genotypic tests (polymerase chain reaction, PCR), mainly used in referral centers. The phenotypic tests for ESBL detection involve testing for resistance to cefpodoxime, cefotaxime, ceftazidime, ceftriaxone, or aztreonam and a confirmatory step based on the demonstration of synergy between the above agents and clavulanic acid. Poor sensitivity of these tests may be observed when the evaluated ESBL-producing isolate additionally produces a β-lactamase not inhibited by clavulanic acid, such as an AmpC β-lactamase or a metallo-β-lactamase; methods to overcome this limitation were developed with cefepime, which is a weak substrate for most AmpC β-lactamases, chromogenic agar, cloxacillin-containing agar, or the addition of EDTA to inactivate metallo-β-lactamases [18]. These principles have been incorporated in commercial systems, but their performance in this regard is variable and their accuracy appears to be lower compared with the conventional phenotypic methods [19].
In infections caused by ESBL-producing Enterobacteriaceae, appropriate monotherapy is effective and carbapenems are the drugs of choice as evidenced by Tamma et al. that reported an increased risk of 14-day mortality in patients with bloodstream infections (BSIs) caused by ESBL-producing E. coli, Klebsiella spp., or Proteus spp. treated with empiric piperacillin–tazobactam versus carbapenems [20]. However, β-lactams/β-lactamase inhibitors (BLBLIs) are regarded as an alternative mainly in patients without severe infections, with E. coli bacteremia with urinary source or with low minimum inhibitory concentrations (MICs) [21, 22].
Therefore, data available may suggest the use of BLBLIs for BSIs caused by ESBL-producing E. coli originating from the urinary tract or with low MICs (≤2 μg/mL in the case of piperacillin–tazobactam). The choice of any β-lactam should be maximized, by a PK/PD point of view, with high dosages and by infusion strategies maximizing the time above the MIC (t > MIC); a loading dose followed by maintenance doses with extended or continuous infusion is recommended [12]. Accordingly, the use of carbapenems, either empiric or targeted, should be reserved for patients with severe infections caused by ESBL-producing bacteria with a complex resistance pattern, and de-escalation therapy from carbapenems should be always performed if feasible [23]. However, there are a number of unsolved issues especially for the use of BLBLIs which often are perceived as inferior in the treatment of infections by ESBL producers, with data not strongly supported by clinical evidence [24]. A randomized controlled trial comparing piperacillin–tazobactam versus meropenem for the definitive treatment of BSIs caused by ceftriaxone non-susceptible E. coli and Klebsiella spp. is ongoing [25].
Carbapenem resistance is frequent in K. pneumoniae and rare in E. coli and Enterobacter spp. [26]. Treatment guidelines are mostly based on expert opinions and retrospective. The majority of the authors suggest a combination treatment, often including carbapenems, for infections caused by CRE, where the predicted mortality rate of patients is high. Many important variables in the treatment such as the role of high dosages and loading doses, the variable degrees of dosage reduction for impaired renal function, and the inclusion of carbapenems or tigecycline are a matter of debate [27–29]. Evidences supporting the efficacy of various antimicrobials are more often reported with appropriate combination therapy, with multiple bias related to the retrospective collection of data, the different range of APACHE scores, and different local epidemiology and differences coming from the possible utility of meropenem (with different dosages and modality of administration), in combination regimens, when the MICs is higher than 8 mg/L. However, there is more debate than consensus on several issues with infections caused by CRE; a consensus has been proposed on issues such as early screening for gastrointestinal colonization of at-risk patients, criteria for early treatment on precocious signs of infections, combination therapy versus monotherapy, and the rationale, if any, of double-carbapenem combination such as meropenem plus ertapenem [30].
Treatment is mostly based on combination regimens, depending on local epidemiology: tigecycline, polymyxins (colistin and polymyxin B), aminoglycosides, carbapenems, fosfomycin, and rifampin are the most frequently used molecules [31, 32]. Particularly, the majority of available retrospective reports highlighted the effectiveness of appropriate combination antibiotic treatment including colistin, tigecycline gentamicin, and meropenem (Table 3) [33–35].
To obtain the maximal benefit from the limited options available, the accuracy of susceptibility testing of these drugs is a crucial issue in the microbiology laboratory. Antimicrobial susceptibilities can be tested using commercially available automated systems, including the VITEK2 (bioMérieux) and MicroScan (Siemens) systems. Problems of low accuracy versus reference broth microdilution (BMD) have been previously reported for testing of colistin and tigecycline susceptibility with KPC-K. pneumoniae and other resistant Gram negatives using automated and gradient diffusion systems, which are the most used systems for susceptibility testing [36, 37]. There are several approaches to confirmatory testing, using either molecular or non-molecular methods, and the most adopted one is the modified Hodge test which is a culture-based test to detect release of carbapenemase into agar media [38]. One caveat is that this test is designed to detect carbapenemases in general and not specifically KPC. A rapid chromogenic test (“Carba NP test”) has also been developed, and it has the same sensitivity but superior specificity in comparison with Hodge test [39]. In countries or regions where KPC-producing organisms are endemic, inhibitor-based testing using a boronic acid compound is an alternative to the aforementioned methods. Finally, molecular testing is emerging as a powerful technology with higher sensitivity but lower specificity and higher costs. On the other hand, PCR is considered to be the preferred method for definitive identification of carbapenemases in Enterobacteriaceae and PCR-based commercial test kits are now available [40].
The application of the pharmacokinetic/pharmacodynamic (PK/PD) principles has progressively gained major relevance. For carbapenems, as for other time-dependent agents, the maintenance of concentrations for about 40 % of the dosing interval above the MIC is the target for bactericidal activity, and, especially in KPC-related infections, there is the need to maintain a C trough level above the MIC for the entire dosing interval [41]. The most recent experimental and clinical data seem to support the use of carbapenems for the treatment of CRE, but with some fundamental conditions that must be met, such as low carbapenem MIC for the infecting organism (≤4 mg/L), optimal pharmacodynamic exposure to carbapenem, and combination with another active compound [35].
A combination treatment including high dosage of tigecycline may be appropriate in patients with KPC-Kp infections, also as part of a carbapenem-sparing strategy. A higher dose of tigecycline (100 mg every 12 h) is not an approved dose, and further studies would be required before this approach can be recommended. Overall, despite the in vitro activity of tigecycline against Gram-negative bacteria, its use, usually in the context of combination therapy for CRE infections, should be considered with double dosage [42].
Randomized clinical trials aimed at comparing colistin alone and colistin plus meropenem for CRE infections are ongoing in the USA and European Union (NCT01597973 and NCT01732250). Findings from these studies are expected to provide some information on the efficacy of these approaches when pharmacokinetically optimized doses are used for these agents [31].
Role of carbapenems
Carbapenems are considered the treatment of choice against serious infections caused by ESBL-producing bacteria and are usually associated with lower failure rates and better outcomes in observational studies, including efficacy of ertapenem in early-onset VAP [43–45]. Most studies evaluated imipenem or meropenem, but some experiences with ertapenem are also reported, especially as empirical therapy in community-acquired severe infections when coverage against Pseudomonas aeruginosa or Acinetobacter baumannii is not needed [46]. Some concerns are rising regarding the resistance to ertapenem in some Klebsiella and Enterobacter due to concurrent loss of porins [47, 48]. A meta-analysis found that mortality was lower in patients who received empirical or definitive therapy with carbapenem in comparison with other antibiotics, including cephalosporins, fluoroquinolones, and aminoglycosides. No statistically significant differences in mortality were found between carbapenems and β-lactam/β-lactamase inhibitor combinations (BL/BLIs) administered as definitive or empirical treatment [49]. This finding was not confirmed by a recent paper on BSIs due to several ESBL-producing Enterobacteriaceae, where patients receiving BL/BLIs had almost two times higher risk of dying compared with those who were treated empirically with carbapenems [20].
In a recent post hoc analysis of prospective cohorts of patients with ESBL-producing E. coli BSIs, empirical or definitive therapy with in vitro active BL/BLIs showed similar results to carbapenems [21]. All together, these data suggest that carbapenems should also be used empirically in patients with severe infections whereas BL/BLIs may be used in patients with urinary source of infection or when susceptibility test display low MICs [12].
The role of carbapenems in infections caused by CRE, mostly KPC-Kp, is still debated. KPC-Kp shows elevated MICs to carbapenem, with a highly variable level of resistance. Meropenem is considered effective in KPC-Kp infections when the MIC is ≤8 mg/L, with appropriate PK/PD considerations, but the issue of carbapenem MIC when deciding the possible addition to other antibiotics still needs to be defined as well as the mechanism that confers therapeutic activity to meropenem or imipenem when the MIC is well above the sensitivity breakpoint [26]. Tumbarello et al., with the limits of a retrospective study, reported that when the KPC-Kp isolate had a meropenem MIC of ≤4 mg/L, inclusion of this drug in a combination regimen was associated with a higher survival rate of (86.6 %), while when meropenem MICs was ≥16 mg/L, there was a lower survival rate (64.7 %) [35]. Similarly, Daikos et al. reported that when carbapenem MIC was ≤4 mg/L, combined therapy with a carbapenem plus one other active drug (an aminoglycoside or colistin or tigecycline) was associated with significantly lower mortality than combinations of non-carbapenem drugs with in vitro activity [50]. For strains with MIC up to 4 mg/L, prolonged infusion of high dosage of carbapenem is suggested for bactericidal effect [31].
In vitro and in vivo studies showed that dual carbapenem regimens may have enhanced efficacy over either agent alone: Ceccarelli et al. reported a successful ertapenem-doripenem combination (500 mg q24h and 250 mg q8h, respectively) treatment of a 65-year-old male patient with bacteremic ventilator-associated pneumonia due to colistin-resistant KPC-Kp [51]. The proposed rational was that ertapenem has a higher affinity to the KPC enzyme, therefore acting as a suicide substrate, thus allowing the second carbapenem to be protected from the KCP carbapenemase. However, only case reports about dual carbapenem therapy are available so far and controlled clinical data are needed to determine the efficacy of this treatment.
Some authors suggested carbapenem-sparing strategies and rotation of antibiotics in order to reduce the selective pressure on patients’ endogenous microflora. For example, Sbrana et al. evaluated the effectiveness of carbapenem sparing combination regimens for treating 26 KPC-Kp infections (ventilator acquired pneumonia = 16; bloodstream infections = 7; urinary tract infections = 2 patients; peritonitis = 1) in 22 intensive care unit (ICU) patients with relatively good health conditions, mostly polytrauma without other substantial comorbidities or immunosuppression. High-dose tigecycline was used in 25 of 26 infections as the “backbone” drug (intravenously, 100 mg every 12 h), in combination with iv gentamicin in 19 episodes or iv colistin in 12 episodes; iv fosfomycin was used as a third drug in 13 of 26 infectious episodes. In this series, a carbapenem-sparing regimen of tigecycline plus gentamicin or colistin was effective for treating 24 of 26 (92 %) KPC-Kp infectious episodes [52]. Carbapenem-sparing strategies may be safely employed and are also useful in reducing the selective pressure of carbapenems in hospital with high prevalence of ESBL-producing Gram-negative bacteria; combination regimens including high-dose tigecycline as backbone drug could be proposed as an early treatment of colonized patients with precocious signs of infection [42].
Role of tigecycline
Tigecycline is approved for the treatment of complicated skin and skin-structures infections (cSSSIs) and complicated intra-abdominal infections (cIAIs) in adults. The growing impact of infections caused by MDR Enterobacteriaceae and the current lack of alternative or new antibiotics suggest that tigecycline continues to represent a good choice in approved indications and in off-label combination regimens in routine clinical practice. According to the results of the SENTRY surveillance program (2010–2013), 88.6 % of the carbapenem-resistant Enterobacteriaceae (CRE) isolated from European medical centers are susceptible to tigecycline [53]. In the setting of infections caused by MDR pathogens, especially deep-seated infections, a major concern is represented by the correct dose of tigecycline.
For tigecycline, the pharmacokinetic/pharmacodynamic (PK/PD) measure that is most predictive of efficacy is the ratio of the area under the concentration-time curve at 24 h to the MIC (AUC0–24/MIC) [54]. Bhavnani et al. conducted a study in patients with complicated intra-abdominal infections, where Enterobacteriaceae were the most frequently isolated pathogens: multivariate logistic regression analyses identified AUC0–24/MIC ratio as being predictive of clinical response to therapy together with other variables. For tigecycline AUC0–24/MIC values ≥3.1, a positive clinical response was reported in 89 % of patients; with lower values, only 50 % of patients experienced a successful clinical response (OR, 33.0; p = 0.003) [55].
About concerning results reported in tigecycline phase 3 and 4 comparative clinical trials, Bassetti et al. recently investigated clinical failure and mortality in cSSSIs and cIAIs trials: using descriptive analyses of a blinded adjudication of mortality and multivariate regression analyses, tigecycline did not appear to be a factor either for failure (cSSSI and cIAI studies) or for death (cIAI studies) [56].
Data from studies showing a good penetration in lung and in the epithelial lining fluid (ELF) suggest that tigecycline may represent a suitable option in the treatment of patients with hospital-acquired pneumonia (HAP), where MDR Enterobacteriaceae play a major role [57, 58]. Anyway, in this setting, the adequate dose continues to represent a matter of debate among clinicians. In a phase 3 study involving patients with HAP, tigecycline administered at the dose used in the approved amounts (100 mg as a loading dose followed by 50 mg every 12 h) did not achieve the pre-established efficacy endpoints compared to imipenem–cilastatin [59]. Assuming that a higher AUC0–24/MIC ratio was necessary in patients with HAP, Ramirez et al. conducted a phase 2 study comparing the safety and efficacy of two higher doses of tigecycline (150 mg followed by 75 mg every 12 h or 200 mg followed by 100 mg every 12 h) with imipenem–cilastatin. In the clinically evaluable population, clinical cure with tigecycline 100 mg (17/20, 85.0 %) was numerically higher than with tigecycline 75 mg (16/23, 69.6 %) and imipenem–cilastatin (18/24, 75.0 %). No new safety signals were identified [60].
In our opinion, despite the obscure vision provided by a notable number of meta-analyses, tigecycline is effective and safe in the treatment of MDR Enterobacteriaceae, as part of a combination regimen in case of infections caused by CRE. In this setting, we support the use of higher doses (200 mg as a loading dose followed by 100 mg every 12 h) in order to achieve an adequate AUC0–24/MIC ratio.
Role of aminoglycosides
The activity of aminoglycosides against ESBL-producing pathogens is diverse according to geographical areas. Overall, amikacin is usually the most frequently active drug among these compounds, and it can be used in combination with other drugs for urinary tract sepsis, in selected patients, to avoid the use of carbapenems [22, 61]. Kim and colleagues reported 15 cases of bacteremia due to ESBL-producing K. pneumoniae and E. coli treated with active aminoglycosides in monotherapy with a 50 % positive clinical response [62].
From a PK/PD point of view, aminoglycosides are concentration-dependent antibiotics; there are preliminary data in 146 critically ill patients from a prospective observational monocentric study showing that even with a very high daily dosage (25 mg/kg once daily of amikacin), up to two thirds of patients may not reach target plasma levels for efficacy [63]. Among independent determinants of C max <60 mg/L, there was a positive 24-h fluid balance (OR per 250-mL increment 1.06, 95 % [CI 1.01–1.11], p = 0.018) which should always be taken into account when caring patients with septic shock.
Gentamicin plays an important role in the treatment of KPC-Kp in combination therapy usually with carbapenem or tigecycline. Concerns are raised about the use of aminoglycosides with colistin due to the high risk of nephrotoxicity. In a recent observational, retrospective cohort study, the use of targeted treatment with gentamicin was associated with lower mortality compared with the use of targeted treatment without gentamicin (20.7 vs. 61.9 %, p = 0.02). Mortality was significantly reduced when the strain was susceptible to gentamicin (7.7 vs. 80.0 %, p = 0.008) and lower when the strain showed intermediate susceptibility (31.2 vs. 53.3 %, p = 0.133). Mortality in the group of patients with optimal targeted treatment containing gentamicin was 20.7 %, compared with 37.5 % of patients with optimal targeted treatment without gentamicin (p = 0.21). The survival analysis performed using Kaplan–Meier curves showed that patients treated with gentamicin had higher survival rates at 30 days after diagnosis (p = 0.001) [64].
Aminoglycoside resistance among Enterobacteriaceae is mediated by multiple mechanisms, including impaired membrane permeability, efflux mechanisms, ribosomal alterations, or expression of aminoglycoside-modifying enzymes (AMEs), but gentamicin seems to be more effective on the KPC-Kp clone ST258 and a concentration of 10 mg/L has been shown to be bactericidal against gentamicin-susceptible strains [65–68].
Oral gentamicin has been used for the selective gut decontamination from KPC-Kp, which could be an important approach to reduce the risk of spreading severe infection in colonized patients. Oral gentamicin may be an ideal agent for gut decontamination due to the fact that oral formulation is virtually non-absorbable, without systemic activity and toxicity, and has a limited spectrum and no activity against anaerobes, being less disruptive to the gastrointestinal flora. So far, data are discordant about the successful eradication rate, which ranges from 42 to 68 %, and the risk of selection of KPC-Kp gentamicin-resistant strains [69–72]. A higher eradication rate was reported in patients who received selective decontamination without concomitant antibiotic therapies [73]. In contrast, aminoglycosides are not considered as an option for NDM-producing Enterobacteriaceae because the majority of the isolates produce 16S ribosomal RNA methyltransferase, which renders them completely resistant to aminoglycosides [74].
Role of colistin
In the management of CRE infections, association of at least two active compounds has been advocated to increased survival rates, prevent emergence of reduced susceptibility, and achieve bacterial synergy [34, 35]. The therapeutic armamentarium is often limited to antibiotics with high potential toxicity, such as colistin, a molecule which plays a major role in combination regimens. Colistin is considered to be the most active in vitro agent against CRE [75]. Anyway, its utility is still limited by an overall lack of understanding on how to optimally administer the agent; furthermore, nephrotoxicity remains a concerning adverse effect of colistin, especially when used at high doses. A recent review suggests that risk factors of colistin nephrotoxicity can be categorized as dose and duration of colistin therapy, co-administration of other nephrotoxic drugs, and patient-related factors such as age, sex, hypoalbuminemia, hyperbilirubinemia, underlying disease, and severity of patient illness [76].
Emergence of resistance to colistin represents a major public health concern in many different regions as USA, Canada, South America, Europe, and China. A laboratory surveillance program conducted in Canada from 2010 to 2012 revealed that 31 % of the isolates were resistant to colistin [77].
A large survey from the northeast of Italy showed that a statistically significant increase in the proportion of colistin-resistant strains occurred in 2013 (25.6 %) and in 2014 (22 %) with respect to 2012 (10.7 %) [78]. In a study conducted in Sicily (Italy), colistin non-susceptibility was found in 42 % of isolates [79]. In another recent Italian paper, 36.1 % of carbapenem-resistant K. pneumoniae strains were shown to be resistant to colistin and resistance to colistin resulted as an independent risk factor for mortality at the multivariate analysis adjusted for appropriate treatment, combination therapy, and infectious-source removal. The unexpected high rate of resistance among isolates was supposed to be due to the increased use of this drug during recent years, especially as monotherapy, but data on colistin use previously the study period were not available [80]. These results were confirmed by another paper in which colistin resistance was identified as an independent predictor of 14-day mortality; furthermore, in this study combination therapy with at least two drugs displaying in vitro activity against the isolate was associated with lower mortality [81].
The optimal regimen for the treatment of colistin-resistant strains is unknown. In an Italian study, the combination of colistin plus rifampicin showed synergistic antimicrobial activity against 13 KPC-producing K. pneumoniae colistin-resistant strains isolated from different pathological samples [32]. Based on this study, another Italian group investigated the synergistic activity and post-antibiotic effect (PAE) of colistin in combination with other antimicrobial agents against colistin-susceptible and colistin-resistant KPC-producing K. pneumoniae strains isolated from bloodstream. The authors observed a synergistic in vitro activity for colistin–rifampicin combinations in all colistin-resistant strains. Time-kill kinetic analysis confirmed synergy and persistent growth inhibition of colistin-resistant strains exposed to colistin–rifampicin combination. The PAE activity of colistin–rifampicin combination was further prolonged by tigecycline [82]. The combination of rifampicin with other antimicrobials, namely tigecycline or meropenem, showed no synergistic activity, supporting that it is the ability of colistin to disrupt the bacterial membrane integrity that allows the access and accumulation of rifampicin.
In the setting of the treatment of CRE, we suggest to include colistin in combination regimens at high doses (9 million units, MU, as a loading dose, followed by 4.5 MU mg every 12 h in a patient with normal renal function; renal dose adjustments are necessary). We strongly recommend close monitoring of the renal function, especially if other nephrotoxic drugs are co-administered. If non-susceptibility to colistin is documented, colistin may be continued and adding of rifampicin should be considered in order to exploit synergism.
Role of fosfomycin
Despite clinical data about the efficacy of fosfomycin against MDR Enterobacteriaceae that are limited, this molecule has attracted renewed interest for the treatment of lower urinary tract and even systemic infections caused by difficult-to-treat Gram-negative pathogens. While oral fosfomycin is available worldwide, an intravenous formulation (fosfomycin disodium) is available in many countries in Europe but not in the USA.
Activity of fosfomycin has been tested in many in vitro studies. In the study by Falagas et al., susceptibility to fosfomycin of the 79 carbapenemase-producing, 34 extended-spectrum β-lactamase-producing, and 24 metallo-β-lactamase-producing isolates was 94.9, 94.1, and 83.3 %, respectively [83]. A recent study has demonstrated that fosfomycin is highly active against Serratia marcescens and Klebsiella pneumoniae resistant to carbapenems harboring blaKPC-2 [84]. Susceptibility of New Delhi metallo-β-lactamase (NDM)-1-producing Enterobacteriaceae to fosfomycin has been reported in a study conducted in Pakistan [85].
Oral fosfomycin (trometamol salt) remains a valuable option in the treatment of uncomplicated urinary tract infections. In a large surveillance from Germany involving 499 Escherichia coli isolated from urine samples, resistance to fosfomycin was shown in six strains only and all but one ESBL-producing strains were fosfomycin susceptible [86]. The well-known ability of fosfomycin to achieve high urinary concentrations has been exploited in some clinical cases which demonstrated the success of oral fosfomycin in the treatment of urinary tract infections caused by KPC- and NDM-producing Enterobacteriaceae [87, 88].
In a small study involving 11 critically ill patients with nosocomial infections caused by KPC-producing K. pneumoniae, intravenous fosfomycin (2–4 g q6h) was administered in combination with colistin, gentamicin, or piperacillin–tazobactam; treatment-related microbiological and clinical outcome was good for all patients while the all-cause hospital mortality was 18.2 % (two patients) [89].
There is a great concern about the use of fosfomycin as a monotherapy because resistance can develop easily. Furthermore, the emergence of resistance has been described even when fosfomycin was used as an adjunct in combination therapy in three cases of KPC-producing K. pneumoniae bacteremia [90].
We strongly suggest to consider the use of intravenous fosfomycin as part of a combination regimen for the treatment of MDR Enterobacteriaceae, especially in complicated urinary tract infections and sepsis. The drug should be usually administered at the dose of 4 g every 6 h, but recent data demonstrated that higher doses, up to 24 g/day, are needed to prevent the emergence of bacterial resistance [91].
New antibiotics
Novel antimicrobials that could provide clinical efficacy towards MDR Gram-negative pathogens, including ESBL and carbapenemase producers, are urgently needed.
The Food and Drug Administration recently approved two novel combination antibiotics, ceftolozane–tazobactam and ceftazidime–avibactam. Both of these combination agents have shown in vitro activity against selected resistant Gram-negative pathogens, including Enterobacteriaceae and Pseudomonas aeruginosa; notably, ceftazidime–avibactam has demonstrated consistent activity against K. pneumoniae carbapenemase (KPC)-producing organisms [92]. Ceftolozane is a new antipseudomonal cephalosporin which has been combined with tazobactam, a well-established β-lactamase inhibitor. Spectrum of activity of ceftolozane–tazobactam includes difficult-to-treat Gram-negative pathogens, including ESBL strains. In vitro studies have demonstrated that ceftozolane has superior activity against resistant strains of Enterobacteriaceae compared to piperacillin–tazobactam and ceftazidime [93, 94].
A phase 3 clinical trial has shown that ceftolozane–tazobactam (1.5 g every 8 h) is noninferior to levofloxacin (750 mg once daily) for the treatment of complicated urinary tract infections (cUTI); adverse events had similar incidence in the two treatment groups and were mainly non-serious [95]. Similarly, in patients with complicated intra-abdominal infections (cIAI), treatment with ceftolozane–tazobactam, administered with metronidazole, was noninferior to meropenem in clinical cure rates at the test-of-cure visit [96].
A phase 3 clinical trial to evaluate the safety and efficacy of ceftolozane–tazobactam for the treatment of nosocomial pneumonia is ongoing. Considering a plasma-to-epithelial lining fluid (ELF) penetration ratio of approximately 50 %, a doubling of the current dose regimen (i.e., 3 g every 8 h in a patient with normal renal function) is needed to achieve >90 % probability of target attainment for nosocomial pneumonia [97].
Avibactam is a novel β-lactamase inhibitor with a broad spectrum of activity, covering class A, class C, and some class D enzymes. Notably, the activity of avibactam also includes carbapenemases such as the KPC and OXA-48, but not metallo-β-lactamases [98]. The combination of avibactam with the cephalosporin ceftazidime is attractive, given the spectrum of activity and the low toxicity of the cephalosporin class. Two phase 2 trials have shown that efficacy and safety of ceftazidime–avibactam were similar to comparator drugs for the treatment of cUTI and cIAI [99, 100]. Phase 3 trials evaluating ceftazidime–avibactam for the treatment of cIAI and cUTI have been recently completed, and results will likely be available in late 2015. Interestingly, preliminary data show that clinical cure rates for ceftazidime–avibactam were lower for patients with a creatinine clearance between 30 and 50 mL/min [101].
An overview of emerging treatment options for MDR Enterobacteriaceae can be found in Table 4.
Infection control measures
Bundled interventions are required to control CRE transmission. Hand hygiene and standard precautions remain the keys of the prevention strategies, as highlighted by ESCMID and CDC guidelines [102, 103]. The use of appropriate infection prevention practices can minimize the risk of spread of CRE infection and colonization. Some factors have been associated with higher risk for colonization, such as intensive care unit stay, being transferred to other facilities, and prolonged hospitalization [104, 105]. The strategy to prevent the spread of KPC-Kp includes different key elements: one of the primary is to act pro-actively and survey those at risk of being colonized or infected. Patients at high risk, such as those previously colonized or infected with KPC-Kp, recently treated at endemic institutions should be subject to screening and isolated until culture results are available, for active surveillance purposes. Asymptomatic carriers, colonized with KPC-Kp, constitute a reservoir for transmission, and most of the papers describing successful infection control measures during outbreaks included an early identification and isolation of infected patients [106]. Schwaber et al. reported a nationwide intervention implemented in 2007 by the Israel Ministry of Health, based on ward-based mandatory guidelines for carrier isolation, patient and staff cohorting, active surveillance, and other interventions including rules for microbiology identification, direct site visits at healthcare facilities, and communications networking. There was a decline of the nosocomial CRE acquisition from a monthly rate of 55.5 to an annual low of 4.8 cases per 100,000 patient-days (p < 0.001) [107]. On the basis of several guidelines, rectal swab is the most common way to detect colonization, although no systematic comparative studies are performed so far to identify the most effective system to screen for KPC organism [108].
For CRE, the use of contact precaution is recommended and both contact isolation and cohorting have been shown to limit the number of secondary cases and control outbreaks in different settings. Moreover, several studies have reported cohorting nursing staff as an effective measure to prevent cross-transmission [109, 110].
The duration of isolation for colonized patients is unknown. The mean duration of excretion of CRE associated with gastrointestinal colonization varies significantly between 9.8 and 19 days, and depends on the carbapenemase enzyme isolated in Enterobacteriaceae. One study found a median carriage time of 3 months [111], but prolonged excretion for up to 1 year has been documented [70, 112]. Several factors are associated with persistent carriage: fluoroquinolone use, intra-facility transfer, and re-admission within 3 months of a culture growing CRE. So far data are discordant regarding the persistence of positive screening, thus many recommend that isolation be maintained until hospital discharge [113].
Other infection prevention strategies have also been used in different outbreaks to control the spread of CRE, such as decolonization of patients by the use of daily chlorhexidine bathing as part of a bundled intervention plan to control an outbreak of KPC-producing Klebsiella species in a long-term-care facility; this approach was found to be successful [114]. Contamination of the environment has been suspected in different outbreaks, and these have led to the recommendation of frequent cleaning of environmental surfaces [115, 116]. Passaretti et al. demonstrated a reduction in the acquisition of MDR Gram-negative bacteria with vaporized hydrogen peroxide decontamination of environment [117].
These studies showed that multiple interventions should be employed to successfully control CRE epidemics, also including simultaneous interventions in different hospitals and antimicrobial stewardship policies which may be useful for other so-called enteropathogenetic syndromes such as infections caused by Clostridium difficile and Candida spp. [118].
Conclusions
Current clinical practice relating to Enterobacteriaceae infections has been extremely challenged by the emergence of multidrug resistance. Treatment options seem to be more optimistic for Gram-positive pathogens (including C. difficile), for which the pipeline is more promising. In the field of Gram-negative MDR infections, there is a great concern about the therapeutic future, as only a handful of the upcoming agents will address the unmet medical needs.
Currently, the most effective approach is the PK/PD optimization of the available antibiotics, particularly given the increasing awareness of the pharmacokinetic alterations that occur in the critically ill patient. Combination treatments seem to be important, at least in the empirical phase of treatment, to ensure adequate coverage of the patient and improve clinical outcome. However, randomized clinical trials are urgently needed to define the possible benefit from combinations in various settings. Most importantly, infection control measures and prompt diagnostics are the cornerstones to prevent further transmission of MDR pathogens in healthcare settings and to optimize early antimicrobial treatment.
References and Recommended Reading
Bassetti M, De Waele JJ, Eggimann P, Garnacho-Montero J, Kahlmeter G, Menichetti F, et al. Preventive and therapeutic strategies in critically ill patients with highly resistant bacteria. Intensive Care Med. 2015;41(5):776–95.
WHO. Antimicrobial Resistance Global Report on surveillance WHO; 2014. http://www.who.int/drugresistance/documents/surveillancereport/en/. Accessed 28 July 2015.
European Centre for Disease Prevention and Control. Annual epidemiological report 2014. Antimicrobial resistance and healthcare-associated infections. Stockholm: ECDC; 2015.
European Centre for Disease Prevention and Control. Carbapenemase-producing bacteria in Europe: interim results from the European Survey on carbapenemase-producing Enterobacteriaceae (EuSCAPE) project. Stockholm: ECDC; 2013.
Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013/index.html. Accessed 28 July 2015.
Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009–2010. Infect Control Hosp Epidemiol. 2013;34(1):1–14.
Xu Y, Gu B, Huang M, Liu H, Xu T, Xia W, et al. Epidemiology of carbapenem resistant Enterobacteriaceae (CRE) during 2000–2012 in Asia. J Thorac Dis. 2015;7(3):376–85.
Frank T, Arlet G, Gautier V, Talarmin A, Bercion R. Extended-spectrum β-lactamase–producing Enterobacteriaceae, Central African Republic. Emerg Infect Dis, www.cdc.gov/eid. 2006;12(5).
Alabi AS, Frielinghaus L, Kaba H, Kösters K, Huson MA, Kahl BC, et al. Retrospective analysis of antimicrobial resistance and bacterial spectrum of infection in Gabon, Central Africa. BMC Infect Dis. 2013;13:455.
Mshana S, Kamugisha E, Mirambo M, Chakraborty T, Lyamuya E. Prevalence of multiresistant gram-negative organisms in a tertiary hospital in Mwanza, Tanzania. BMC Res Notes. 2009;2:49.
Eshetie S, Unakal C, Gelaw A, Ayelign B, Endris M, Moges F. Multidrug resistant and carbapenemase producing Enterobacteriaceae among patients with urinary tract infection at referral Hospital, Northwest Ethiopia. Antimicrob Resist Infect Control. 2015;4:12.
Viale P, Giannella M, Tedeschi S, Lewis R. Treatment of MDR-Gram negative infections in the 21st century: a never ending threat for clinicians. Curr Opin Pharmacol. 2015;24:30–7.
Leibman V, Martin ET, Tal-Jasper R, Grin L, Hayakawa K, Shefler C, et al. Simple bedside score to optimize the time and the decision to initiate appropriate therapy for carbapenem-resistant Enterobacteriaceae. Ann Clin Microbiol Antimicrob. 2015;14:31.
Paul M, Shani V, Muchtar E, Kariv G, Robenshtok E, Leibovici L. Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother. 2010;54:4851–63.
Ku K, Moshos J, Bheemreddy S, Wang Y, Bhargava A, Campbell M, et al. Colistin versus tigecycline for the treatment of Acinetobacter baumannii and/or carbapenem resistant Enterobacteriaceae infections. Society for Healthcare Epidemiology of America (SHEA) 21st annual meeting, Dallas, TX, USA; 2011.
Schwaber MJ, Carmeli Y. Carbapenem-resistant Enterobacteriaceae: a potential threat. JAMA. 2008;300:2911–3.
Falagas ME, Karageorgopoulos DE. Extended-spectrum beta-lactamase-producing organisms. J Hosp Infect. 2009;73(4):345–54.
Drieux L, Brossier F, Sougakoff W, Jarlier V. Phenotypic detection of extended-spectrum beta-lactamase production in Enterobacteriaceae: review and bench guide. Clin Microbiol Infect. 2008;14 Suppl 1:90–103.
Wiegand I, Geiss HK, Mack D, Stürenburg E, Seifert H. Detection of extended-spectrum beta-lactamases among Enterobacteriaceae by use of semiautomated microbiology systems and manual detection procedures. J Clin Microbiol. 2007;45(4):1167–74.
Tamma PD, Han JH, Rock C, Harris AD, Lautenbach E, Hsu AJ, et al. Carbapenem therapy is associated with improved survival compared with piperacillin–tazobactam for patients with extended-spectrum beta-lactamase bacteremia. Clin Infect Dis. 2015;60(9):1319–25.
Rodríguez-Baño J, Navarro MD, Retamar P, Picón E, Pascual Á. β-Lactam/β-lactam inhibitor combinations for the treatment of bacteremia due to extended-spectrum β-lactamase-producing Escherichia coli: a post hoc analysis of prospective cohorts. Clin Infect Dis. 2012;54(2):167–74.
Delgado-Valverde M, Sojo-Dorado J, Pascual A, Rodríguez-Baño J. Clinical management of infections caused by multidrug-resistant Enterobacteriaceae. Ther Adv Infect Dis. 2013;1(2):49–69.
Lew KY, Ng TM, Tan M, Tan SH, Lew EL, Ling LM, et al. Safety and clinical outcomes of carbapenem de-escalation as part of an antimicrobial stewardship programme in an ESBL-endemic setting. J Antimicrob Chemother. 2015;70(4):1219–25.
Harris PN, Tambyah PA, Paterson DL. β-Lactam and β-lactamase inhibitor combinations in the treatment of extended-spectrum β-lactamase producing Enterobacteriaceae: time for a reappraisal in the era of few antibiotic options? Lancet Infect Dis. 2015;15(4):475–85.
Harris PN, Peleg AY, Iredell J, Ingram PR, Miyakis S, Stewardson AJ, et al. Meropenem versus piperacillin–tazobactam for definitive treatment of bloodstream infections due to ceftriaxone non-susceptible Escherichia coli and Klebsiella spp (the MERINO trial): study protocol for a randomised controlled trial. Trials. 2015;16:24.
Lee CS, Doi Y. Therapy of infections due to carbapenem-resistant gram-negative pathogens. Infect Chemother. 2014;46(3):149–64.
Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13(9):785–96.
Hirsch EB, Tam VH. Detection and treatment options for Klebsiella pneumoniae carbapenemases (KPCs): an emerging cause of multidrug-resistant infection. J Antimicrob Chemother. 2010;65(6):1119–25.
Borer A, Saidel-Odes L, Riesenberg K, Eskira S, Peled N, Nativ R, et al. Attributable mortality rate for carbapenem-resistant Klebsiella pneumoniae bacteremia. Infect Control Hosp Epidemiol. 2009;30(10):972–6.
De Rosa FG, Corcione S, Cavallo R, Di Perri G, Bassetti M. Critical issues for Klebsiella pneumoniae KPC-carbapenemase producing K. pneumoniae infections: a critical agenda. Future Microbiol. 2015;10(2):283–94.
Doi Y, Paterson DL. Carbapenemase-producing Enterobacteriaceae. Semin Respir Crit Care Med. 2015;36(1):74–84.
Tascini C, Tagliaferri E, Giani T, Leonildi A, Flammini S, Casini B, et al. Synergistic activity of colistin plus rifampin against colistin-resistant KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2013;57(8):3990–3.
Qureshi ZA, Paterson DL, Potoski BA, Kilayko MC, Sandovsky G, Sordillo E, et al. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob Agents Chemother. 2012;56(4):2108–13.
Zarkotou O, Pournaras S, Tselioti P, Dragoumanos V, Pitiriga V, Ranellou K, et al. Predictors of mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae and impact of appropriate antimicrobial treatment. Clin Microbiol Infect. 2011;17(12):1798–803.
Tumbarello M, Viale P, Viscoli C, Trecarichi EM, Tumietto F, Marchese A, et al. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis. 2012;55(7):943–50.
Lat A, Clock SA, Wu F, Whittier S, Della-Latta P, Fauntleroy K, et al. Comparison of polymyxin B, tigecycline, cefepime, and meropenem MICs for KPC-producing Klebsiella pneumoniae by broth microdilution, Vitek 2, and Etest. J Clin Microbiol. 2011;49(5):1795–8.
Tan TY, Ng SY. Comparison of Etest, Vitek and agar dilution for susceptibility testing of colistin. Clin Microbiol Infect. 2007;13(5):541–4.
Anderson KF, Lonsway DR, Rasheed JK, Biddle J, Jensen B, McDougal LK, et al. Evaluation of methods to identify the Klebsiella pneumoniae carbapenemase in Enterobacteriaceae. J Clin Microbiol. 2007;45(8):2723–5.
Nordmann P, Poirel L, Dortet L. Rapid detection of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 2012;18(9):1503–7.
Cuzon G, Naas T, Bogaerts P, Glupczynski Y, Nordmann P. Evaluation of a DNA microarray for the rapid detection of extended-spectrum β-lactamases (TEM, SHV and CTX-M), plasmid-mediated cephalosporinases (CMY-2-like, DHA, FOX, ACC-1, ACT/MIR and CMY-1-like/MOX) and carbapenemases (KPC, OXA-48, VIM, IMP and NDM). J Antimicrob Chemother. 2012;67(8):1865–9.
Pea F, Viale P, Cojutti P, Furlanut M. Dosing nomograms for attaining optimum concentrations of meropenem by continuous infusion in critically ill patients with severe gram-negative infections: a pharmacokinetics/pharmacodynamics-based approach. Antimicrob Agents Chemother. 2012;56(12):6343–8.
De Rosa FG, Corcione S, Di Perri G, Scaglione F. Re-defining tigecycline therapy. New Microbiol. 2015;38(2):121–36.
Endimiani A, Luzzaro F, Perilli M, Lombardi G, Colì A, Tamborini A, et al. Bacteremia due to Klebsiella pneumoniae isolates producing the TEM-52 extended-spectrum beta-lactamase: treatment outcome of patients receiving imipenem or ciprofloxacin. Clin Infect Dis. 2004;38(2):243–51.
Bassetti M, Righi E, Fasce R, Molinari MP, Rosso R, Di Biagio A, et al. Efficacy of ertapenem in the treatment of early ventilator-associated pneumonia caused by extended-spectrum beta-lactamase-producing organisms in an intensive care unit. J Antimicrob Chemother. 2007;60(2):433–5.
De Rosa FG, Pagani N, Fossati L, Raviolo S, Cometto C, Cavallerio P, et al. The effect of inappropriate therapy on bacteremia by ESBL-producing bacteria. Infection. 2011;39(6):555–61.
Collins VL, Marchaim D, Pogue JM, Moshos J, Bheemreddy S, Sunkara B, et al. Efficacy of ertapenem for treatment of bloodstream infections caused by extended-spectrum-β-lactamase-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2012;56(4):2173–7.
Pitout JD. Infections with extended-spectrum beta-lactamase-producing Enterobacteriaceae: changing epidemiology and drug treatment choices. Drugs. 2010;70(3):313–33.
Elliott E, Brink AJ, van Greune J, Els Z, Woodford N, Turton J, et al. In vivo development of ertapenem resistance in a patient with pneumonia caused by Klebsiella pneumoniae with an extended-spectrum beta-lactamase. Clin Infect Dis. 2006;42(11):e95–8.
Vardakas KZ, Tansarli GS, Rafailidis PI, Falagas ME. Carbapenems versus alternative antibiotics for the treatment of bacteraemia due to Enterobacteriaceae producing extended-spectrum β-lactamases: a systematic review and meta-analysis. J Antimicrob Chemother. 2012;67(12):2793–803.
Daikos GL, Tsaousi S, Tzouvelekis LS, Anyfantis I, Psichogiou M, Argyropoulou A, et al. Carbapenemase-producing Klebsiella pneumoniae bloodstream infections: lowering mortality by antibiotic combination schemes and the role of carbapenems. Antimicrob Agents Chemother. 2014;58(4):2322–8.
Ceccarelli G, Falcone M, Giordano A, Mezzatesta ML, Caio C, Stefani S, et al. Successful ertapenem-doripenem combination treatment of bacteremic ventilator-associated pneumonia due to colistin-resistant KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2013;57(6):2900–1.
Sbrana F, Malacarne P, Viaggi B, Costanzo S, Leonetti P, Leonildi A, et al. Carbapenem-sparing antibiotic regimens for infections caused by Klebsiella pneumonia carbapenemase-producing K. pneumoniae in intensive care unit. Clin Infect Dis. 2013;56(5):697–700.
Sader HS, Castanheira M, Flamm RK, Mendes RE, Farrell DJ, Jones RN. Tigecycline activity tested against carbapenem-resistant Enterobacteriaceae from 18 European nations: results from the SENTRY surveillance program (2010–2013). Diagn Microbiol Infect Dis. 2015. doi:10.1016/j.diagmicrobio.2015.06.011.
Ambrose PG, Bhavnani SM, Rubino CM, Louie A, Gumbo T, Forrest A, et al. Pharmacokinetics-pharmacodynamics of antimicrobial therapy: it’s not just for mice anymore. Clin Infect Dis. 2007;44(1):79–86.
Bhavnani SM, Rubino CM, Ambrose PG, et al. Pharmacokinetic-pharmacodynamic analyses of efficacy using estimates of serum and effect site tigecycline exposures in patients with complicated intra-abdominal infections [abstract O-361]. In: Program and abstracts of the 16th European Congress of Clinical Microbiology and Infectious Diseases (Nice, France). Basel, Switzerland: European Society of Clinical Microbiology and Infectious Diseases, 2006:88.
Bassetti M, McGovern PC, Wenisch C, Meyer RD, Yan JL, Wible M, et al. Clinical response and mortality in tigecycline complicated intra-abdominal infection and complicated skin and soft-tissue infection trials. Int J Antimicrob Agents. 2015;46(3):346–50.
Rodvold KA, Gotfried MH, Cwik M, Korth-Bradley JM, Dukart G, Ellis-Grosse EJ. Serum, tissue and body fluid concentrations of tigecycline after a single 100mg dose. J Antimicrob Chemother. 2006;58(6):1221–9.
Conte Jr JE, Golden JA, Kelly MG, Zurlinden E. Steady-state serum and intrapulmonary pharmacokinetics and pharmacodynamics of tigecycline. Int J Antimicrob Agents. 2005;25(6):523–9.
Freire AT, Melnyk V, Kim MJ, Datsenko O, Dzyublik O, Glumcher F, et al. Comparison of tigecycline with imipenem/cilastatin for the treatment of hospital-acquired pneumonia. Diagn Microbiol Infect Dis. 2010;68(2):140–51.
Ramirez J, Dartois N, Gandjini H, Yan JL, Korth-Bradley J, McGovern PC. Randomized phase 2 trial to evaluate the clinical efficacy of two high-dosage tigecycline regimens versus imipenem-cilastatin for treatment of hospital-acquired pneumonia. Antimicrob Agents Chemother. 2013;57(4):1756–62.
Pitout JD, Le P, Church DL, Gregson DB, Laupland KB. Antimicrobial susceptibility of well-characterised multiresistant CTX-M-producing Escherichia coli: failure of automated systems to detect resistance to piperacillin/tazobactam. Int J Antimicrob Agents. 2008;32(4):333–8.
Kim YK, Pai H, Lee HJ, Park SE, Choi EH, Kim J, et al. Bloodstream infections by extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in children: epidemiology and clinical outcome. Antimicrob Agents Chemother. 2002;46(5):1481–91.
de Montmollin E, Bouadma L, Gault N, Mourvillier B, Mariotte E, Chemam S, et al. Predictors of insufficient amikacin peak concentration in critically ill patients receiving a 25 mg/kg total body weight regimen. Intensive Care Med. 2014;40(7):998–1005.
Gonzalez-Padilla M, Torre-Cisneros J, Rivera-Espinar F, Pontes-Moreno A, López-Cerero L, Pascual A, et al. Gentamicin therapy for sepsis due to carbapenem-resistant and colistin-resistant Klebsiella pneumoniae. J Antimicrob Chemother. 2015;70(3):905–13.
The most frequently occurring aminoglycoside resistance mechanisms—combined results of surveys in eight regions of the world. J Chemother. 1995;7 Suppl 2:17–30.
Naparstek L, Carmeli Y, Navon-Venezia S, Banin E. Biofilm formation and susceptibility to gentamicin and colistin of extremely drug-resistant KPC-producing Klebsiella pneumoniae. J Antimicrob Chemother. 2014;69(4):1027–34.
Clancy CJ, Hao B, Shields RK, Chen L, Perlin DS, Kreiswirth BN, et al. Doripenem, gentamicin, and colistin, alone and in combinations, against gentamicin-susceptible, KPC-producing Klebsiella pneumoniae strains with various ompK36 genotypes. Antimicrob Agents Chemother. 2014;58(6):3521–5.
Michail G, Labrou M, Pitiriga V, Manousaka S, Sakellaridis N, Tsakris A, et al. Activity of tigecycline in combination with colistin, meropenem, rifampin, or gentamicin against KPC-producing Enterobacteriaceae in a murine thigh infection model. Antimicrob Agents Chemother. 2013;57(12):6028–33.
Oren I, Sprecher H, Finkelstein R, Hadad S, Neuberger A, Hussein K, et al. Eradication of carbapenem-resistant Enterobacteriaceae gastrointestinal colonization with nonabsorbable oral antibiotic treatment: a prospective controlled trial. Am J Infect Control. 2013;41(12):1167–72.
Saidel-Odes L, Polachek H, Peled N, Riesenberg K, Schlaeffer F, Trabels Y, et al. A randomized, double-blind, placebo-controlled trial of selective digestive decontamination using oral gentamicin and oral polymyxin E for eradication of carbapenem-resistant Klebsiella pneumoniae carriage. Infect Control Hosp Epidemiol. 2012;33(1):14–9.
Lübbert C, Faucheux S, Becker-Rux D, Laudi S, Dürrbeck A, Busch T, et al. Rapid emergence of secondary resistance to gentamicin and colistin following selective digestive decontamination in patients with KPC-2-producing Klebsiella pneumoniae: a single-centre experience. Int J Antimicrob Agents. 2013;42(6):565–70.
Zuckerman T, Benyamini N, Sprecher H, Fineman R, Finkelstein R, Rowe JM, et al. SCT in patients with carbapenem resistant Klebsiella pneumoniae: a single center experience with oral gentamicin for the eradication of carrier state. Bone Marrow Transplant. 2011;46(9):1226–30.
Tascini C, Sbrana F, Flammini S, Tagliaferri E, Arena F, Leonildi A, et al. Oral gentamicin gut decontamination for prevention of KPC-producing Klebsiella pneumoniae infections: relevance of concomitant systemic antibiotic therapy. Antimicrob Agents Chemother. 2014;58(4):1972–6.
Livermore DM, Mushtaq S, Warner M, Zhang JC, Maharjan S, Doumith M, et al. Activity of aminoglycosides, including ACHN-490, against carbapenem-resistant Enterobacteriaceae isolates. J Antimicrob Chemother. 2011;66(1):48–53.
Gales AC, Jones RN, Sader HS. Contemporary activity of colistin and polymyxin B against a worldwide collection of Gram-negative pathogens: results from the SENTRY Antimicrobial Surveillance Program (2006–09). J Antimicrob Chemother. 2011;66(9):2070–4.
Ordooei Javan A, Shokouhi S, Sahraei Z. A review on colistin nephrotoxicity. Eur J Clin Pharmacol. 2015;71(7):801–10.
Lefebvre B, Lévesque S, Bourgault AM, Mulvey MR, Mataseje L, Boyd D, et al. Carbapenem non-susceptible enterobacteriaceae in Quebec, Canada: results of a laboratory surveillance program (2010–2012). PLoS One. 2015;10(4), e0125076. doi:10.1371/journal.pone.0125076. eCollection 2015.
Parisi SG, Bartolini A, Santacatterina E, Castellani E, Ghirardo R, Berto A, et al. Prevalence of Klebsiella pneumoniae strains producing carbapenemases and increase of resistance to colistin in an Italian teaching hospital from January 2012 To December 2014. BMC Infect Dis. 2015;15:244.
Bonura C, Giuffrè M, Aleo A, Fasciana T, Di Bernardo F, Stampone T, et al. An update of the evolving epidemic of blaKPC carrying Klebsiella pneumoniae in Sicily, Italy, 2014: emergence of Multiple Non-ST258 Clones. PLoS One. 2015;10(7), e0132936. doi:10.1371/journal.pone.0132936.
Capone A, Giannella M, Fortini D, Giordano A, Meledandri M, Ballardini M, et al. High rate of colistin resistance among patients with carbapenem-resistant Klebsiella pneumoniae infection accounts for an excess of mortality. Clin Microbiol Infect. 2013;19(1):E23–30.
Tumbarello M, Trecarichi EM, De Rosa FG, Giannella M, Giacobbe DR, Bassetti M, et al. Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. J Antimicrob Chemother. 2015;70(7):2133–43.
Gaibani P, Lombardo D, Lewis RE, Mercuri M, Bonora S, Landini MP, et al. In vitro activity and post-antibiotic effects of colistin in combination with other antimicrobials against colistin-resistant KPC-producing Klebsiella pneumoniae bloodstream isolates. J Antimicrob Chemother. 2014;69(7):1856–65.
Falagas ME, Maraki S, Karageorgopoulos DE, Kastoris AC, Mavromanolakis E, Samonis G. Antimicrobial susceptibility of multidrug-resistant (MDR) and extensively drug-resistant (XDR) enterobacteriaceae isolates to fosfomycin. Int J Antimicrob Agents. 2010;35(3):240–3.
Rizek C, Ferraz JR, van der Heijden IM, Giudice M, Mostachio AK, Paez J, et al. In vitro activity of potential old and new drugs against multidrug-resistant gram-negatives. J Infect Chemother. 2015;21(2):114–7.
Perry JD, Naqvi SH, Mirza IA, Alizai SA, Hussain A, Ghirardi S, et al. Prevalence of faecal carriage of enterobacteriaceae with NDM-1 carbapenemase at military hospitals in Pakistan, and evaluation of two chromogenic media. J Antimicrob Chemother. 2011;66(10):2288–94.
Kresken M, Pfeifer Y, Hafner D, Wresch R, Körber-Irrgang B, Working Party ‘Antimicrobial Resistance’ of the Paul-Ehrlich-Society for Chemotherapy. Occurrence of multidrug resistance to oral antibiotics among Escherichia coli urine isolates from outpatient departments in Germany: extended-spectrum β lactamases and the role of fosfomycin. Int J Antimicrob Agents. 2014;44(4):295–300.
Kitchel B, Sundin DR, Patel JB. Regional dissemination of KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2009;53(10):4511–3.
Peirano G, Ahmed-Bentley J, Woodford N, Pitout JD. New Delhi metallo-beta-lactamase from traveler returning to Canada. Emerg Infect Dis. 2011;17(2):242–4.
Michalopoulos A, Virtzili S, Rafailidis P, Chalevelakis G, Damala M, Falagas ME. Intravenous fosfomycin for the treatment of nosocomial infections caused by carbapenem-resistant Klebsiella pneumoniae in critically ill patients: a prospective evaluation. Clin Microbiol Infect. 2010;16(2):184–6.
Karageorgopoulos DE, Miriagou V, Tzouvelekis LS, Spyridopoulou K, Daikos GL. Emergence of resistance to fosfomycin used as adjunct therapy in KPC Klebsiella pneumoniae bacteraemia: report of three cases. J Antimicrob Chemother. 2012;67(11):2777–9.
Docobo-Pérez F, Drusano GL, Johnson A, Goodwin J, Whalley S, Ramos-Martín V, et al. Pharmacodynamics of fosfomycin: insights into clinical use for antimicrobial resistance. Antimicrob Agents Chemother. 2015;59(9):5602–10.
Liscio JL, Mahoney MV, Hirsch EB. Ceftolozane/tazobactam and ceftazidime/avibactam: two novel β-lactam/β-lactamase inhibitor combination agents for the treatment of resistant Gram-negative bacterial infections. Int J Antimicrob Agents. 2015;46(3):266–71.
Titelman E, Karlsson IM, Ge Y, Giske CG. In vitro activity of CXA-101 plus tazobactam (CXA-201) against CTX-M-14- and CTX-M-15-producing Escherichia coli and Klebsiella pneumoniae. Diagn Microbiol Infect Dis. 2011;70(1):137–41.
Sader HS, Rhomberg PR, Farrell DJ, Jones RN. Antimicrobial activity of CXA-101, a novel cephalosporin tested in combination with tazobactam against enterobacteriaceae, Pseudomonas aeruginosa, and Bacteroides fragilis strains having various resistance phenotypes. Antimicrob Agents Chemother. 2011;55(5):2390–4.
Wagenlehner FM, Umeh O, Steenbergen J, Yuan G, Darouiche RO. Ceftolozane-tazobactam compared with levofloxacin in the treatment of complicated urinary-tract infections, including pyelonephritis: a randomised, double-blind, phase 3 trial (ASPECT-cUTI). Lancet. 2015;385(9981):1949–56.
Solomkin J, Hershberger E, Miller B, Popejoy M, Friedland I, Steenbergen J, et al. Ceftolozane/tazobactam plus metronidazole for complicated intra-abdominal infections in an era of multidrug resistance: results from a randomized, double-blind, phase 3 trial (ASPECT-cIAI). Clin Infect Dis. 2015;60(10):1462–71.
Xiao AJ, Miller BW, Huntington JA, Nicolau DP. Ceftolozane/tazobactam pharmacokinetic/pharmacodynamic derived dose justification for phase 3 studies in patients with nosocomial pneumonia. J Clin Pharmacol. 2015. doi:10.1002/jcph.566.
Castanheira M, Farrell SE, Krause KM, Jones RN, Sader HS. Contemporary diversity of beta-lactamases among enterobacteriaceae in the nine U.S. census regions and ceftazidime-avibactam activity tested against isolates producing the most prevalent beta-lactamase groups. Antimicrob Agents Chemother. 2014;58(2):833–8.
Vazquez JA, Gonzalez Patzan LD, Stricklin D, Duttaroy DD, Kreidly Z, Lipka J, et al. Efficacy and safety of ceftazidime-avibactam versus imipenem-cilastatin in the treatment of complicated urinary tract infections, including acute pyelonephritis, in hospitalized adults: results of a prospective, investigator-blinded, randomized study. Curr Med Res Opin. 2012;28(12):1921–31.
Lucasti C, Popescu I, Ramesh MK, Lipka J, Sable C. Comparative study of the efficacy and safety of ceftazidime/avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal infections in hospitalized adults: results of a randomized, double-blind, phase II trial. J Antimicrob Chemother. 2013;68(5):1183–92.
Actavis plc. Actavis Receives U.S. FDA Approval for AVYCAZ™ (CEFTAZIDIME-AVIBACTAM). 2015. Feb 25. http://www.prnewswire.com/news-releases/actavis-receives-us-fda-approval-foravycaz-ceftazidime-avibactam-300041592.html. Accessed 29 July 2015.
Tacconelli E, Cataldo MA, Dancer SJ, De Angelis G, Falcone M, Frank U, et al. ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients. Clin Microbiol Infect. 2014;20 Suppl 1:1–55.
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases, Division of Healthcare Quality Promotion. Guidance for control of carbapenem-resistant Enterobacteriaceae (CRE).2012 Toolkit. http://www.cdc.gov/hai/pdfs/cre/CRE-guidance-508.pdf. Accessed 29 July 2015.
Arnold RS, Thom KA, Sharma S, Phillips M, Kristie Johnson J, Morgan DJ. Emergence of Klebsiella pneumonia carbapenemase-producing bacteria. South Med J. 2011;104(1):40–5.
Schwaber MJ, Klarfeld-Lidji S, Navon-Venezia S, Schwartz D, Leavitt A, Carmeli Y. Predictors of carbapenem-resistant Klebsiella pneumonia acquisition among hospitalized adults and effect of acquisition on mortality. Antimicrob Agents Chemother. 2008;52(3):1028–33.
Centers for Disease Control and Prevention. Notes from the field: hospital outbreak of carbapenem-resistant Klebsiella pneumoniae producing New Delhi metallo-beta-lactamase—Denver, Colorado, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(6):108.
Schwaber MJ, Carmeli Y. An ongoing national intervention to contain the spread of carbapenem-resistant enterobacteriaceae. Clin Infect Dis. 2014;58(5):697–703.
Savard P, Perl TM. Combating the spread of carbapenemase in enterobacteriaceae: a battle that infection prevention should not lose. Clin Microbiol Infect. 2014;20(9):854–61.
Vaux S, Carbonne A, Thiolet JM, Jarlier V, Coignard B, RAISIN and Expert Laboratories Groups. Emergence of carbapenemase-producing Enterobacteriaceae in France, 2004 to 2011. Euro Surveill. 2011;16(22).
Sypsa V, Psichogiou M, Bouzala GA, Hadjihannas L, Hatzakis A, Daikos GL. Transmission dynamics of carbapenemase-producing Klebsiella pneumoniae and anticipated impact of infection control strategies in a surgical unit. PLoS One. 2012;7(7), e41068.
Akova M, Daikos GL, Tzouvelekis L, Carmeli Y. Interventional strategies and current clinical experience with carbapenemase-producing Gram-negative bacteria. Clin Microbiol Infect. 2012;18(5):439–48.
Schechner V, Kotlovsky T, Kazma M, Mishali H, Schwartz D, Navon-Venezia S, et al. Asymptomatic rectal carriage of blaKPC-producing carbapenem-resistant Enterobacteriaceae: who is prone to become clinically infected? Clin Microbiol Infect. 2013;19(5):451–6.
Savard P, Carroll KC, Wilson LE, Perl TM. The challenges of carbapenemase-producing enterobacteriaceae and infection prevention: protecting patients in the chaos. Infect Control Hosp Epidemiol. 2013;34(7):730–9.
Munoz-Price LS, Hayden MK, Lolans K, Won S, Calvert K, Lin M, et al. Successful control of an outbreak of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae at a long-term acute care hospital. Infect Control Hosp Epidemiol. 2010;31(4):341–7.
Gopinath R, Savard P, Carroll KC, Wilson LE, Landrum BM, Perl TM. Infection prevention considerations related to New Delhi metallo-beta-lactamase enterobacteriaceae: a case report. Infect Control Hosp Epidemiol. 2013;34(1):99–100.
Snitkin ES, Zelazny AM, Thomas PJ, Stock F, NISC Comparative Sequencing Program Group, Henderson DK, et al. Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci Transl Med. 2012;4(148):148ra116.
Passaretti CL, Otter JA, Reich NG, Myers J, Shepard J, Ross T, et al. An evaluation of environmental decontamination with hydrogen peroxide vapor for reducing the risk of patient acquisition of multidrug-resistant organisms. Clin Infect Dis. 2013;56(1):27–35.
De Rosa FG, Corcione S, Raviolo S, Montrucchio C, Aldieri C, Pagani N, et al. Candidemia, and infections by Clostridium difficile and carbapenemase-producing enterobacteriaceae: new enteropathogenetic opportunistic syndromes? Infez Med. 2015;23(2):105–16.
Lee GC, Burgess DS. Treatment of Klebsiella pneumoniae carbapenemase (KPC) infections: a review of published case series and case reports. Ann Clin Microbiol Antimicrob. 2012;11:32.
Tzouvelekis LS, Markogiannakis A, Piperaki E, Souli M, Daikos G. Treating infections caused by carbapenemase-producing Enterobacteriaceae. Clin Microbiol Infect. 2014;20(9):862–72.
De Oliveira MS, de Assis DB, Freire MP, Boas do Prado GV, Machado AS, Abdala E, et al. Treatment of KPC-producing enterobacteriaceae: suboptimal efficacy of polymyxins. Clin Microbiol Infect. 2015;21(2):179.e1-7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Matteo Bassetti, Davide Pecori, Francesco Giuseppe De Rosa, Marcella Sibani and Silvia Corcione have no disclosures relevant to this work.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Bacterial Infections and Drug Resistant Pathogens
Rights and permissions
About this article
Cite this article
Bassetti, M., Pecori, D., Sibani, M. et al. Epidemiology and Treatment of MDR Enterobacteriaceae . Curr Treat Options Infect Dis 7, 291–316 (2015). https://doi.org/10.1007/s40506-015-0065-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40506-015-0065-1