Abstract
In this study, a comparison is made of the findings of B-mode ultrasound and ultrasound elastography with the Lens Opacities Classification (LOCS) grade in patients with senile cataracts. A total of 74 patients with cataracts and 32 age-matched healthy volunteers as the control group were evaluated in the departments of ophthalmology and radiology between 2016 and 2017. In the patient group, cataracts were graded according to LOCS, and B-mode sonographic appearance and elasticity measurements were recorded, after which the cataract grade and sonoelastography/B-mode ultrasound findings were compared using statistical methods. Among the 74 patients with cataracts, 38 were females (51.4%) and 36 were males (48.6%), and the mean age was 62.05 ± 7.95 (43–78) years. A Chi-square test revealed a significant relationship between ultrasound echogenicity of cataract and grade of cataract (p < 0.005). The ultrasound elastography revealed a mean shear-wave velocity of 2.90 m/s ± 0.371 (2.13–3.53) among patients with grade 3 cataracts, 3.1 m/s ± 0.45 (2.26–3.98) among patients with grade 4, 3 m/s ± 0.58 (2.35–4.60) among patients with grade 5 and 3 m/s ± 0.528 (2.31–4.50) among patients with grade 6 cataracts, and 3 m/s ± 0.258 (2.36–3.58) among the normal subjects. No statistically significant difference was noted in the analysis of variance (p > 0.005). While cataract grade and B mode echogenicity were directly proportional, there was no significant difference in lens elasticity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The lens is located behind the iris, and is avascular structured, lacking both blood vessels and nerves. The primary function of the lens is to allow the entry of light and to focus on the retina. The transparency of the lens is a result of the high amount of proteins in the cytoplasm and its regular organization; while the lucidity of the lens depends on the organization and arrangement of the protein structure, and subtle changes in this structure leads to lens opacification [1, 2]. A cataract is a cloudiness of the lens that results in impaired vision, and occurs when the lens loses its ability to absorb and radiate light rays, and can lead to a decrease in visual acuity and blindness. The prevalence rate is higher in females and it is among the leading causes of blindness in developing countries [3,4,5].
Cataracts are diagnosed through biomicroscopic examinations. The most common form is senile cataract, which has various subtypes, including nuclear cataract, posterior subcapsular cataract and cortical cataract.
Various classification methods are used to evaluate cataract density. The Lens Opacities Classification System II (LOCS II) and LOCS III are based on a slit-lamp examination performed by an ophthalmologist [6, 7].
In this study, it was aimed to compare lens density classification of senile cataract using LOCS III system, with lens’s B-mode ultrasound and shear-wave elastography findings.
Materials and method
A total of 74 patients with senile cataracts (56 unilateral, 18 bilateral) and 32 control subjects in the same age range were evaluated in the ophthalmology and radiology departments of our hospital between 2016 and 2017. The ethics committee of the hospital approved the study and written informed consent was obtained from all of the patients. The Lens Opacities Classification System III (LOCS III) is based on a comparison of standardized photographs, and is commonly used in the grading of lens density in patients with senile cataracts [7]. The system makes use of a slit-lamp examination [8]. Cataracts are graded from 1 to 6, according to cataract density.
The patients diagnosed with senile cataracts in the department of ophthalmology and the subjects assigned to the control group all underwent complete ophthalmologic examinations. Using traditional methods, cataract density was graded through a slit-lamp examination based on LOCS III. (Fig. 1) After evaluating the best visual acuity of the patients, a biomicroscopic examination was performed, intraocular pressure was measured, and cataract density was graded with a biomicroscopic slit-lamp examination after pupil dilation had been achieved using tropicamide eye drops (1%) (grading range 3.0–6.0), after which a fundoscopic examination was carried out. All ophthalmologic examinations and cataract gradings were made by a single experienced ophthalmologist. The patients were then evaluated in the department of radiology. The radiologist performing the elastography and B-mode ultrasound was blinded to the study groups (cataract group, control group) and cataract grades.
The LOCS III standard images in an 8.5-inch, 11-inch color transparency as used in the office at the slit-lamp microscopy. The Lens Opacities Classification System version III (LOCS III) is a standardized photographic comparison system for grading the features of cataract. It has been used to grade the type and severity of cataract in cross-sectional studies. It also has been used to grade cataracts at the slit lamp. The brightness of scatter from the nuclear region has been designated nuclear opalescence and the intensity of brunescence, nuclear color. The amount of cortical cataract and the estimated amount of posterior subcapsular cataract is determined by comparing
Patients diagnosed with senile cataracts were included in the study, while patients with other cataract types, such as traumatic cataract and congenital cataract, patients with glaucoma, patients with an ocular disease hindering lens examination, patients with grade 1 or 2 cataract on ophthalmologic examination, and patients with a systemic disorder like diabetes that could cause cataracts were excluded.
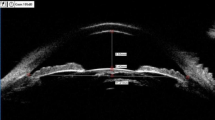
The B-mode sonographic examination and quantitative shear-wave elastography measurements of the lens were performed by the same radiologist, who had 11-year ultrasound experience and 3 years of elastography experience. During the radiological examination, the patients were instructed to close their eyes while placed in supine position and to stare up straight at the ceiling without blinking or looking around, to the best of their ability. The probe was pressed softly onto the eyelid in contact with the skin, with particular attention paid to the thickness of the gel between the probe and the eyelid. Lens to be evaluated with ultrasound elastography was detected and the echogenicity of the lens was determined as hypoechoic, isoechoic or hyperechoic, based on the neighboring subcutaneous fat tissue planes. A split window was created on the display screen with the dual button, and the margins of the cataract lens were marked in the right window (gray-scale US). In the left window (US elastography), the margins of the same lens were marked automatically by the device within the gray-scaled region of interest (ROI). Small boxes measuring shear-wave velocity were placed within this area. The boxes were placed in a certain sequence on the vertical–horizontal planes to cover the entire axial section of the lens so as to obtain a more reliable average value (Fig. 2a, b). At least four measurements were made on a single axial plane. The average shear-wave velocity, and thus the rigidity of the lens, was calculated based on these variable numbers. US imaging and elastography examinations were made using a Siemens ACUSON S2000™ ultrasound device (Siemens Healthcare, Erlangen, Germany). The Acoustic Radiation Force Impulse (ARFI) elastography application was performed using the Virtual Touch IQ option with a 4–9 MHz 9L4 linear probe. In the following stage, the relationship of cataract grade with echogenicity in the B-mode ultrasound and elasticity values were investigated. The mean echo values in B mode ultrasound were calculated as decibels for each grade.
Cataract LOCS III grade was compared with the B-mode images using a Chi-squared test. A one-way analysis of variance (ANOVA) was used to evaluate the relationship between elasticity values and ophthalmologic grade. All statistical analyses were made using SPSS version 20.0 software (IBM Corporation, Armonk, NY, USA).
Results
A total of 106 subjects (74 patients that underwent ophthalmologic cataract grading in the last 1 year in our hospital and 32 normal subjects) underwent B-mode ultrasonographic and elastographic examinations. In patients with senile cataracts, 38 were females (51.4%) and 36 were males (48.6%), and the mean age was 62.05 ± 7.95 (43–78) years. Of the subjects in the control group, 16 were males (50%) and 16 were females (50%), and the mean age was 64.37 ± 7.76 (51–80) years. Based on the B-mode ultrasound examination of 106 subjects, in which the neighboring subcutaneous fat tissue was referenced, lens echogenicity was classified as hypoechoic, isoechoic or hyperechoic. Average echo amplitudes in decibels were shown graphically. (Fig. 3).
Patients classified as grade 1 or 2 in the ophthalmologic examination were excluded from the study, being regarded as clinically normal. Among the patients with grade 3 cataracts, the lens was found to be hypoechoic in 12 and isoechoic in four patients in the B-mode ultrasound examination. None of the patients had a hyperechoic appearance. Among the 19 patients with grade 4 cataracts, the lens was hypoechoic in 10, isoechoic in 4 and hyperechoic in 5 patients; while among the 24 patients with grade 5 cataracts, the lens was hypoechoic in 6, isoechoic in 12 and hyperechoic in 6 patients. Similarly, among the 15 patients with grade 6 cataracts, the lens was hypoechoic in 3, isoechoic in 2 and hyperechoic in 10 patients and 32 hypoechoic in normal patients (Fig. 4; Table 1). In a statistical analysis using a Chi-squared test, a relationship was identified between B-mode echogenicity and ophthalmologic grade (p < 0.001).
The ultrasound elastography revealed a mean shear-wave velocity of 2.90 m/s ± 0.371 (2.13–3.53) among patients with grade 3 cataracts, 3.1 m/s ± 0.45 (2.26–3.98) among patients with grade 4, 3 m/s ± 0.58 (2.35–4.60) among patients with grade 5, 3 m/s ± 0.528 (2.31–4.50) among patients with grade 6 cataracts, and 3 m/s ± 0.258 (2.36–3.58) among the normal subjects, and there was no statistically significant difference in the analysis of variance (p > 0.005).
Discussion
Cataracts occur when the lens loses its ability to absorb and radiate light beams. The prevalence of cataracts is higher in females around the world, and occurs at young ages in developing countries [1,2,3]. The most important risk factor is the patient’s age. The majority of the patients in the present study were older people, and there was a higher ratio of women.
LOCS III is currently the most preferred system for the grading of senile cataracts, although the system is limited by the bias of the examiner and the lack of reproducibility [10, 11]. Previous studies have adopted other lens grading systems, such as the Scheimpflug system, which results quantitative values using lens densitometry [12,13,14], although the accuracy of these systems is limited by problems inherent to the cornea and changes in the anterior surface of the lens that complicate the examination of the interior structure of the lens [10, 15]. There have also been studies evaluating lens opacities using anterior segment optic coherence computed tomography [16, 17]. There is ongoing research into the formulation of new classification systems that are based on more objective, reproducible, and quantitative data. In cataract patients, the lens is initially more homogeneous and light colored and its density increases with time. Ultrasonic elastography is a new radiological method used to numerically evaluate tissue stiffness or elasticity. It has been developed over many years and has been the subject of many studies. When external forces are applied to any tissue, deformation occurs in the tissue. Elastography measures this deformation in the tissue and converts the data into ultrasound images, whereas traditional B-mode ultrasonography shows the morphology of the tissue [18]. Although we could not find a statistically significant difference between the measurements taken in all grade cataracts and normal patients when examined by ultrasound elastography, we believe that a statistically significant difference could be detected with a larger group of patients. Besides the small number of patients, the fact that ultrasound is dependent on the worker also leads to this result. As another reason, we think that even though there is an increase in echo in the lens due to fluid decrease over time, tissue elasticity due to probable internal necrosis might not change.
In a B-mode ultrasound examination, the lens normally appears hypoechoic in reference to subcutaneous fat tissue, although no study could be found in literature supportive this finding. The lens can be expected to be hyperechoic to subcutaneous fat planes due to its protein-rich structure. In our cases, the echogenicity was increased in B-mode ultrasound as cataract degree increased, and these findings were found to be statistically significant (p = 0.0002). We think that, therefore, ultrasound echogenicity may be supportive in the grading of cataract lens, and that a non-invasive sonographic examination of the lens could be useful in the evaluation of the severity of cataract and in the prognosis.
Shiina et al. found that by quantitatively measuring lens ultrasound attenuation values, cataract patients differed from the normal lens, which would be helpful in early cataract diagnosis and distinguishing cataract types [19]. We also found that echogenicity increased as the grade of senile cataract increased and we obtained similar results.
There are important limitations in this study, the first of which relates to the lack of a sufficient number of patients representing each cataract grade; while, a second limitation was the lack of intra- and interobserver evaluations. The third limitation relates to the subjective nature of the measurements, considering the small working area and its sensitivity to positional changes. Finally, no gender analysis was performed.
In conclusion, increases in sonographic B-mode echogenicity are directly proportional to increases in cataract grade, while we could not find significant relationship between lens elasticity on shear-wave elastography and cataract grade. Thus, in clinically indistinguishable cases, lens echogenicity may be used in the diagnosis of cataract.
References
Nirmalan PK, Robin AL, Katz J, Tielsch JM, Thulasiraj RD, Krishnadas R, Ramakrishnan R (2004) Risk factors for age related cataract in a rural population of southern India: the Aravind Comprehensive Eye Study. Br J Ophthalmol 88:989–994 [PubMed: 15258010]
Allen D, Vasavada A (2006) Cataract and surgery for cataract. BMJ 333:128–132 [PubMed: 16840470]
Chatterjee A, Milton RC, Thyle S (1982) Prevalence and aetiology of cataract in Punjab. Br J Ophthalmol 66:35–42 [PubMed: 7055541]
Congdon NG, Friedman DS, Lietman T (2003) Important causes of visual impairment in the world today. JAMA 290(15):2057–2060
Pascolini D, Mariotti SP, Pokharel GP et al (2004) 2002 global update of available data on visual impairment: a compilation of population-based prevalence studies. Ophthalmic Epidemiol 11:67–115
Maraini G, Pasquini P, Tomba MC et al (1989) An independent evaluation of the Lens Opacities Classification System II (LOCS II); the Italian–American Cataract Study Group. Ophthalmology 96:611–615
Chylack LT, Wolfe JK, Singer DM et al (1993) The lens opacities classification system III. Arch Ophthalmol 111:831–836
Karbassi M, Khu PM, Singer DM, Chylack LT Jr (1993) Evaluation of Lens Opacities Classification System III applied at the slitlamp. Optom Vis Sci 70:923–928
Hall NF, Lempert P, Shier RP, Zakir R, Phillips D (1999) Grading nuclear cataract: reproducibility and validity of a new method. Br J Ophthalmol 83(10):1159–1163
McAlinden C, Khadka J, Pesudovs K (2011) A comprehensive evaluation of the precision (repeatability and reproducibility) of the Oculus Pentacam HR. Invest Ophthalmol Vis Sci 52(10):7731–7737
Skiadaresi E, McAlinden C, Ravalico G, Moore J (2012) Optical coherence tomography measurements with the LENTIS Mplus multifocal intraocular lens. Graefe’s Arch Clin Exp Ophthalmol 250(9):1395–1398
Hockwin O, Dragomirescu V, Laser H (1982) Measurements of lens transparency or its disturbances by densitometric image analysis of scheimpflug photographs. Graefe’s Arch Clin Exp Ophthalmol 219(6):255–262
Magno BV, Freidlin V, Datiles MB III (1994) Reproducibility of the NEI scheimpflug cataract imaging system. Investig Ophthalmol Vis Sci 35(7):3078–3084
Datiles MB III, Magno BV, Freidlin V (1995) Study of nuclear cataract progression using the national eye institute scheimpflug system. Br J Ophthalmol 79(6):527–534
Dubbelman M, Van der Heijde GL (2001) The shape of the aging human lens: curvature, equivalent refractive index and the lens paradox. Vis Res 41(14):1867–1877
Wong AL, Leung CK-S, Weinreb RN et al (2009) Quantitative assessment of lens opacities with anterior segment optical coherence tomography. Br J Ophthalmol 93(1):61–65
Kim YN, Park JH, Tchah H (2016) Quantitative analysis of lens nuclear density using optical coherence tomography (OCT) with a liquid optics interface: correlation between OCT images and LOCS III grading. J Ophthalmol 2016:3025413
Ozgokce M, Yavuz A, Akbudak I, Durmaz F et al (2018) Usability of transthoracic shear wave elastography in differentiation of subpleural solid masses. Ultrasound Q 34(4):233–237. https://doi.org/10.1097/RUQ.0000000000000374
Shiina T, Ito M, Sugata Y, Yamamoto Y (1992) An application of ultrasonic tissue characterization to the diagnosis of cataract. In Proceedings of the annual international conference of the IEEE Engineering in Medicine and Biology Society, vol 14. Paris, France, 29 October–1 November 1992, 2768A
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its amendments or comparable ethical standards.
Funding
No funding was received.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozgokce, M., Batur, M., Alpaslan, M. et al. A comparative evaluation of cataract classifications based on shear-wave elastography and B-mode ultrasound findings. J Ultrasound 22, 447–452 (2019). https://doi.org/10.1007/s40477-019-00400-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-019-00400-6