Abstract
Background
Cataracts are lens opacifications that are responsible for more than half of blindness cases worldwide, and the only treatment is surgical intervention. Phacoemulsification surgery, the most frequently performed cataract surgery in developed countries, has associated risks, some of which are related to excessive phacoemulsification energy levels and times. The protocol proposed in herein will be used to evaluate the feasibility of a new experimental medical device, the Eye Scan Ultrasound System (ESUS), for the automatic classification of cataract type and severity and quantitative estimation of the optimal phacoemulsification energy.
Methods
The pilot study protocol will be used to evaluate the feasibility and safety of the ESUS in clinical practice. The study will be conducted in subjects with age-related cataracts and on healthy subjects as controls. The procedures include data acquisition with the experimental ESUS, classification based on the Lens Opacity Classification System III (LOCS III, comparator) using a slit lamp, contrast sensitivity test, optical coherence tomography, specular microscopy and surgical parameters.
ESUS works in A-scan pulse-echo mode, with a central frequency of 20 MHz. From the collected signals, acoustic parameters will be extracted and used for automatic cataract characterization and optimal phacoemulsification energy estimation.
The study includes two phases. The data collected in the first phase (40 patients, 2 eyes per patient) will be used to train the ESUS algorithms, while the data collected in the second phase (10 patients, 2 eyes per patient) will be used to assess the classification performance. System safety will be monitored during the study.
Discussion
The present pilot study protocol will evaluate the feasibility and safety of the ESUS for use in clinical practice, and the results will support a larger clinical study for the efficacy assessment of the ESUS as a diagnostic tool. Ultimately, the ESUS is expected to represent a valuable tool for surgical planning by reducing complications associated with excessive levels of phacoemulsification energy and surgical times, which will have a positive impact on healthcare systems and society. The study is not yet recruiting.
Trial registration
ClinicalTrials.gov identifier NCT04461912, registered on July 8, 2020.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Background
Cataracts account for over half of blindness cases worldwide, with the only established treatment being the surgical removal of the cataractous lens and replacement with an intraocular lens (IOL) [1, 2]. Several scientific contributions were crucial to the evolution of cataract surgery. The first key finding was identified in the mid-twentieth century for Second World War fighter pilots, in which intraocular fragments of shattered acrylic from canopies were well tolerated. This fact led to the development of the first IOL using this material [3]. In approximately 1960, A-scan ultrasonic systems emerged for measuring the axial eye length [4], which allowed to determine the refractive power of the IOLs, thereby reducing the previously significant postoperative refractive errors [3, 4]. In 1967, high-precision ultrasonic equipment working at 10 MHz was further developed, which solved some remaining limitations of the previous systems, such as the deformation produced by the probe over the cornea, inability to perform alignments within the visual axis and large beam diameters [5]. Moreover, in the same year, the first phacoemulsification surgery was performed using ultrasonic waves for fragmentation of the cataractous lens [6]. This technique introduced a more controlled, faster and safer method of extracapsular cataract extraction, which provided significant advantages for cataract treatment.
Cataract surgery has evolved in recent years, thus making the method safer and more efficient. However, risks are still associated with this procedure. Among them, posterior lens capsular rupture and corneal endothelial cell loss related to excessive levels of phacoemulsification energy represent approximately 5 to 10% of postoperative complications [7, 8]. Posterior capsular rupture has diverse associated risks such as vitreous loss and dropped nucleus, increasing the risk of cystoid macular oedema or retinal detachment. In turn, corneal oedema and opacification may result from corneal endothelial cell loss. These complications may limit or prevent visual recovery [7].
Acoustic parameters extracted from ultrasonic waves propagating in cataractous lenses have been widely studied to characterize their structural and biomechanical properties. Several studies have characterized the presence and severity of cataracts using this approach [4, 8,9,10,11,12]. Moreover, studies have used ultrasound for cataract hardness estimation [8, 13,14,15,16,17,18,19,20] since the efficient energy that must be applied to phacoemulsification surgeries is directly related to cataract hardness [17]. Most of these studies were conducted in porcine lenses due to the similarities in their acoustic parameters with human lenses [21].
Preclinical studies were conducted by the research team with two models of cataracts: ex vivo in porcine lenses [8, 20] and in vivo in rat lenses [12]. These studies evaluated several automatic classification methods for cataract hardness and severity based on features extracted from the ultrasonic signals. The results showed a precision, sensitivity and specificity of 99.7% for cataract severity classification, as well as a statistically significant difference in lens hardness for the different cataract severities [12].
The present pilot study protocol aims to evaluate the Eye Scan Ultrasound System (ESUS), which was developed in the preclinical studies [22] and adapted for clinical applications [23] in human lenses in vivo. Because it is a first in human study, and to reduce risks and optimize human and financial resources, a pilot protocol was designed for feasibility assessment of the ESUS in clinical practice. It aims to assess the feasibility of detecting and characterizing human cataracts by ultrasound and the suitability and safety of the technique for use in clinical practice. Related to cataract characterization, the study protocol was designed to evaluate the performance of the experimental medical device ESUS for the automatic classification of cataract type and severity based on the Lens Opacity Classification System III (LOCS III, [24]) and to estimate the optimal phacoemulsification energy (OPE).
The study protocol is organized in two phases. In the first phase, the collected data will be used for training the automatic detection and classification algorithm for human cataracts. In the second phase, the collected data will be used for a preliminary assessment of the algorithm performance. Cataracts classified according to the LOCS III for type and severity [24] will be used as comparators. Safety will be evaluated throughout the study.
The experimental medical device may represent an important advance in cataract treatment based on two main contributions. First, cataracts should be detected at incipient stages, even before the onset of symptoms, in patients at high risk of developing cataracts. At incipient stages, visual acuity is preserved, which may favour the outcomes of emerging pharmacological therapies [1, 25]. On the other hand, with ESUS, it is expected to achieve quantitative and automatic estimation of OPE. It may represent a valuable tool in surgical planning by reducing complications associated with excessive levels of phacoemulsification energy and excessive surgical times [7]. These advances are relevant not only for patients but also for public health systems because they may reduce waiting lists and associated costs.
Further clinical studies will be needed to enlarge the database to improve the performance of cataract classification and better evaluate the technique’s efficacy and to include other causes of cataracts since only age-related cataracts are considered in the present protocol.
The manuscript follows the SPIRIT [26] and CONSORT [27] reporting guidelines and checklists and the editorials [28, 29].
Objectives
Primary objective
Evaluate the feasibility of the ESUS (experimental medical device) for cataract characterization in humans.
Secondary objectives
-
i.
Automatically detect and classify cataracts according to their type and severity.
-
ii.
Detect cataract in the incipient stage.
-
iii.
Estimate the OPE.
-
iv.
Assess the automatic classification performance.
-
v.
Evaluate the safety of the ESUS.
Methods
Trial design
Pilot, nonblinded and monocentre study.
Participants
Study setting
The participants will be recruited from patients who have a medical consultation scheduled at the clinical centre (Coimbra Surgical Centre, Portugal).
Two groups are considered in this study. For the cataract group, the patients will be invited to participate after being diagnosed with cataracts and referred to phacoemulsification surgery by the physician. For the control group, the patients will be invited to participate after the presence of cataracts is excluded. For both groups, the inclusion/exclusion criteria must be verified.
Inclusion and exclusion criteria
Inclusion criteria
-
i.
Between 50 and 70 years old
-
ii.
Either gender
-
iii.
Cataract group
-
○ Patients with age-related cataract
-
○ Indication for phacoemulsification surgery
-
iv.
Control group
-
○ Patients without cataract
-
xxii.
Signed consent
Exclusion criteria
-
i.
The presence of any other ophthalmological condition or systemic disease that could affect the results.
Recruitment procedure and informed consent
Medical investigators of the research team will recruit the participants. He/she must inform the patients about the study objectives, the procedures involved, the visit schedule, the benefits and risks of their participation, the privacy policies and the freedom to participate or withdraw. The investigator must provide enough time for consent form reading and clarify all doubts. If the patient agrees to participate, he/she (or their legal representative) and the medical investigator must sign the consent form. One copy of the consent form will be given to the participant, and the original document will be kept at the clinical centre.
Participation time and anticipated withdrawal
The maximum participation time for each subject is 3 months. Participant inclusion will be confirmed on the same day that cataracts are diagnosed or excluded. Participants in the control group will complete the procedures on the same day, and a remote follow-up will be conducted 1 week later. Participants in the cataract group will complete the study on the day of the second postoperative follow-up (1 month after surgery). If the second eye receives an indication for phacoemulsification surgery, data for this second eye will also be collected.
An anticipated withdrawal of the participants is considered in the following situations: the occurrence of any unanticipated adverse effects, anticipation of a risk situation, any physical condition that makes it impossible to conduct the procedures involved in the study, or the voluntary withdrawal of the participant. In all these cases, the causes for participant withdrawal should be registered in the individual case report form (CRF), and the participants will be encouraged to perform a final follow-up. Codified data collected before the participant withdrew can be used for the purpose of the study.
Sample size and allocation
In the first phase of the clinical study, forty participants will be included, and the two eyes will be studied. The participants will be equally distributed into four groups (based on slit lamp/LOCS III classification): participants with incipient, moderate and severe cataracts and participants without cataracts will be included as the control group. The second phase will include at least ten participants, and the two eyes will be studied. Safety will be evaluated for all the recruited participants along the first and second phases.
Since this is a protocol for a pilot study, no sample size estimate was performed. The number of eyes expected to be analysed along the study (i.e. 20 per arm) was considered adequate for this study [30]. The statistical power will be determined at the end of the study for statistically significant results.
Procedures
The participants’ visit schedule is presented in Table 1, and descriptions of the interventions and assessments are given below.
ESUS (investigational medical device)
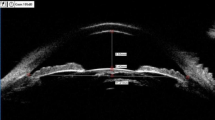
The ESUS components are presented in Fig. 1 and Table 2. The system is composed of an A-scan ophthalmic probe working in pulse-echo mode, with an acoustic working frequency of 20 MHz and focal distance of approximately 8 mm. The active probe surface is shaped to match the cornea curvature, thus favouring their coupling and signal transmission with minimal coupling pressure. The probe front face (that contacts the eye) is manufactured with biocompatible material. The probe is connected to the xScan, whose functions are as follows: send excitation pulses to the probe, generate synchronism signals, digitize the signals captured back by the probe (at a sample frequency of 100 MHz) and preprocess the digitized signals (filtering and amplification). The output of the xScan system is connected to a computer. To establish communication between the xScan and the computer, a programme was developed in C++. This programme is automatically executed through a user-friendly interface (UI) developed in MATLAB (MathWorks, Inc., Natick, MA, USA). The UI was programmed so that the ESUS is automatically configured within safe acoustic outputs.
Based on Annex VIII of Regulation (EU) 2017/745 of the European Parliament, the ESUS is classified as a type 2a medical device. This system has been developed in agreement with the Portuguese regulation, Law n° 145/2009 and with Regulation (EU) 2017/745 of the European Parliament.
ESUS procedures
-
i.
Participant preparation: To reduce the discomfort generated by coupling the probe, topical anaesthesia (oxybuprocaine hydrochloride) will be applied before starting the acquisitions. However, if the participant has any known contraindication to this anaesthetic, a disposable neutral contact lens will be used as a replacement for the coupling medium between the probe and the cornea.
-
ii.
The acquisitions are initiated through a starting button in the user interface, and the probe (previously clean and disinfected) is coupled to the eye after applying eye drops. The probe must be kept in place for a few seconds for automatic signal recording. During this period, signals are visualized in the user interface. Notably, as part of the clinical practice, the participant pupils will be previously dilated.
-
iii.
Finally the probe is uncoupled, and the signals are saved in a directory along with other participant information.
Demographic and medical record
This information will be obtained from the patient record at the clinical centre with the purpose of confirming the inclusion/exclusion criteria and identifying biases. The data to be recorded are birth date, sex, occupation history, smoking and drinking habits and history of any ophthalmic or systemic diseases and associated treatments.
Slit lamp and LOCS III
Slit lamp is a noninvasive method in which cataracts are photographed by retroillumination. The cataract images will be classified according to the LOCS III for cataract type and severity [24]. Cataract classification by this method will be the comparator for this study, used to train the automatic classification system and evaluate its performance in humans.
Contrast sensitivity test
This test consists of observing images and identifying shapes of variable contrast. Contrast sensitivity is particularly affected in cataracts. Cases of incipient cataract, where slit lamp observation may not be sufficiently sensitive, may be identified by this method.
Specular microscopy
Specular microscopy is a noninvasive technique in which images are reconstructed from the specular reflection of an incident light beam magnified by a microscope. The density and shape of corneal endothelial cells will be evaluated by this method to diagnose corneal endothelial cell loss, which relates to excessive levels of phacoemulsification energy.
Optical coherence tomography (OCT)
OCT is a noninvasive diagnostic method, in which the reflection of a low-coherence light beam is used for image reconstruction. OCT will be used for measuring macular thickness to detect the presence of macular oedema, one of the possible postoperative complications of phacoemulsification surgeries [7]. This study is conducted as part of the clinical practice in patients submitted to phacoemulsification surgery.
Phacoemulsification surgery
The phacoemulsification procedure will be performed according to normal clinical practice. The maximum energy level used in the phacoemulsification surgery, the phacoemulsification time and possible surgical complications will be recorded to evaluate the appropriateness of phacoemulsification energy levels. This study will not interfere with the clinical surgery protocols.
Safety monitoring
The safety of the experimental medical device will be further monitored by clinical examination of the participants immediately after the ESUS study and by remote follow-up 1 week later. After this period, no adverse events related to the ESUS study will be expected.
Overall safety conditions will be monitored through the occurrence of unanticipated adverse events or serious adverse events. If these situations occur, the reportable adverse events will be communicated to the competent authorities according to current regulation, and the corrective actions will be implemented.
Outcomes
Primary outcome
The presence of cataract is obtained with the ESUS.
Secondary outcomes are as follows:
-
i.
Cataract type and severity estimated with ESUS based on the LOCS III
-
ii.
Cataract hardness estimated with ESUS, measured in GPa
-
iii.
OPE level estimated with ESUS based on the parameters indicated by the phacoemulsifier
-
iv.
Number and severity of ESUS-related adverse events
Timelines and methods for outcomes recording
Study status: not yet recruiting
Starting date: October 2022
The total duration of the clinical study will be 15 months, and it will be divided into two phases:
-
First phase: 9 months (6 months for recruitment and 3 months for participant follow-up).
-
Second phase: 6 months (3 months for recruitment and 3 months for participant follow-up).
In the first phase, the cataract type and severity measured with slit lamp/LOCS III and contrast sensitivity will be used to train the algorithms for cataract detection and classification in humans. The surgical records (maximum phacoemulsification energy, phacoemulsification time and surgical complications), number and morphology of endothelial cells (measured by specular microscopy), the presence of macular oedema (assessed by OCT) and postoperative complications will support algorithm development for the estimation of OPE.
In the second phase, the cataract type and severity classification and OPE estimation will be implemented with the ESUS using the algorithms developed/trained in the first phase. The remaining study assessments will be used for preliminary performance evaluations. The methods for algorithm development are described in the “Statistical analysis” section.
Statistical analysis
Feasibility assessment
The feasibility of the ESUS technique will be evaluated based on cataract detectability, cataract classification and OPE estimative performances and on the ESUS safety.
Cataract detectability will be considered suitable if at least 90% of the cases detected through slit lamp observations are identified by the ESUS.
The cataracts classification will be considered suitable if sensitivity levels higher than 90 %, with a maximum significance level of 5%, are reached.
The system efficacy for the OPE will be considered suitable if the prediction accuracy is higher than 90%.
Since the clinical procedure involved in data acquisition with the ESUS is similar to the used in biometry for IOL power calculation, the procedure viability is not object of the study.
The ESUS safety will be considered suitable under two conditions: (i) there are no occurrence of serious adverse event associated with ESUS whose causes cannot be rectified; (ii) the occurrence rate of mild to moderate ESUS-related adverse events is lower than 5%.
The feasibility study will be considered successful if at least the primary objective, detection of the presence of cataracts, and the secondary objective of cataracts classification (type and severity) are reached and if the safety of the ESUS technique is verified.
Cataract type and severity estimation
The automatic classification system will classify the cataract type (nuclear, cortical, or posterior subcapsular) and evaluate the severity.
From the acquired ultrasonic signals, several acoustic parameters in the time and frequency domains will be extracted. Then, more representative parameters will be selected through a principal component analysis and used for automatic classifier training (e.g. support vector machine, Bayes network and random forest). The performance of the different classifiers will be compared. The classification obtained by a trained specialist using the LOCS III will be used as a reference.
In the second study phase, a preliminary evaluation of the automatic classification performance will be conducted using a new dataset. It will be considered suitable if it reaches sensitivity levels higher than 90%, with a maximum significance level of 5%.
All the participants/eyes performing the ESUS study will be included in the analysis.
OPE estimation
To develop an OPE estimator, the acoustic parameters extracted from the ultrasonic signals in the first phase will be correlated with the maximum energy used in the phacoemulsification surgery for each participant eye. Only surgeries without surgical or postoperative complications will be considered. A confidence interval of 95% followed by multiple comparison correction will be used to assess the significance of the correlations.
In the second phase, the acoustic parameters extracted from the ultrasonic signals will be used to predict the safety and risk intervals of phacoemulsification energy based on the correlation curves. To evaluate the prediction accuracy, surgeons should initiate surgeries at minimum energy levels and increase them gradually until they reach an efficient energy level. Then, the maximum energy level applied during surgery and the occurrence of surgical and/or postoperative complications will be compared with the safe and risk energy intervals predicted with the correlation curves. The system efficacy will be considered suitable if the prediction accuracy is higher than 90%.
Interim analysis
An interim analysis will be performed between the end of the first phase of the study and the beginning of the second phase of the study.
The sponsor will continuously analyse safety data and will evaluate the results from the interim analysis. Based on the analyses, a consensus between the responsible investigator and the sponsor may end or suspend the study. The Portuguese National Authority for Medicaments and Health Products (INFARMED, I.P.) or the Portuguese National Ethical Committee for Clinical Research (CEIC) may also prematurely end the study.
Ethics, safety and dissemination
Ethical considerations
The protocol is based on respect for the life, health, well-being and privacy of the participants. The study will be conducted in accordance with the ethical principles stated in the Helsinki Declaration. The study protocol was approved by the INFARMED, I.P., the CEIC and the independent Ethical Committee of the Coimbra Surgical Centre.
Patient and public involvement
The patients or the public were not involved in the design of the clinical study.
Safety considerations
A safety evaluation of the ESUS has been previously reported [31]. The ESUS has been implemented in agreement with Portuguese Law n° 145/2009 and with Regulation (EU) 2017/745 of the European Parliament. Safety assessment was based on the standards DIN EN ISO 14971:2009-10 [32], IEC 60601-2-37 [33], IEC 62127-1 [34] and IEC 62359 [35]. Several potential risks were identified and managed, including the following:
-
i.
Thermal and mechanical effects of ultrasound
-
ii.
Excessive surface temperatures
-
iii.
Electrical leakage
-
iv.
Allergies
-
v.
Mechanical risks
-
vi.
Contamination
-
vii.
Biocompatibility
-
viii.
Configuration errors
-
ix.
Electromagnetic interferences
Based on the ESUS risk assessment and management, there are no predictable adverse effects related to the use of the experimental medical device. Nonetheless, the sponsor will continuously monitor safety data and take the necessary measures to ensure participant safety. The remaining procedures to be implemented in the context of the study are noninvasive and will be carried out with certificated and commercial devices and by experienced specialists, not representing potential risks.
Financing and insurance
The participants will not receive any monetary compensation or incur any expenses related to their participation in the study. However, they will be covered by an insurance policy from the HDI Global SE company.
Protocol amendments
Any significant amendment in the protocol should be previously authorized by the sponsor and the competent authorities. If any protocol adjustment requires rapid execution due to safety reasons, it will be implemented without previous authorization and communicated a posteriori within no more than 10 business days.
Dissemination
The results obtained in this study will be published in peer-reviewed journals and presented at national and international congresses. Study publications will be written in agreement between the sponsor and the principal investigator. Additionally, a patent for the ESUS is expected at the end of the study.
Data management and confidentiality
All participants’ data will be recorded on individuals’ CRF in a legible and reliable way. The sponsor/representative should verify the complete and correct data.
Each participant will be identified by a unique numerical code of three digits. The principal investigator will be responsible for protecting the forms that identify the individual and relate them to the numerical code (i.e. the consent form and contact information pages of the CRF). The codified parts of the CRF will be transmitted to the sponsor.
A digital and a printed copy of the CRF will be kept to avoid accidental loss. All data collected during the study should be maintained at the investigational centre for a period of 25 years according to Regulation (EU) 536/2014 of the European Parliament.
The identity of the participants will not be revealed in any publication, in agreement with Regulation (EU) 2016/679 of the European Parliament.
Roles and responsibilities
-
Sponsor: University of Coimbra; contact name: Jaime Batista Santos, PhD, Department of Electrical and Computer Engineering, Faculty of Science and Technology, Pole II of the University of Coimbra, 3030-290, Coimbra, Portugal; phone: +351 239 796 263; and e-mail: jaime@deec.uc.pt
-
Principal investigator: António Casa Nova Tavares Travassos, MD, Coimbra Surgical Centre, Dr. Manuel Campos Pinheiro street, n° 51, São Martinho do Bispo, 3054-089, Coimbra, Portugal
-
Responsible investigator: Luís Miguel da Luz Caixinha Duarte, OD, PhD, University of Beira Interior, Department of Physics, 6291-001 Covilhã, Portugal
The clinical protocol (version n° 3, December 2019) was designed jointly by the sponsor and the principal investigator. The principal investigator and the clinical staff will conduct the participants’ recruitment and interventions in agreement with the protocol. The sponsor is responsible for the experimental device and data analysis. The sponsor will carry out monitoring activities, respond to the competent authorities, elaborate on reports and provide any other required documentation. The responsible investigator will coordinate and verify the correct performance of the clinical study; therefore, there will be no external data monitoring committee.
Discussion
Preclinical studies showed that the experimental device presented positive performance for cataract classification and did not identify potential risks when used within the safety range by trained professionals. The present protocol refers to the first human pilot study of the experimental medical device ESUS. This study aims to evaluate the feasibility and safety of ESUS for quantitative and automatic cataract characterization and OPE estimation in human lenses. It is expected that the obtained results will be used in a larger clinical study to increase the dataset, to improve the performance of the algorithms for automatic classification and to train the algorithms for other causes of cataracts (in addition to age-related cataracts).
Several measures have been taken to minimize bias in the clinical study. The acquisition software was optimized to identify the correct probe positioning, thereby minimizing errors due to misalignment. The cataract group will be limited to age-related cataracts to reduce divergences in clinical conditions that could influence the results. A number of demographic and clinical information from participants will also be analysed for the identification of any additional source of bias.
The clinical study protocol presented here is a key piece of long-term translational research. The quantitative characterization of cataracts and estimation of OPE could significantly reduce postoperative complications and surgical times related to phacoemulsification surgeries, thus providing important social and economic benefits.
Availability of data and materials
Not applicable.
Abbreviations
- CEIC:
-
National Ethical Committee for the Clinical Research
- CRF:
-
Case report form
- ESUS:
-
Eye Scan Ultrasound System
- INFARMED, I.P.:
-
National Authority for Medicaments and Health Products
- IOL:
-
Intraocular lens
- LOCS III:
-
Lens Opacity Classification System III
- OCT:
-
Optical coherence tomography
- OPE:
-
Optimal phacoemulsification energy
- UI:
-
User’s interface
References
Zhao L, Chen XJ, Zhu J, Xi YB, Yang X, Hu LD, et al. Lanosterol reverses protein aggregation in cataracts. Nature. 2015;523(7562):607–11.
Sunkireddy P, Jha SN, Kanwar JR, Yadav SC. Natural antioxidant biomolecules promises future nanomedicine based therapy for cataract. Colloids Surf B: Biointerfaces. 2013;112:554–62.
Silverman R. Focused ultrasound in ophthalmology. Clin Ophthalmol. 2016;10:1865–75.
Thijssen JM. The history of ultrasound techniques in ophthalmology. Ultrasound Med Biol. 1993;19(8):599–618 Available from: https://linkinghub.elsevier.com/retrieve/pii/030156299390068Y.
Coleman DJ, Carlin B. A new system for visual axis measurements in the human eye using ultrasound. Arch Ophthalmol. 1967;77(1):124–7.
Linebarger EJ, Hardten DR, Shah GK, Lindstrom RL. Phacoemulsification and modern cataract surgery. Surv Ophthalmol. 1999;44(2):123–47.
Chan E, Mahroo OAR, Spalton DJ. Complications of cataract surgery. Clin Exp Optom. 2010;93(6):379–89. https://doi.org/10.1111/j.1444-0938.2010.00516.x.
Caixinha M, Jesus DA, Velte E, Santos MJ, Santos JB. Using ultrasound backscattering signals and Nakagami statistical distribution to assess regional cataract hardness. IEEE Trans Biomed Eng. 2014;61(12):2921–9.
Jansson F, Kock E. Determination of the velocity of ultrasound in the human lens and vitreous. Acta Ophthalmol. 1962;40:420–33.
Sugata Y, Murakami K, Ito M, Shiina T, Yamamoto Y. An application of ultrasonic tissue characterization to the diagnosis of cataract. Acta Ophthalmol. 1992;204(2):35–9.
Paunksnis A, Kurapkiene S, Maciulis A, Kopustinskas A, Paunksniene M. Ultrasound quantitative evaluation of human eye cataract. Informatica. 2007;18(2):267–78.
Caixinha M, Amaro J, Santos M, Perdigao F, Gomes M, Santos J. In-vivo automatic nuclear cataract detection and classification in an animal model by ultrasounds. IEEE Trans Biomed Eng. 2016;63(11):2326–35.
Huang CC, Ameri H, DeBoer C, Rowley AP, Xu X, Sun L, et al. Evaluation of lens hardness in cataract surgery using high-frequency ultrasonic parameters in vitro. Ultrasound Med Biol. 2007;33(10):1609–16.
Tabandeh H, Wilkins M, Thompson G, Nassiri D, Karim A. Hardness and ultrasonic characteristics of the human crystalline lens. J Cataract Refract Surg. 2000;26(6):838–41.
Tsui PH, Huang CC, Chang CC, Wang SH, Shung KK. Feasibility study of using high-frequency ultrasonic Nakagami imaging for characterizing the cataract lens in vitro. Phys Med Biol. 2007;52(21):6413–25.
Huang CC, Zhou Q, Ameri H, Wu DW, Sun L, Wang SH, et al. Determining the acoustic properties of the lens using a high-frequency ultrasonic needle transducer. Ultrasound Med Biol. 2007;33(12):1971–7.
Huang C, chung, Chen R, Tsui P hsiang, Zhou Q, Humayun MS, Shung K. Measurements of attenuation coefficient for evaluating the hardness of a cataract lens by a high-frequency ultrasonic needle transducer. Phys Med Biol. 2009;54(19):5981–94.
Tsui PH, Huang CC, Zhou Q, Shung KK. Cataract measurement by estimating the ultrasonic statistical parameter using an ultrasound needle transducer: an in vitro study. Physiol Meas. 2011;32(5):513–22.
Zhou Z, Huang CC, Shung KK, Tsui PH, Fang J, Ma HY, et al. Entropic imaging of cataract lens: an in vitro study. PLoS One. 2014;9(4):e96195.
Caixinha M, Santos M, Santos J. Automatic cataract hardness classification ex vivo by ultrasound techniques. Ultrasound Med Biol. 2016;42(4):989–98.
de Korte CL, van der Steen AFW, Thijssen JM. Acoustic velocity and attenuation of eye tissues at 20 MHz. Ultrasound Med Biol. 1994;20(5):471–80 Available from: https://linkinghub.elsevier.com/retrieve/pii/0301562994901023.
Santos J, Gomes M, Santos M, Perdigão F, Morgado M, Caixinha M, et al. Sistema ultrassônico de exame ocular para deteção precoce e classificação da catarata em tempo real. Portugal; PT109646B. 2019.
Petrella L, Gomes M, Perdigão F, Santos M, Fernandes P, Pinto C, et al. Eye Scan Ultrasound System for automatic cataract detection: from a preclinical to a clinical prototype. In: Medicon [Internet]. Vol. 1. Coimbra: Springer; 2020. p. 811–9. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/978-3-030-31635-8_97.
Chylack LT, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, et al. The lens opacities classification system III. Arch Ophthalmol. 1993;111:831–6.
Abdelkader H, Alany RG, Pierscionek B. Age-related cataract and drug therapy: opportunities and challenges for topical antioxidant delivery to the lens. J Pharm Pharmacol. 2015;67(4):537–50.
Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. 2016;24:i5239.
Thabane L, Lancaster G. A guide to the reporting of protocols of pilot and feasibility trials. Pilot Feasibility Stud. 2019;5(1):37.
Lancaster GA, Thabane L. Guidelines for reporting non-randomised pilot and feasibility studies. Pilot Feasibility Stud. 2019;5(1):114.
Billingham SA, Whitehead AL, Julious SA. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med Res Methodol. 2013;13(1).
Petrella L, Fernandes P, Santos M, Caixinha M, Nunes S, Pinto C, et al. Safety assessment of an A-scan ultrasonic system for ophthalmic use. J Ultrasound Med. 2020;39(11):2143–50 Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/jum.15323.
ISO. DIN EN ISO 14971:2007 Medical devices - application of risk management to medical devices. International Organization for Standarization; 2007.
IEC. IEC 60601-2-37, Medical electrical equipment – Part 2-37: particular requirements for the basic safety and essential performance of ultrasonic medical diagnostic and monitoring equipment. Geneva: International Electrotechnical Commission; 2007.
IEC. IEC 62127-1 ultrasonics - hydrophones - part 1: measurement and characterization of medical ultrasonic fields up to 40 MHz. Geneva: International Electrotechnical Commission; 2007.
IEC. IEC 62359 ultrasonics - field characterization - test methods for the determination of thermal and mechanical indices related to medical diagnostic ultrasonic fields. Geneva: International Electrotechnical Commission; 2017.
Acknowledgements
Not applicable.
Funding
This research is sponsored by the FCT - Fundação para a Ciência e a Tecnologia, I.P./MCTES though national funds and when applicable cofounded by FEDER – PT2020 within the scope of the project PTDC/SAU-SER/28758/2017, and of R&D units UIDB/00285/2020, UIDB/50008/2020, UIDP/50008/2020 and UIDP/00326/2020. The funding sources had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results.
Author information
Authors and Affiliations
Contributions
LP, safety considerations, study design and manuscript writing; SN, study design and manuscript revision; FP, experimental medical device development and safety considerations; MG, experimental medical device development and safety considerations; MS, experimental medical device development and safety considerations; CP, experimental medical device development; MM, manuscript revision; AT, study design and manuscript revision; JS, experimental medical device development and study design; MC, experimental medical device development, study design and manuscript revision. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the INFARMED, I.P. (Process N° EC/010/2019), the CEIC (Process N° PPF 2001HQ023) and the independent Ethical Committee of the Coimbra Surgical Centre. Together with the medical investigator, participants (or their representatives) should read and assign an informed consent form for their inclusion in the clinical trial.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Petrella, L., Nunes, S., Perdigão, F. et al. Feasibility assessment of the Eye Scan Ultrasound System for cataract characterization and optimal phacoemulsification energy estimation: protocol for a pilot, nonblinded and monocentre study. Pilot Feasibility Stud 8, 219 (2022). https://doi.org/10.1186/s40814-022-01173-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40814-022-01173-2