Abstract
Introduction
Accessory spleen, also known as supernumerary spleen or splenunculum, is a congenital anomaly of the spleen due to a fusion defect during the embryogenesis. Usually it is detected casually during an ultrasound (US) examination of the abdomen and it is asymptomatic.
Case report: results
We present a case of a 12 years old male patient, with 2-days history of left abdominal pain, without fever, gastrointestinal or genitourinary symptoms. The day before our observation, the patient had gone to another hospital, from where he had been discharged with medical analgesic therapy, without any benefit. Blood tests were normal, the Ultrasound abdominal examination showed normal aspect of abdominal organs, but the presence in the left side of a small round parenchymal structure surrounded by hyperechogenic mesenteric fat. We interpreted this image as an accessory spleen, complicated by torsion. As the torsion of accessory spleen is a quite rare occurrence, we carried out a contrast enhanced ultrasound (CEUS) to get more information. CEUS showed the absence of enhancement of the nodular formation, suggestive for a complete lack of vascularization; the spleen was normally enhanced. While the management in case of accessory spleen torsion is non-operative, in this case the patient underwent surgical exploration, due to the persistence of abdominal pain despite the medical therapy, with clinical signs of peritoneal reaction, mimicking an acute abdomen. Surgery confirmed the diagnosis of accessory spleen torsion.
Discussion and conclusions
In conclusion, US is the first diagnostic tool in pediatric abdominal pain and allows to direct the diagnosis; the use of CEUS helps to clarify the US reports, without leaving doubts about the parenchymal vascularization of the abdominal organ involved.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Accessory spleen is not rare this is found commonly in 10–30% of the population. It consists of one or more (from one to six) small round or oval masses of ectopic splenic tissue, separated from the main body of the spleen. This condition is frequently asymptomatic [1,2,3]. During the fifth week of embryogenesis the spleen arises, it is divided into several parts that normally merge before birth. The incomplete or missing fusion may lead to some congenital splenic variations among which accessory spleens [1, 4]. The sizes of the ectopic splenic tissue vary from few millimeters to several centimeters; even the location is variable, the most frequent is close to the splenic hilum (75%), but there are many others locations: about 20% are adjacent to the pancreatic tail, the remaining 5% occur along the splenic artery, and in the gastrosplenic, splenocolic, or gastrocolic ligament [1, 2, 5, 6]. Accessory spleen is important in all patients who have undergone splenectomy for various causes such as hematological diseases or trauma: in these patients the ectopic splenic tissue increases in size for compensatory hypertrophy [1, 7].
Case report
We present the case of a 12-year-old male who presented to Emergency Department after 2 days of left upper quadrant acute abdominal pain without fever or gastrointestinal or urinary symptoms. He had already been visited in another hospital the day before, being discharged only with analgesic therapy. The blood tests were normal. The patient was submitted to an ultrasound (US) exam of the abdomen, which demonstrated a small round soft tissue close to the spleen, surrounded by strongly hyperechogenic mesenteric tissue. The US image was not of univocal meaning, however, the radiologist made the hypothesis of an accessory spleen twisting. To support this thesis, a contrast enhanced ultrasound (CEUS) was carried out. CEUS demonstrated the complete lack of vascularization of the tissue. Given the persistence of the symptoms, and the appearance of clinical signs of peritoneal reaction, the patient underwent laparoscopic surgery, which revealed a twisted accessory spleen. The treatment was the surgical resection.
Results
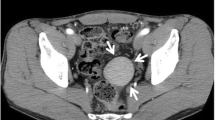
The US evaluation of the patient was performed with both a convex probe and a linear probe, to obtain both a more panoramic and detailed view. At the US all the abdominal parenchymal organs were normal in size and structure. The small rounded parenchymal nodule, which showed regular margins, size about 16 mm, was located close to the lower pole of the spleen and had the same echostructure of the spleen, slightly more inhomogeneous and hypoechoic in the central portion. The vascular pedicle of the accessory spleen was not recognizable at B-mode US and at color Doppler exploration. The surrounding mesenteric fat was very echogenic; there was no free fluid (Fig. 1a–d). At the CEUS evaluation the splenic parenchyma enhanced homogeneously while the small accessory spleen showed no enhancement at all phases of the examination. This lack of contrast enhancement is typical of non-vascularized tissues and confirmed the hypothesis of accessory spleen torsion (Fig. 2a, b). For the persistence of acute pain that did not pass despite medical therapy, considered the ultrasound and CEUS findings, the patient underwent surgical intervention that confirmed the torsion of accessory spleen with parenchymal necrosis (Fig. 3). The result at pathology exam it was of an ischemic splenic nodule Discussion The detection of one or more accessory spleens is usually incidental, because the presence of ectopic splenic tissue is often asymptomatic [3]. Torsion of accessory spleen is a rare cause of acute abdomen in pediatric patients; it may present as an acute pain in the left flank or as an intermittent pain. The vascularization of the ectopic tissue is supplied by arterial branches arising from the splenic artery [8]. When the vascular supply is compromised due to the torsion, the pain is very intense and the organ goes into ischemia. In this case, a conservative approach can be attempted; otherwise the therapy is the surgical removal of the accessory spleen. Risks for torsion are unknown; there is no association between torsion and location or size of the ectopic tissue, and patient age at the time of diagnosis [8, 9]. In our case the patient had only acute left flank pain but the symptoms can also include vomiting, nausea, fever, leukocytosis, and peritoneal signs mimicking an acute abdomen [2, 6, 10]. In the pediatric patient, diagnostic imaging must consider radioprotection problems; it is mandatory to choose, when possible, the use of a technique that does not use ionizing radiations. Therefore, US examination is usually used as a first evaluation in the pediatric patient with abdominal pain US is a fast noninvasive imaging technique, widely available, well accepted by the young patient and parents, free from contraindications. In our case the initial US examination gave the possibility to suspect a pathology of the accessory spleen, due to the mild inhomogeneity of the parenchyma and, above all, to the altered appearance of the surrounding mesenteric fat. However, in some cases the US evaluation of increased echogenicity of fatty mesenteric tissue may be difficult to appreciate, whereas increased density and stranding of mesenteric fat can be quite easily and definitely demonstrated by CT. The use of CEUS in children, first reported in 2002, has been approved in the United States by the Food and Drug Administration (FDA) for characterizing focal liver lesions and vesico-ureteral reflux in adult and pediatric patients. Currently in Europe, CEUS in children is mostly “off-label” use, as many drugs, which are used off-label in pediatric patients; nowadays its use for the evaluation of vesico-ureteral reflux is accepted in Europe [11,12,13]. However, its use, and its safety, have now been proven by numerous studies [14,15,16]; it has been proven that with the CEUS we can perform accurate diagnostic exam, in many cases, especially in pediatric patients, also comparable and sometimes superior to the performance of computed tomography (CT) and magnetic resonance imaging (MRI) [17,18,19,20,21]. CT and MRI, however, can provide different information: MRI is superior to US in identifying hemorrhagic areas in the infarcted spleen, while CT is better in demonstrating the twisting of the vascular pedicle. We must consider that to undergo the CEUS examination, no laboratory tests are required, no sedation is needed and it can be done next in the presence of child parents, thus obtaining full cooperation from the pediatric patient. The ultrasound contrast agent is composed of microbubbles of an inert gas: sulphur hexafluoride, enclosed by a membrane (SonoVue™/Lumason™, Bracco SpA, Milan, Italy), as with any contrast study it is necessary to obtain informed consent from the patient’s parents. In our case, the use of CEUS has allowed us to highlight, without any doubt, the lack of vascular supply of the accessory spleen, which in fact did not show any enhancement; therefore, in this case it was not necessary to complete the diagnostic examination with contrast-enhanced computed tomography (CE-CT), although in many other cases it may be essential to carry out a more panoramic technique, such as CT or MR, to confirm the diagnosis before submitting the patient to surgery.
a Ultrasound detects the accessory spleen, close to the lower pole of the spleen. b, c US details: note the inhomogeneous structure with hypoechoic central portion (calipers) and the hyperechogenicity of the surrounding mesenteric fat (white arrows). d, US scan, obtained with linear probe, confirms the hypoechoic structure. There is no evidence of vascular flow in the color Doppler examination
Conclusions
The proven diagnostic accuracy of CEUS in highlighting parenchymal vascularization places it as a valid alternative to CE-CT in all cases of acute abdomen, where simple B-mode non-enhanced US is not conclusive and a vascular pathology is suspected. The lower costs compared to the CT/MRI examinations, the greater diffusion of the ultrasound equipment and the short time required to perform the exam make CEUS a suitable method for the evaluation of the acute abdominal pathology in pediatric patient in emergency department.
References
Di Serafino M, Verde F, Ferro F et al (2018) Ultrasonography of the pediatric spleen: a pictorial essay. J Ultrasound. https://doi.org/10.1007/s40477-018-0341-2
Landmann A, Johnson JJ, Webb KM et al (2016) Accessory spleen presenting as acute abdomen: a case report and operative management. J Pediatr Surg Case Rep 12:9–10. https://doi.org/10.1016/j.epsc.2016.05.011
Ishibashi H, Oshio T, Sogami T et al (2012) Torsion of an accessory spleen with situs inversus in a child. J Med Investig 59:220–223
Gayer G, Hertz M, Strauss S et al (2006) Congenital anomalies of the spleen. Semin Ultrasound CT MR 27:358–369. https://doi.org/10.1053/j.sult.2006.06.002
Paterson A, Frush DP, Donnelly LF et al (1999) A pattern-oriented approach to splenic imaging in infants and children. Radiographics 19:1465–1485. https://doi.org/10.1148/radiographics.19.6.g99no231465
Babcock TL, Coker DD, Haynes JL et al (1974) Infarction of an accessory spleen causing an acute abdomen. Am J Surg 127:336–337
Back SJ, Maya CL, Khwaja A (2017) Ultrasound of congenital and inherited disorders of the pediatric hepatobiliary system, pancreas and spleen. Pediatr Radiol 47:1069–1078. https://doi.org/10.1007/s00247-017-3869-y
Ozeki M, Asakuma M, Go N et al (2015) Torsion of an accessory spleen: a rare case preoperatively diagnosed and cured by single-port surgery. Surg Case Rep 1:100. https://doi.org/10.1186/s40792-015-0101-x
Bard V, Goldberg N, Kashtan H (2014) Torsion of a huge accessory spleen in a 20-year-old patient. Int J Surg Case Rep 5:67–69
Di Giacomo V, Trinci M, Van der Byl G (2015) Ultrasound in newborns and children suffering from non-traumatic acute abdominal pain: imaging with clinical and surgical correlation. J Ultrasound 18:385–393. https://doi.org/10.1007/s40477-014-0087-4
Dietrich CF, Averkiou M, Nielsen MB et al (2018) How to perform contrast-enhanced ultrasound (CEUS). Ultrasound Int Open 4:E2–E15. https://doi.org/10.1055/s-0043-123931
Schreiber-Dietrich DG, Cui XW, Piscaglia F et al (2014) Contrast enhanced ultrasound in pediatric patients: a real challenge. Z Gastroenterol 52:1178–1184. https://doi.org/10.1055/s-0034-1366766
Chiorean L, Cui XW, Tannapfel A et al (2015) Benign liver tumors in pediatric patients—review with emphasis on imaging features. World J Gastroenterol 21:8541–8561. https://doi.org/10.3748/wjg.v21.i28.8541
Riccabona M (2012) Application of a second-generation US contrast agent in infants and children—a European questionnaire-based survey. Pediatr Radiol 42:1471–1480. https://doi.org/10.1007/s00247-012-2472-5
Menichini G, Sessa B, Trinci M et al (2015) Accuracy of contrast-enhanced ultrasound (CEUS) in the identification and characterization of traumatic solid organ lesions in children: a retrospective comparison with baseline US and CE-MDCT. Radiol Med 120:989–1001. https://doi.org/10.1007/s11547-015-0535-z
Miele V, Piccolo CL, Trinci M et al (2016) Diagnostic imaging of blunt abdominal trauma in pediatric patients. Radiol Med 121:409–430. https://doi.org/10.1007/s11547-016-0637-2
Rafaelsen SR, Jakobsen A (2011) Contrast-enhanced ultrasound vs multidetector computed tomography for detecting liver metastases in colorectal cancer: a prospective, blinded, patient-by-patient analysis. Colorectal Dis 13:420–425. https://doi.org/10.1111/j.1463-1318.2010.02288.x
Bernatik T, Schuler A, Kunze G et al (2015) Benefit of Contrast-Enhanced Ultrasound (CEUS) in the follow-up care of patients with colon cancer: a prospective multicenter study. Ultraschall Med 36:590–593. https://doi.org/10.1055/s-0041-107833
Miele V, Piccolo CL, Sessa B et al (2016) Comparison between MRI and CEUS in the follow-up of patients with blunt abdominal trauma managed conservatively. Radiol Med 121:27–37. https://doi.org/10.1007/s11547-015-0578-1
Piccolo CL, Trinci M, Pinto A et al (2018) Role of contrast-enhanced ultrasound (CEUS) in the diagnosis and management of traumatic splenic injuries. J Ultrasound 21:315–327. https://doi.org/10.1007/s40477-018-0327-0
Dietrich CF, Kratzer W, Strobe D et al (2006) Assessment of metastatic liver disease in patients with primary extrahepatic tumors by contrast-enhanced sonography versus CT and MRI. World J Gastroenterol 12:1699–1705. https://doi.org/10.3748/wjg.v12.i11.1699
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interests associated with this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Trinci, M., Ianniello, S., Galluzzo, M. et al. A rare case of accessory spleen torsion in a child diagnosed by ultrasound (US) and contrast-enhanced ultrasound (CEUS). J Ultrasound 22, 99–102 (2019). https://doi.org/10.1007/s40477-019-00359-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-019-00359-4