Abstract
Introduction
Localized low-energy abdominal trauma is very frequent in the pediatric population. The findings of several studies have shown that ultrasonography (US) can represent a useful and cost-effective tool in the evaluation of blunt abdominal trauma both in adults and children. However, many parenchymal injuries are not correctly visualized at baseline US examination. The introduction of specific US contrast agents contrast-enhanced ultrasound (CEUS) has enabled a better identification of traumatic organ injuries. The correct use of CEUS could therefore identify and select the children who need further diagnostic investigation computed tomography (CT), avoiding unnecessary radiation and iodinated contrast medium exposure. The purpose of our study was to assess the sensibility and feasibility of CEUS in the assessment of low-energy abdominal trauma compared to baseline US in pediatric patients, using contrast-enhanced MDCT as the reference standard.
Materials and methods
We retrospectively reviewed 73 children (51 M and 22 F; mean age 8.7 ± 2.8 years) who presented in our Emergency Department between October 2012 and October 2013, with history of minor abdominal trauma according to the Abbreviated Injury Scale and who underwent US, CEUS, and CE-MDCT. Inclusion criteria were: male or female, aged 0–16, hemodynamically stable patients with a history of minor blunt abdominal trauma. Exclusion criteria were adulthood, hemodynamical instability, history of major trauma. Sensitivity, specificity, PPV, NPV, and accuracy were determined for US and CEUS compared to MDCT.
Results
6/73 patients were negative at US, CEUS, and MDCT for the presence of organ injuries. In the remaining 67 patients, US depicted 26/67 parenchymal lesions. CEUS identified 67/67 patients (67/67) with parenchymal lesions: 21 lesions of the liver (28.8 %), 26 lesions of the spleen (35.6 %), 7 lesions of right kidney (9.6 %), 13 lesions of left kidney. MDCT confirmed all parenchymal lesions (67/67). Thus, the diagnostic performance of CEUS was better than that of US, as sensitivity, specificity, PPV, NPV, and accuracy were 100, 100, 100, 100, and 100 % for CEUS and 38.8, 100, 100, 12.8, and 44 % for US. In some patients CEUS identified also prognostic factors as parenchymal active bleeding in 8 cases, partial devascularization in 1 case; no cases of vascular bleeding, no cases of urinoma. MDCT confirmed all parenchymal lesions. Parenchymal active bleeding was identified in 16 cases, vascular bleeding in 2 cases, urinoma in 2 cases, partial devascularization in 1 case.
Conclusions
CEUS is more sensitive and accurate than baseline US and almost as sensitive as CT in the identification and characterization of solid organs lesions in blunt abdominal trauma. CT is more sensitive and accurate than CEUS in identifying prognostic indicators, as active bleeding and urinoma. CEUS should be considered as a useful tool in the assessment and monitoring of blunt abdominal trauma in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Localized low-energy abdominal trauma is very frequent in the pediatric population as it can easily happen during the child normal daily activities (scholastic or sportive accident, recreational activities, etc.).
The findings of several studies have shown that ultrasonography (US) can represent a useful and cost-effective tool in the evaluation of blunt abdominal trauma both in adults [1–3] and children [4–7]. Nowadays, this modality is widely accepted in Europe and is becoming part for the triage of blunt abdominal trauma patients also in the United States [8].
However, many parenchymal injuries are not correctly visualized at baseline US examination and, moreover, the absence of peritoneal free fluid does not enable serious organ lesions to be excluded [9, 10]: some researchers have reported that 29–34 % of solid organ lesions can occur in trauma patients without hemoperitoneum [11, 12].
CT therefore remains the radiologic standard for evaluating patients with abdominal trauma [13]. The introduction of specific US contrast agents has enabled a better identification of traumatic organ injuries at US examination [14–19]. The correct use of contrast-enhanced ultrasound (CEUS) in the triage of pediatric patients with history of blunt abdominal trauma could therefore identify and select the children who need further diagnostic investigation (CT), avoiding unnecessary radiation and iodinated contrast-medium exposure.
This last consideration is even more important if we take into account the pediatric population.
Thus, the purpose of our study was to assess the sensibility and reproducibility of CEUS in the assessment of low-energy abdominal trauma compared to baseline US in pediatric patients, using contrast-enhanced MDCT as the reference standard.
Materials and methods
This study was conducted at a large Italian Hospital in Rome that serves as a regional center for trauma patients.
We performed a retrospective case-series study that included a total of 73 consecutive pediatric patients (51M and 22F; mean age 8.7 ± 2.8 years) who arrived in our Emergency Department with a history of minor blunt abdominal trauma between October 2012 and October 2013 with these inclusion criteria: male or female, aged 0–16, hemodynamically stable patients with a history of minor blunt abdominal trauma.
Exclusion criteria were adulthood, hemodynamical instability, and history of major trauma. According to the ATLS Guidelines [20] a major trauma is defined basing both on clinical (Table 1) and dynamic criteria (Table 2); all the patients who are not classified as major traumatic patient could be identified as patient with history of minor trauma or low-energy abdominal trauma.
Patients with hemoperitoneum at US examination but with unstable vital signs were immediately referred to surgery and therefore were excluded from the study, as already declared.
Patients with negative US findings were also excluded,were submitted to 24 h clinical observation and then discharged without further abdominal imaging.
The remaining 73 patients, who had a history of minor trauma, hemodynamic stability and at least one positive finding at baseline US, such as abdominal free fluid, perirenal fluid collection, signs of hepatic, splenic, or renal injury, were subjected both to CEUS and CE-MDCT.
Written informed consent from parents was always obtained, including the information that the use of contrast medium that is used is not recommended for children. In the 73 patients included in the study, the mechanism of trauma was fall from bicycle in 17/73 cases (23.3 %), sports in 20/73 (27.3 %), scholastic activity in 12/73 (16.5 %), car accident as passenger in 10/73 (13.7 %) and as pedestrian in 6/73 (8.2 %), and miscellaneous other causes in 8/73 (11 %).
Vital sign recording, laboratory tests, and baseline US to detect free abdominal fluid as a routine minor trauma protocol were performed.
US, CEUS, and CT were performed and interpreted by three different radiologists (R1, R2, and R3) interchanged throughout the different patients included and with at least 10 years of experience in the Emergency Department (R1, 25 years of experience, R2, 15 years of experience; R3, 10 years of experience), blinded to the results of the other examinations.
The US examination was performed using a Acuson Sequoia 512 Ultrasound System (Siemens, Germany), equipped with both curved- and linear-array probes. The study was conducted to detect the presence of free intraperitoneal fluid in the perihepatic area, the Morrison pouch, the epigastric region, the perisplenic region, the paracolic gutters, and the Douglas pouch and the presence of perirenal fluid collection. Intraabdominal organs were specifically evaluated for evidence of injury.
CEUS was performed immediately after baseline US.
Adequate ultrasound technology consisting of a contrast-specific software which operates in real-time at a low mechanical index (pulse inversion technology) was applied. Two 1.2 ml bolus of second-generation blood pool contrast agent (Sonovue, Bracco, Italy), were administered through a 20-gage catheter placed in antecubital vein, followed by saline (0.9 % NaCl). An abdominal scanning of 3 consecutive minutes was performed for each bolus, starting from the right and left kidney, liver and pancreas; last, the spleen.
A traumatic lesion was identified as the presence of an hypoechoic area which persisted unchanged during all the acquisition phases, with a subcapsular distribution in the case of hematoma or a parenchymal localization in the case of lacerations. The presence of intralesional hyperechoic spots was interpreted as a sign of active bleeding.
Biphasic CE-MDCT examination was performed using a MDCT 16 scanner (LightSpeed 16—GE Healthcare, USA). The scanning parameters were as follows: 100–250 mAs (applied with the care-dose technique and with a medium value of 115 mAs), 100–120 kV (according to body habitus), 2.5 mm collimation, 13,5 mm/s table, and 1 mm reconstruction interval.
A dose of 2.5 ml/kg of non-ionic contrast agent (Xenetix 350, Guerbet, France) was injected at a rate of 1.5–2 ml/s. Arterial phase is performed with an acquisition delay of 40 s; a venous phase is routinely performed with 70 s delay; late phase (5 min) was performed only in case of suspected urinary tract lesion.
The presence of a parenchymal bleeding was defined as the presence of hyperechoic/hyperdense post-contrast intralesional spots.
At MDCT, vascular bleeding was stated if hemoperitoneum with an evident active extravasation was identified.
The main vital sign and liver and kidney laboratory tests were recorded for 24 h to evaluate any adverse effect due to contrast medium administration.
Sensitivity, specificity, and positive and negative predictive values were determined for US and CEUS compared to MDCT, considered as the reference standard.
Results
On baseline US, 6/73 patients (8.2 %) (5F; 1M) showed the presence of free intraperitoneal fluid, but were negative at US, CEUS, and MDCT examination for the presence of organ injuries; these patients were considered to have free intraperitoneal fluid for gynecological causes (n = 3), gastroenteritis (n = 2), miscellaneous (n = 1).
In the remaining 67 patients, baseline US depicted 26/67 parenchymal lesions (38 %), defined as a inhomogeneous hyper or hypoechoic area in a solid organ or a distortion of the normal echostructure. Baseline US did not detect any case of parenchymal active bleedings, vascular bleeding, and urinomas.
On CEUS examination, organ injuries appeared as strongly hypoechoic areas with or without interruption of the anatomic profile. Microbubbles within the lesion were considered as a sign of parenchymal active bleeding.
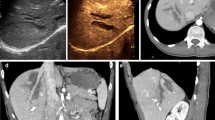
CEUS identified 67/67 patients (67/67) with parenchymal lesions (Table 3): 21 lesions of the liver (28.8 %) (Fig. 1), 26 lesions of the spleen (35.6 %) (Fig. 2), 7 lesions of right kidney (9.6 %) (Fig. 3), and 13 lesions of left kidney (17.8 %).
12-year-old girl admitted to the hospital after a fall from horse during riding. a Baseline US shows a diffuse inhomogeneity within the right hepatic lobe (white arrows). b At CEUS examination is clearly visible a well-defined hypoechoic lesion (white arrows) classified as IV grade (AAST classification). (c, d) Axial and coronal MDCT images that confirm the CEUS findings
Splenic laceration in 9-year-old child who beated the left flank against the school desk (a) longitudinal scanning at baseline US shows normal findings. b At CEUS examination is clearly visible a splenic laceration with associated hemoperitoneum c (white arrows), findings subsequently confirmed at MDCT (d, e)
II grade renal injury in a 9-year-old girl. a At baseline US is visible a mild hyperechoic area within the middle-third of the right kidney, without evidence of renal fracture (white arrow). b CEUS examination shows a linear renal fracture not <1 cm parenchymal depth in renal cortex (white arrow) with associated perirenal hematoma (arrowhead), II grade renal injury, confirmed at MDCT (c)
In 9 patients CEUS identified also prognostic indicators: 8 cases of parenchymal active bleeding (53.3 %) (Fig. 4), 1 case of partial devascularization (Fig. 5), no cases of vascular bleeding, no cases of urinoma (Table 4).
9-year-old-boy with history of sportive accident. a At baseline US is appreciable only a mild inhomogeneity of the IV hepatic segment without a clearly visible lesion (white arrows). b Transverse contrast-enhanced sonogram shows a well-defined hepatic laceration (white arrow) with evidence of microbubbles within the lesion (white arrowhead), interpreted as a sign of parenchymal active bleeding, subsequently confirmed at MDCT examination (c, d) (black arrowheads)
10-year-old boy, who fell in the pool, beating the left flank. Baseline US (a) shows swelling and echostructural inhomogeneity of the lower pole of the spleen (white arrow). CEUS shows a large triangular-shaped hypoechoic area at the lower pole of the spleen (white arrow), interpreted as an area of devascularization. Axial and coronal MDCT views (c, d), confirm the triangular-shaped area of devascularization at the lower pole of the spleen
MDCT confirmed all parenchymal lesions (67/67), 21 lesions of the liver, 26 lesions of the spleen, 7 lesions of right kidney, 13 lesions of left kidney, Parenchymal active bleeding was identified in 16 cases (Fig. 6), partial devascularisation in 1 case (Fig. 5), vascular bleeding in 2 cases, urinoma in 2 cases (Fig. 7).
Renal injury in 12-year-old girl with history of bicycle accident. a Baseline US shows a mild hyperechoic area in the middle-third of the right kidney. b Longitudinal and transverse c CEUS images of the same patients in which it is evident a renal fracture with an associated perirenal collection (arrowhead) and evidence of hyperechoic spots within it (white arrow) that at a subsequent angiography examination showed to be an active bleeding from a segmental renal artery and not extravasation from the urinary system. d, e MDCT urographic-phase: the perirenal collection showed to be a perirenal hematoma with evidence of active bleeding (white arrow); a clot is visible in the right urinary system (black arrowhead)
Renal injury in a 10-year-old girl after a bicycle accident. a Longitudinal baseline US of the right kidney with no relevant traumatic findings. b, c CEUS shows a well-defined renal fracture and the presence of a perirenal collection that seems to be a perirenal hematoma (white arrows). d MDCT examination (courtesy of prof. G. Gualdi, Sapienza University of Rome-Italy) confirms the renal injury; in the delayed phase, performed 5 min after contrast medium administration e, f the perirenal collection turns out to be a urinoma with evidence of opacified urine leakage
Using CT as the reference standard, baseline US missed 41 (62 %) parenchymal lesions and all cases of parenchymal or vascular active bleeding, urinomas and devascularization. CEUS identified all parenchymal lesions (100 %), 8/16 parenchymal active bleeding (50 %), 1/1 partial devascularization, 0/2 vascular bleeding, 0/2 urinomas.
Thus, in the evaluation of parenchymal lesions the diagnostic performance of CEUS was much better than that of US, as sensitivity, specificity, PPV, NPV, and accuracy in the evaluation of parenchymal lesions were, respectively, 100, 100, 100, 100, and 100 % for CEUS and 38.8, 100, 100, 12.8, and 44 % for US (Table 5).
No adverse effects were observed for both CEUS and CE-MDCT.
Discussion
CE-MDCT is the most used and sensitive imaging modality in traumatic lesion assessment. It is able to depict both parenchymal and vascular lesions (including active bleeding) which are the major predictors of nonsurgical management [21–23].
Baseline US has a low sensitivity in the detection of parenchymal lesions and, as hemoperitoneum is not always present in patients with solid organ injuries, it is not reliable in the exclusion of traumatic abdominal lesions [24–26]. Poletti PA et al. [27] found that up to 31 % of CT-proved intra-abdominal injuries do not have associated free fluid and that US has a very low sensitivity in directly demonstrating organ injuries, especially splenic lacerations, even with optimal condition of use. This consideration is disappointing, if we consider the fact that trauma to the splenic parenchyma can result in massive and unpredictable delayed bleeding [28–31].
Regarding pediatric population, Emery et al. [32] found that 34 % of US negative examination children had an intra-abdominal injury at CT and so reached the conclusion that screening US for the depiction of blunt abdominal trauma should be approached with caution.
In our population, we found that the presence of free intraperitoneal fluid is not always due to traumatic causes: in the 8.2 % of cases it was related to other different causes—gynecological (50 %), gastroenteritis (33.3 %), miscellaneous (16.7 %)—and it should not be considered a reliable specific indirect sign of organ traumatic injuries.
The introduction of US contrast agents has led to an increase in the diagnostic accuracy of US in many organs and many studies conducted to assess trauma in adults have showed that its sensitivity is almost the same as that of CE-MDCT [13, 28]. Few studies exist on the use of CEUS in childhood [33], because the use of ultrasound contrast agents in children has not been officially approved since these contrast media are not licensed for pediatric use. However, a large survey study were carried out, which also included the use of product in intravenous route: responses suggest a favorable safety profile of this second-generation ultrasound contrast agents in children and also demonstrate a demand for such contrast agents from pediatric radiologists [34].
CEUS allows to demonstrate lesions even in places of difficult exploration with US, such as the upper pole of the spleen, whose study is often made difficult from the air of the pulmonary basis (Fig. 8).
At baseline US traumatic lesions appear as mild and irregular hyperechoic areas. During the CEUS examination, organ injuries appear as strongly hypoechoic areas compared to the homogeneous echogenicity of the surrounding parenchyma (Figs. 2, 9).
9-year-old boy, domestic accident (a) Baseline US shows only a mild and irregular hyperechoic areas within the right hepatic lobe (white arrows). b At CEUS examination, the traumatic lesion appear as a strongly hypoechoic area (white arrows) that can be classified as a IV grade lesion according to the AAST classification. c, d Axial and coronal MDCT views confirm the findings
In our study, we were able to correctly identify at CEUS examination 100 % of solid organ lesions, with great accuracy in defining also the extension of the lesions compared to CE-MDCT.
In fact, the capability of contrast-enhanced US of correctly identify the extension of the traumatic lesion can be considered a very useful tool not only in the injury detection but also in the traumatic lesion grading and classification.
The sensitivity, NPV, and accuracy were significantly higher than those of baseline US, with good agreement with CT findings.
In particular, considering the high NPV obtained in our study (100 %), we can be pretty sure that a patient with CEUS negative findings does not have solid organ traumatic injuries and therefore should not perform a CE-MDCT examination but could be safely clinically observed.
According to these results, we propose the use of CEUS examination as the first line approach in children with history of minor blunt abdominal trauma (Table 6).
In particular, according to our results, in case of CEUS negative findings, the patients could be discharged home and eventually followed-up with another CEUS examination after 7 days and phone-interviews up to 30 days. In case of positive-CEUS findings the patient should undergo a CE-MDCT examination in order to confirm the traumatic lesions and to assess the presence of negative prognostic factors as active bleeding and urinomas [35, 36].
The poor ability to detect active bleeding and urinomas is the largest limit of CEUS in the blunt abdominal trauma examination.
Regarding urinomas, we can say that US contrast agents are intravascular and are unsuitable for demonstrating extravasation in the renal collecting system (Fig. 7).
As concern the active bleeding, we must differentiate between parenchymal and vascular bleeding: we were able to correctly identify only 50 % of parenchymal bleeding (8/16) and no cases of vascular bleeding (0/2). However, in these last cases, both US and CEUS identified massive hemoperitoneum which represents an indirect sign of severe abdominal organ injury and put the clinical indication to perform a CT.
Another significant limitation is that CEUS can not detect direct signs of peritoneal bleeding due to injuries of the intestine and mesentery. However, should be considered that these lesions, unlike those of solid organs that are the object of the present work, occur more frequently in high-energy trauma, rather than in the minor trauma. Moreover, both baseline ultrasound and CEUS are able to detect the presence of free fluid in the peritoneal cavity, thus placing the suspected diagnosis of a traumatic injury.
Conclusions
In conclusion, our findings show that CEUS in children is more sensitive and accurate than baseline US and almost as sensitive as CT in the identification and characterization of blunt abdominal trauma. These results are in agreement with the experience of Valentino et al. [33] who suggest that CEUS can be considered for the triage of hemodynamically stable children with history of abdominal trauma.
CT is more sensitive and accurate than CEUS in identifying prognostic indicators, as active bleeding and urinoma.
Moreover, CEUS can be performed at the patient’s bedside, without moving the traumatized child to the CT section, representing a useful alternative to CT also in the follow-up of hospitalized children with a known abdominal injury [37].
Finally, but not less important, no sedation is needed to perform CEUS examination, avoiding the possibility of inducing a hypotension crisis in the little traumatized patient.
According to ALARA’s criteria, our data suggest that CEUS should be considered as a useful and cost-effective tool in the assessment and monitoring of blunt abdominal trauma in children.
References
Boulanger BR, Kearney PA, Brenneman FD, Tsuei B, Ochoa J (2000) Utilization of FAST (Focused Assessment with Sonography for Trauma) in 1999: results of a survey of North American Trauma Centers. Am Surg 66:1049–1055
Nural MS, Yardan T, Guven H, Baydin A, Bayrak IK, Kati C (2005) Diagnostic value of ultrasonography in the evaluation of blunt abdominal trauma. Diagn Interv Radiol 11:41–44
Lingawi SS, Buckley AR (2000) Focused abdominal US in patients with trauma. Radiology 217:426–429
Richards JR, Knopf NA, Wang L, Mc Gahan JP (2002) Blunt abdominal trauma in children: evaluation with emergency US. Radiology 222:749–754
Soudack M, Epelman M, Maor L et al (2004) Experience with focused abdominal sonography for trauma (FAST) in 313 pediatric patients. J Clin Ultrasound 32:53–61
Tas F, Ceran C, Atalar MH, Bulut S, Selbes B, Isik AO (2004) The efficacy of ultrasonography in hemodynamically stable children with blunt abdominal trauma: a prospective comparison with computed tomography. Eur J Radiol 51:91–96
Miele V, Di Giampietro I, Ianniello S, Pinto F, Trinci M (2015) Diagnostic Imaging in pediatric polytrauma management. Radiol Med 120:33–49
Lee BC, Ormsby EL, McGahan JP, Melendres GM, Richards JR (2007) The utility of sonography for the triage of blunt abdominal patients to exploratory laparatomy. AJR Am J Roentgenol 188:415–421
Taylor GA, Sivit CJ (1995) Post-traumatic peritoneal fluid: is it a reliable indicator of intraabdominal injury in children? J Pediatr Surg 30:1644–1648
Benya EC, Lim-Dunham JE, Landrum O, Statter M (2000) Abdominal sonography in examination of children with blunt abdominal trauma. AJR Am J Roentgenol 174:1613–1616
Chiu WC, Cushing BM, Rodriguez A et al (1997) Abdominal injuries without hemoperitoneum: a potential limitation of focused abdominal sonography for trauma (FAST). J Trauma 42:617–625
Shanmuganathan K, Mirvis SE, Sherbourne CD, Chiu WC, Rodriguez A (1999) Hemoperitoneum as the sole indicator of abdominal visceral injuries: a potential limitation of screening abdominal US for trauma. Radiology 212:423–430
ACEP Clinical Policies Committee; Clinical Policies Subcommittee on (2004) Acute blunt abdominal trauma. clinical policy: critical issues in the evaluation of adult patients presenting to the emergency department with acute blunt abdominal trauma. Ann Emerg Med 43:278–290
Valentino M, Serra C, Zironi G, De Luca C, Pavlica P, Barozzi L (2006) Blunt abdominal trauma: emergency contrast-enhanced sonography for detection of solid organ injuries. AJR Am J Roentgenol 186:1361–1367
Poletti PA, Platon A, Becker CD et al (2004) Blunt abdominal trauma: does the use of a second-generation sonographic contrast agent help to detect solid organ injuries? AJR Am J Roentgenol 183:1293–1301
Valentino M, Serra C, Pavlica P, Barozzi L (2007) Contrast-enhanced ultrasound for blunt abdominal trauma. Seminars Ultrasound CT MR 28:130–140
Kool DR, Blickman JC (2007) Advanced life trauma support: ABCDE from a radiological point of view. Emerg Radiol 14:135–141
Miele V, Buffa V, Stasolla A, Regine G, Atzori M, Ialongo P, Adami L (2004) Contrast enhanced ultrasound with second generation contrast agent in traumatic liver lesions. Radiol Med 108:82–91
Regine G, Atzori M, Miele V, Buffa V, Galluzzo M, Luzietti M, Adami L (2007) Second-generation sonographic contrast agents in the evaluation of renal trauma. Radiol Med 112:581–587
Greenspan L, McLellan BA, Greig H (1985) Abbreviated injury scale and injury severity score: a scoring chart. J Trauma 25:60–64
Pinto F, Miele V, Scaglione M, Pinto A (2014) The use of contrast-enhanced ultrasound in blunt abdominal trauma: advantages and limitations. Acta Radiol 55:776–784
Gavant ML, Schurr M, Flick PA, Croce MA, Fabian TC, Gold RE (1997) Predicting clinical outcome of non surgical management of blunt splenic injury: using CT to reveal abnormalities of splenic vasculature. AJR Am J Roentgenol 168:207–212
Soto JA, Anderson SW (2012) Multidetector CT of blunt abdominal trauma. Radiology 265:678–693
McGahan JP, Wang L, Richards JR. (2001) From the RSNA refresher courses: focused abdominal US for trauma. Radiographics 21(Spec Issue):S191–S199
Emery K, McAneney CM, Racadio JM, Johnson ND, Evora DK, Garcia VF (2001) Absent peritoneal fluid on screening trauma ultrasonography in children: a prospective comparison with computed tomography. J Pediatr Surg 36:565–569
Shanmuganathan K, Mirvis SE, Sherbourne CD, Chiu WC, Rodriguez A (1999) Hemoperitoneum as the sole indicator of abdominal visceral injuries: a potential limitation of screening abdominal US for trauma. Radiology 212:423–430
Poletti PA, Kinkel K, Vermeulen B, Irmay F, Unger PF, Terrier F (2003) Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? Radiology 227:95–103
Federle MP, Courcoulas AP, Powell M, Ferris JV, Peitzman AB (1998) Blunt splenic injury in adults: clinical and CT criteria for management, with emphasis on active extravasation. Radiology 206:137–142
Shanmuganathan K, Mirvis SE, Boyd-Kranis R, Takada T, Scalea TM (2000) Nonsurgical management of blunt splenic injury: use of CT criteria to select patients for splenic arteriography and potential endovascular therapy. Radiology 217:75–82
Mirvis SE, Whitley NO, Gens DR (1989) Blunt splenic trauma in adults: CT-based classification and correlation with prognosis and treatment. Radiology 171:33–39
Gavant ML, Schurr M, Flick PA, Croce MA, Fabian TC, Gold RE (1997) Predicting clinical outcome of nonsurgical management of blunt splenic injury: using CT to reveal abnormalities of splenic vasculature. AJR Am J Roentgenol 168:207–212
Emery K, McAneney CM, Racadio JM, Johnson ND, Evora DK, Garcia VF (2001) Absent peritoneal fluid on screening trauma ultrasonography in children: a prospective comparison with computed tomography. J Pediatr Surg 36:565–569
Valentino M, Serra C, Pavlica P, Morselli Labate AM, Lima M, Baroncini S, Barozzi L (2008) Blunt abdominal trauma: diagnostic performance of contrast-enhanced US in children: initial experience. Radiology 246:903–909
Riccabona M (2012) Application of a second-generation US contrast agent in infants and children: a European questionnaire-based survey. Pediatr Radiol 42:1471–1480
Sessa B, Trinci M, Ianniello S, Menichini G, Galluzzo M, Miele V (2015) Blunt abdominal trauma: role of contrast enhanced ultrasound (CEUS) in the detection and staging of abdominal traumatic lesions compared to US and CE-MDCT. Radiol Med 120:180–189
Trinci M, Sessa B, Menichini G, Valentini V, Miele V. (2015) Abdominal trauma. In: Miele V, Trinci M (eds) Imaging trauma and polytrauma in pediatric patients, Springer, Switzerland, pp 65–100
Pinto F, Valentino M, Romanini L, Basilico R, Miele V (2015) The role of CEUS in the assessment of haemodinamically stable patients with blunt abdominal trauma. Radiol Med 120:3–11
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menichini, G., Sessa, B., Trinci, M. et al. Accuracy of contrast-enhanced ultrasound (CEUS) in the identification and characterization of traumatic solid organ lesions in children: a retrospective comparison with baseline US and CE-MDCT. Radiol med 120, 989–1001 (2015). https://doi.org/10.1007/s11547-015-0535-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-015-0535-z