Abstract
As part of its single technology appraisal (STA) process, the UK National Institute for Health and Care Excellence (NICE) invited the manufacturer (Incyte Corporation) of ponatinib (Inclusig®) to submit evidence of its clinical and cost effectiveness for previously treated Philadelphia-chromosome-positive acute lymphoblastic leukaemia (Ph+ ALL) and chronic myeloid leukaemia. This paper focusses on Ph+ ALL. The School of Health and Related Research Technology Appraisal Group at the University of Sheffield was commissioned to act as the independent evidence review group (ERG). This article presents the critical review of the company’s submission by the ERG and the outcome of the NICE guidance. The clinical-effectiveness evidence in the company’s submission was derived from a phase II, single-arm, open-label, non-comparative study. Given the lack of comparative evidence, a naïve indirect comparison was performed against re-induction chemotherapy comparing major cytogenetic response and complete remission. Best supportive care (BSC) was assumed to produce no disease response. Despite the limited evidence and potential for biases, this study demonstrated that ponatinib was likely to be an effective treatment for patients with Ph+ ALL. The company submitted a state transition model that analysed the incremental cost effectiveness of ponatinib versus re-induction therapy and BSC for the treatment of Ph+ ALL in patients whose disease is resistant to dasatinib, who are intolerant to dasatinib and for whom subsequent treatment with imatinib is not clinically appropriate or who have the threonine-315-isoleucine mutation. This population was further subdivided into those who were suitable for allogeneic stem cell transplant (allo-SCT) and those who were not. The company’s revised economic evaluation, following the clarification process, estimated incremental cost-effectiveness ratios (ICERs) in those suitable for allo-SCT of £31,123 per quality-adjusted life-year (QALY) gained for ponatinib compared with re-induction chemotherapy and £26,624 per QALY gained compared with BSC. For those for whom allo-SCT was unsuitable, the company-estimated ICER compared with BSC was £33,954 per QALY gained. Following a critique of the model, the ERG undertook exploratory analyses that, when combined, produced a range in ICERs (due to uncertainty of the most appropriate overall survival function) of dominant (being less expensive and providing more QALYs) to £11,727 per QALY gained compared with re-induction chemotherapy and between £7892 and £31,696 per QALY gained compared with BSC for those in whom allo-SCT was suitable. For those in whom allo-SCT was not suitable, the ERG estimated that ponatinib was dominant. During the consultation period, the company agreed a revised patient access scheme (PAS) that reduced the ICER ranges to £7156 to £29,995 per QALY gained versus BSC and to less than £5000 per QALY gained versus re-induction chemotherapy. In people for whom allo-SCT was unsuitable, ponatinib dominated BSC. The NICE appraisal committee concluded that ponatinib is a cost-effective use of UK NHS resources in the considered population, subject to the company providing the agreed discount in the PAS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is uncertainty in the cost effectiveness of ponatinib for treating Philadelphia chromosome-positive acute lymphoblastic leukaemia (Ph+ ALL) because the main clinical evidence was derived from a non-comparative study, meaning that naïve indirect comparisons were necessary. |
In patients with Ph+ ALL who are unsuitable for allogeneic stem cell transplant, the use of ponatinib rather than best supportive care is estimated to be less costly and provide more quality-adjusted life-years. |
In patients with Ph+ ALL who are suitable for allogeneic stem cell transplant, the use of ponatinib rather than re-induction chemotherapy or best supportive care is expected to provide more health but at a greater cost. The anticipated cost per quality-adjusted life-year gained is likely to be less than £30,000. |
1 Introduction
The National Institute for Health and Care Excellence (NICE) is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health in priority areas with significant impact. Health technologies must be shown to be clinically effective and to represent a cost-effective use of UK National Health Service (NHS) resources in order for NICE to recommend their use within the NHS in England. The NICE single technology appraisal (STA) process usually covers new single health technologies within a single indication soon after their UK market authorisation [1]. Within the STA process, the company provides NICE with a written submission and a mathematical model that summarises the company’s estimates of the clinical and cost effectiveness of the technology. This submission is reviewed by an external organisation independent of NICE (the evidence review group [ERG]), which consults with clinical specialists and produces a report. After considering the company’s submission, the ERG report and testimony from experts and other stakeholders, the NICE appraisal committee (AC) formulates preliminary guidance, the appraisal consultation document (ACD), which indicates the initial decision of the AC regarding the recommendation (or not) of the technology. Stakeholders are then invited to comment on the submitted evidence and the ACD, after which a further ACD may be produced or a final appraisal determination (FAD) issued, which is open to appeal. An ACD is not produced when the technology is recommended within its full marketing authorisation; in this case, an FAD is produced directly.
This paper presents a summary of the ERG report [2] for the STA of ponatinib for the treatment of Philadelphia chromosome positive (Ph+) acute lymphoblastic leukaemia (ALL) in patients whose disease is resistant to dasatinib, who are intolerant to dasatinib and for whom subsequent treatment with imatinib is not clinically appropriate or who have the threonine-315-isoleucine (T315I) mutation. A summary of the subsequent development of the NICE guidance for the use of this technology in England is also provided. Full details of all relevant appraisal documents (including the appraisal scope, ERG report, company and consultee submissions, FAD and comments from consultees) can be found on the NICE website [2].
2 The Decision Problem
ALL is a rare and rapidly progressing form of leukaemia characterised by the excess production of immature white blood cells, called lymphoblasts (sometimes referred to as blast cells). Eventually, this affects the production of normal blood cells, which leads to a reduction in the numbers of red cells, white cells and platelets in the blood [3]. ALL represents about 20% of all leukaemias in adults and is the most common form of childhood leukaemia [4,5,6]. Approximately 25% [5, 7, 8] of adults with ALL have an acquired chromosomal abnormality (known as Ph+ disease) caused by reciprocal translocations between chromosomes 9 and 22. The presence of the Ph chromosome in adults increases with age [4,5,6], and individuals with Ph+ ALL typically have a worse prognosis than those without this abnormality [9].
Survival in adult patients with ALL is poor. The 5-year survival rate for those aged 25–64 years in England was 37.1% for those diagnosed in 2008, whereas for individuals aged over 65 years, 5-year survival was 12.7% [10].
2.1 Current Treatment
The management of patients with Ph+ ALL is complex, and there is currently no NICE guidance or pathway of care for the treatment of adults with Ph+ ALL in England. In general, the treatment of Ph+ ALL varies according to age, general fitness and health at diagnosis and the results of cytogenetic testing.
An allogeneic stem cell transplant (allo-SCT) is the only potentially curative treatment for Ph+ ALL; however, it is limited by patient suitability as well as the availability of suitable donors and is associated with a significant risk of morbidity and mortality [11]. The use of oral tyrosine kinase inhibitors (TKIs) has become an integral component of therapy for people with Ph+ ALL. Currently, three TKIs (imatinib [12], dasatinib [13] and ponatinib [14]) have an EU marketing authorisation for the treatment of Ph+ ALL. Neither imatinib nor dasatinib for the treatment of adult Ph+ ALL have been appraised by NICE, and the extent to which these TKIs are used in current clinical practice is unknown. Dasatinib [13] was available for the treatment of adults with Ph+ ALL with resistance or intolerance to prior therapy, including imatinib through the Cancer Drugs Fund until November 2015 when it was removed from the Cancer Drugs Fund list [15].
3 The Independent Evidence Review Group (ERG) Review
In accordance with the process for STAs, the ERG and NICE had the opportunity to seek clarification on specific points in the company’s submission (CS) [16], in response to which the company provided additional information [16]. The ERG also modified the company’s decision analytic model to produce an ERG base case and to assess the impact of alternative parameter values and assumptions on the model results. The evidence presented in the company’s submission and the ERG’s review of that evidence is summarised here.
3.1 Clinical Evidence Provided by the Company
Evidence was presented in the CS [16] relating to the clinical effectiveness of ponatinib in ALL. No randomised controlled trials (RCTs) relevant to the decision problem were identified from the systematic review of the literature. The company identified a phase I dose-finding study [17, 18], which was not deemed entirely relevant to either the recommended dose or the licensed indication, and a phase II study (PACE) [19,20,21]. Therefore, PACE was considered the pivotal evidence. No ongoing studies of ponatinib in Ph+ ALL patients were identified.
PACE was an industry-sponsored, single-arm, non-comparative, open-label, multicentre study (including five sites in the UK) designed to evaluate the effectiveness of oral ponatinib at a starting dose of 45 mg once daily, in 449 people (53% male; 78% Caucasian) with chronic-phase chronic myeloid leukaemia (n = 270), accelerated-phase chronic myeloid leukaemia (n = 85), blast-phase chronic myeloid leukaemia (n = 62) or Ph+ ALL (n = 32) who were resistant or intolerant to either dasatinib or nilotinib or who had the T315I mutation after any TKI therapy (as confirmed by direct sequencing) [7, 19, 22]. Study participants in the PACE study were heavily pre-treated with prior TKIs and conventional therapy: 37% (167/449) had received two TKIs out of a possible four (imatinib, dasatinib, nilotinib or bosutinib). This population was the target population in the company’s decision problem for Ph+ ALL, reflecting the anticipated place in therapy of ponatinib, after treatment failure with prior TKI therapy. The primary outcome measure for patients with Ph+ ALL in the PACE study was major haematological response (MaHR), which included complete haematologic responses (CHRs) and no evidence of leukaemia at 6 months. The summary of product characteristics posology recommends considering discontinuation of ponatinib if a CHR has not occurred by 3 months (90 days) [14].
The average daily dose for patients receiving ponatinib was 42.3 mg per day. The study was started in September 2010, with the company estimating a completion date of March 2017 in its submission. Data to August 2015 were provided within the company’s submission.
In response to a request for clarification [16], the company provided updated data (approaching 3 years longer follow-up than in the pivotal paper [19]). However, the updated data were marked commercial-in-confidence and cannot be presented in this paper.
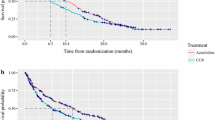
Among patients with Ph+ ALL (all lines, n = 32 [data not reported separately by line of therapy]), 41% (95% confidence interval [CI] 24–59) achieved an MaHR within the first 6 months (primary endpoint). The duration of response ranged from 2 to 14 months or more (median 3 months), and the estimated rate of a sustained response of at least 12 months was 8%. The median time to MaHR for responders was 2.9 weeks (range 1.6–24). Furthermore, major cytogenetic response (MCyR) was reached in 47% of patients, and 38% had a complete cytogenetic response (CCyR). The median time to MCyR for responders was 1 month (range 0.9–3.7), with an estimated 32% of responding patients maintaining this response for at least 12 months. In patients with Ph+ ALL, the progression-free survival and overall survival at 12 months was estimated to be 7% (median 3 months) and 40% (median 8 months), respectively [19]. In addition, overall survival at 36 months was estimated to be 16% [20].
Among the subgroup of patients with Ph+ ALL who had the T315I mutation (n = 22, all lines) [19], 36% (95% CI not reported) had an MaHR within the first 6 months. A total of 40% of patients with Ph+ ALL achieved MCyR and 32% reached CCyR (95% CI not reported for either outcome) [19]. The ERG believes that caution should be used in the interpretation of the T315I data because of the small population size and study design limitations.
At the latest data cut for treatment discontinuation, 31 of 32 patients had stopped ponatinib treatment. Of these, 53% of patients discontinued because of disease progression, 16% had died and 12% discontinued because of lack of efficacy. At the last data-cut (November 2012) where safety data can be presented in this paper, the following severe or life-threatening treatment-related adverse events were observed: neutropenia (12%), anaemia (12%), thrombocytopenia (6%), febrile neutropenia (6%), abdominal pain (6%) and increased lipase (6%). All other serious or life-threatening treatment-related adverse events occurred in one (3%) or fewer patients.
3.2 Critique of the Clinical Evidence and Interpretation
The systematic review process followed by the company was reasonably comprehensive. Despite minor limitations in the company’s search strategy, the ERG was reasonably confident that all relevant published studies (RCTs and non-randomised/non-controlled evidence) of ponatinib were included in the CS, including data from ongoing studies.
Based on the quality assessment tool for non-randomised studies [23], the ERG considered the PACE study to be a well-reported and conducted single-arm study. However, single-arm studies are associated with an array of potential biases [24], most importantly the ability to estimate a relative treatment effect compared with a concurrent control.
The clinical advisor to the ERG considered MaHR to be a weak surrogate endpoint for patients with Ph+ ALL. Ideally, a better endpoint for bridging to transplant would be minimal residual disease levels in the bone marrow, which is a more stringent criterion. However, although response milestones for patients with Ph+ ALL have not been well established, treatment strategies usually involve achieving an MaHR with the aim of proceeding to allo-SCT, if feasible.
The main uncertainties surrounding the clinical evidence for ponatinib relate to the unbiased estimation of treatment effects, optimal dosing and duration of treatment. Whilst the clinical advisor to the ERG considered that the PACE study population was reflective of the Ph+ ALL population in England, it was noted that patients in the study had received nilotinib, which is not representative of NHS practice.
3.3 Cost-Effectiveness Evidence Provided by the Company
The company submitted an economic model to assess the cost effectiveness of ponatinib in Ph+ ALL from the perspective of the NHS and Personal Social Services over a lifetime horizon. Both benefits and costs were discounted at a rate of 3.5% per annum. The model employed a state transition approach, with 3-monthly time cycles and includes a half-cycle correction. The model originally submitted was amended by the company following the clarification process; only the revised model is detailed here. The company had a patient access scheme (PAS) agreed, which represents a simple discount, the value of which is commercial in confidence; during the appraisal process, the company agreed a second PAS with a larger discount. Only results incorporating the PAS are presented within this report.
Having entered the model, a hypothetical patient could receive one of three interventions: (1) ponatinib, (2) re-induction chemotherapy or (3) best supportive care (BSC). The characteristics of the hypothetical patients were based on those in the PACE study, with 62.5% male and an initial age of 53 years [19].
The simulated patient pathway was identical for patients receiving ponatinib or re-induction chemotherapy in that if an MyCR (for ponatinib) or complete remission (CR) (for re-induction chemotherapy) was achieved, the patient was assumed to receive allo-SCT (if suitable). The different response levels were chosen to align with the study data. Clinical advice provided to the ERG suggested that results following an allo-SCT are better in patients with minimal residual disease than in those with greater disease levels at the time of transplant. For patients who received BSC, it was assumed there would be no response (NR). For all treatments, death could occur at any time point.
For patients who received ponatinib or re-induction chemotherapy, the model simulated the response of patients to the treatment, which was assumed to occur in the first cycle only. It was assumed that patients would fall into one of two mutually exclusive and exhaustive states: remission (which incorporated either MyCR [ponatinib] or CR [re-induction chemotherapy]) and NR. For patients simulated to experience remission, the next event in the model (a term that has been used to identify the next event whilst excluding remaining in the same health state) would be allo-SCT, if appropriate. Following allo-SCT, the next event is death. For those who experienced NR and/or who are unsuitable for allo-SCT, the next event is death. For patients who received BSC, the only event possible is death.
The response rates assumed in the model for each treatment in Ph+ ALL are detailed in Table 1. Data for MCyR for ponatinib were taken from the PACE study [19], whereas data on CR for re-induction therapy were taken from Tavernier et al. [25]. No attempts were made by the company to account for differences in prognostic variables and treatment effect modifiers between PACE and external comparator studies. The ERG commented that this is a naïve unadjusted indirect comparison and could be associated with a high risk of bias. Advice provided by the clinical advisor to the ERG indicated that MCyR is harder to achieve than CR: if this is correct, the relative effectiveness between ponatinib and re-induction chemotherapy would be unfavourable to ponatinib.
The treatment-emergent serious adverse events described earlier were incorporated in the model along with peripheral vascular events (5%) and venous thromboembolism events (4%). Adverse events were only assumed to occur with ponatinib, not with chemotherapy or BSC.
After simulating the response rates associated with each treatment, many other parameters in the model were assumed independent of initial treatment. This is appropriate where pivotal studies are of relatively short duration, but the reliance on extrapolating from surrogate data increases the uncertainty in the results. The company used the Solver function in Microsoft® Excel to minimise the sum of squared errors (SSE) between the predicted survival function and that of the digitised points and, if the extrapolation was believed by the company to be clinically plausible, the survival function with the lowest SSE was selected.
For patients who experienced remission (MyCR or CR), it was assumed that—if a patient were suitable for allo-SCT—this would occur. The probability of death was conditional on whether a patient received allo-SCT and whether the patient experienced remission or not.
The probability of death following allo-SCT was derived from data presented in Tavernier et al. [25]. Standard parametric models were undertaken using exponential, Weibull, Gompertz, log-normal and log-logistic survivor functions. All distributions pooled data from patients with MCyR and NR and used a covariate for response level. The data were digitised and survival functions fitted by minimising the SSE between the observed data-points and fitted survival function. With the exception of the exponential distribution, the range in SSE was relatively small (0.04–0.05). The company selected the log-logistic distribution for use in the base-case model.
The probability of death for patients who experienced remission but were not suitable for allo-SCT was estimated from data collected in the PACE study [19]. The company fitted standard parametric models to these data. Based on these analyses, the company stated that the best fit using the Akaike information criterion (AIC) and Bayesian information criteria (BIC) were not in agreement, but—of the two best-fitting models for AIC and BIC—the exponential distribution was selected as it was considered more clinically plausible than the Gompertz survival function (data were marked as academic-in-confidence). It was assumed that the probability of death was independent of whether ponatinib or re-induction chemotherapy provoked the remission.
It was also assumed that the probability of death following NR would be the same following ponatinib or re-induction chemotherapy, with these risks estimated from the PACE study [19] using the survival analysis method described previously. The exponential survival function was selected as this was deemed by the company to be more clinically plausible than the Gompertz survival function. For patients who received BSC, the risk of death was estimated using data reported from an Italian single-centre retrospective study in patients with ALL [26]. This study reported a median overall survival of 2.6 months, and this value was used to fit an exponential function, although no justification for a constant hazard was provided.
The duration of ponatinib treatment was estimated using individual patient data from the PACE study [19]. The company fitted standard parametric models to these data. Based on this analysis, the company stated that the best fit using the AIC and BIC criteria was the log-logistic survival function (data were marked as academic-in-confidence). The duration of re-induction chemotherapy was a maximum of 6 weeks. Following cessation of ponatinib or re-induction chemotherapy, it was assumed that BSC would be provided until death; where BSC was the first-line treatment, it was assumed to be continued until death.
The company performed a systematic review to identify evidence regarding health-related quality of life and assumed that the utilities reported by Szabo et al. [27] for blast-phase chronic myeloid leukaemia were applicable for patients with Ph+ ALL. As such, patients who responded to treatment were assumed to have a utility decrement of 0.286, and patients who did not respond to treatment had a utility decrement of 0.556 compared with the general population [28]. Patients who received allo-SCT were assumed to have a utility decrement that reduced over time, being 0.296 within the first 3 months [29], 0.136 after 6 months [30] and assumed to be 0.216 between 3 and 6 months. The utilities for all adverse events were assumed to be 0.52 based on Szabo et al. [27], from which a utility decrement was estimated based on the estimated general population value.
The cost of a 6-week course of re-induction chemotherapy was assumed to be £18,000, based on British National Formulary data (reference not provided) and an assumption that Leucémie Aiguës Lymphoblastique de l’Adulte (LALA-94), hyperfractionated cyclophosphamide, vincristine, doxorubicin (adriamycin), dexamethasone and cytarabine and methotrexate (Hyper-CVAD) and fludarabine, cytarabine, methotrexate, granulocyte colony-stimulating factor and idarubicin (FLAG-IDA) were used equally. The cost of BSC was assumed to be £4064 based on Pagano et al. [26]. The cost of ponatinib was stated to be commercial-in-confidence because of the PAS and the dosing regimens observed in PACE [19].
Based on a UK survey conducted by the company, the number of days in hospital per cycle was assumed to be zero for those with a response and 26.64 for those with no response. Monitoring costs were assumed to be independent of treatment for the response and non-response states. The company assumed that patients with Ph+ ALL who responded to treatment would require the same monitoring resources as patients with chronic-phase chronic myeloid leukaemia, whereas those with Ph+ ALL who did not respond to treatment were assumed to require the same monitoring resources as patients with blast-phase chronic myeloid leukaemia. No additional costs of monitoring cardiovascular events were considered for ponatinib. Hospitalisation and monitoring costs per cycle were estimated as £208 for responders and £24,070 for non-responders. The company assumed the cost of allo-SCT was £60,092, based on data from the UK Stem Cell Strategy Oversight Committee [31]. The follow-up costs decreased over time, with a per-cycle cost of £12,215 in year 1, £3518 in year 2 and £420 in year 3. A cost of £5766 was assumed to be incurred at death based on a survey undertaken by the company. The components of each cost estimate were valued at 2014–2015 values unless a more recent value was available.
Following the clarification period, the company estimated that the incremental cost-effectiveness ratio (ICER) for ponatinib was £26,624 per quality-adjusted life-year (QALY) gained compared with BSC and £31,123 per QALY gained compared with re-induction chemotherapy. Sensitivity analysis comparing ponatinib against re-induction chemotherapy showed that the ICER was very sensitive to the response rate generated by re-induction chemotherapy. For patients for whom allo-SCT was unsuitable, the company-estimated ICER was £33,954 per QALY gained for ponatinib compared with BSC. This ICER was most sensitive to the assumed response rate associated with ponatinib. Results from probabilistic sensitivity analyses were consistent with those from deterministic analyses.
During the appraisal, the company agreed an increased commercial-in-confidence discount and amended errors highlighted by the ERG. This resulted in base-case ICERs estimated by the company of £26,319 per QALY gained compared with BSC and was £29,812 per QALY gained compared with re-induction chemotherapy for patients suitable for allo-SCT. The company-estimated ICER compared with BSC for those unsuitable for allo-SCT was £31,210 per QALY gained.
3.4 Critique of the Cost-Effectiveness Evidence and Additional Work Undertaken by the ERG
The ERG made changes to the model/analyses presented by the company. These are detailed below.
The ERG believed that the method used by the company in fitting survival functions to digitised survival data was inappropriate. The ERG had concerns with the approach used as this method weighted points equally despite the number of patients contributing data to the curve declining as time progressed and provided no information about parameter uncertainty. A better approach would have been to use the method presented by Guyot et al. [32], which allows estimation of parameters and their uncertainty.
The ERG believed insufficient sensitivity analyses were undertaken by the company. Kass and Raftery [33] stated that a difference in the BIC of less than two is barely worth a mention, whereas only difference values of six or greater indicate strong evidence that one survival function may be preferable to another. In addition, measures of goodness-of-fit of the models to the sample data such as the BIC does not take clinical plausibility of the extrapolated survival functions into account. Taking the BIC and clinical plausibility into consideration, the ERG undertook exploratory results using alternative survival functions to those selected by the company. Where multiple survival functions were thought plausible, the company’s base case was explored along with the survival function that had the most different predictions of long-term outcome to that produced by the company’s default survival function, to test extreme values. The survival functions considered to be potentially credible by the ERG and the clinical advisor to the ERG were as follows: for overall survival following response to ponatinib treatment but not receiving allo-SCT, the exponential and the Gompertz distributions; for duration of ponatinib treatment, the log-normal and the log-logistic distributions; and for overall survival after allo-SCT, the Gompertz, the log-normal and the log-logistic distributions.
The company had used two different sources in the model for non-responding patients, assuming a median life expectancy of 5.57 months based on data from the PACE study [19]. For patients who received BSC, the median life expectancy was assumed to be 2.60 months, as reported by Pagano et al. [26]. This difference in estimated survival for non-responders, which is based on a naïve indirect comparison, did not have face validity with the clinical advisor to the ERG. In the clarification response [16], the company reported that the median age in Pagano et al. [26] was higher (77 years) than the median age in PACE (62 years) and that this could have caused the longer mean survival observed in PACE. The ERG amended the model to explore the impact of setting the survival following non-response equal for those who have ponatinib and those that have BSC, which was supported by clinical advice provided to the ERG.
The ERG was concerned that the company assumption that unused tablets in a prescription would eventually be used was incorrect, and an analysis was conducted assuming drug wastage. The construct of the model meant that prescriptions were assumed to occur at 3-monthly intervals, and this interval could not be altered by the ERG in the timelines of the STA. As such, the ICER was likely to be greater than were the true frequency of prescriptions, which is anticipated to be more frequent than 3 months, used.
In addition to the errors identified by the ERG and corrected by the company, the intervention costs were half-cycle corrected by the manufacturer, and there was an implementation error that resulted in immortality for one cycle for a small subset of patients. These perceived errors were corrected by the ERG. The inclusion of treatment-related deaths was explored but omitted from the ERG base case, which is likely to be favourable to ponatinib.
The company provided no analyses for patients with the T315I mutation. If the presence of the mutation were known, then re-induction chemotherapy would not be an option. If a person was known to not have the T315I mutation, then the ICER compared with re-induction chemotherapy would likely be less favourable to ponatinib, although the extent of the increase is uncertain.
The results of the ERG base-case analyses are provided in Table 2 for patients suitable for allo-SCT and in Table 3 for patients unsuitable for allo-SCT.
3.5 Conclusions of the ERG Report
The key clinical-effectiveness evidence for ponatinib was a single-arm study recruiting 32 patients with Ph+ ALL. Naïve indirect comparisons were used to compare ponatinib against re-induction chemotherapy and BSC, which are biased. The changes made by the ERG, and the company following the clarification process, along with a larger PAS, resulted in the ICER estimated by the ERG to be between £7,156 per QALY gained and £29,995 per QALY gained compared with BSC in patients suitable for allo-SCT. For patients unsuitable for allo-SCT, ponatinib was assumed to dominate (that is, be less costly and more beneficial) than BSC.
4 Key Methodological Issues
Analyses conducted based on naïve indirect comparisons are biased. The face validity of each comparison should be carefully assessed. In the company submission, the expected survival for patients who had no response to ponatinib or re-induction chemotherapy was assumed to be longer than for patients receiving BSC, who were assumed to have no response. This assumption was not supported by the clinical advisor to the ERG. When the survival functions were set equal, the ICER changed markedly, in favour of ponatinib.
The exploration of the impact of using alternative, plausible survival functions on the ICER was not undertaken by the company. The analyses undertaken by the ERG indicate that the range of the ICER was large and that a decision based on an ICER from a single survival function could be misleading.
5 National Institute for Health and Care Excellence Guidance
In June 2017, on the basis of the evidence available (including verbal testimony of invited clinical experts and patient representatives), the NICE AC produced guidance that ponatinib was recommended as an option for treating Ph+ ALL when the disease is resistant to dasatinib, or when the patient cannot tolerate dasatinib and for whom subsequent treatment with imatinib is not clinically appropriate, or the T315I gene is present and when the company provides the drug with the agreed PAS.
5.1 Consideration of Clinical and Cost-Effectiveness Issues Included in the Final Appraisal Determination
This section summarises the key issues considered by the AC. The full list of the issues considered by the AC can be found in the FAD [34].
5.1.1 Uncertainties in the Clinical Evidence
The AC noted the lack of a comparator in the PACE study [19], which was justified by the company on the basis that it was unethical to randomise patients to placebo or ponatinib in addition to BSC who have not responded to previous treatment. The AC was aware that, for some patients in the study, the dosage was changed or treatment was stopped, which led to uncertainties about the best dosing level, the duration of treatment and the generalisability of the response rates. The AC also noted the small number of patients with Ph+ ALL in the PACE study. The committee concluded that, despite these uncertainties, the evidence presented was sufficient for decision making.
5.1.2 Uncertainties in the Economic Modelling
The AC noted that the company had “done indirect comparisons because of a lack of direct comparative evidence.” Nevertheless, the AC concluded that there was sufficient evidence for its decision making. The AC considered the range of ICERs presented by the ERG. The AC understood that survival time following non-response was independent of treatment and concluded that the sensitivity analyses undertaken by the ERG accounted for this uncertainty. The AC concluded that there was uncertainty about which parametric distributions were most plausible and clinically appropriate.
5.1.3 End-of-Life Criteria
The AC concluded that the end-of-life criteria (a survival of less than 2 years and an extension of life of more than 3 months) had been met for all patients with Ph+ ALL regardless of suitability for allo-SCT.
6 Conclusions
The AC recognised that there was considerable uncertainty in the value of the ICERs, and therefore their most likely value fell within a range. The AC concluded that, in all instances, this range included cost-effective values, and therefore ponatinib was a cost-effective use of NHS resources.
References
National Institute for Health and Care Excellence (NICE). Guide to the methods of technology appraisal 2013—process and methods [PMG9]. London: NICE. 2013. https://www.nice.org.uk/article/pmg9/. Accessed 23 November 2016.
Pandor A, Stevenson M, Martyn-St James M, Stevens J, Hamilton J, Rawdin A et al. Ponatinib for treating acute lymphoblastic leukaemia: a single technology appraisal. School of Health and Related Research (ScHARR). 2016. https://www.nice.org.uk/guidance/ta451/documents/committee-papers. Accessed 20 Nov 2017.
National Institute for Health and Care Excellence. Ponatinib for treating chronic myeloid leukaemia and acute lymphoblastic leukaemia. Final Scope. National Institute for Health and Care Excellence (NICE), London. 2016. https://www.nice.org.uk/guidance/ta451/documents/committee-papers. Accessed 20 Nov 2017.
Alvarnas JC, Brown PA, Aoun P, Ballen KK, Bellam N, Blum W, et al. Acute lymphoblastic leukemia. J Natl Compr Canc Netw. 2012;10(7):858–914.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Chronic Myelogenous Leukemia. Version 1.0. 2016. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed 23 Nov 2016.
Radich JP. Philadelphia chromosome-positive acute lymphocytic leukemia. Hematol Oncol Clin North Am. 2001;15(1):21–36.
European Medicines Agency (EMA). Assessment Report for Inclusig® (ponatinib). Procedure No EMEA/H/C/002695/0000. London: EMA. 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002695/WC500145648.pdf. Accessed 23 November 2017.
Fielding AK, Richards SM, Chopra R, Lazarus HM, Litzow MR, Buck G, et al. Outcome of 609 adults after relapse of acute lymphoblastic leukemia (ALL); an MRC UKALL12/ECOG 2993 study. Blood. 2007;109(3):944–50.
Fielding AK. Current treatment of Philadelphia chromosome-positive acute lymphoblastic leukemia. Hematol Am Soc Hematol Educ Program 2011:231–7.
Public Health England. National Cancer Intelligence Network Trends in incidence and outcome for haematological cancers in England: 2001–2010. London: Public Health England. 2015. http://www.ncin.org.uk/view?rid=2818. Accessed 20 November 2017.
Ravandi F. Managing Philadelphia chromosome-positive acute lymphoblastic leukemia: role of tyrosine kinase inhibitors. Clin Lymphoma Myeloma Leuk. 2011;11(2):198–203.
Novartis Europharm Limited. Glivec® (imatinib) 50-mg and 100-mg hard capsules and 100-mg and 400-mg film-coated tablets: Summary of Product Characteristics. [updated 28 November 2016]. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000406/WC500022207.pdf. Accessed 1 Dec 2016.
Bristol-Myers Squibb Pharma. Sprycel® (dasatinib) 20-mg, 50-mg, 70-mg, 80-mg, 100-mg, 140-mg film-coated tablets: Summary of Product Characteristics. [updated 20 July 2016]. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000709/WC500056998.pdf. Accessed 1 Dec 2016.
ARIAD Pharma Ltd. Iclusig® (ponatinib) 15-mg, 30-mg, and 45-mg film-coated tablets: summary of product characteristics. [updated 16 September 2016]. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002695/WC500145646.pdf. Accessed 1 Dec 2016.
Adcock A, Powell T. Removal of drugs from Cancer Drugs Fund list. London: House of Commons Library. 2016. http://researchbriefings.parliament.uk/ResearchBriefing/Summary/CDP-2016-0009. Accessed 1 Dec 2016.
Incyte Corporation. Ponatinib for treating chronic myeloid leukaemia and acute lymphoblastic leukaemia [ID671]. Response to clarification letter. 2016. https://www.nice.org.uk/guidance/ta451/documents/committee-papers. Accessed 22 Nov 2017.
Cortes JE, Kantarjian H, Shah NP, Bixby D, Mauro MJ, Flinn I, et al. Ponatinib in refractory Philadelphia chromosome-positive leukemias. N Engl J Med. 2012;367(22):2075–88. https://doi.org/10.1056/NEJMoa1205127.
Talpaz M, Cortes JE, Kantarjian HM, Shah NP, Bixby DL, Flinn I et al. Four-year minimum follow-up of ongoing patients (pts) with chronic-phase chronic myeloid leukemia (CP-CML) in a phase 1 trial of ponatinib (PON). J Clin Oncol (Meeting Abstracts). 2015;33(15_suppl):7047.
Cortes JE, Kim D-W, Pinilla-Ibarz J, le Coutre P, Paquette R, Chuah C, et al. A phase 2 trial of ponatinib in Philadelphia chromosome-positive leukemias. N Engl J Med. 2013;369(19):1783–96. https://doi.org/10.1056/NEJMoa1306494.
Cortes JE, Kim D-W, Pinilla-Ibarz J, le Coutre P, Paquette R, Chuah C, et al. Ponatinib efficacy and safety in heavily pretreated leukemia patients: 3-Year results of the pace trial. P234. Haematologica. 2015;100(S1):64.
Hochhaus A, Cortes JE, Kim DW, Pinilla-Ibarz J, le Coutre PD, Paquette R, et al. Efficacy and safety of ponatinib in CP-CML patients by number of prior tyrosine kinase inhibitors: 4-year follow-up of the phase 2 PACE trial. Blood. 2015;126(23):4025.
U.S. Food and Drug Administration Center for Drug Evaluation and Research. Application number: 203469Orig1s000 Medical review. 2012. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/203469Orig1s000MedR.pdf. Accessed 23 Nov 2016.
Chambers D, Rodgers M, Woolacott N. Not only randomized controlled trials, but also case series should be considered in systematic reviews of rapidly developing technologies. J Clin Epidemiol. 2009;62(12):1253–60. https://doi.org/10.1016/j.jclinepi.2008.12.010.
Evans S. Clinical trial structures. J Exp Stroke Transl Med. 2010;3(1):8–18.
Tavernier E, Boiron JM, Huguet F, Bradstock K, Vey N, Kovacsovics T, et al. Outcome of treatment after first relapse in adults with acute lymphoblastic leukemia initially treated by the LALA-94 trial. Leukemia. 2007;21(9):1907–14. https://doi.org/10.1038/sj.leu.2404824.
Pagano L, Mele L, Casorelli I, Fianchi L, Di Febo A, Leone G. Acute lymphoblastic leukemia in the elderly. A twelve-year retrospective, single center study. Haematologica. 2000;85(12):1327–9.
Szabo SM, Levy AR, Davis C, Holyoake TL, Cortes J. A multinational study of health state preference values associated with chronic myelogenous leukemia. Val Health. 2010;13(1):103–11. https://doi.org/10.1111/j.1524-4733.2009.00573.x.
Kind P, Hardman G, Macran S. UK population norms for EQ-5D. 1999. http://EconPapers.repec.org/RePEc:chy:respap:172chedp. Accessed 1 Dec 2016.
van Agthoven M, Vellenga E, Fibbe WE, Kingma T, Uyl-de Groot CA. Cost analysis and quality of life assessment comparing patients undergoing autologous peripheral blood stem cell transplantation or autologous bone marrow transplantation for refractory or relapsed non-Hodgkin’s lymphoma or Hodgkin’s disease. a prospective randomised trial. Eur J Cancer (Oxford, England: 1990). 2001;37(14):1781–9.
Loveman E, Cooper K, Bryant J, Colquitt JL, Frampton GK, Clegg A. Dasatinib, high-dose imatinib and nilotinib for the treatment of imatinib-resistant chronic myeloid leukaemia: a systematic review and economic evaluation. Health Technol Assess (Winchester, England). 2012;16(23):iii–xiii, 1–137. https://doi.org/10.3310/hta16230.
UK Stem Cell Strategy Oversight Committee. NHS Blood and Transplant. Unrelated Donor Stem Cell Transplantation in the UK. Effective Affordable Sustainable. 2014. http://www.nhsbt.nhs.uk/download/unrelated_donor_stem_cell_transplantation_in_the_uk.pdf. Accessed 1 Dec 2016.
Guyot P, Ades AE, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan–Meier survival curves. BMC Med Res Methodol. 2012;12:9. https://doi.org/10.1186/1471-2288-12-9.
Kass RE, Raftery AE. Bayes factors. J Am Stat Assoc. 1995;90(430):773–95. https://doi.org/10.2307/2291091.
National Institute for Health and Care Excellence (NICE). Ponatinib for treating chronic myeloid leukaemia and acute lymphoblastic leukaemia—technology appraisal guidance [TA451]. NICE, London. 2017. https://www.nice.org.uk/guidance/ta451/. Accessed 23 Nov 2017.
Acknowledgements
This summary of the ERG report was compiled after NICE issued the FAD. All authors have commented on the submitted manuscript and have given their approval for the final version to be published. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of NICE or the Department of Health. Any errors are the responsibility of the authors.
Funding
This project was funded by the National Institute for Health Research (NIHR) Health Technology Assessment Programme (Project Number 16/51/11). Visit the HTA programme website for further project information (http://www.hta.ac.uk).
Author information
Authors and Affiliations
Contributions
Matt Stevenson and Andrew Rawdin critiqued the mathematical model provided and the cost-effectiveness analyses submitted by the company. Abdullah Pandor and Marrissa Martyn-St James critiqued the clinical-effectiveness data reported by the company. Jean Hamilton and John Stevens critiqued the statistical aspects of the submission and the analyses performed by the company. Ruth Wong critiqued the literature searches undertaken by the company. Clare Rowntree provided clinical advice to the ERG throughout the project. All authors were involved in drafting and commenting on the final document. Matt Stevenson acts as the guarantor of the manuscript. This summary has not been externally reviewed by PharmacoEconomics.
Corresponding author
Ethics declarations
Conflict of interest
Dr Clare Rowntree undertook some consulting work in 2015–2016 for ARIAD Pharmaceuticals, the manufacturer of ponatinib. This work resulted in an authored published abstract in a health economics journal. MS, AP, JH, JS, MMSJ, AR, RW have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Stevenson, M., Pandor, A., Hamilton, J. et al. Ponatinib for Treating Acute Lymphoblastic Leukaemia: An Evidence Review Group Perspective of a NICE Single Technology Appraisal. PharmacoEconomics 36, 759–768 (2018). https://doi.org/10.1007/s40273-018-0624-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-018-0624-7