Abstract
As part of its single technology appraisal process, the National Institute for Health and Care Excellence (NICE) invited the company that manufactures ponatinib (Inclusig®; Incyte Corporation) to submit evidence for the clinical and cost effectiveness for previously treated chronic myeloid leukaemia (CML) and Philadelphia-chromosome-positive acute lymphoblastic leukaemia (Ph+ ALL). This paper focusses on the three phases of CML: the chronic phase (CP), the accelerated phase (AP) and the blast crisis phase (BP). The School of Health and Related Research Technology Appraisal Group at the University of Sheffield was commissioned to act as the independent Evidence Review Group (ERG). This article presents the critical review of the company’s submission by the ERG and the outcome of the NICE guidance. Clinical evidence for ponatinib was derived from a phase II, industry-sponsored, single-arm, open-label, multicentre, non-comparative study. Despite the limited evidence and potential for biases, this study demonstrated that ponatinib was likely to be an effective treatment (in terms of major cytogenetic response and major haematological response) with an acceptable safety profile for patients with CML. Given the absence of any head-to-head studies comparing ponatinib with other relevant comparators, the company undertook a matching-adjusted indirect comparison (MAIC) of ponatinib with bosutinib. The approach was only used for patients with CP-CML because comprehensive data were not available for the AP- or BP-CML groups to allow the matching technique to be used. Despite the uncertainty about the MAIC approach, ponatinib was considered likely to offer advantages over bosutinib in the third-line setting, particularly for complete cytogenetic response. The company developed two health economic models to assess the cost effectiveness of ponatinib for the treatment of patients in CP-CML or in advanced CML (AP- or BP-CML, which were modelled separately). The company did not adequately explore the uncertainty in the survivor functions. As a result, the ERG believed the uncertainty in the decision problem was underestimated. Exploratory analyses undertaken by the ERG produced the following results for ponatinib. In CP-CML, from £18,246 to £27,667 per quality-adjusted life-year (QALY) gained compared with best supportive care (BSC), from £19,680 to £37,381 per QALY gained compared with bosutinib and from £18,279 per QALY gained to dominated compared with allogeneic stem cell transplant (allo-SCT). In AP-CML, the cost per QALY gained for ponatinib ranged from £7123 to £17,625 compared with BSC, and from dominating to £61,896 per QALY gained compared with allo-SCT. In BP-CML, the cost effectiveness of ponatinib ranged from £5033 per QALY gained to dominated compared with allo-SCT, although it was likely to be at the more favourable end of this range, and dominant in all scenarios compared with BSC. The NICE appraisal committee concluded that ponatinib is a cost-effective use of NHS resources in the considered population, subject to the company providing the agreed discount in the Patient Access Scheme.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
There is uncertainty in the relative efficacy of ponatinib because of the main clinical evidence being derived from a non-comparative study. |
The cost per quality-adjusted life-year (QALY) gained values for ponatinib compared with bosutinib, allogeneic stem cell transplant and best supportive care were uncertain because of the uncertainty associated with extrapolated survivor functions. |
The exploratory analyses performed by the Evidence Review Group provided ranges in which the cost per QALY gained were likely to fall for patients with chronic phase, accelerated phase, and blast crisis phase chronic myeloid leukaemia. These ranges included values which fall both above and below the National Institute for Health and Care Excellence reported cost-effectiveness thresholds of typically between £20,000 and £30,000 per QALY gained. |
1 Introduction
The National Institute for Health and Care Excellence (NICE) is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health in priority areas with significant impact. Health technologies must be shown to be clinically effective and to represent a cost-effective use of National Health Service (NHS) resources in order for NICE to recommend their use within the NHS in England. The NICE Single Technology Appraisal (STA) process usually covers new health technologies within a single indication, soon after their UK market authorisation [1]. Within the STA process, the company provides NICE with a written submission, alongside a mathematical model that summarises the company’s estimates of the clinical and cost effectiveness of the technology. This submission is reviewed by an external organisation independent of NICE (the Evidence Review Group [ERG]), which consults with clinical specialists and produces a report. After consideration of the company’s submission, the ERG report and testimony from experts and other stakeholders, the NICE Appraisal Committee (AC) formulates preliminary guidance—the Appraisal Consultation Document (ACD), which indicates the initial decision of the AC regarding the recommendation (or not) of the technology. Stakeholders are then invited to comment on the submitted evidence and the ACD, after which a further ACD may be produced or a Final Appraisal Determination (FAD) issued, which is open to appeal. An ACD is not produced when the technology is recommended within its full marketing authorisation; in this case, a FAD is produced directly.
This paper presents a summary of the ERG report [2] for the STA of ponatinib for the treatment of chronic phase (CP), accelerated phase (AP) or blast phase (BP) chronic myeloid leukaemia (CML) in patients whose disease is resistant to dasatinib or nilotinib, who are intolerant to dasatinib or nilotinib and for whom subsequent treatment with imatinib is not clinically appropriate, or who have the Threonine-315-Isoleucine (T315I) mutation. A summary of the subsequent development of the NICE guidance for the use of this technology in England is also provided. Full details of all relevant appraisal documents (including the appraisal scope, ERG report, company and consultee submissions, FAD and comments from consultees) can be found on the NICE website [2].
2 The Decision Problem
CML is a rare type of cancer affecting the blood and is characterised by a proliferation of granulocytes in the bone marrow and blood [3]. Approximately 95% of patients with CML have an acquired chromosomal abnormality (known as Philadelphia chromosome-positive disease, Ph+) caused by reciprocal translocations between chromosomes 9 and 22 [3, 4]. CML occurs in all age groups, but is most common in older adults (median age at diagnosis in the UK is 59 years) [5]. CML is typically characterised as having three distinct phases: the initial indolent chronic phase (CP-CML) that lasts for several years, an intermediate accelerated phase (AP-CML) that lasts for < 1–1.5 years, and an aggressive blast phase (BP-CML) that is usually fatal within 3–6 months [6]. The stage of the disease at diagnosis is an important prognostic factor and may predict the pattern of disease progression [7]. In general, around 90% of CML cases are diagnosed during the chronic phase, with approximately 40% being asymptomatic and diagnosed as a result of a routine blood test [3]. From the chronic phase, patients with CML either go through the accelerated phase or move directly into blast crisis, in which the disease transforms into a fatal acute leukaemia [3]. The phases are defined mainly by the percentage of blast cells in the blood and bone marrow [8].
2.1 Current Treatment
The management of patients with CML is complex. Allogeneic stem cell transplant (allo-SCT) is the only potentially curative treatment for CML. However, it is associated with a substantial rate of morbidity and mortality and is therefore limited by patient suitability as well as the availability of suitable donors [9]. The use of oral tyrosine kinase inhibitors (TKIs) has become the mainstay of treatment in CML. Currently, five TKIs (imatinib [10], dasatinib [11], nilotinib [12], bosutinib [13] and ponatinib [14]) have a European Union marketing authorisation for the treatment of CML.
Guidance issued by NICE recommends imatinib (standard dose) or dasatinib and nilotinib (with a Patient Access Scheme [PAS]) as first-line treatment options for adults with Ph+ CP-CML [15]. Imatinib is also recommended as an option for the treatment of patients with Ph+ CML who initially present in the AP or BP, and for CML that presents in the CP and then progresses to the AP/BP, if imatinib has not been used previously (see TA70) [16]. It is noteworthy that the UK patent protection for imatinib was expected to expire during the STA and substantial cost reductions were expected with generic imatinib [17], which may lead to the potential for increased uptake. For second- and subsequent-line treatments, NICE recommends dasatinib and nilotinib (with a PAS) for patients with Ph+ CP-CML and AP-CML where treatment with imatinib is not tolerated or where there is resistance [18].
Furthermore, sequential use of second-generation TKIs such as dasatinib after nilotinib is common in UK clinical practice and is also recommended in European clinical practice guidelines [9]. However, there is a lack of clinical evidence to support the benefit of sequential use of second-generation TKIs in patients who are resistant/intolerant to prior therapy and sequential use is not an approved indication for these drugs [10, 11].
Bosutinib (with a PAS) was recently recommended by NICE as an option, within its conditional marketing authorisation, for Ph+ CP, AP- and BP-CML in adults when they have previously had one or more TKI, and imatinib, nilotinib and dasatinib are not appropriate [19]. The ERG notes that although bosutinib may be an option for some patients as a second-line treatment (if other second-generation TKI drugs are not suitable), bosutinib is likely to be predominantly used third-line or later in clinical practice [20]. Other treatment options for patients with TKI resistant/intolerant CML include interferon alfa (in rare cases), best supportive/palliative care (including hydroxycarbamide), and allo-SCT.
3 The Independent Evidence Review Group (ERG) Review
In accordance with the process for STAs, the ERG and NICE had the opportunity to seek clarification on specific points in the company’s submission (CS) [21], in response to which the company provided additional information [22]. The ERG also modified the company’s decision analytic model to produce an ERG base case and to assess the impact of alternative parameter values and assumptions on the model results. The evidence presented in the company’s submission and the ERG’s review of that evidence is summarised here.
3.1 Clinical Evidence Provided by the Company
The CS [21] included a systematic review of the clinical effectiveness evidence of ponatinib for the treatment of CML. In the absence of randomised controlled trial evidence, the company identified two relevant single-arm, non-comparative studies (a phase I dose finding study [23, 24] and a phase II study) [25,26,27]. However, the design and context of the phase I study was not deemed entirely relevant to either the recommended dose or the licenced indication. As such, evidence from the phase II PACE (Ponatinib Ph-positive acute lymphoblastic leukaemia [ALL] and CML Evaluation) study formed the main pivotal evidence in the CS [21]. In reporting the data, 95% confidence intervals (CI) are replicated where these were provided by the company.
The PACE study was an industry-sponsored, single-arm, non-comparative, open-label, multicentre study (66 sites across 12 countries including five sites in the UK) designed to evaluate the efficacy and safety of ponatinib (administered orally at a starting dose of 45 mg once daily), in 449 patients (53% male; 78% Caucasian) with CP-CML (n = 270), AP-CML (n = 85), BP-CML (n = 62) or Ph+ ALL (n = 32) who were resistant or intolerant to either dasatinib or nilotinib, or who had the T315I mutation after any TKI therapy (as confirmed by direct sequencing) [26, 28, 29].
Study participants in the PACE study were heavily pre-treated with prior TKIs and conventional therapy: 37% (167/449) had received two TKIs (imatinib, dasatinib, nilotinib or bosutinib). This population comprised the target population in the company’s decision problem for CP-CML, AP-CML and BP-CML (i.e. in the third-line treatment setting), reflecting the anticipated place in therapy of ponatinib, after treatment failure with imatinib and either nilotinib or dasatinib.
For CP-CML patients, the primary outcome measure was the proportion of patients achieving major cytogenetic response (MCyR, defined as complete cytogenetic response or partial cytogenetic response) within 12 months of starting treatment. For patients with AP-CML and BP-CML, the primary outcome measure was the proportion of patients achieving a major haematological response (MaHR, defined as complete haematological response or no evidence of leukaemia, confirmed by blood analyses) within 6 months of starting treatment.
Among the subgroup of CP-CML patients who received third-line ponatinib (i.e. the main target population in the CS), 67% (95% CI 57–76) achieved MCyR by 12 months (primary endpoint). In an updated analysis (at a median follow up of 48.2 months) [27], 71% of CP-CML patients (n = 97) achieved MCyR and an estimated 88% of responding patients maintained this response for at least 3 years. At 4 years, progression-free survival (defined as death, development of AP or BP, loss of complete haematological response in absence of cytogenetic response, loss of MCyR, or increasing white blood cell count without complete haematological response) and overall survival rates in CP-CML patients who received ponatinib third-line were 68 and 79%, respectively (median not reached for either outcome). Ponatinib is the only TKI with activity against the T315I mutation. Among the subgroup of CP-CML patients who had the T315I mutation (n = 64, all lines [data were not reported separately by line of therapy]) [26], 70% achieved an MCyR by 12 months. In an updated analysis at 4 years [30], 72% of CP-CML patients achieved a MCyR, progression-free survival was 56% and overall survival was 72%.
In the subgroup of AP-CML patients (n = 33) who received ponatinib third-line, 61% had an MaHR within the first 6 months (primary endpoint). Among those who had the T315I mutation (n = 18, all lines), 50% achieved an MaHR by 6 months. Overall and progression-free survival was not reported. Among patients with BP-CML (all lines, n = 62 [data not reported separately by line of therapy]), 31% (95% CI 20–44) achieved an MaHR within the first 6 months (primary endpoint). The rates of progression-free survival and overall survival at 12 months were estimated to be 19% (median 4 months) and 29% (median 7 months), respectively. Among the BP-CML patients who had the T315I mutation (n = 24, all lines), 29% had an MaHR within the first 6 months [26]. Overall and progression-free survival was not reported. The ERG believes that caution should be used in the interpretation of the data because of the small population size and study design limitations.
At the latest data cut for treatment discontinuation among CML patients who received at least one dose of the study drug (all lines), 18.5% of CP-CML patients (n = 270), 11.8% of AP-CML patients (n = 85), and 14.5% of BP-CML patients (n = 62) withdrew from treatment because of adverse events [26].
In terms of safety, at the last data-cut where data can be presented, the following severe or life-threatening treatment-related adverse events were observed: thrombocytopenia (CP-CML 32%, AP-CML 33%, BP-CML 26%), neutropenia (CP-CML 14%, AP-CML 26%, BP-CML 18%); increased lipase (CP-CML 10%, AP-CML 13%, BP-CML 11%) and anaemia (CP-CML 6%, AP-CML 9%, BP-CML 21%). All other serious or life-threatening treatment-related adverse events occurred in < 10% of patients [26].
Given the absence of any head-to-head studies comparing ponatinib with other relevant comparators for the treatment of CP-CML, the company undertook a matching-adjusted indirect comparison (MAIC) to facilitate an indirect comparison between treatments and to inform the economic model. The objective of the MAIC was to adjust outcomes to account for imbalances between treatments in (observed) prognostic factors in different studies; prognostic factors were T315I mutation status, sex, median age, race, duration of CML, and Eastern Cooperative Oncology Group (ECOG) performance status. The main effectiveness outcome measures for the MAIC were cytogenetic best response rates, haematological best response rates and duration of response. The MAIC adjusted responses to ponatinib in the PACE study (phase II) as if ponatinib had been included in the phase I/II study [31] that evaluated bosutinib rather than adjusting responses to bosutinib as if it had been included in the PACE study. From the MAIC, the company estimated that ponatinib provided considerably higher complete cytogenetic response rates than bosutinib in the third-line (61 versus 24%). The ERG’s main critique of the MAIC was that indirect estimates of treatment effect may be biased as a consequence of unmeasured confounders, although clinical input to the ERG did not highlight any important omissions. In addition, no adjustment was made to other outcomes, including overall survival and adverse events, or for any AP-CML and BP-CML outcomes.
3.1.1 Critique of the Clinical Evidence and Interpretation
The systematic review process followed by the company was reasonably comprehensive. Despite minor limitations in the company’s search strategy, the ERG was reasonably confident that all relevant published studies (randomised controlled and non-randomised/non-controlled evidence) of ponatinib were included in the CS, including data from ongoing studies. Based on the quality assessment tool for non-randomised studies [32], the ERG considered the PACE study to be a well reported and conducted single-arm study. However, single-arm studies are associated with an array of potential biases [33], including a high risk of selection bias (because of the absence of randomisation), and performance and detection bias (because of the absence of blinding) [34, 35]. In addition, because of the absence of a comparator group in the PACE study, inferences about treatment effects were made indirectly to a phase I/II study of bosutinib using MAIC as if ponatinib had been included in that study. A further limitation to the robustness of the efficacy and safety data relate to the small subgroups that comprise the target population in the CS.
The key uncertainties in the clinical evidence relate to optimal dosing, duration of treatment and the unbiased estimate of treatment effect. In the PACE study [26], patients received an initial dose of ponatinib 45 mg orally once daily; however, dose adjustments (e.g. lowering of the dose to 30 or 15 mg once daily and frequency of treatment) were allowed for the management of treatment toxicity. As such, it remains unclear if the adjusted lower dosing regimens would have been clinically effective over the entire PACE study period. In addition, no data were available on the alternative treatments given to patients who stopped study treatment in the PACE study. Clinical advisors to the ERG commented that in UK practice, stopping treatment is dependent on patient choice, but clinicians would discourage patients from doing so if they were not in complete remission. The summary of product characteristics posology recommends considering discontinuing ponatinib if a complete haematological response has not occurred by 3 months (90 days) [14]. The PACE study reported outcomes over a median follow-up of 48.2 months (4 years) [27]. As a result, the longer-term safety and efficacy of ponatinib is currently unknown.
3.2 Cost-Effectiveness Evidence Provided by the Company
The company developed two health economic models to assess the cost effectiveness of ponatinib for the treatment of patients in CP-CML or in advanced CML (AP- or BP-, which were modelled separately). Both models adopted the perspective of the NHS and Personal Social Services over a lifetime horizon and discounted both quality-adjusted life-years (QALYs) and costs at a rate of 3.5% per annum. The model employed a state transition approach, with 3-monthly time cycles and included a half-cycle correction. The models that were originally submitted were amended by the company following the clarification process: only the revised models are detailed here. The company initially provided a simple discount to the price of ponatinib via a PAS, the value of which is commercial in confidence. During the consultation process, the company submitted a revised PAS, with a larger discount. Only results incorporating the revised PAS are presented within this report.
3.2.1 Model Structures Presented by the Company
3.2.1.1 Chronic Phase (CP)-Chronic Myeloid Leukaemia (CML) Model
Within the CP-CML model, a hypothetical patient could receive one of five interventions: (1) ponatinib; (2) bosutinib; (3) hydroxyurea, representing best supportive care (BSC); (iv) interferon alfa; or (v) allo-SCT.
The simulated patients receiving non-allo-SCT treatments were distributed amongst four response states: (1) complete cytogenic response (CCyR); (2) partial cytogenic response (PCyR); (3) complete haematological response (CHR); or (iv) no response (NR). In subsequent cycles, patients receiving pharmacological treatments could continue in their current response state, experience disease progression to AP-CML, lose response within the CCyR and PCyR states, or die. Patients receiving an allo-SCT could continue in a post allo-SCT state, experience remission or die. Patients were at risk of all-cause mortality and CML-associated mortality. However, CML-associated mortality applied only to patients who had progressed to AP-CML. All-cause mortality was based on mortality functions for the general population [36]. Patients receiving allo-SCT in the CP-CML state were assumed to enter a relapse-free state from which they could die or relapse; within the relapse state only death could occur. Following allo-SCT the model assumed the same life expectancy for those who relapsed and for those who did not, although a utility difference was assumed.
A key driver of patients’ long-term prognoses, both in terms of life expectancy and utility, is the assumed response rates for non-allo-SCT treatments. As previously stated, these were divided into CCyR, PCyR, CHR and NR for those in CP-CML, whereas for those in AP-CML and BP-CML there were only two health states: MaHR or NR.
In patients with CP-CML, response probabilities for ponatinib were taken from the PACE study [26], whilst probabilities for bosutinib were taken from Khoury et al. [31]. The company assumed that patients receiving BSC or interferon alfa would not achieve either CCyR or PCyR but could achieve CHR with a probability taken from Dalziel et al. [37]. The response probabilities assumed by the company for each treatment are presented in Table 1. The summary of product characteristics [38] suggest stopping ponatinib if there had not been at least a CHR in the initial 3 months, and reducing the dosage to 15 mg if there has been an MaHR. The model assumed that ponatinib treatment was discontinued if the patient experienced NR.
The duration of response in CP-CML before progression to AP-CML was taken from the BMS-043 study reported by Loveman et al. [39] and reproduced in Table 2. These data were extrapolated using survival functions which were chosen by the company based on the observed fit, using the Akaike information criterion (AIC) and Bayesian information criterion (BIC) and clinical plausibility. Gompertz distributions were chosen for CCyR and PCyR, a Weibull distribution was used for CHR, and an exponential distribution for NR.
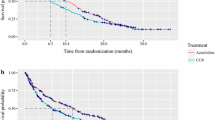
Loss of CCyR and PCyR responses were assumed to differ between bosutinib and ponatinib. For ponatinib, the company fitted standard parametric models to data from the PACE study [26] for patients with CCyR and PCyR using response level as a covariate. The Gompertz distribution was selected by the company as most appropriate for loss of response. For bosutinib, data from Gambacorti-Passerini et al. [40], which combined patients with PCyR and CCyR, were digitised by the company parameters estimated using the Solver function in Microsoft Excel® by minimising the sum of squared errors (SSE) for different survivor functions. Although this method provides estimates of the parameters for each survivor function, it provides no meaningful estimates of the variances (and covariances) associated with the parameters. The Gompertz distribution was selected by the company as most appropriate for loss of response and used for patients with either a CCyR or a PCyR.
Time until treatment discontinuation was assumed to differ between ponatinib and bosutinib. For bosutinib the company used data from Khoury et al. [31] to fit an exponential distribution, which was assumed applicable for CCyR, PCyR and CHR. For ponatinib, the company fitted standard parametric models separately to CCyR, PCyR and CHR using data from the PACE study [26] and selected the exponential distribution in all cases “for consistency with the function used for bosutinib”. Patients discontinuing treatment in CCyR were assumed to remain in that state. Patients discontinuing in the PCyR and CHR states were allocated to either the CHR state (41%) or the NR state (59%) based on the reported efficacy of hydroxyurea [37], which was assumed to be generalisable to BSC. Patients receiving interferon alfa or BSC would not have their treatment discontinued.
The pathway for patients who progressed to AP-CML from CP-CML was dependent on whether the patient was suitable for allo-SCT, the proportion of which was assumed to be 27.3% based on a UK survey conducted by the company. Following progression from the CP-CML health state, the model estimated the costs incurred and QALYs accrued in the AP-CML and the BP-CML phases and added these to the values accrued in the CP-CML stage.
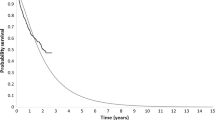
For those patients in AP-CML not suitable for allo-SCT, possible transitions were to BP-CML or death. The company assumed that whilst in AP-CML patients would be treated with one of the following: (dasatinib, nilotinib, bosutinib, imatinib and BSC), with each having a 20% proportion of market share. The probability of death in AP-CML was estimated by the company using data from Kantarjian et al. [41]. The data were digitised and parametric distributions were fitted to the data in Microsoft Excel. The company selected the log-normal distribution as the most appropriate distribution. The risk of progression from AP-CML to BP-CML was estimated by the company using data in Kantarjian et al. [41], which reported that the mean progression-free survival in AP-CML was 9.16 months; this value was used to derive an exponential function. For patients who progressed to BP-CML, the probability of death was estimated using data from Kantarjian et al. [41] and the method used in AP-CML. The company selected the log-logistic distribution as the most appropriate distribution. The duration in AP-CML before progressing to BP-CML was considered independent of prior treatment in CP-CML. Overall survival was extrapolated with the company selecting the log-normal distribution for overall survival in AP-CML and the log-logistic distribution in BP-CML.
For patients suitable for allo-SCT, the durations of overall survival were extrapolated by fitting parametric survival models to data extracted from an observational study conducted by Jabbour et al. [42]. The company selected the exponential distribution for both CP-CML and AP-CML; patients in the CP-CML model were assumed ineligible to receive an allo-SCT if they had progressed to BP-CML. The company assumed that relapse-free survival following allo-SCT was the same regardless of whether the patient was in CP-CML or AP-CML. The duration of relapse-free survival data were extrapolated by fitting parametric survival models to data reported in Craddock et al. [43].
The model included the following ponatinib-related serious adverse events: arterial occlusive events (cardiovascular, cerebrovascular, peripheral vascular events) and venous thromboembolism events, which were assumed to have a risk of recurrence. Other serious adverse events (grade 3 or 4) were included if at least 5% of the PACE study population experienced the event, but these were only assumed to occur in the first cycle (3 months). Patients treated with bosutinib were assumed to have no serious adverse events as reported in Kantarjian et al. [44]. BSC, interferon alfa, and allo-SCT were not assumed to have adverse events, although the mortality rates after allo-SCT were assumed to be significantly higher than in the general population with CP-CML. The same adverse events were included in the AP- and BP-CML models, although the incidence differed by stage of CML.
Health-related quality of life data used in the model were based on those reported by Kind et al. [45]. The model used utility decrements for the various disease states based on data reported by Szabo et al. [46]. The disutility associated with CP-CML, AP-CML and BP-CML were 0.116, 0.316 and 0.556, respectively. CP-CML patients who have CCyR were assumed to experience no disease-related disutility. The disutility associated with adverse events serious enough to require treatment discontinuation (0.326) was taken from Szabo et al. [46]. Disutility following allo-SCT was assumed to decrease over time. Disutility in the first 3 months was 0.296 based on data reported by van Agthoven et al. [47]. Disutility 6 months after allo-SCT was 0.136 based on data in Loveman et al. [39], with the average of these two values used for the 3- to 6-month period after allo-SCT. Following relapse after an allo-SCT, a disutility of 0.260 was used based on data reported by Kantarjian et al. [48] and Olavarria et al. [49]. These utility data were also used in the AP- and BP-CML models.
The cost of 3 months of treatment with bosutinib, interferon alfa and hydroxyurea were assumed to be £10,714, £6833 and £38, respectively. The cost associated with an allo-SCT was £60,092 with follow-up costs of £12,215, £3518 and £420 in years 1, 2 and 3 and subsequent, respectively, based on data from the UK stem-cell oversight committee [50] and the health technology assessment (HTA) report published for bosutinib [20]. The cost of ponatinib was commercial-in-confidence because of both the PAS and the relative dose intensity observed in the PACE study [26]. These cost data were also used in the AP- and BP-CML models. The components of each cost estimate were valued at 2014/15 prices unless a more recent value was available.
For non-allo-SCT patients, based on a survey undertaken by the company, the number of days in hospital per cycle was assumed to be zero for those with CP-CML, 2.13 days for patients with AP-CML and 26.64 for patients with BP-CML. Monitoring costs were assumed to be independent of treatment. The per-cycle hospitalisation and monitoring costs for CP-CML (responding), CP-CML (non-responding), AP-CML and BP-CML were £208, £495, £2648 and £20,319, respectively. End-of-life care was assumed to cost £5766 based on resource use estimated in a UK clinical expert survey conducted by the company. These cost data were also used in the AP- and BP-CML models. The components of each cost estimate were valued at 2014/15 prices unless a more recent value was available.
3.2.1.2 Accelerated Phase (AP)- and Blast Crisis Phase (BP)-CML Models
The CP-CML model structure described earlier was used to evaluate the cost effectiveness of ponatinib for both patients with AP-CML and for patients with BP-CML. Having entered the model, a hypothetical patient could receive one of four treatments: (1) ponatinib; (2) bosutinib; (3) BSC or (4) immediate allo-SCT, if the patient was eligible. Ponatinib and bosutinib were used as a bridge to allo-SCT, with patients experiencing an MaHR progressing to allo-SCT.
Simulated patients who entered the model after receiving ponatinib or bosutinib had one of two responses: MaHR or NR. MaHR could only occur in the first cycle (3 months), with patients achieving MaHR receiving an allo-SCT. Patients who entered the AP-CML model and had NR were assumed to discontinue ponatinib treatment but not bosutinib. These patients could remain in NR, progress to BP-CML where BSC is provided, or die. Patients who received an allo-SCT entered a post-allo-SCT health state and in subsequent cycles either remained in that state or died. The prognoses for patients who received an allo-SCT after achieving an MaHR were assumed better than for patients who had allo-SCT immediately.
Patients who enter the model with BP-CML could receive ponatinib, bosutinib or BSC. Patients experiencing an MaHR will receive an allo-SCT, the remainder discontinue ponatinib treatment, but not bosutinib treatment, and in each cycle remain in NR or die. MaHR response data for each treatment are presented in Table 3 and represent a naïve indirect comparison.
Patients in AP-CML who had allo-SCT after an MaHR were assumed to remain in this state until death. The assumed probability of death was estimated from data in Radich [51], which provided data on the following three groups of patients: (1) those with AP-CML; (2) those with BP-CML in remission; and (3) those with BP-CML without remission. Patients with MaHR in AP-CML were assumed to be equivalent to those reported as in AP-CML by Radich [51]. Parametric functions were fitted to the data by minimising the SSE, as previously described. The company did not select the distribution that fitted best according to AIC and BIC (the Gompertz distribution), but instead selected the exponential distribution as this was believed by the company to be more clinically plausible (i.e. constant hazards).
For patients with AP-CML who had NR, the time to progression to BP-CML was estimated by fitting parametric survival distributions to the data from the PACE study [26]. These data were marked as academic-in-confidence by the company. The survivor function used by the company relating to death for patients with AP-CML whilst in NR was also marked as academic-in-confidence.
Patients in AP-CML who had allo-SCT on entering the model were assumed to remain in this state until death. The probability of death was derived from Radich [51] assuming that the ratio between the two functions relating to BP-CML (remission and non-remission) would be applicable in AP-CML and that patients who had allo-SCT directly on entering the model were equivalent to AP-CML without remission, whereas those who had allo-SCT after MaHR were equivalent to allo-SCT with remission.
For patients with BP-CML who had NR, the time to death was estimated by fitting parametric distributions to data from the PACE study [26]. These data were marked as academic-in-confidence by the company. The time to death for those who experienced NR whilst on bosutinib treatment was assumed to be equal to that of those who had received ponatinib treatment. For patients receiving BSC, the probability of death was estimated using data from Kantarjian et al. [41].
3.2.2 Results Presented by the Company
As advised by NICE, all results presented by the company used the discounted price for ponatinib but the list price for comparators.
3.2.2.1 CP-CML Model
Following the clarification process, the base-case incremental cost-effectiveness ratios (ICERs) estimated by the company for ponatinib versus bosutinib, BSC, interferon alfa and allo-SCT were £18,213; £15,200; £4042 and £6395 per QALY gained, respectively. The probabilistic analysis of ponatinib versus bosutinib produced an ICER of £20,657 per QALY gained. The company conducted a number of sensitivity analyses, which showed that the results were sensitive to the costs associated with hospital admission in BP-CML.
3.2.2.2 AP-CML Model
Following the clarification process, the base-case ICER estimated by the company for ponatinib versus bosutinib, BSC and immediate allo-SCT were dominant, £14,750 and £13,279 per QALY gained, respectively. The probabilistic analysis of ponatinib versus BSC produced an ICER of £13,481 per QALY gained. The company conducted a number of sensitivity analyses which showed that the results were relatively robust to the changes explored.
3.2.2.3 BP-CML Model
Following the clarification process, the base-case ICER estimated by the company for ponatinib versus BSC, immediate allo-SCT and bosutinib were dominant, dominant and £17,601 per QALY gained, respectively. The probabilistic analysis of ponatinib versus bosutinib produced an ICER of £16,229 per QALY gained. The company conducted a number of sensitivity analyses which showed that the results were sensitive to the costs of hospitalisation in the BP-CML phase.
3.3 Critique of the Cost-Effectiveness Evidence and Additional Work Undertaken by the ERG
The ERG undertook a number of exploratory deterministic sensitivity analyses. Analyses that noticeably changed the ICER are detailed below.
First, the ERG believed that the company’s selection of distributions used for progression-free survival and overall survival functions was questionable. The ERG undertook further analyses to provide a range of plausible ICERs. The ERG generated parametric survival functions, where possible, using the method proposed by Guyot et al. [52] to reconstruct patient-level data and then using maximum likelihood estimation to fit the parametric distributions. Analyses were conducted in R using flexsurvreg. Second, clinical advice to the ERG suggested that the assumption made by the company that any missed doses will be saved by patients for later use (resulting in fewer packs of ponatinib and bosutinib being issued) was potentially plausible for patients in CP-CML but unlikely in AP- and BP-CML. The ERG conducted an analysis assuming full wastage of missed doses. Third, the company’s model assumes that treatment with bosutinib, unlike ponatinib, would continue for patients with NR in CP-CML, and for patients without MaHR in AP-CML and BP-CML. Based on clinical advice, the ERG adapted the model so that the same stopping rules applied to both ponatinib and bosutinib. Fourth, the company applied a half-cycle correction to the costs of pharmacological treatments. However, the ERG believes that once pharmacological treatments are issued to a patient, any unused drugs would be disposed of and thus the half-cycle correction was incorrect. The ERG acknowledges that this assumption will mean that costs are overestimated in this scenario as it unlikely that patients will be issued with 3 months’ treatment at once. Fifth, the survival estimated for these patients are not aligned with cost estimates. The ERG explored the impact of setting the costs of treatment after CP-CML progression and allo-SCT relapse equal to that of either BSC or the estimated costs of generic imatinib. Finally, the ERG explored the use of alternative survivor functions to those chosen by the company.
A summary of the results of the ERG’s exploratory analyses is provided. The ERG did not believe that interferon alfa would be on the efficiency frontier and so did not perform exploratory analyses versus this treatment. The ERG did not conduct further analyses comparing ponatinib with bosutinib in the AP- or BP-CML states as ponatinib was typically dominant. As instructed by NICE, the results presented by the ERG contain the PAS for ponatinib but not for comparator treatments.
3.3.1 CP-CML Model
The combination of recalculating the survivor functions, incorporating a 3-month stopping rule for bosutinib, removing half-cycle correction of interventions, reducing the costs associated with progressing beyond CP-CML, along with minor corrections, produced the following range of ICERs for ponatinib: £18,246–£27,667 per QALY gained compared with BSC; £19,680–£37,381 per QALY gained compared with bosutinib; and £18,279 per QALY gained to dominated compared with allo-SCT.
3.3.2 AP-CML Model
The combination of recalculating the survivor functions, adding in drug wastage, incorporating a 3-month stopping rule for bosutinib, removing half-cycle correction of interventions, along with minor corrections, produced the following range of ICERs for ponatinib: £7123–£17,625 per QALY gained compared with BSC; and from dominating to £61,896 per QALY gained compared with allo-SCT.
3.3.3 BP-CML Model
The combination of recalculating the survivor functions, adding in drug wastage, incorporating a 3-month stopping rule for bosutinib, removing half-cycle correction of interventions, along with minor corrections, produced the following range of ICERs for ponatinib: £5033 per QALY gained to dominated compared with allo-SCT, although likely to be at the more favourable end of this range; and dominant in all scenarios compared with BSC. The ERG did not conduct further analyses comparing ponatinib with bosutinib as ponatinib was typically dominant.
3.4 Conclusions of the ERG Report
The key clinical effectiveness evidence for ponatinib was derived from a single-arm study of patients with CML (CP, AP or BP). As such, an MAIC was conducted to compare the response rates for ponatinib with bosutinib only in CP-CML patients (comprehensive data were not available for the AP- or BP-CML group to allow the matching technique to be used). However, MAIC are biased because of unmeasured confounders. For AP- and BP-CML, naïve indirect comparisons (which were considered biased) were necessary to compare ponatinib against bosutinib (excluding CP-CML), allo-SCT and BSC. Naïve indirect comparison methods are considered to be equivalent to observational data and subject to similar biases [53, 54]. The exploratory analyses performed by the ERG provided the AC with ranges in which the ICERs were likely to lie for patients with CP-, AP-, and BP-CML. These ranges included values which fell both below and above NICE’s reported cost-effectiveness thresholds, typically between £20,000 and £30,000 per QALY gained.
4 Key Methodological Issues
Naïve indirect comparison methods are considered to be equivalent to observational data and subject to similar biases. Furthermore, analyses based on the MAIC approach are subject to potential biases because of unobserved confounders. As a result, the face validity of each naïve adjusted indirect comparison and MAIC should be carefully assessed.
The exploration of the impact of using alternative, plausible survival functions on the ICER was not undertaken by the company. The analyses undertaken by the ERG indicates that the range of the ICER was large and that a decision based on an ICER from a single survival function could be misleading.
5 National Institute for Health and Care Excellence Guidance
In June 2017, on the basis of the evidence available (including verbal testimony of invited clinical experts and patient representatives), the NICE Appraisal Committee (AC) produced guidance that ponatinib was recommended as an option for treating adults with CP-, AP- or BP-CML when the disease is resistant to dasatinib/nilotinib, or when the patient cannot tolerate dasatinib/nilotinib and for whom subsequent treatment with imatinib is not clinically appropriate, or the T315I gene is present and when the company provides the drug with the agreed PAS [55].
5.1 Consideration of Clinical and Cost-Effectiveness Issues Included in the Final Appraisal Determination (FAD)
This section summarises the key issues considered by the AC. The full list of the issues considered by the AC can be found in the FAD.[55]
5.1.1 Uncertainties in the Clinical Evidence
The AC noted the lack of a comparator in the PACE study [26], “but was aware of the ethical considerations (offering placebo to patients who have not responded to previous treatment) which prevented a randomised control trial design”. The AC was aware that for some patients in the study, the dosage was changed or treatment was stopped, which led to uncertainties about the best dosing level, the duration of treatment, and the generalisability of the reported outcomes. The committee concluded that despite these uncertainties the evidence presented was sufficient for decision making.
To allow for a comparison with bosutinib, the company presented an MAIC. The approach was only used for patients with CP-CML because comprehensive data were not available for the AP- or BP-CML groups to allow the matching technique to be used. The AC noted the limitations of the company’s MAIC but accepted that it could be used for decision making. However, the AC concluded that the company had neither properly explored the effect of alternative parametric distributions nor justified its chosen distribution, but concluded that the alternative fitting undertaken by the ERG was appropriate.
5.1.2 Uncertainties in the Economic Modelling
The AC noted that whilst the ERG stated that the probabilistic sensitivity analyses done by the company were not robust because of the inappropriate characterisation of uncertainty, including correlation, in survivor functions, and arbitrary choices of standard error to represent uncertainty, the model structure was appropriate for decision making.
Following testimony from clinical experts that stated that clinicians would stop treatment with bosutinib or ponatinib as soon as possible if the disease were no longer responding to treatment, the AC concluded that a 3-month stopping rule for bosutinib should be applied.
The AC concluded that drug wastage should be assumed in AP- and BP-CML, and that zero wastage was unlikely to occur in CP-CML, and that some allowance should have been made for this, although it noted that this had only a small effect on the ICER.
5.1.3 End-of-Life Criteria
The AC concluded that the end-of-life criteria (a survival of < 2 years and an extension of life of > 3 months) had been met for the following groups only: for patients with AP-CML for whom allo-SCT or bosutinib were not appropriate and for patients with BP-CML.
6 Conclusions
The AC recognised that there was considerable uncertainty in the value of the ICERs, and therefore their most likely value fell within a range. The AC concluded that in all instances this range, when including PAS of other interventions used in the treatment of CML, included cost-effective values, and therefore ponatinib was a cost-effective use of NHS resources.
References
National Institute for Health and Care Excellence (NICE). Guide to the methods of technology appraisal 2013—process and methods [PMG9]. London: NICE. 2013. https://www.nice.org.uk/article/pmg9/. Accessed 23 Nov 2016.
Pandor A, Stevenson M, Martyn-St James M, Stevens J, Hamilton J, Rawdin A et al. Ponatinib for treating chronic myeloid leukaemia: a single technology Appraisal. School of Health and Related Research (ScHARR). 2016. https://www.nice.org.uk/guidance/ta451/documents/committee-papers Accessed 20 Nov 2017.
National Institute for Health and Care Excellence (NICE). Dasatinib, high-dose imatinib and nilotinib for the treatment of imatinib-resistant chronic myeloid leukaemia (CML) (part review of NICE technology appraisal guidance 70), and dasatinib and nilotinib for people with CML for whom treatment with imatinib has failed because of intolerance. Technology appraisal TA241. London: NICE. 2012. https://www.nice.org.uk/guidance/ta241. Accessed 23 Nov 2016.
Goldman J. Chronic myeloid leukaemia. Medicine. 2009;37(4):195–7.
Roman E, Smith A, Appleton S, Crouch S, Kelly R, Kinsey S, et al. Myeloid malignancies in the real-world: occurrence, progression and survival in the UK’s population-based Haematological Malignancy Research Network 2004–2015. Cancer Epidemiol. 2016;42:186–98.
Kantarjian HM, Deisseroth A, Kurzrock R, Estrov Z. M. T. chronic myelogenous leukemia: a concise update. Blood. 1993;82(3):691–703.
Karbasian Esfahani M, Morris EL, Dutcher JP, Wiernik PH. Blastic phase of chronic myelogenous leukemia. Curr Treat Options Oncol. 2006;7(3):189–99.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: chronic myelogenous leukemia. Version 1.0. 2016. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed 23 Nov 2016.
Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 2013;122(6):872–84.
Novartis Europharm Limited. Glivec® (imatinib) 50-mg and 100-mg hard capsules and 100-mg and 400-mg film-coated tablets: summary of product characteristics. [Updated 28 Nov 2016]. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000406/WC500022207.pdf Accessed 1 Dec 2016.
Bristol-Myers Squibb Pharma. Sprycel® (dasatinib) 20-mg, 50-mg, 70-mg, 80-mg, 100-mg, 140-mg film-coated tablets: summary of product characteristics. [Updated 20 Jul 2016]. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000709/WC500056998.pdf Accessed 1 Dec 2016.
Novartis Europharm Limited. Tasigna® (nilotinib) 150-mg and 200-mg hard capsules: Summary of Product Characteristics. [Updated 29 Sept 2016]. Camberley, UK. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000798/WC500034394.pdf. Accessed 1 Dec 2016.
Pfizer Ltd. Bosulif® (bosutinib) 100-mg and 500-mg film-coated tablets: Summary of Product Characteristics. [Updated 10 Jun 2016]. Sandwich, UK. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002373/WC500141721.pdf Accessed 1 Dec 2016.
ARIAD Pharma Ltd. Iclusig® (ponatinib) 15-mg, 30-mg, and 45-mg film-coated tablets: summary of product characteristics. [Updated 16 Sept 2016]. 2016. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002695/WC500145646.pdf Accessed 1 Dec 2016.
National Institute of Health and Care Excellence (NICE). Dasatinib, nilotinib and imatinib for untreated chronic myeloid leukaemia - Technology appraisal guidance [TA426]. NICE, London. 2016. https://www.nice.org.uk/guidance/ta426 Accessed 22 Nov 2017.
National Institute for Health and Care Excellence. Guidance on the use of imatinib for chronic myeloid leukaemia. Technology appraisal guidance [TA70]. London: NICE. 2003. https://www.nice.org.uk/guidance/ta70. Accessed 23 Nov 2016.
Hill A, Gotham D, Fortunak J, Meldrum J, Erbacher I, Martin M, et al. Target prices for mass production of tyrosine kinase inhibitors for global cancer treatment. BMJ Open. 2016;6(1):e009586.
National Institute for Health and Care Excellence (NICE). Dasatinib, nilotinib and high-dose imatinib for treating imatinib-resistant or intolerant chronic myeloid leukaemia—technology appraisal guidance [TA425]. NICE, London. 2016. https://www.nice.org.uk/guidance/ta425. Accessed 20 Nov 2017.
National Institute for Health and Care Excellence. Ponatinib for treating chronic myeloid leukaemia and acute lymphoblastic leukaemia. Final Scope. National Institute for Health and Care Excellence (NICE), London. 2016. https://www.nice.org.uk/guidance/ta451/documents/committee-papers. Accessed 20 Nov 2017.
National Institute for Health and Care Excellence (NICE). Bosutinib for previously treated chronic myeloid leukaemia. Technology appraisal guidance [TA401]. London: NICE. 2016. https://www.nice.org.uk/guidance/ta401. Accessed 23 Nov 2016.
Incyte Corporation. Ponatinib for treating chronic myeloid leukaemia and acute lymphoblastic leukaemia[ID671]. Company’s evidence submission to the National Institute for Health and Care Excellence. 2016. https://www.nice.org.uk/guidance/ta451/documents/committee-papers. Accessed 22 Nov 2017.
Incyte Corporation. Ponatinib for treating chronic myeloid leukaemia and acute lymphoblastic leukaemia[ID671]. Response to clarification letter. 2016. https://www.nice.org.uk/guidance/ta451/documents/committee-papers. Accessed 22 Nov 2017.
Cortes JE, Kantarjian H, Shah NP, Bixby D, Mauro MJ, Flinn I, et al. Ponatinib in refractory philadelphia chromosome-positive leukemias. N Engl J Med. 2012;367(22):2075–88. https://doi.org/10.1056/NEJMoa1205127.
Talpaz M, Cortes JE, Kantarjian HM, Shah NP, Bixby DL, Flinn I, et al. Four-year minimum follow-up of ongoing patients (pts) with chronic-phase chronic myeloid leukemia (CP-CML) in a phase 1 trial of ponatinib (PON). J Clin Oncol. 2015;33(15_suppl):7047 (Meeting Abstracts).
Cortes JE, Kim D-W, Pinilla-Ibarz J, le Coutre P, Paquette R, Chuah C, et al. Ponatinib efficacy and safety in heavily pretreated leukemia patients: 3-year results of the pace trial. P234. Haematologica. 2015;100(S1):64.
Cortes JE, Kim D-W, Pinilla-Ibarz J, le Coutre P, Paquette R, Chuah C, et al. A phase 2 trial of ponatinib in philadelphia chromosome-positive leukemias. N Engl J Med. 2013;369(19):1783–96. https://doi.org/10.1056/NEJMoa1306494.
Hochhaus A, Cortes JE, Kim DW, Pinilla-Ibarz J, le Coutre PD, Paquette R, et al. Efficacy and safety of ponatinib in CP-CML patients by number of prior tyrosine kinase inhibitors: 4-year follow-up of the phase 2 PACE trial. Blood. 2015;126(23):4025.
European Medicines Agency (EMA). Assessment Report for Inclusig® (ponatinib). Procedure No EMEA/H/C/002695/0000. London: EMA. 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/002695/WC500145648.pdf. Accessed 23 Nov 2017.
U.S. Food and Drug Administration Center for Drug Evaluation and Research. Application number: 203469Orig1s000 medical review. 2012. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/203469Orig1s000MedR.pdf. Accessed 23 Nov 2016.
Cortes JE, Pinilla-Ibarz J, Le Coutre PD, Paquette R, Chuah C, Nicolini FE, et al. 4-year results of the ponatinib phase II PACE trial in patients (pts) with heavily pretreated leukemia. J Clin Oncol. 2016;34(suppl; abstr 7013).
Khoury HJ, Cortes JE, Kantarjian HM, Gambacorti-Passerini C, Baccarani M, Kim DW, et al. Bosutinib is active in chronic phase chronic myeloid leukemia after imatinib and dasatinib and/or nilotinib therapy failure. Blood. 2012;119(15):3403–12. https://doi.org/10.1182/blood-2011-11-390120.
Chambers D, Rodgers M, Woolacott N. Not only randomized controlled trials, but also case series should be considered in systematic reviews of rapidly developing technologies. J Clin Epidemiol. 2009;62(12):1253–60. https://doi.org/10.1016/j.jclinepi.2008.12.010.
Evans S. Clinical trial structures. J Exp Stroke Transl Med. 2010;3(1):8–18.
Centre for Reviews and Dissemination. Systematic review: CRD’s guidance for undertaking reviews in health care. CRD, University of York. 2009. https://www.york.ac.uk/crd/SysRev/!SSL!/WebHelp/SysRev3.htm Accessed 23 Nov 2016.
Higgins JPT, Green S (ed). Cochrane handbook for systematic reviews of interventions version 5.1.0 [Updated Mar 2011]. The Cochrane Collaboration. 2011. www.handbook.cochrane.org. Accessed 23 Nov 2016.
Office for National Statistics. Interim life tables: England [Internet]. [Updated 23 Sept]. 2015 http://www.ons.gov.uk/ons/taxonomy/index.html?nscl=Interim+Life+Tables#tab-data-table. Accessed 23 November 2016.
Dalziel K, Round A, Stein K, Garside R, Price A. Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis. Health Technol Assess Winch, Engl. 2004;8(28):iii (1–120).
Incyte Biosciences UK Ltd. Iclusig 15 mg 30 mg and 45 mg film-coated tablets. 2017. https://www.medicines.org.uk/emc/medicine/28145 Accessed 23 Nov 2017.
Loveman E, Cooper K, Bryant J, Colquitt JL, Frampton GK, Clegg A. Dasatinib, high-dose imatinib and nilotinib for the treatment of imatinib-resistant chronic myeloid leukaemia: a systematic review and economic evaluation. Health Technol Assess Winch, Engl. 2012;16(23):iii–xiii. https://doi.org/10.3310/hta16230 (1–137).
Gambacorti-Passerini C, Kantarjian HM, Kim DW, Khoury HJ, Turkina AG, Brummendorf TH, et al. Long-term efficacy and safety of bosutinib in patients with advanced leukemia following resistance/intolerance to imatinib and other tyrosine kinase inhibitors. Am J Hematol. 2015;90(9):755–68. https://doi.org/10.1002/ajh.24034.
Kantarjian H, O’Brien S, Talpaz M, Borthakur G, Ravandi F, Faderl S, et al. Outcome of patients with Philadelphia chromosome-positive chronic myelogenous leukemia post-imatinib mesylate failure. Cancer. 2007;109(8):1556–60. https://doi.org/10.1002/cncr.22569.
Jabbour E, Cortes J, Santos FP, Jones D, O’Brien S, Rondon G, et al. Results of allogeneic hematopoietic stem cell transplantation for chronic myelogenous leukemia patients who failed tyrosine kinase inhibitors after developing BCR-ABL1 kinase domain mutations. Blood. 2011;117(13):3641–7. https://doi.org/10.1182/blood-2010-08-302679.
Craddock C, Szydlo RM, Klein JP, Dazzi F, Olavarria E, van Rhee F, et al. Estimating leukemia-free survival after allografting for chronic myeloid leukemia: a new method that takes into account patients who relapse and are restored to complete remission. Blood. 2000;96(1):86–90.
Kantarjian HM, Cortes JE, Kim DW, Khoury HJ, Brummendorf TH, Porkka K, et al. Bosutinib safety and management of toxicity in leukemia patients with resistance or intolerance to imatinib and other tyrosine kinase inhibitors. Blood. 2014;123(9):1309–18. https://doi.org/10.1182/blood-2013-07-513937.
Kind P, Hardman G, Macran S. UK population norms for EQ-5D. 1999. http://EconPapers.repec.org/RePEc:chy:respap:172chedp Accessed 1 Dec 2017.
Szabo SM, Levy AR, Davis C, Holyoake TL, Cortes J. A multinational study of health state preference values associated with chronic myelogenous leukemia. Value Health J Int Soc Pharmacoecon Outcomes Res. 2010;13(1):103–11. https://doi.org/10.1111/j.1524-4733.2009.00573.x.
van Agthoven M, Vellenga E, Fibbe WE, Kingma T, Uyl-de Groot CA. Cost analysis and quality of life assessment comparing patients undergoing autologous peripheral blood stem cell transplantation or autologous bone marrow transplantation for refractory or relapsed non-Hodgkin’s lymphoma or Hodgkin’s disease. a prospective randomised trial. Eur J Cancer. 2001;37(14):1781–9.
Kantarjian HM, O’Brien S, Cortes JE, Giralt SA, Rios MB, Shan J, et al. Imatinib mesylate therapy for relapse after allogeneic stem cell transplantation for chronic myelogenous leukemia. Blood. 2002;100(5):1590–5.
Olavarria E, Ottmann OG, Deininger M, Clark RE, Bandini G, Byrne J, et al. Response to imatinib in patients who relapse after allogeneic stem cell transplantation for chronic myeloid leukemia. Leukemia. 2003;17(9):1707–12. https://doi.org/10.1038/sj.leu.2403068.
UK Stem Cell Strategy Oversight Committee. NHS Blood and Transplant. Unrelated Donor Stem Cell Transplantation in the UK. Effective Affordable Sustainable. 2014. http://www.nhsbt.nhs.uk/download/unrelated_donor_stem_cell_transplantation_in_the_uk.pdf Accessed 1 Dec 2016.
Radich JP. Allogeneic transplant for chronic myeloid leukemia in 2010. Ther Adv Hematol. 2010;1(1):5–13. https://doi.org/10.1177/2040620710388339.
Guyot P, Ades AE, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12:9. https://doi.org/10.1186/1471-2288-12-9.
Glenny AM, Altman DG, Song F, Sakarovitch C. Deeks JJ, al. e. Indirect comparisons of competing interventions. Health Technol Assess. 2005;9(26):1–134.
Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol. 1997;50(6):683–91.
National Institute for Health and Care Excellence (NICE). Ponatinib for treating chronic myeloid leukaemia and acute lymphoblastic leukaemia—technology appraisal guidance [TA451]. NICE, London. 2017. https://www.nice.org.uk/guidance/ta451/ Accessed 23 Nov 2017.
Acknowledgements
All authors have commented on the submitted manuscript and have given their approval for the final version to be published. The views expressed in this report are those of the authors and not necessarily those of the NIHR HTA Programme. Any errors are the responsibility of the authors.
Author information
Authors and Affiliations
Contributions
AP drafted the final version of the manuscript and takes responsibility as the overall guarantor of the content. All authors have commented on the submitted manuscript and have given their approval for the final version to be published. MS and AR reviewed the cost-effectiveness evidence, AP and MMJ reviewed the clinical-effectiveness evidence, JS and JH reviewed statistical analyses, RW reviewed search strategies. JB and CR provided clinical input and advice. This summary has not been externally reviewed by PharmacoEconomics.
Corresponding author
Ethics declarations
Funding
This project was funded by the National Institute for Health Research (NIHR) Health Technology Assessment Programme (Project number 16/51/11). See the HTA programme website for further project information (http://www.hta.ac.uk). This summary of the ERG report was compiled after NICE issued the FAD.
Conflict of interest
Dr. J. Byrne has received honoraria from ARIAD Pharmaceuticals and Pfizer in the past for advisory boards and speaker meetings. AP, MS, JS, MMSJ, JH, CR, AR and RW have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Pandor, A., Stevenson, M., Stevens, J. et al. Ponatinib for Treating Chronic Myeloid Leukaemia: An Evidence Review Group Perspective of a NICE Single Technology Appraisal. PharmacoEconomics 36, 903–915 (2018). https://doi.org/10.1007/s40273-018-0627-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-018-0627-4