Abstract
Psychotropic medications have a high risk of serious adverse events and small effect size for changed behaviours for people with dementia. Non-pharmacological approaches are recommended as first-line treatment for changed behaviours, yet psychotropic medications remain highly prevalent in long-term aged care settings. This narrative review describes the current evidence regarding deprescribing psychotropic medications for people with dementia in long-term care. Deprescribing psychotropic medications can be achieved without harm to the person with dementia, and most people experience no withdrawal symptoms. Interventions to deprescribe psychotropic medications should be multifactorial, including lowering the dose of the medication over time, educational interventions and psychological support. However, implementing this is a significant challenge due to the overreliance on psychotropic medications for behavioural management in long-term aged care. Facilitators to deprescribing psychotropic medications in long-term care include multidisciplinary teams with adequate training, education and managerial support, engaging residents and families and change ‘champions’. Deprescribing practices should be person-centred, and an individualised deprescribing protocol should be in place, followed by careful monitoring of the individual. The person with dementia and their family, general practitioner, pharmacist, and allied health and direct care staff should all be involved throughout the deprescribing process. Direct care staff need adequate support, education and training, so they can effectively help the individual and implement person-centred approaches in the absence of psychotropic medications. Effective communication between residents and staff and amongst staff is consistently shown to be an important factor for deciding whether deprescribing of a medication should occur and the successful implementation of deprescribing psychotropic medications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Psychotropic medications are frequently prescribed in long-term care for changed behaviours in people living with dementia, despite recommendations stating that non-pharmacological interventions should be used where possible. |
Interventions have shown that deprescribing psychotropic medications in long-term care is feasible, with the majority of people experiencing no withdrawal symptoms. |
Deprescribing regular psychotropic medications should be gradual and should actively involve the residents, their family members and a multidisciplinary team to personalise a deprescribing protocol and monitor the progress of the individual. |
1 Introduction
Changed behaviours exhibited by people with dementia living in long-term care are often referred to as behavioural and psychological symptoms of dementia (BPSD), but dementia pathology is rarely the only underlying cause. Behaviours (e.g. agitation, depression) are often triggered by unmet needs that cause pain or distress, rather than dementia pathology [1]. International guidelines recommend non-pharmacological approaches for changed behaviours as first-line treatments, and pharmacological approaches should be only considered when non-pharmacological approaches fail or when the behaviour is severe and the person with dementia is at risk of harm to himself/herself or others [2,3,4,5]. Non-pharmacological approaches can offer a similar level of efficacy to pharmacological treatments, but without adverse side effects [6]. Despite these recommendations, psychotropic medication use remains high among people with dementia living in long-term aged care settings [7].
Deprescribing is the process of rational supervised withdrawal of medication for which the risk currently outweighs the benefit to the individual. Psychotropic medications, including antipsychotics, can be deprescribed without harm to the person with dementia and usually without relapse of symptoms if a person-centred care approach is established [8]. However, this is a clinical challenge given the overreliance on these medications for management of changed behaviours in people with dementia in long-term care settings [7], widespread misunderstanding about their use among staff [9] and prescribing physicians [10], and the serious impact of behaviour change on resident and staff wellbeing [11,12,13].
This article is not an exhaustive review of the vast literature on this topic. The aim of this review is to provide an overview of the evidence to inform practical approaches for deprescribing psychotropic medications for people living with dementia in long-term aged care settings, with a focus on strategies clinicians can apply to overcome the barriers to these approaches.
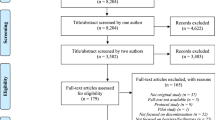
This review was informed by literature searches of PubMed and Google Scholar conducted in March 2018 using different combinations and variations of the keywords psychotropic*, antipsychotic*, antidepressant*, anxiolytic*, benzodiazepine*, hypnotic*, sedative*, deprescribing, withdrawal, nursing homes, residential aged care, behavioural/behavioral and psychological symptoms of dementia and linking terms using standard Boolean operators (AND/OR). The searches were limited from the year 2000 and to articles published in English. Further relevant articles were identified from reference lists and from clinical discussions.
2 Psychotropic Use for People with Dementia Living in Long-Term Aged Care
Behaviour change is highly prevalent among people with dementia living in long-term care, especially apathy (49%), depression (42%), agitation/aggression (40%), anxiety (39%), and sleep disorders (39%) [14]. There is some evidence to support the use of psychotropic medications to treat some of these symptoms, but the effect size is small and similar to that of non-pharmacological interventions [6]. Some expert consensus guidelines state that selective-serotonin reuptake inhibitors (SSRIs) (particularly citalopram) may be appropriate for agitation for people with dementia [2]. The evidence of efficacy for SSRIs for treating depression in people with dementia has been mixed [17], with two large trials reporting negative findings [18, 19]. Atypical antipsychotics (particularly risperidone and olanzapine) and memantine (an N-methyl-d-aspartate antagonist) have small-modest effects for severe agitation and aggression [20, 21]. The recent international Delphi consensus for management of changed behaviours for people with Alzheimer’s disease prioritised citalopram and a stepped protocol for analgesics ahead of antipsychotics if pharmacological approaches are needed after assessment and identification of underlying causes [22]. Benzodiazepines may be useful for short-term treatment of acute anxiety [23].
Some pharmacological treatments for behaviour change (particularly antipsychotics) are increasingly recommended against because of the risks associated with their use and availability of safer alternatives. Antipsychotic use is associated with an increased risk of all-cause mortality in people with dementia [24, 25] and is estimated to contribute to 1800 deaths in the UK each year [20]. Several meta-analyses have demonstrated an increased risk for cerebrovascular effects, including stroke, extra-pyramidal side effects, somnolence, and gait abnormality [26]. Antipsychotic medications do not improve (and may worsen) function or quality of life [27]. Sustained use of benzodiazepines is associated with sedation, dizziness, falls, worsening cognition, respiratory depression, and paradoxical disinhibition [23], and there is little evidence for their efficacy in managing behaviour change [28]. Cognitive and cardiovascular adverse effects of citalopram should be considered before clinical use [15, 16]. Mood stabilisers have limited efficacy and may worsen behaviour symptoms [29].
3 Non-pharmacological Approaches for People with Dementia in Long-Term Aged Care
As the evidence base for non-pharmacological approaches for changed behaviours has been discussed in detail in previous systematic reviews [6, 39, 40], only a brief overview is provided here for context.
Non-pharmacological approaches to changed behaviours should be meaningful and tailored to the individual, using a person-centred approach [22, 41, 42]. Person-centred approaches are known to improve outcomes such as reduced agitation for the residents [43]; how care staff engage with residents to support shared decision making is critical [42]. Certain therapies and interventions will be more favourable for different people, depending on their personal enjoyment of the activities and subsequent willingness to participate, and it is likely such approaches will be better received by residents if they have been involved in the decision-making process about their care [39].
Some evidence exists to support the use of functional analysis-based interventions to treat changed behaviours in long-term care, whereby those involved in the care of a person with dementia actively seek an understanding of the meaning of the person’s behaviour [44]. Evidence-based behaviour frameworks such as the Describe, Investigate, Create, Evaluate (DICE) approach or the Antecedent, Behaviour and Consequence (ABC) approach have been developed to help clinicians to assess the changed behaviours people with dementia experience and to guide subsequent person-centred interventions [45, 46].
Music therapy is a promising non-pharmacological approach for overall changed behaviours for people with dementia [22]; it can reduce depression and may improve emotional wellbeing, quality of life and reduce anxiety and mild-moderate agitation [40, 47,48,49]. Receptive music therapy (listening to preferred music in a quiet place) is more effective than interactive music therapy (singing or playing musical instruments with a music therapist or trained professional) for reducing agitation [50].
Psychological treatments (such as cognitive behavioural therapy, interpersonal therapy, counselling or multi-component interventions centred on psychological therapy) have small-to-moderate effect sizes for reducing depressive symptoms and anxiety for people with dementia [51]. However, the quality of evidence for psychological therapy is low-moderate overall, and further research is required [51]. Individual reminiscence therapy for long-term care residents is associated with improvements in mood [52]. Evidence is inconsistent about the benefits of other non-pharmacological therapies such as aromatherapy [53], exercise [54, 55], and animal-assisted therapy (pet therapy) for changed behaviours [56]. Person-centred care and novel strategies such as humour therapy have been shown to reduce agitation significantly in high-quality cluster randomised controlled trials [57,58,59]. Adaptations to the long-term care environment have also been recognised as promising approaches for changed behaviours for people with dementia [22]. Lower rates of psychotropic medications have been reported in Dutch small-scale homes and Australian clustered domestic homes compared to more traditional care [60, 61].
4 Approaches to Deprescribing Psychotropic Medications in Long-Term Aged Care
4.1 Guidelines and Recommendations
Clinical guidelines in Canada [4], the United States [5], the UK [3], Australia [2] and elsewhere recommend that psychotropic treatments should only be trialled after non-pharmacological therapies have failed for a specific indication (e.g. distressing delusions), and where the behaviour is severe and high risk to the individual or others around them. Antipsychotic medications should be prescribed at the lowest effective dose for the shortest time required and regularly reviewed. Nonetheless, psychotropic medications are routinely prescribed to long-term care residents with dementia. Approximately 60% are prescribed one or more psychotropic medications at any given time [7, 30, 31], most commonly anti-depressants (46% in the USA, 41% in Australia, and 40% in the UK), antipsychotics (29% in the USA, 22% in Australia, and 27% in the UK), and benzodiazepines (13% in the USA, 22% in Australia, and 15% in the UK) [7, 32,33,34,35]. Psychotropic polypharmacy is commonplace [36] despite very limited evidence of efficacy for combinations and the risk of cumulative toxicity from multiple drugs with sedative, anticholinergic and serotonergic effects. The extent to which these prescriptions are inappropriate (i.e. off-label and/or contrary to guidelines for use) can be difficult to identify because indications and guidance vary internationally, but use of antipsychotics and benzodiazepines well in excess of the recommended duration [28, 37] and to treat non-indicated behaviour changes has been reported [30, 33, 38].
Deprescribing inappropriate psychotropic medications in long-term care residents with dementia is an area of clinical need, but is challenging in practice. The development of regulations to limit the amount of antipsychotics in long-term care is not new. In the USA in 1987, federal legislation was designed to reduce unnecessary use of psychotropic medications as part of the Federal Nursing Home Reform Act [or Omnibus Budget Reconciliation Act (OBRA ’87)], and interpretive guidelines to fulfil the OBRA requirements were implemented in 1990 [62, 63]. Compliance with the regulations outlined in the OBRA has been shown to be good for more specific regulations (e.g. documenting target symptoms), but further interventions are needed to improve monitoring adverse effects and efficacy of medications and increase the use of non-pharmacological interventions [64]. Comparisons with other countries without such regulations suggest this policy has reduced the likelihood of being prescribed an antipsychotic or antianxiety/hypnotic medication in long-term care [65]. However, research has also shown variation in antipsychotic prescribing rates in the USA despite the regulations and may be influenced by the ‘prescribing culture’ of the particular aged care home [33, 66]. In Australia, risperidone is the only antipsychotic approved by the Therapeutic Goods Administration (TGA) for changed behaviours in dementia. Risperidone was previously indicated for the treatment of changed behaviours (referred to as behavioural disturbances) in dementia without strict limitations. Since 2015, restrictions have stated that for changed behaviours for people with dementia, risperidone is only to be used for moderate-to-severe dementia of the Alzheimer type for “up to 12 weeks of psychotic symptoms or persistent agitation or aggression unresponsive to non-pharmacological approaches” [67].
Further large-scale policy initiatives used to curb inappropriate prescribing of psychotropic medications include black-box warnings in the USA. Black-box warnings on atypical antipsychotic medications were introduced in 2005, with warnings of the increased risk of cerebrovascular events and death [68]. There is some evidence that these warnings may have contributed to a reduction in the use of atypical antipsychotics in long-term care, but it is not clear if this resulted in other psychotropic medications being substituted for antipsychotics or increases in diagnoses such as bipolar or schizophrenia in the older population to legitimise the prescribing [68]. In older people living with dementia living in the community, black-box warnings appeared to have no significant effect on atypical antipsychotic medication use, and the use of benzodiazepines and anti-dementia medications increased during this time [69]. Similar warnings were made in 2009 in the UK [20], and associated recommendations for use were incorporated as guidelines in a National Dementia Strategy. This made no difference to prescribing rates over the following 4 years [70].
Medication management reviews by doctors and pharmacists are recommended to regulate the quality of prescribing in long-term care in countries such as Australia (Residential Medication Management Reviews), the USA (Medication/Drug Regimen Review) [71] and the UK (Medication Reviews) [72]. The recommended frequency of medication reviews differs between countries (e.g. “monthly” in the USA [73], “interval between medication reviews should be no more than 1 year, and many residents will need more frequent medication reviews” and for new residents “as soon as possible after admission” in the UK [72], and on a “clinical needs basis” in Australia [74]). Pharmacists are usually involved in medication reviews, either alone or as part of a multidisciplinary team [75]. In the UK, medication reviews were traditionally conducted by general practitioners (GPs), but more recently, a programme to have pharmacy teams (pharmacists and pharmacy technicians) work with care staff, residents and families as a strategy to optimise medication prescribing in long-term aged care homes has been implemented [76]. A review is intended to identify any contraindicated medication use or inappropriate polypharmacy and suggest solutions in a written report to a primary care physician. Pharmacist-led medication reviews in long-term care have been shown to reduce anticholinergic and sedative medication prescribing [77] and may improve the quality of prescribing [78]. Guidance for medication reviews in the UK specifically states that during medication reviews there should be a re-assessment of the “need for unlicensed medicines, for example antipsychotics used for the treatment of behavioural and psychological symptoms of dementia” [79]. However, the impact of medication reviews on prescribing and deprescribing of psychotropic medications is influenced by the culture of the aged care homes. While this is a ‘tool for change’ in some aged care homes, it can be reduced to a ‘box-ticking exercise’, where reports are given to the primary care physician and no further action is taken [80].
Regulations also exist in countries such as Australia to ensure that appropriate ‘substitute consent’ is obtained for medical treatment for people who lack capacity to provide informed consent. This is an important issue for people with dementia, as cognitive impairment associated with dementia may interfere with a person’s capacity to provide consent, depending on the individual and the progression of dementia. Yet, there are poor rates of adherence to regulations to obtaining substitute consent for psychotropic medications for people with dementia in Australia who do not have capacity to give informed consent [81].
4.2 Evidence of the Benefits and Harms of Deprescribing Psychotropic Medications
Despite the potential harms of psychotropic medications and small effect sizes for changed behaviours, prescribing rates of psychotropics for people living with dementia in long-term care remain high. Even where regular antipsychotic medication use has declined, as required [pro re nata (prn)] antipsychotic and benzodiazepine use has increased [7]. This suggests these medicines are being used as substitutes for long-term antipsychotic use despite guidelines recommending non-pharmacological approaches as alternatives.
Concerns from residents and family members about the potential for withdrawal symptoms, exacerbation of behaviour changes, and negative impacts on quality of life and wellbeing upon the deprescribing of psychotropic medication are common, particularly in cases of long-term use [82]. A recent Cochrane review examining long-term antipsychotic medication use in older people with dementia concluded that deprescribing can be achieved without worsening behaviour, although the quality of the evidence was low [8]. A US study of 180 people with Alzheimer’s disease identified a slightly increased risk of re-emergence of agitation and psychosis, but included people living at home and in assisted-living facilities where fewer non-pharmacological alternatives might be available [83].
Interventions to optimise prescribing in long-term care by examining the whole medication regimen suggest appropriateness of medications can be improved through multi-component interventions including pharmacist-led medication reviews, transfer of information and multidisciplinary case conferencing, but the long-term effects on resident outcomes are unclear [71]. A recent longitudinal study examining a multi-component antipsychotic deprescribing protocol in Australian long-term care settings indicated that antipsychotics can be withdrawn without an increase in changed behaviours or adverse outcomes or a significant increase of prn antipsychotic or benzodiazepine prescriptions [84]. This intervention included re-education and training of care staff (registered nurses, GPs and pharmacists involved in the supply of medications to care homes) and a personalised deprescribing protocol developed by pharmacists. An 81.7% reduction in regular antipsychotic use after 12 months was reported [84]. Effective communication between GPs, families and care staff coupled with managerial support in the long-term care facility and deprescribing nurse ‘champions’ who were empowered to lead the change process were shown to be crucial to help care staff apply a person-centred approach to changed behaviours [85]. A different longitudinal study of a multi-component intervention in Australian long-term care settings showed a cessation or reduction in antipsychotics or benzodiazepines for 39% of the residents over 6 months with no substitution for other psychotropic medications [86]. This intervention included education for staff to challenge beliefs that antipsychotics and benzodiazepines were effective for changed behaviours, training for champion nurses and psychotropic audits and feedback to prescribers [86].
Previous studies have shown staff training interventions alone may reduce antipsychotic use in long-term care by 19.1% [87], whereas interventions which actively involve a multidisciplinary team involved in the direct care of the individual may improve deprescribing success rates [88]. A randomised controlled trial in the Netherlands found that 6-monthly medication reviews by a multidisciplinary team (GP, pharmacist and nurse) can improve appropriate psychotropic prescribing in long-term care defined by the Appropriate Psychotropic drug use in Dementia (APID) score [89]. Withdrawing antipsychotics can also improve survival rates in long-term care residents [90]. The Australian guidelines for the use of antipsychotics in long-term care recommend that withdrawing antipsychotics should be considered when the individual has not experienced the targeted changed behaviours for a period of time, such as 3 months [91]. Deprescribing should happen gradually, with the support of a secondary care mental health team. The longer the medication has been prescribed for, the slower the withdrawal should be.
Benzodiazepine withdrawal is also feasible without affecting sleep quality or quality of life [92], though withdrawal rates vary according to the interventions and the population (reported rates 27–80%) [93]. As previously described, a multi-component intervention showed a reduction in benzodiazepine use in long-term care following deprescribing recommendations, education for staff, and implementation of ‘champion’ nurses. This intervention resulted in a 21% reduction in the proportion of residents regularly prescribed benzodiazepines [86]. Tapering benzodiazepine use in conjunction with cognitive behaviour therapy may enhance success rates and could be considered for individuals who are more resistant to withdrawal protocols, though this has not been examined specifically in long-term care. Cognitive behaviour therapy may improve some outcomes for people with mild dementia such as clinician-rated anxiety symptoms [51, 93,94,95,96]. Similarly to deprescribing antipsychotics, a personalised person-centred approach is recommended for benzodiazepines, with gradual withdrawal and continued monitoring from a multidisciplinary team [50].
Withdrawing antidepressants should also be considered in long-term care because of the high rate of use and risk of therapeutic substitution when withdrawing other psychotropic medications. There have been few studies conducted which have examined the potential benefits and harms of deprescribing antidepressants for people with dementia in long-term care, despite the potentially low efficacy reported for depression for people with dementia and potential adverse effects [15, 16, 97]. Potential withdrawal symptoms may occur with any type of SSRI from treatment durations as short as 2 months [98]. One randomised controlled trial showed that withdrawing antidepressant medications for people with dementia in long-term care resulted in worsening of depressive symptom scores after 25 weeks. However, the authors questioned whether this change was clinically significant as most people who were withdrawn from antidepressants remained in the same subgroup for depression scale scores [99].
When withdrawing psychotropic medications, the person should be carefully monitored for recurrence of symptoms (such as depression after withdrawal of antidepressants) or other negative outcomes such as a reduction in quality of life or an increase in other changed behaviours. Non-pharmacological alternatives should be employed before and after cessation of the medication. If negative withdrawal symptoms occur and represcribing, abandoned deprescribing or prescribing of an alternative medication is considered necessary, monitoring should continue, and the medication should be reviewed at least 12 weekly. Discussions should continue with the person with dementia, staff, and family members about whether to attempt to withdraw the medications again. If the medication is reinstated, it should be restarted at the lowest effective dose that was established during weaning.
5 Facilitators and Barriers to Deprescribing Psychotropic Medications in Long-Term Aged Care
The facilitators and barriers to deprescribing have been previously reviewed [100, 101] although these may differ between people living in long-term care and people living in the community. Much of the research of facilitators and barriers to deprescribing has been conducted with GPs in primary care settings [102]. Fewer studies have investigated the views of other healthcare professionals, residents, and family members, and none has been specific to psychotropic medications. A summary of the most important facilitators and barriers to deprescribing is presented in Table 1.
It is often difficult for GPs, nurses and pharmacists to consider deprescribing psychotropic medications when residents are newly admitted, especially when insufficient information about treatment indication and longitudinal course are provided [82]. Residents and family members will not always be able to identify when and why a medication was prescribed. Further studies should examine a more efficient method of communicating medication histories about new residents to staff. Furthermore, initiation of psychotropic medications for residents of long-term aged care settings often occurs in hospital and outpatient settings, and communication of why the medication was prescribed, or what the outgoing plan is, does not always occur [103]. Frequent review of medications for residents in long-term care settings, including during transitions between hospital and long-term care, is critical to optimise prescribing of appropriate medications [104].
Engaging individuals and their carers in healthcare decisions (shared decision making) is the most important attribute of person-centred care [105]. Deprescribing is likely to be acceptable to residents if a clinician says it is possible, but this has not been specifically investigated in relation to psychotropic medications [106]. Residents and their family members may be unaware that different options for their medications exist and may not know that deprescribing is an option [107] and may be unaware that they have a legal right to approve the use of the medication. The views of a clinician are highly valued by older people and can affect their inclination to withdraw or continue a medication. Involving family members in discussions about the resident’s medications and potential underlying causes of behaviours enable partnerships to be formed between staff and family members, further enabling appropriate person-centred care [85]. Optimising clinician knowledge and confidence will facilitate these discussions, and deprescribing guidelines such as guidelines produced in Canada for deprescribing antipsychotics are important to support this [4].
To assist with optimal decision making around deprescribing, healthcare professionals can discuss the options with residents and families using decision aids. Decision aids may include educational materials explaining the risks and benefits of withdrawing psychotropic medications and an explanation that non-pharmacological approaches are the preferred method of treatment based on current available evidence. Qualitative research in long-term care involving residents and healthcare professionals is inconsistent with regard to what factors are perceived to be the most important when deciding on whether to deprescribe medications [102]. However, both healthcare professionals and residents have stressed the importance of communication (e.g. between residents and health professionals and between healthcare professionals such as nurses, pharmacists, GPs and specialist physicians) [102].
Inadequate staffing and/or training or inefficient skills mix of staff can be barriers to effective communication and behaviour management. Staff who are inexperienced or time poor will find it difficult to engage the person in non-pharmacological approaches such as music therapy [85], leading to an overreliance of psychotropic medications to help people with changed behaviours. Organisational culture is also a key factor that profoundly shapes decisions to use psychotropic medicines, as it is the frame by which staff manage perceptions about the work environment (e.g. staff levels, workload, inter-professional conflict) with ideal practices [108]. On-site and visiting staff perceptions of staffing levels, low managerial expectations and poor teamwork among care staff are important barriers to appropriate psychotropic prescribing in long-term care [109]. Managerial prioritising of non-pharmacological approaches for changed behaviours and adequate support for care staff to monitor and review psychotropic medications can improve teamwork and reduce reliance on psychotropic medications [109]. The attitudes of healthcare professionals may lead to a ‘prescribing culture’ where medications are first-line treatments and non-pharmacological methods are not favoured. Deprescribing may be viewed as too time-consuming or not valuable. Further, healthcare professionals may lack confidence to recommend non-pharmacological approaches for changed behaviours if they think they lack sufficient knowledge regarding different treatment options or if they do not have confidence that the facility can provide these [110]. Changing the behaviours of healthcare professionals to reduce reliance on psychotropics may be facilitated by increased awareness of appropriate guidelines and reimbursement systems that acknowledge the time needed to adequately implement deprescribing [111], as well as adequate resources for non-pharmacological alternatives.
A multidisciplinary approach should be taken when deprescribing, to ensure all staff involved with an individual’s use of psychotropic medications are adequately supported, educated and trained to improve deprescribing practices. By improving the whole ‘prescribing culture’ rather than focusing only on people who prescribe medications, all stakeholders become agents of change [112].
Recommendations by direct care staff regarding psychotropic medications will only be effective if prescribers act on them. Communication between direct care staff, pharmacists, GPs, family members, and residents must be based on mutual respect to ensure potential opportunities for deprescribing are not missed [102, 109, 112]. Continuity of staff should be encouraged where possible as residents have described that unfamiliar staff are less likely to be aware of medication histories [102].
That most of those prescribed psychotropic medications in long-term care have cognitive impairment or dementia adds a level of complexity regarding capacity for individuals to make a decision on deprescribing. People living with dementia should not be presumed to be unable to make a choice regarding their medications, and health professionals must work with residents and their families/supporters to plan the withdrawal of long-term medications. Questionnaires have been developed to capture beliefs and attitudes towards deprescribing for people living with mild-to-moderate dementia [113] and for carers [114] and may be useful to determine a person’s willingness to deprescribe or perceived barriers to deprescribing.
Continuity of staff is also important for choice, as clinicians who know the residents better will be better informed about the capacity of the individual to make a decision regarding withdrawal of medications [102]. Residents may be anxious about withdrawing a medication that they have been taking for a long time; educational materials may help, and staff can help residents work with the clinician to make an informed choice. In many instances, the resident may prefer to have a family member involved in the decision-making process, and residents and their family members may be fearful of deterioration if they change their current medications [102]. Explaining the process of deprescribing and ensuring residents and their family members are fully informed of both the risks and benefits of deprescribing psychotropic medications may help [92]. Figure 1 provides an overview of the steps to take when deprescribing psychotropic medications in long-term aged care settings.
6 Areas for Future Research
The risks associated with inappropriate prescribing of psychotropic medications and benefits of deprescribing are well established. Multi-component deprescribing interventions that target several levels of organisational structure simultaneously appear to be most effective at reducing inappropriate psychotropic use in long-term care. Further evidence from randomised controlled trials on the prescribing and clinical outcomes of interventions that encourage healthcare professionals to initiate deprescribing of psychotropics would be beneficial.
As discussed in this review, psychotropic medications may have been prescribed prior to the resident starting long-term care. This adds a level of complexity, as the indications for prescribing may be unclear and the residents and family members will not always be able to describe the reason, response or intended duration. Further studies should examine prescribing trajectories of psychotropic medications for older people prior to starting long-term care to enable a clear understanding of when, why and where these medications are prescribed before long-term care and how the staff of long-term care could be better informed about the prescribing history of the resident.
Work remains to close the gap between clinical guidelines and practice, and research can be useful to expedite this process. Implementation trials that consider the contextual barriers and facilitators to deprescribing can provide important insights for long-term care settings working to make positive change. As mentioned, the need to limit prescribing of inappropriate therapeutic substitutes has been identified [e.g. 7, 115]. It is evident that physicians and care staff need adequate access to resources, education, and support to deprescribe and to transition to managing behaviour change with non-pharmacological means. Research demonstrating the cost-effectiveness of this transition will help to establish a business case for policy-makers and providers. In addition, some research examining the efficacy of collaborative or system-based interventions is underway [116, 117] and should help to demonstrate the broader contextual and policy factors that facilitate sustained change. As mentioned, large scale policy initiatives (such as black-box warnings or medication review systems) have had limited effects to date. Policy-makers need guidance about legislative or regulatory measures that could promote best practice.
7 Conclusions
The high prevalence of psychotropic medications in long-term aged care settings demonstrates the gap between guidelines for the treatment of changed behaviours for people with dementia and clinical practice. Psychotropic medications can be effectively deprescribed using multi-component, multidisciplinary and person-centred interventions. Suitable education, training and support of clinicians deprescribing and of direct care staff, GPs and families to effectively help people experiencing changed behaviours without the use of psychotropic medications is needed. It is important to identify and address elements of culture which hinder appropriate psychotropic prescribing. Improved communication (between GPs, pharmacists, care staff, residents and their families) and appropriate managerial support coupled with training of care staff will promote optimal outcomes from deprescribing psychotropic medications in people living with dementia in long-term care.
References
NHS England. Optimising treatment and care for people with behavioural and psychological symptoms of dementia. 2017. http://medicine.exeter.ac.uk/media/universityofexeter/medicalschool/pdfs/nhs-dementia-best-practice-guide.pdf. Accessed 4 Apr 2018.
Laver K, Cumming RG, Dyer SM, Agar MR, Anstey KJ, Beattie E, et al. Clinical practice guidelines for dementia in Australia. Med J Aust. 2016;204(5):191–3.
National Collaborating Centre for Mental Health. Dementia: a NICE-SCIE guideline on supporting people with dementia and their carers in health and social care. Leicester: British Psychological Society; 2007.
Bjerre LM, Farrell B, Hogel M, Graham L, Lemay G, McCarthy L, et al. Deprescribing antipsychotics for behavioural and psychological symptoms of dementia and insomnia: evidence-based clinical practice guideline. Can Fam Physician. 2018;64(1):17–27.
Reus VI, Fochtmann LJ, Eyler AE, Hilty DM, Horvitz-Lennon M, Jibson MD, et al. The American Psychiatric Association practice guideline on the use of antipsychotics to treat agitation or psychosis in patients with dementia. Am J Psychiatry. 2016;173(5):543–6.
Dyer SM, Harrison SL, Laver K, Whitehead C, Crotty M. An overview of systematic reviews of pharmacological and non-pharmacological interventions for the treatment of behavioral and psychological symptoms of dementia. Int Psychogeriatr. 2018;30(3):295–309.
Westbury J, Gee P, Ling T, Kitsos A, Peterson G. More action needed: psychotropic prescribing in Australian residential aged care. Aust N Z J Psychiatry. 2018. https://doi.org/10.1177/0004867418758919.
Van Leeuwen E, Petrovic M, van Driel ML, De Sutter AI, Vander Stichele R, Declercq T, et al. Withdrawal versus continuation of long-term antipsychotic drug use for behavioural and psychological symptoms in older people with dementia. Cochrane Database Syst Rev. 2018;3:Cd007726.
Lemay CA, Mazor KM, Field TS, Donovan J, Kanaan A, Briesacher BA, et al. Knowledge of and perceived need for evidence-based education about antipsychotic medications among nursing home leadership and staff. J Am Med Dir Assoc. 2013;14(12):895–900.
Janus SI, van Manen JG, Zuidema SU, Snijder C, Drossaert CH, Ijzerman MJ. Reasons for (not) discontinuing antipsychotics in dementia. Psychogeriatrics. 2018;18(1):13–20.
Pulsford D, Duxbury J. Aggressive behaviour by people with dementia in residential care settings: a review. J Psychiatr Ment Health Nurs. 2006;13(5):611–8.
Cubit K, Farrell G, Robinson A, Myhill M. A survey of the frequency and impact of behaviours of concern in dementia on residential aged care staff. Australas J Ageing. 2007;26(2):64–70.
Hoe J, Hancock G, Livingston G, Orrell M. Quality of life of people with dementia in residential care homes. Br J Psychiatry. 2018;188(5):460–4.
Zhao Q-F, Tan L, Wang H-F, Jiang T, Tan M-S, Tan L, et al. The prevalence of neuropsychiatric symptoms in Alzheimer’s disease: systematic review and meta-analysis. J Affect Disord. 2016;190:264–71.
Seitz DP, Adunuri N, Gill SS, Gruneir A, Herrmann N, Rochon P. Antidepressants for agitation and psychosis in dementia. Cochrane Database Syst Rev. 2011;16(2):Cd008191.
Porsteinsson AP, Drye LT, Pollock BG, Devanand DP, Frangakis C, Ismail Z, et al. Effect of citalopram on agitation in Alzheimer disease: the CitAD randomized clinical trial. J Am Med Assoc. 2014;311(7):682–91.
Buterbaugh WM, Jamrose T, Lazzara J, Honaker L, Thomas CJ. Review of antidepressants in the treatment of behavioral and psychiatric symptoms in dementia (BPSD). Ment Health Clin. 2014;4(4):183–8.
Rosenberg PB, Martin BK, Frangakis C, Mintzer JE, Weintraub D, Porsteinsson AP, et al. Sertraline for the treatment of depression in Alzheimer disease. Am J Geriatr Psychiatry. 2010;18(2):136–45.
Banerjee S, Hellier J, Dewey M, Romeo R, Ballard C, Baldwin R, et al. Sertraline or mirtazapine for depression in dementia (HTA-SADD): a randomised, multicentre, double-blind, placebo-controlled trial. Lancet. 2011;378(9789):403–11.
Banerjee S. The use of antipsychotic medication for people with dementia: time for action. A report for the Minister of State for Care Services United Kingdom Department of Health From the website. 2009.
Wilcock GK, Ballard CG, Cooper JA, Loft H. Memantine for agitation/aggression and psychosis in moderately severe to severe Alzheimer’s disease: a pooled analysis of 3 studies. J Clin Psychiatry. 2008;69(3):341–8.
Kales HC, Lyketsos CG, Miller EM, Ballard C. Management of behavioral and psychological symptoms in people with Alzheimer’s disease: an international Delphi consensus. Int Psychogeriatr. 2018;2:1–8.
Tible OP, Riese F, Savaskan E, von Gunten A. Best practice in the management of behavioural and psychological symptoms of dementia. Ther Adv Neurol Disord. 2017;10(8):297–309.
Ralph SJ, Espinet AJ. Increased all-cause mortality by antipsychotic drugs: updated review and meta-analysis in dementia and general mental health care. J Alzheimer’s Dis Rep. 2018;2(1):287–312.
Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. J Am Med Assoc. 2005;294(15):1934–43.
Tampi RR, Tampi DJ, Balachandran S, Srinivasan S. Antipsychotic use in dementia: a systematic review of benefits and risks from meta-analyses. Ther Adv Chronic Dis. 2016;7(5):229–45.
Declercq T, Petrovic M, Azermai M, Vander Stichele R, De Sutter AI, van Driel ML, et al. Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia. Cochrane Database Syst Rev. 2013;4:CD007726.
Defrancesco M, Marksteiner J, Fleischhacker WW, Blasko I. Use of benzodiazepines in Alzheimer’s disease: a systematic review of literature. Int J Neuropsychopharmacol. 2015;18(10):pvy055.
Konovalov S, Muralee S, Tampi RR. Anticonvulsants for the treatment of behavioural and psychological symptoms of dementia: a literature review. Int Psychogeriatr. 2008;20(2):293–308.
Gustafsson M, Isaksson U, Karlsson S, Sandman P-O, Lövheim H. Behavioral and psychological symptoms and psychotropic drugs among people with cognitive impairment in nursing homes in 2007 and 2013. Eur J Clin Pharmacol. 2016;72(8):987–94.
Jacquin-Piques A, Sacco G, Tavassoli N, Rouaud O, Bejot Y, Giroud M, et al. Psychotropic drug prescription in patients with dementia: nursing home residents versus patients living at home. J Alzheimer’s Dis. 2016;49(3):671–80.
Janus SI, van Manen JG, IJzerman MJ, Zuidema SU. Psychotropic drug prescriptions in Western European nursing homes. Int Psychogeriatr. 2016;28(11):1775–90.
Chen Y, Briesacher BA, Field TS, Tjia J, Lau DT, Gurwitz JH. Unexplained variation across us nursing homes in antipsychotic prescribing rates. Arch Intern Med. 2010;170(1):89–95.
Shah SM, Carey IM, Harris T, DeWilde S, Cook DG. Quality of prescribing in care homes and the community in England and Wales. Br J Gen Pract. 2012;62(598):e329–36.
Stevenson DG, Decker SL, Dwyer LL, Huskamp HA, Grabowski DC, Metzger ED, et al. Antipsychotic and benzodiazepine use among nursing home residents: findings from the 2004 National Nursing Home Survey. Am J Geriatr Psychiatry. 2010;18(12):1078–92.
Nørgaard A, Jensen-Dahm C, Gasse C, Hansen ES, Waldemar G. Psychotropic polypharmacy in patients with dementia: prevalence and predictors. J Alzheimer’s Dis. 2017;56(2):707–16.
Rojas-Fernandez C, Mikhail M, Brown SG. Psychotropic and cognitive-enhancing medication use and its documentation in contemporary long-term care practice. Ann Pharmacother. 2014;48(4):438–46.
van der Spek K, Gerritsen DL, Smalbrugge M, Nelissen-Vrancken MH, Wetzels RB, Smeets CH, et al. Only 10% of the psychotropic drug use for neuropsychiatric symptoms in patients with dementia is fully appropriate. The PROPER I-study. Int Psychogeriatr. 2016;28(10):1589–95.
de Oliveira AM, Radanovic M, de Mello PC, Buchain PC, Vizzotto AD, Celestino DL, et al. Nonpharmacological interventions to reduce behavioral and psychological symptoms of dementia: a systematic review. BioMed Res Int. 2015;2015:218980.
Livingston G, Kelly L, Lewis-Holmes E, Baio G, Morris S, Patel N, et al. Non-pharmacological interventions for agitation in dementia: systematic review of randomised controlled trials. Br J Psychiatry. 2014;205(6):436–42.
Edvardsson D, Sandman PO, Borell L. Implementing national guidelines for person-centered care of people with dementia in residential aged care: effects on perceived person-centeredness, staff strain, and stress of conscience. Int Psychogeriatr. 2014;26(7):1171–9.
Daly RL, Bunn F, Goodman C. Shared decision-making for people living with dementia in extended care settings: a systematic review. BMJ Open. 2018;8(6):e018977.
Chenoweth L, Forbes I, Fleming R, King MT, Stein-Parbury J, Luscombe G, et al. PerCEN: a cluster randomized controlled trial of person-centered residential care and environment for people with dementia. Int Psychogeriatr. 2014;26(7):1147–60.
Moniz Cook ED, Swift K, James I, Malouf R, De Vugt M, Verhey F. Functional analysis-based interventions for challenging behaviour in dementia. Cochrane Database Syst Rev. 2012;15(2):Cd006929.
Fraker J, Kales HC, Blazek M, Kavanagh J, Gitlin LN. The role of the occupational therapist in the management of neuropsychiatric symptoms of dementia in clinical settings. Occup Ther Health Care. 2014;28(1):4–20.
Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ. 2015;350:h369.
van der Steen J, Smaling H, Bruinsma M, Scholten R, Vink A. Music-based therapeutic interventions for people with dementia. Cochrane Database Syst Rev. 2018;7:CD003477.
Gerdner LA. Effects of individualized versus classical “relaxation” music on the frequency of agitation in elderly persons with Alzheimer’s disease and related disorders. Int Psychogeriatr. 2000;12(1):49–65.
Livingston G, Sommerlad A, Orgeta V, Costafreda SG, Huntley J, Ames D, et al. Dementia prevention, intervention, and care. Lancet. 2017;390(10113):2673–734.
Tsoi KKF, Chan JYC, Ng YM, Lee MMY, Kwok TCY, Wong SYS. Receptive music therapy is more effective than interactive music therapy to relieve behavioral and psychological symptoms of dementia: a systematic review and meta-analysis. J Am Med Dir Assoc. 2018;19(7):568–76.
Orgeta V, Qazi A, Spector A, Orrell M. Psychological treatments for depression and anxiety in dementia and mild cognitive impairment: systematic review and meta-analysis. Br J Psychiatry. 2015;207(4):293–8.
Woods B, O’Philbin L, Farrell EM, Spector AE, Orrell M. Reminiscence therapy for dementia. Cochrane Database Syst Rev. 2018;3:Cd001120.
Forrester LT, Maayan N, Orrell M, Spector AE, Buchan LD, Soares-Weiser K. Aromatherapy for dementia. Cochrane Database Syst Rev. 2014;25(2):Cd003150.
Lamb SE, Sheehan B, Atherton N, Nichols V, Collins H, Mistry D, et al. Dementia and physical activity (DAPA) trial of moderate to high intensity exercise training for people with dementia: randomised controlled trial. BMJ. 2018;361:k1675.
Forbes D, Forbes SC, Blake CM, Thiessen EJ, Forbes S. Exercise programs for people with dementia. Cochrane Database Syst Rev. 2015;15(4):Cd006489.
Yakimicki ML, Edwards NE, Richards E, Beck AM. Animal-assisted intervention and dementia: a systematic review. Clin Nurs Res. 2018. https://doi.org/10.1177/1054773818756987.
Chenoweth L, King MT, Jeon YH, Brodaty H, Stein-Parbury J, Norman R, et al. Caring for Aged Dementia Care Resident Study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: a cluster-randomised trial. Lancet Neurol. 2009;8(4):317–25.
Low L-F, Brodaty H, Goodenough B, Spitzer P, Bell J-P, Fleming R, et al. The Sydney Multisite Intervention of LaughterBosses and ElderClowns (SMILE) study: cluster randomised trial of humour therapy in nursing homes. BMJ Open. 2013;3:e002072.
Brodaty H, Low L-F, Liu Z, Fletcher J, Roast J, Goodenough B, et al. Successful ingredients in the SMILE study: resident, staff, and management factors influence the effects of humor therapy in residential aged care. Am J Geriatr Psychiatry. 2014;22(12):1427–37.
Verbeek H, Zwakhalen SM, van Rossum E, Ambergen T, Kempen GI, Hamers JP. Effects of small-scale, home-like facilities in dementia care on residents’ behavior, and use of physical restraints and psychotropic drugs: a quasi-experimental study. Int Psychogeriatr. 2014;26(4):657–68.
Harrison SL, Bradley C, Milte R, Liu E, Kouladjian O’Donnell L, Hilmer SN, et al. Psychotropic medications in older people in residential care facilities and associations with quality of life: a cross-sectional study. BMC Geriatr. 2018;18(1):60.
Health Care Financing Administration. Survey procedures and interpretive guidelines for skilled nursing facilities and intermediate care facilities. Baltimore; 1990.
Stoudemire A, Smith DA. OBRA regulations and the use of psychotropic drugs in long-term care facilities: impact and implications for geropsychiatric care. Gen Hosp Psychiatry. 1996;18(2):77–94.
Llorente MD, Olsen EJ, Leyva O, Silverman MA, Lewis JE, Rivero J. Use of antipsychotic drugs in nursing homes: current compliance with OBRA regulations. J Am Geriatr Soc. 1998;46(2):198–201.
Hughes CM, Lapane KL, Mor V, Ikegami N, Jonsson PV, Ljunggren G, et al. The impact of legislation on psychotropic drug use in nursing homes: a cross-national perspective. J Am Geriatr Soc. 2000;48(8):931–7.
Huybrechts KF, Rothman KJ, Brookhart MA, Silliman RA, Crystal S, Gerhard T, et al. Variation in antipsychotic treatment choice across US nursing homes. J Clin Psychopharmacol. 2012;32(1):11–7.
Therapeutic Goods Administration. Risperidone and risk of cerebrovascular adverse events in dementia patients. Med Saf Update. 2015. https://www.tga.gov.au/publication-issue/medicines-safety-update-volume-6-number-4-august-2015#risperidone. Accessed 10 Aug 2018.
Dorsey ER, Rabbani A, Gallagher SA, Conti RM, Alexander GC. Impact of FDA black box advisory on antipsychotic medication use. Arch Intern Med. 2010;170(1):96–103.
Singh RR, Nayak R. Impact of FDA black box warning on psychotropic drug use in noninstitutionalized elderly patients diagnosed with dementia: a retrospective study. J Pharm Pract. 2016;29(5):495–502.
Szczepura A, Wild D, Khan AJ, Owen DW, Palmer T, Muhammad T, et al. Antipsychotic prescribing in care homes before and after launch of a national dementia strategy: an observational study in English institutions over a 4-year period. BMJ Open. 2016;6(9):e009882.
Alldred DP, Kennedy MC, Hughes C, Chen TF, Miller P. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev. 2016;2:Cd009095.
National Institute for Health and Care Excellend. Medication management in nursing homes. Quality statement 5: medication reviews. 2015. https://www.nice.org.uk/guidance/qs85/chapter/quality-statement-5-medication-reviews. Accessed 28 Nov 2018.
Register Federal. Medicare and Medicaid programs; reform of requirements for long-term care facilities. Final rule. Fed Regist. 2016;81(192):68688–872.
Pharmaceutical Society of Australia. Guidelines for pharmacists providing Residential Medication Management Review (RMMR) and Quality Use of Medicines (QUM) services. 2011. www.psa.org.au/site.php?id=6730. Accessed 20 May 2018.
Kallio SE, Kiiski A, Airaksinen MSA, Mantyla AT, Kumpusalo-Vauhkonen AEJ, Jarvensivu TP, et al. Community pharmacists’ contribution to medication reviews for older adults: a systematic review. J Am Geriatr Soc. 2018;66(8):1613–20.
NHS England. Medicines optimisation in care homes. https://www.england.nhs.uk/commissioning/primary-care/pharmacy/medicines-optimisation-in-care-homes/. Accessed 10 Aug 2018.
Nishtala PS, Hilmer SN, McLachlan AJ, Hannan PJ, Chen TF. Impact of residential medication management reviews on drug burden index in aged-care homes: a retrospective analysis. Drugs Aging. 2009;26(8):677–86.
Thiruchelvam K, Hasan SS, Wong PS, Kairuz T. Residential aged care medication review to improve the quality of medication use: a systematic review. J Am Med Dir Assoc. 2017;18(1):87.e1–.e14.
General Medical Council. Reviewing medicines. https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/prescribing-and-managing-medicines-and-devices/reviewing-medicines. Accessed 10 Aug 2018.
Sawan MJ, Jeon YH, Fois RJ, Chen TF. A qualitative study exploring visible components of organizational culture: what influences the use of psychotropic medicines in nursing homes? Int Psychogeriatr. 2016;28(10):1725–35.
Rendina N, Brodaty H, Draper B, Peisah C, Brugue E. Substitute consent for nursing home residents prescribed psychotropic medication. Int J Geriatr Psychiatry. 2009;24(3):226–31.
Plakiotis C, Bell JS, Jeon YH, Pond D, O’Connor DW. Deprescribing psychotropic medications in aged care facilities: the potential role of family members. Adv Exp Med Biol. 2015;821:29–43.
Devanand DP, Mintzer J, Schultz SK, Andrews HF, Sultzer DL, de la Pena D, et al. Relapse risk after discontinuation of risperidone in Alzheimer’s disease. N Engl J Med. 2012;367(16):1497–507.
Brodaty H, Aerts L, Harrison F, Jessop T, Cations M, Chenoweth L, et al. Antipsychotic deprescription for older adults in long-term care: the HALT study. J Am Med Dir Assoc. 2018;19(7):592–600.e7.
Chenoweth L, Jessop T, Harrison F, Cations M, Cook J, Brodaty H. Critical contextual elements in facilitating and achieving success with a person-centred care intervention to support antipsychotic deprescribing for older people in long-term care. BioMed Res Int. 2018;2018:12.
Westbury JL, Gee P, Ling T, Brown DT, Franks KH, Bindoff I, et al. RedUSe: reducing antipsychotic and benzodiazepine prescribing in residential aged care facilities. Med J Aust. 2018;208(9):398–403.
Fossey J, Ballard C, Juszczak E, James I, Alder N, Jacoby R, et al. Effect of enhanced psychosocial care on antipsychotic use in nursing home residents with severe dementia: cluster randomised trial. BMJ. 2006;332(7544):756–61.
Lawrence V, Fossey J, Ballard C, Moniz-Cook E, Murray J. Improving quality of life for people with dementia in care homes: making psychosocial interventions work. Br J Psychiatry. 2012;201(5):344–51.
van der Spek K, Koopmans R, Smalbrugge M, Nelissen-Vrancken M, Wetzels RB, Smeets CHW, et al. The effect of biannual medication reviews on the appropriateness of psychotropic drug use for neuropsychiatric symptoms in patients with dementia: a randomised controlled trial. Age Ageing. 2018;47(3):430–7.
Ballard C, Hanney ML, Theodoulou M, Douglas S, McShane R, Kossakowski K, et al. The dementia antipsychotic withdrawal trial (DART-AD): long-term follow-up of a randomised placebo-controlled trial. Lancet Neurol. 2009;8(2):151–7.
The Royal Australian & New Zealand College of Psychiatrists. Antipsychotic medications as a treatment of behavioural and psychological symptoms of dementia. 2016. https://www.ranzcp.org/Files/Resources/College_Statements/Practice_Guidelines/pg10-pdf.aspx. Accessed 20 Jul 2018.
Reeve E, Ong M, Wu A, Jansen J, Petrovic M, Gnjidic D. A systematic review of interventions to deprescribe benzodiazepines and other hypnotics among older people. Eur J Clin Pharmacol. 2017;73(8):927–35.
Paquin AM, Zimmerman K, Rudolph JL. Risk versus risk: a review of benzodiazepine reduction in older adults. Expert Opin Drug Saf. 2014;13(7):919–34.
Gosselin P, Ladouceur R, Morin CM, Dugas MJ, Baillargeon L. Benzodiazepine discontinuation among adults with GAD: a randomized trial of cognitive-behavioral therapy. J Consult Clin Psychol. 2006;74(5):908–19.
Morin CM, Bastien C, Guay B, Radouco-Thomas M, Leblanc J, Vallieres A. Randomized clinical trial of supervised tapering and cognitive behavior therapy to facilitate benzodiazepine discontinuation in older adults with chronic insomnia. Am J Psychiatry. 2004;161(2):332–42.
Vicens C, Fiol F, Llobera J, Campoamor F, Mateu C, Alegret S, et al. Withdrawal from long-term benzodiazepine use: randomised trial in family practice. Br J Gen Pract. 2006;56(533):958–63.
Orgeta V, Tabet N, Nilforooshan R, Howard R. Efficacy of antidepressants for depression in Alzheimer’s disease: systematic review and meta-analysis. J Alzheimer’s Dis. 2017;58(3):725–33.
Fava GA, Gatti A, Belaise C, Guidi J, Offidani E. Withdrawal symptoms after selective serotonin reuptake inhibitor discontinuation: a systematic review. Psychother Psychosom. 2015;84(2):72–81.
Bergh S, Selbaek G, Engedal K. Discontinuation of antidepressants in people with dementia and neuropsychiatric symptoms (DESEP study): double blind, randomised, parallel group, placebo controlled trial. BMJ. 2012;344:e1566.
Reeve E, Bell JS, Hilmer SN. Barriers to optimising prescribing and deprescribing in older adults with dementia: a narrative review. Curr Clin Pharmacol. 2015;10(3):168–77.
Anderson K, Stowasser D, Freeman C, Scott I. Prescriber barriers and enablers to minimising potentially inappropriate medications in adults: a systematic review and thematic synthesis. BMJ Open. 2014;4(12):e006544.
Turner JP, Edwards S, Stanners M, Shakib S, Bell JS. What factors are important for deprescribing in Australian long-term care facilities? Perspectives of residents and health professionals. BMJ Open. 2016;6(3):e009781.
Zhang Y, Letuchy EM, Carnahan RM. Where are antipsychotics prescribed in nursing homes initiated? J Am Geriatr Soc. 2018;66(6):1082–8.
Sawan M, Chen T, Jeon YH, Hilmer SN. Interventions to reduce antipsychotic prescribing in nursing homes must cross healthcare silos. J Am Geriatr Soc. 2018;66(6):1235–6.
Barry MJ, Edgman-Levitan S. Shared decision making—pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–1.
Kalogianis MJ, Wimmer BC, Turner JP, Tan EC, Emery T, Robson L, et al. Are residents of aged care facilities willing to have their medications deprescribed? Res Soc Admin Pharm. 2016;12(5):784–8.
Jansen J, Naganathan V, Carter SM, McLachlan AJ, Nickel B, Irwig L, et al. Too much medicine in older people? Deprescribing through shared decision making. BMJ. 2016;353:i2893.
Sawan M, Jeon YH, Chen TF. Shaping the use of psychotropic medicines in nursing homes: a qualitative study on organisational culture. Soc Sci Med. 2018;202:70–8.
Sawan M, Jeon YH, Fois RA, Chen TF. Exploring the link between organizational climate and the use of psychotropic medicines in nursing homes: a qualitative study. Res Soc Admin Pharm. 2017;13(3):513–23.
Jennings AA, Foley T, Walsh KA, Coffey A, Browne JP, Bradley CP. General practitioners’ knowledge, attitudes, and experiences of managing behavioural and psychological symptoms of dementia: a mixed-methods systematic review. Int J Geriatr Psychiatry. 2018;7(1):62.
Ailabouni NJ, Nishtala PS, Mangin D, Tordoff JM. Challenges and enablers of deprescribing: a general practitioner perspective. PLoS One. 2016;11(4):e0151066.
Tjia J, Gurwitz JH, Briesacher BA. Challenge of changing nursing home prescribing culture. Am J Geriatr Pharmacother. 2012;10(1):37–46.
Reeve E, Anthony AC, Kouladjian O’Donnell L, Low LF, Ogle SJ, Glendenning JE, et al. Development and pilot testing of the revised Patients’ Attitudes Towards Deprescribing questionnaire for people with cognitive impairment. Australas J Ageing. 2018. https://doi.org/10.1111/ajag.12576.
Reeve E, Low LF, Shakib S, Hilmer SN. Development and validation of the Revised Patients’ Attitudes Towards Deprescribing (rPATD) Questionnaire: versions for older adults and caregivers. Drugs Aging. 2016;33(12):913–28.
Olivieri-Mui BL, Devlin JW, Ochoa A, Schenck D, Briesacher B. Perceptions vs. evidence: therapeutic substitutes for antipsychotics in patients with dementia in long-term care. Aging Ment Health. 2018;22(4):544–9.
Anrys P, Strauven G, Boland B, Dalleur O, Declercq A, Degryse J-M, et al. Collaborative approach to Optimise MEdication use for Older people in Nursing homes (COME-ON): study protocol of a cluster controlled trial. Implement Sci. 2015;11(1):35.
Mahlknecht A, Nestler N, Bauer U, Schüßler N, Schuler J, Scharer S, et al. Effect of training and structured medication review on medication appropriateness in nursing home residents and on cooperation between health care professionals: the InTherAKT study protocol. BMC Geriatr. 2017;17(1):24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Henry Brodaty is an Advisory Board Member for Nutricia. Monica Cations has been employed in the past 5 years to assist with data collection for Alzheimer’s disease drug trials funded by Janssen and Merck. Stephanie Harrison, Tiffany Jessop, Sarah Hilmer and Mouna Sawan report no conflicts of interest.
Funding
No specific funding sources were received for the preparation of this manuscript.
Rights and permissions
About this article
Cite this article
Harrison, S.L., Cations, M., Jessop, T. et al. Approaches to Deprescribing Psychotropic Medications for Changed Behaviours in Long-Term Care Residents Living with Dementia. Drugs Aging 36, 125–136 (2019). https://doi.org/10.1007/s40266-018-0623-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-018-0623-6