Abstract
Background
Sarcopenia, defined as the pathological decline in muscle mass, muscle strength and physical performance with aging, has become one of the geriatric giants because of its increasing prevalence and devastating health effects. The Belgian Society of Gerontology and Geriatrics (BSGG) is currently developing evidence-based guidelines for the prevention and therapy of sarcopenia for use in broad clinical practice. This systematic review summarizes the results of the Working Group on Pharmacology.
Objective
Our objective was to provide an evidence-based overview of the possible pharmacological interventions for sarcopenia with a focus on interventions that have already been studied in systematic reviews or meta-analyses.
Methods
We conducted a systematic umbrella review. Using the electronic databases PubMed and Web of Science, we identified systematic reviews and meta-analyses that assessed the effect of pharmacological interventions on criteria for sarcopenia in subjects aged ≥ 65 years. Study selection, quality assessment and data extraction were performed by two independent reviewers.
Results
We identified seven systematic reviews or meta-analyses, encompassing ten pharmacological interventions: vitamin D, combined estrogen–progesterone, dehydroepiandrosterone, growth hormone, growth hormone-releasing hormone, combined testosterone–growth hormone, insulin-like growth factor-1, pioglitazone, testosterone and angiotensin-converting enzyme inhibitors. Importantly, very few systematic reviews or meta-analyses clearly mentioned baseline sarcopenia status. Therefore, our recommendations are generalised to older people, without specifying whether the muscle effect is more effective in healthy, pre-sarcopenic or sarcopenic older people. Vitamin D had a significant effect on muscle strength and physical performance, especially in women with low baseline values (< 25 nmol/l). Adverse events were rare. Testosterone had a strong effect on muscle mass and a modest to minimal effect on muscle strength and physical performance, respectively, when supplementing men with low serum levels (< 200–300 ng/dl). The adverse events were rare and mild. Insufficient evidence was available to recommend other pharmacological interventions.
Conclusion
Only vitamin D, especially in older women, and testosterone in older men with clinical muscle weakness and low testosterone serum levels can be justified in daily clinical practice to improve muscle mass, muscle strength and/or physical performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
No distinct pharmacological recommendations for healthy, pre-sarcopenic and sarcopenic older people can be made because specific characterization of the sarcopenia status was lacking from most studies. However, recommendations can be made for older people in general. |
Vitamin D—especially in older women with low baseline levels (< 25 nmol/l)—and testosterone—in older men with low baseline levels (< 200–300 ng/dl) and clinical muscle weakness—can be justified in clinical practice to improve muscle mass, muscle strength and/or physical performance. |
Insufficient evidence exists to justify other pharmacological interventions in clinical practice. |
1 Introduction
While a progressive and generalised loss of skeletal muscle mass and strength is inherent to aging, some older people experience accelerated muscle decline with a high risk of adverse outcomes. Below a certain clinical threshold, this accelerated muscle decline is called sarcopenia. Sarcopenia has received increasing attention in both research and public communities. Different definitions and cut-offs exist for sarcopenia, but one of the more commonly used is from the European Working Group on Sarcopenia in Older People (EWGSOP) [1]. They recommend using the presence of both low muscle mass and low muscle function (strength or performance) for the diagnosis of sarcopenia. Consequently, diagnosis requires documentation of criterion 1 (low muscle mass) plus documentation of either criterion 2 (low muscle strength) or criterion 3 (low physical performance) [2]. Other definitions, e.g. from the International Working Group on Sarcopenia (IWGS), require only one or two from the three mentioned criteria to diagnose sarcopenia [1].
The first reason for this growing attention to sarcopenia derives from its increasing prevalence due to global human aging. The EWGSOP points out that sarcopenia affects more than 50 million people today worldwide and that this number will increase to more than 200 million people over the next 40 years [2]. Second, sarcopenia is a predictor of physical disability, poor quality of life and all-cause mortality and is an important risk factor for falls in older people [3].
The underlying (patho)physiology of sarcopenia is complex and still insufficiently understood. Inflammation, hormonal dysregulation, changed neuronal activity, (epi)genetics, nutritional changes and immobility have all been shown to be involved and are highly heterogeneous between individuals [4, 5]. As the exact pathophysiology is unknown, the ultimate (i.e. targeted and highly efficient) therapy for sarcopenia does not yet exist. However, some interventions have already been recognized as having a positive effectiveness/safety profile or are currently under investigation. Three groups of interventions can currently be differentiated: exercise, nutrition and pharmacological.
This clinical review presents the results of the Working Group on Pharmacology within the Sarcopenia Guidelines Development group of the Belgian Society of Gerontology and Geriatrics (BSGG) (see Appendix S1 in the Electronic Supplementary Material [ESM]). The aim is to provide an overview of the possible pharmacological interventions targeting one or more of the three sarcopenia domains (muscle mass, muscle strength or physical performance), with a focus on interventions that have already been studied in systematic reviews or meta-analyses. Therefore, we conducted a systematic umbrella review.
2 Methods
2.1 Search Strategy and Selection Criteria
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for this review [6]. We systematically searched two databases (PubMed and Web of Science) from the earliest date available (1950s for PubMed, 1900 for Web of Science) until 31 October 2017. Keywords used corresponded to the PICOS design (Population: older adults; Intervention: pharmacological; Comparison: non-exposed control; Outcomes: sarcopenia; Study design: systematic review) (see Appendix S2 in the ESM for the full search strategies).
2.2 Study Selection
Systematic reviews in English regarding the effect of pharmacological interventions on one or more of the three criteria of sarcopenia in older adults (≥ 65 years), i.e. muscle mass, muscle strength or physical performance, were eligible for inclusion in the umbrella review. Original studies, editorials, letters to the editor and animal studies were excluded. Two reviewers, blinded for each other’s results, screened the titles and abstracts for eligibility using the Rayyan web application for systematic reviews [7]. The same reviewers then screened the full-text articles of studies. They resolved disagreements by discussion.
2.3 Data Extraction and Methodological Quality Assessment
Two authors completed data extraction using a data extraction form based on a template provided by the Cochrane Collaboration. The authors extracted data regarding the key characteristics of the reviews, including participants, pharmacological treatment and outcomes assessed. No assumptions were made on missing or unclear data. Besides sarcopenia-related outcomes (muscle mass, muscle strength, physical performance), the authors also considered adverse effects.
Two reviewers assessed the methodological quality of the studies using the Assessment of Multiple Systematic Reviews (AMSTAR) tool [8]. This 11-item tool assesses the degree to which review methods avoid bias. The reviewers rated methodological quality as high (score 8–11), moderate (score 4–7) or low (score 0–3). However, they did not assess the quality of studies included within reviews.
To organise the evidence, one investigator systematically synthesized each review’s extracted data, resulting in statements for all reviews mapped to that intervention. In addition, two investigators with clinical experience then independently developed an overall synthesis, beyond a simple summary of the main results of each review. We considered these overall syntheses ‘bottom line statements’ about the main effect of interventions within each intervention. The two investigators resolved disagreements by discussion or by consulting a third investigator. Finally, we rated the quality of the evidence (1 very low, 2 low, 3 moderate, 4 high) supporting each bottom line statement using a method based on the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach for primary evidence [9]. The methods take into account the ‘study design’ (meta-analysis yes/no) and the quality of evidence ratings of the included systematic reviews (AMSTAR) (see Fig. 1).
Method used to rate the quality of the evidence supporting each ‘bottom line’ statement. AMSTAR assessment of multiple systematic reviews [8]
3 Results and Discussion
3.1 Included Studies
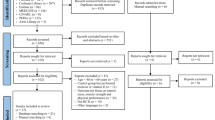
We screened a total of 460 studies for eligibility (Fig. 2). After screening the titles and abstracts, we excluded 446 studies. Eventually, we included seven systematic reviews [10,11,12,13,14,15,16]. AMSTAR scores varied between 1 [12] and 8 [13] (Fig. 3).
AMSTAR scores. Red indicates no; yellow indicates can’t answer/not applicable; green indicates yes. AMSTAR assessment of multiple systematic reviews [8]
The reviews investigated the effect of the following pharmacological interventions: angiotensin-converting enzyme inhibitors (ACEIs) [16], vitamin D [10, 15], beta-estradiol combined with cyclic norethisterone acetate [14], dehydroepiandrosterone (DHEA) [11], growth hormone (GH) [11], growth hormone-releasing hormone (GHRH) [11], insulin-like growth factor (IGF)-1 [11], pioglitazone [14], testosterone [11,12,13] and testosterone combined with GH [11]. Table 1 presents an overview of all included articles.
It was difficult for this umbrella review to distinguish between subjects with sarcopenia and healthy subjects as most systematic reviews did not characterize the sarcopenia or frailty status of the subjects. The most important reason for this is probably that no universally accepted criteria for the diagnosis of sarcopenia exist. Therefore, the conclusions in this umbrella review focus on elderly subjects in a broader sense.
Based on the body of evidence, bottom line statements about the main effects of each intervention—including a rating of the quality of the evidence supporting each bottom line statement—are presented in Table 2. In the following subsections, consideration of each pharmacological intervention starts with a recommendation based on these bottom line statements followed by the results of our umbrella review and discussion.
3.2 Vitamin D
We recommend vitamin D supplementation to improve muscle strength and physical performance in older people, especially in older women with very low baseline levels. Serum calcium should be monitored (low quality of evidence).
Anagnostis et al. [10] summarized the muscle effects of vitamin D supplementation in older women. Although no significant effect was seen of vitamin D supplementation on muscle mass (criterion 1) (pooled standardized mean difference [SMD] 0.058; 95% confidence interval [CI] − 0.118 to 0.233), a small but significant effect was seen on muscle strength (criterion 2) (pooled SMD 0.25; 95% CI 0.01 to 0.48) and physical performance (criterion 3) (e.g. pooled Timed Up and Go [TUG] − 0.19; 95% CI − 0.35 to − 0.02). More prominent effects were seen in patients with deficient baseline vitamin D levels (< 25 nmol/l) and in coadministration with calcium. In addition, a significant decrease in mortality and fall risk was shown when supplementing with vitamin D. Adverse events of vitamin D supplementation described in this review were hypercalcaemia (risk ratio [RR] 3.18; 95% CI 1.17–8.68) and nephrolithiasis (RR 1.17; 95% CI 1.02–1.34), both rare. The meta-analysis by Beaudart et al., encompassing other clinical trials, also suggested a small but significant effect on physical performance (gait speed and TUG) but found no significant effect on muscle mass or muscle strength [15, 17]. It is noteworthy that, in both systematic reviews, most studies concerned supplementation with the inactive forms of vitamin D, i.e. cholecalciferol (D3) or ergocalciferol (D2).
We hypothesize that the more pronounced effects on functional outcomes in contrast to the lack of effect on muscle mass could be explained by vitamin D causing mostly a gain in muscle quality instead of quantity. Indeed, recent studies suggest that activation of intracellular vitamin D receptors in muscle induces a decline of intramuscular lipids, enhancing muscle quality [18, 19]. A recent systematic meta-analysis by Rosendahl-Riise et al. [20], albeit not retrieved in our search because it does not focus on the syndrome of sarcopenia, found no significant effect of vitamin D supplementation on muscle strength and physical performance in older people, as measured by grip strength and TUG, respectively. This contrast with our results could be explained by the large heterogeneity of the studies in the meta-analysis (I2 ≥ 95%) and the focus on community-dwelling older people. The heterogeneity was both on the level of patient characteristics and on the level of the intervention. Concerning the side effects of vitamin D, a Cochrane systematic review of vitamin D/calcium supplementation on preventing fractures in older people found a small but significant increase in gastrointestinal symptoms and renal disease associated with vitamin D and calcium intake, probably related to the hypercalcaemia and nephrolithiasis, in accordance with our results [21]. Interestingly, high vitamin D doses (> 1000 IU daily) seem to increase the risk of falling in older people [22]. It must be highlighted that most studies so far have been conducted in postmenopausal women, and clinical trials in older men are lacking. In conclusion, it seems that vitamin D supplementation, especially in older women, can be beneficial to improve muscle strength or physical performance, mostly when supplementing those with very low baseline vitamin D levels (< 25 nmol/l), without ‘over-supplementing’ (< 1000 IU daily). However, it is clear that more subgroup analyses are needed to find subjects with a ‘good’ genetic profile, sarcopenia, and vitamin D baseline levels that benefit from a particular dose and duration of vitamin D/calcium supplementation, in line with the concept of personalized medicine. Indeed, current studies are already focusing on subgroup analyses, e.g. the meta-analysis in community-dwelling older people from Rosendahl-Riise et al. [20], and investigating genetic variants responsible for vitamin D status and dose response [23, 24].
3.3 Beta-Estradiol + Cyclic Norethisterone Acetate
We do not recommend the combination of estrogen and progesterone to improve muscle mass, muscle strength or physical performance in older people (very low quality of evidence).
Of the included systematic reviews, only Poggiogalle et al. [14] discussed the combination of estrogen and progesterone. They found a small but significant improvement in muscle mass after sex hormone-replacement therapy in postmenopausal women. However, we found no results on muscle strength, physical performance or adverse events in this systematic review [14].
A meta-analysis published in 2009 [25] found a beneficial effect on muscle strength from estrogen-based treatments in postmenopausal women. In contrast, a large randomized clinical trial in 2010 [26] found no significant improvement in muscle strength or physical performance with hormone-replacement therapy. More subgroup analyses are needed in the future to elucidate this discrepancy.
3.4 Dehydroepiandrosterone
We do not recommend DHEA supplementation to improve muscle mass, muscle strength or physical performance in older people (very low quality of evidence).
Dehydroepiandrosterone, a steroid that can be transformed into estrogen or testosterone in the body, could possibly have some effect on muscle strength, but the results were inconclusive, and data on muscle mass, physical performance and adverse events were lacking [11].
Although the only included systematic review [11] dates from 2004, later trials and reviews not included in our umbrella review remain inconclusive about the effects on muscle of DHEA [27]. It needs to be pointed out that no randomized clinical trial of DHEA supplementation measuring one of the three sarcopenia domains was published in the last 5 years. One of the possible reasons could be the status of relatively cheap over-the-counter DHEA, making it less interesting for pharmaceutical companies. More studies will be needed in the future to enable conclusions to be made about the muscle benefits of DHEA in older people.
3.5 Growth Hormone
We do not recommend GH supplementation to improve muscle mass, muscle strength or physical performance in older people (very low quality of evidence).
Borst [11] concluded that, although GH replacement in older subjects increases muscle mass, it does not univocally improve muscle strength or physical performance and has a high incidence of adverse events, making it inappropriate as a muscle intervention in older people. Adverse events described were fluid retention, gynaecomastia, orthostatic hypotension, carpal tunnel compression, hyperglycaemia, arthralgia and general malaise. Borst [11] reported a drop-out rate in some clinical trials of around 40% in the supplemented group versus 10% in the placebo group, attributed to the adverse events.
A long-term clinical trial (10 years) found a mitigation of the expected age-related decline in muscle strength when supplementing GH in older people with overt pituitary disease [28]. However, this trial was not controlled, and the baseline IGF-1 levels, downstream targets of GH, were much lower than expected in older people without overt pituitary disease. No long-term controlled clinical trials in older people without overt pituitary disease exist to recommend GH supplementation.
3.6 Growth Hormone-Releasing Hormone and Insulin-Like Growth Factor 1
We do not recommend GH-releasing hormone (GHRH) or IGF-1 supplementation to improve muscle mass, muscle strength or physical performance in older people (very low quality of evidence).
The GH/IGF-1 pathway is complex, and it may be that a better efficacy/safety profile is obtained when supplementing with pathway molecules other than GH. In their systematic review, Borst [11] discussed GH and GHRH and IGF-1, upstream and downstream molecules from GH, respectively. Some studies found that muscle mass and strength increased when supplementing GHRH in healthy older people, and muscle strength was increased when supplementing IGF-1 in older women after hip fracture. No data were provided on physical performance. Both molecules were well tolerated and had a good safety profile, with only transient hyperlipidaemia reported [11].
Recent studies seem to confirm the potency of GHRH and the related GH secretagogue receptor (GHSR) agonists and ghrelin analogues to combat muscle aging in older people [29,30,31]. However, no firm conclusions can be made as yet.
3.7 Pioglitazone
We do not recommend pioglitazone to improve muscle mass, muscle strength or physical performance in older people (very low quality of evidence).
Poggiogalle et al. [14] discussed the effect of pioglitazone, a peroxisome proliferator-activated receptor gamma (PPARγ) agonist, on muscle mass. Although a positive significant effect of pioglitazone was seen on visceral fat loss in obese men, only a small, non-significant effect was measured on muscle mass gain in this population. Our results did not contain data on muscle strength, physical performance or adverse events.
One other randomized clinical trial [32], not included in the review by Poggiogalle et al. [14], investigated the effects of pioglitazone on muscle outcomes in older people. In accordance with our results, this study [32] did not show a strong, unequivocal effect on muscle outcome, instead only a potentiating effect of pioglitazone on muscle power in women, but not in men, when associated with resistance training. Reasons for this sex difference are not clear. It is thought that the potential positive muscle effects of pioglitazone are mediated by an improved fatty acid metabolism, a known effect of PPARγ agonists [33].
3.8 Testosterone
We consider testosterone supplementation a possible intervention to improve muscle mass and muscle strength in older men with low serum testosterone levels (< 200–300 ng/dl) and clinical muscle weakness. Haematocrit, lipid profile and prostatic parameters should be monitored (high quality of evidence).
Three systematic reviews/meta-analyses with data on testosterone supplementation targeting one or more sarcopenia domains met our eligibility criteria [11,12,13]. All discussed supplementation only in older men. Although a consensus exists about the clear effect on muscle mass, a less pronounced effect was seen on muscle strength and an even lesser effect on physical performance. The less pronounced effects on muscle strength and physical performance can be explained by insufficient treatment duration, low test sensitivity and absence of androgen deficiency at baseline. Possible adverse events of testosterone supplementation were fluid retention, gynaecomastia, worsening of sleep apnoea, polycythaemia and acceleration of benign or malign prostatic tumours. However, physiological doses of testosterone supplementation in both healthy and older people with frailty were well tolerated: most studies found only mild polycythaemia without an increase in prostatic or cardiovascular events [11,12,13].
These results align with those from two recent large trials: the Testosterone’s Effects on Atherosclerosis Progression in Aging Men (TEAAM) trial and the Testosterone Trials (TTrials), in which testosterone supplementation in community-dwelling healthy older men was associated with only modest improvements in physical performance and was considered safe [34, 35]. Recent studies measuring cardiovascular endpoints in older men supplemented with testosterone also suggest a beneficial cardiovascular effect in those with low levels [36, 37]. Further clinical investigations, including pharmacogenomics and other new insights from personalized medicines, are needed to select individuals who would benefit most from testosterone supplementation. However, pending the results of such trials, we currently recommend that a trial phase may be worthwhile in older patients with clinical muscle weakness and low serum testosterone levels. If no clinical effects are seen after 6 months, supplementation should be stopped [38]. A practical guide to starting testosterone supplementation can be found in the review by De Spiegeleer et al. [38].
3.9 Testosterone + Growth Hormone
We do not recommend the combination of testosterone and GH supplementation to improve muscle mass, muscle strength or physical performance in older people (very low quality of evidence).
Borst [11] reviewed the effects of testosterone combined with GH. They found an increase in muscle mass in healthy older men but no significant effect on muscle strength. No data were available on physical performance or adverse events.
More recent trials do suggest a synergistic effect [39, 40]. However, long-term studies will be needed to elucidate both the possible effects and the adverse events.
3.10 Angiotensin-Converting Enzyme Inhibitors
We do not recommend ACEIs to improve muscle mass, muscle strength or physical performance in older people (moderate quality of evidence).
One systematic meta-analysis reported the effects of ACEIs on muscle strength and physical performance [16]. Three different ACEIs were used in the included original studies: enalapril, perindopril and fosinopril. The meta-analysis did show a modest positive effect in favour of the intervention, but no significant results were obtained. They attributed the reason for the non-significance to the short intervention times (5–9 months) and limitations of the meta-analysis (high heterogeneity and limited number of studies, with only studies between 2000 and 2015). No data on muscle mass or possible adverse events were available.
More recent clinical trials not included in the systematic review also found no significant effect of ACEIs on one of the three sarcopenia criteria [41, 42]. However, it is speculated that subgroups of older people, e.g. with heart failure or with severe sarcopenic, might benefit from ACEIs in terms of muscle outcomes [1, 43]. It might also be that some ACEIs are superior to others, contradicting the idea of a class effect. Further studies are ongoing. As yet, there is no evidence for the use of ACEIs to improve muscle mass, muscle strength or physical performance in older people.
3.11 Strengths and Limitations
The most important strength of the umbrella-review method is the power to efficiently extract clinically relevant information on which general consensus exists, in contrast to conclusions from one research group, i.e. an umbrella review considers for inclusion the highest level of evidence. Our literature search is also systematic in nature, in accordance with the PRISMA guidelines, which provides a higher level of evidence than a narrative review. Because our umbrella review depends on the quality of the systematic reviews/meta-analyses, we assessed this quality using the AMSTAR criteria.
A limitation inherent to our strict search terms (see Sect. 2.1) is the low total number of eligible reviews (seven reviews in total). In combination with the often low quality of the systematic reviews/meta-analyses, this results in low to moderate ratings of evidence supporting most bottom line statements. Another limitation, inherent to an umbrella review, is that we did not evaluate the quality of the individual randomized clinical trials or analyse the clinical trials to the level of the raw data. Lastly, physical activity and nutrition, two interventions with generally accepted effects against sarcopenia, and pharmacological interventions not yet discussed in systematic reviews or meta-analyses (e.g. myostatin inhibitors, selective androgen receptor modulators [SARMs]), were outside the scope of this review.
4 Conclusion
Based on the results of this umbrella review, we conclude that vitamin D—especially in older women with very low baseline levels (< 25 nmol/l)—and testosterone—in men with clinical muscle weakness and low serum testosterone levels (< 200–300 ng/dl)—are the only pharmacological interventions that could be justified in clinical practice to improve one or more of the three sarcopenia domains (muscle mass, muscle strength and physical performance). Scientific evidence for other pharmacological treatments, including combined estrogen–progesterone, DHEA, GH, GHRH, combined testosterone–GH, IGF-1, pioglitazone and ACEIs, is insufficient.
References
von Haehling S, Ebner N, dos Santos MR, Springer J, Anker AD. Muscle wasting and cachexia in heart failure: mechanisms and therapies. Nat Rev Cardiol. 2017;14(6):323–41.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing. 2010;39(4):412–23.
Visser M, Schaap LA. Consequences of sarcopenia. Clin Geriatr Med. 2011;27(3):387–99.
Narici MV, Maffulli N. Sarcopenia: characteristics, mechanisms and functional significance. Br Med Bull. 2010;95(1):139–59.
Urano T, Inoue S. Recent genetic discoveries in osteoporosis, sarcopenia and obesity. Endocr J. 2015;62(6):475–84.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10.
Austin TM, Richter RR, Sebelski CA. Introduction to the GRADE approach for guideline development: considerations for physical therapist practice. Phys Ther. 2014;94(11):1652–9.
Anagnostis P, Dimopoulou C, Karras S, Lambrinoudaki I, Goulis DG. Sarcopenia in post-menopausal women: Is there any role for vitamin D? Maturitas. 2015;82(1):56–64.
Borst SE. Interventions for sarcopenia and muscle weakness in older people. Age Ageing. 2004;33(6):548–55.
O’Connell MD, Tajar A, Roberts SA, Wu FC. Do androgens play any role in the physical frailty of ageing men? Int JAndrol. 2011;34(3):195–211.
Ottenbacher KJ, Ottenbacher ME, Ottenbacher AJ, Acha AA, Ostir GV. Androgen treatment and muscle strength in elderly men: a meta-analysis. J Am Geriatr Soc. 2006;54(11):1666–73.
Poggiogalle E, Migliaccio S, Lenzi A, Donini LM. Treatment of body composition changes in obese and overweight older adults: insight into the phenotype of sarcopenic obesity. Endocrine. 2014;47(3):699–716.
Beaudart C, Dawson A, Shaw SC, Harvey NC, Kanis JA, Binkley N, et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int. 2017;28(6):1817–33.
Zhou LS, Xu LJ, Wang XQ, Huang YH, Xiao Q. Effect of angiotensin-converting enzyme inhibitors on physical function in elderly subjects: a systematic review and meta-analysis. Drugs Aging. 2015;32(9):727–35.
Vasquez-Morales A, Wanden-Berghe C, Sanz-Valero J. Exercise and nutritional supplements; effects of combined use in people over 65 years; a systematic review. Nutr Hosp. 2013;28(4):1077–84.
Ceglia L, Niramitmahapanya S, Morais MD, Rivas DA, Harris SS, Bischoff-Ferrari H, et al. A randomized study on the effect of vitamin D-3 supplementation on skeletal muscle morphology and vitamin D receptor concentration in older women. J Clin Endocrinol Metab. 2013;98(12):E1927–35.
Chanet A, Salles J, Guillet C, Giraudet C, Berry A, Patrac V, et al. Vitamin D supplementation restores the blunted muscle protein synthesis response in deficient old rats through an impact on ectopic fat deposition. J Nutr Biochem. 2017;46:30–8.
Rosendahl-Riise H, Spielau U, Ranhoff AH, Gudbrandsen OA, Dierkes J. Vitamin D supplementation and its influence on muscle strength and mobility in community-dwelling older persons: a systematic review and meta-analysis. J Hum Nutr Diet. 2017;30(1):3–15.
Avenell A, Mak JCS, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev. 2014;(4):CD000227.
Dawson-Hughes B. Vitamin D and muscle function. J Steroid Biochem Mol Biol. 2017;173:313–6.
Zhang MZ, Zhao LJ, Zhou Y, Badr R, Watson P, Ye A, et al. SNP rs11185644 of RXRA genes identified for dose-response variability to vitamin D3 supplementation: a randomized clinical trial. Sci Rep. 2017;7:40593.
Takiar R, Lutsey PL, Zhao D, Guallar E, Schneider ALC, Grams ME, et al. The associations of 25-hydroxyvitamin D levels, vitamin D binding protein gene polymorphisms, and race with risk of incident fracture-related hospitalization: Twenty-year follow-up in a bi-ethnic cohort (the ARIC Study). Bone. 2015;78:94–101.
Greising SM, Baltgalvis KA, Lowe DA, Warren GL. Hormone therapy and skeletal muscle strength: a meta-analysis. J Gerontol A Biol Sci Med Sci. 2009;64(10):1071–81.
Michael YL, Gold R, Manson JE, Keast EM, Cochrane BB, Woods NF, et al. Hormone therapy and physical function change among older women in the Women’s Health Initiative: a randomized controlled trial. Menopause. 2010;17(2):295–302.
Baker WL, Karan S, Kenny AM. Effect of dehydroepiandrosterone on muscle strength and physical function in older adults: a systematic review. J Am Geriatr Soc. 2011;59(6):997–1002.
Gotherstrom G, Elbornsson M, Stibrant-Sunnerhagen K, Bengtsson BA, Johannsson G, Svensson J. Muscle strength in elderly adults with GH deficiency after 10 years of GH replacement. Eur J Endocrinol. 2010;163(2):207–15.
White HK, Petrie CD, Landschulz W, MacLean D, Taylor A, Lyles K, et al. Effects of an oral growth hormone secretagogue in older adults. J Clin Endocrinol Metab. 2009;94(4):1198–206.
Veldhuis JD, Patrie JT, Frick K, Weltman JY, Weltman A. Sustained growth hormone (GH) and insulin-like growth factor I responses to prolonged high-dose twice-daily GH-releasing hormone stimulation in middle-aged and older men. J Clin Endocrinol Metab. 2004;89(12):6325–30.
Veldhuis JD, Patrie JM, Frick K, Weltman JY, Weltman AL. Administration of recombinant human GHRH-1,44-amide for 3 months reduces abdominal visceral fat mass and increases physical performance measures in postmenopausal women. Eur J Endocrinol. 2005;153(5):669–77.
Marsh AP, Shea MK, Locke RMV, Miller ME, Isom S, Miller GD, et al. Resistance training and pioglitazone lead to improvements in muscle power during voluntary weight loss in older adults. J Gerontol A Biol Sci Med Sci. 2013;68(7):828–36.
Yokota T, Kinugawa S, Hirabayashi K, Suga T, Takada S, Omokawa M, et al. Pioglitazone improves whole-body aerobic capacity and skeletal muscle energy metabolism in patients with metabolic syndrome. J Diabetes Investig. 2017;8(4):535–41.
Snyder PJ, Bhasin S, Cunningham GR, Matsumoto AM, Stephens-Shields AJ, Cauley JA, et al. Effects of testosterone treatment in older men. N Engl J Med. 2016;374(7):611–24.
Storer TW, Basaria S, Traustadottir T, Harman SM, Pencina K, Li ZY, et al. Effects of testosterone supplementation for 3 Years on muscle performance and physical function in older men. J Clin Endocrinol Metab. 2017;102(2):583–93.
Traish AM, Haider A, Haider KS, Doros G, Saad F. Long-term testosterone therapy improves cardiometabolic function and reduces risk of cardiovascular disease in men with hypogonadism: a real-life observational registry study setting comparing treated and untreated (control) groups. J Cardiovasc Pharmacol Ther. 2017;22(5):414–33.
Elagizi A, Kohler TS, Lavie CJ. Testosterone and cardiovascular health. Mayo Clin Proc. 2018;93(1):83–100.
De Spiegeleer A, Petrovic M, Boeckxstaens P, Van den Noortgate N. Treating sarcopenia in clinical practice: where are we now? Acta Clin Belg. 2016;71(4):197–205.
Sattler FR, Castaneda-Sceppa C, Binder EF, Schroeder ET, Wang Y, Bhasin S, et al. Testosterone and growth hormone improve body composition and muscle performance in older men. J Clin Endocrinol Metab. 2009;94(6):1991–2001.
Giannoulis MG, Sonksen PH, Umpleby M, Breen L, Pentecost C, Whyte M, et al. The effects of growth hormone and/or testosterone in healthy elderly men: a randomized controlled trial. J Clin Endocrinol Metab. 2006;91(2):477–84.
Shrikrishna D, Tanner RJ, Lee JY, Natanek A, Lewis A, Murphy PB, et al. A randomized controlled trial of angiotensin-converting enzyme inhibition for skeletal muscle dysfunction in COPD. Chest. 2014;146(4):932–40.
Spira D, Walston J, Buchmann N, Nikolov J, Demuth I, Steinhagen-Thiessen E, et al. Angiotensin-converting enzyme inhibitors and parameters of sarcopenia: relation to muscle mass, strength and function: data from the Berlin Aging Study-II (BASE-II). Drugs Aging. 2016;33(11):829–37.
Band MM, Sumukadas D, Struthers AD, Avenell A, Donnan PT, Kemp PR, et al. Leucine and ACE inhibitors as therapies for sarcopenia (LACE trial): study protocol for a randomised controlled trial. Trials. 2018;19(1):6.
Sumukadas D, Band M, Miller S, Cvoro V, Witham M, Struthers A, et al. Do ACE inhibitors improve the response to exercise training in functionally impaired older adults? A randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2014;69(6):736–43.
Bhasin S, Woodhouse L, Casaburi R, Singh AB, Mac RP, Lee M, et al. Older men are as responsive as young men to the anabolic effects of graded doses of testosterone on the skeletal muscle. J Clin Endocrinol Metab. 2005;90:678–88.
Srinivas-Shankar U, Roberts SA, Connolly MJ, O’Connell MDL, Adams JE, Oldham JA, et al. Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab. 2010;95:639–50.
Acknowledgements
The Sarcopenia Guideline Development Group of the BSGG includes the following members: Bautmans I, Beaudart C, Beckwée D, Beyer I, Bruyère O, De Breucker S, De Cock A-M, Delaere A, de Saint-Hubert M, De Spiegeleer A, Gielen E, Perkisas S, Vandewoude M.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Conflict of interest
Anton De Spiegeleer, David Beckwée, Ivan Bautmans and Mirko Petrovic have no conflicts of interest that are directly relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
De Spiegeleer, A., Beckwée, D., Bautmans, I. et al. Pharmacological Interventions to Improve Muscle Mass, Muscle Strength and Physical Performance in Older People: An Umbrella Review of Systematic Reviews and Meta-analyses. Drugs Aging 35, 719–734 (2018). https://doi.org/10.1007/s40266-018-0566-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-018-0566-y