Abstract
Background
Pharmacotherapy with statins (HMG-CoA reductase inhibitors) is the cornerstone for lipid management in individuals with or at risk of developing cardiovascular diseases. Although the clinical benefits of statins are established for both women and men, there is evidence of a gender difference in their use. The current study extends prior scientific research by estimating the extent to which individual-level variables may explain gender differences in statin use by using a post-regression non-linear decomposition technique.
Objective
The objective of this study was to estimate the magnitude of gender differences in statin use among the elderly and examine individual-level variables that can explain the gender differences in statin use among elderly individuals with or at risk of cardiovascular diseases.
Methods
A retrospective cross-sectional study design was adopted. Data were derived from the 2005 Medicare Current Beneficiary Survey (MCBS), a nationally representative survey of Medicare beneficiaries in the US. The analytic study sample consisted of community-dwelling elderly Medicare beneficiaries, aged 65 years or older, who had reported any of the following conditions: heart disease, hyperlipidaemia or diabetes mellitus, and who were alive during the observation year. Chi-square tests were used to evaluate the unadjusted associations between gender and statin use for each of the characteristics. Multivariate logistic regressions were used to evaluate the relationship between gender and statin use. A post-regression non-linear decomposition approach was used to understand individual-level variables that could explain gender differences in statin use.
Results
Among 5,508 elderly, 47.2 % of the women and 55.5 % of the men reported any statin use in 2005, which translates to an 8.3 percentage point difference in statin use. In the multivariate logistic regression on statin use, women were 21 % less likely than men to use statins (adjusted odds ratio = 0.79; 95 % CI 0.69, 0.89). Post-regression non-linear decomposition analysis revealed that of the 8.3 percentage point difference in statin use, 29.5 % was explained by the individual-level variables. Lifestyle risk factors accounted for most of the explained portion of the gender difference in statin use.
Conclusions
Among elderly Medicare beneficiaries, women were less likely than men to report any use of statins. Less than one third of the total gender difference in statin use was attributed to individual-level variables such as demographics, economic status, physical health status, depression and lifestyle risk factors. Further research is needed to identify whether provider and/or organizational-level factors can further explain the gender difference in statin use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Increased plasma cholesterol levels, especially low-density lipoprotein cholesterol (LDL-C) levels, have been found to be significantly associated with a high risk of cardiovascular diseases (CVDs) [1]. In this context, 3-hydroxy-3-methyl-glutaryl-CoA reductase inhibitors (HMG-CoA reductase inhibitors), commonly known as statins, have been shown to decrease LDL-C levels, leading to a reduction in mortality, CVD events, such as myocardial infarction, as well as fatal and non-fatal strokes in both women and men [2–4]. In elderly individuals undergoing statin therapy, one clinical trial has documented a twofold absolute risk reduction of all-cause and CVD-specific mortality [5]. Similarly, the Heart Protection Study (HPS) and PROspective Study of Pravastatin in the Elderly at Risk (PROSPER) study demonstrated the efficacy of statins in the reduction of mortality among elderly individuals [6, 7].
Due to the beneficial effects of statin therapy on survival, current guidelines suggest the use of statins for LDL-C reduction [8]. For example, the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) recommends pharmacotherapy with statins based on the individual-level risk score to achieve targeted levels of <2.59 mmol/L (<100 mg/dL) among those with diabetes mellitus or CVD [8]. LaRosa [9], in his review article, concluded that identical benefits of lower LDL-C levels were obtained in both women and men, and therefore suggested that statin therapy should be administered to individuals with coronary artery disease (CAD) and those at increased risk of CAD, irrespective of gender.
While the beneficial effects of statin therapy have been reported in both women and men among those with established CVD, there is some evidence of gender differences in statin use. However, while there are many studies on gender differences in statin use among adults [10–18], there are only a handful of studies on how gender affects use of statins among elderly individuals aged 65 years and older [19–21]. These studies have generated mixed findings. In one study, which linked medical claims data on high-risk individuals who were hospitalized for myocardial infarction in New Jersey and Pennsylvania, USA, men were less likely to receive statins than women [19]. However, among individuals with CAD and diabetes from the National Health and Nutrition Examination Survey for the years 2001 through 2006, elderly women in the age group between 70 and 74 years were less likely to use statins (62.3 %) than men in the same age group (71.2 %) [20]. Furthermore, among all veterans with diabetes, it was reported that women over age 65 years were less likely to use lipid-lowering therapies (84 %) than men (86 %) [21].
While some of these findings could be due to different subpopulations, a comprehensive analysis of statin use among the elderly who are at risk of developing or are presently diagnosed with cardiovascular conditions is yet to be done. Our literature review highlights the need for examining gender difference in statin use among elderly individuals with established heart disease, diabetes, and those with hyperlipidaemia who may be at high risk for CVD. In addition, it was noted that studies that examined gender difference used gender as one of the independent variables within a multivariate framework; however, they did not evaluate the extent to which each of the individual-level variables contributed to gender differences in statin use.
The current study extends the literature by adopting a post-regression approach to explain factors that may contribute to gender difference in the use of statins among elderly Medicare beneficiaries. Examination of gender difference in statin use among the elderly is important because with increased age there is an elevation of CVD risk [22, 23]. Furthermore, analysing the use of statins will help identify subgroups that are at risk of not receiving statins, which could be beneficial in reducing LDL-C levels and improving survival.
Therefore, the primary objective of the study was to estimate the magnitude of differences in statin use by gender among the elderly population, using data from a nationally representative survey of Medicare beneficiaries. The extent to which individual-level variables such as demographics, economic status, physical health status, depression and lifestyle risk factors explain the gender differences in statin use were also analysed in this study.
2 Methods
2.1 Study Design
This study adopted a retrospective cross-sectional study design utilizing data from the 2005 Medicare Current Beneficiary Survey (MCBS).
2.1.1 Data Source
The MCBS is a nationally representative survey of Medicare beneficiaries in the USA, sponsored by the Centers for Medicare & Medicaid Services (CMS). According to the CMS, the MCBS is the “only comprehensive source of information on the health status, health care use and expenditures, health insurance coverage, and socioeconomic and demographic characteristics of the entire spectrum of Medicare beneficiaries” [24]. The MCBS can be used for both cross-sectional and longitudinal designs. The MCBS is described as the “best of both worlds” [25] because it combines Medicare data from claims and non-Medicare data from surveys of the Medicare beneficiaries. Survey data were collected by using in-depth computer-assisted personal interviews and were conducted every 4 months to capture healthcare utilization (including prescriptions filled) and non-Medicare payment sources as reported by respondents. The respondents were interviewed 12 times over a 4-year period to collect three complete years of utilization data. The current study used the annual data from the calendar year 2005 ‘Cost and Use’ files.
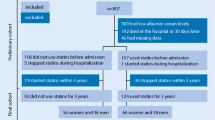
2.1.2 Analytical Sample
Elderly Medicare beneficiaries who reported diabetes, heart disease or hyperlipidaemia comprised the analytic sample. Additional restrictions included the following inclusion criteria: the individual was (1) community dwelling; (2) aged 65 years and older; and (3) reported to be alive throughout the study period. The final sample consisted of Medicare beneficiaries who had heart disease, hyperlipidaemia and/or diabetes. Moreover, individuals with end-stage renal disease (ESRD) and end-stage liver disease (ESLD) identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes of ESRD (585.6) and ESLD (155.0, 571.0–9) were excluded as statins are contraindicated in these conditions [26, 27].
2.2 Measures
2.2.1 Dependent Variable: Statin Use
Statin use was derived from annual self-reported prescription drug use data. Statins were identified using generic and brand name drugs and included lovastatin, simvastatin, atorvastatin, fluvastatin, pravastatin, rosuvastatin, Mevacor®, Zocor®, Lipitor®, Lescol®, Lescol® XL, Pravachol® and Crestor®. Elderly Medicare beneficiaries with any use of these drugs were categorized as ‘statin users.’
2.2.2 Key Independent Variable: Gender
Gender (women and men) was derived from survey reports. Men served as the reference category in the multivariate regressions.
2.2.3 Other Independent Variables
Other individual-level variables consisted of demographic, economic, prescription drug coverage, health status, functional status, depression and lifestyle risk factors. Demographic variables consisted of race/ethnicity (White, African American, Latino and other), age (65–69, 70–74 and 75 years and older), marital status (married, widowed, divorced/separated and other) and area of residence (metropolitan and non-metropolitan). Economic characteristics included education, poverty status and prescription drug coverage. Education was categorized into four groups: (1) less than high school; (2) high school; (3) some college; and (4) college graduate and above. Poverty status was measured as a percentage of the federal poverty level using personal income, which was categorized into two levels: <200 %; and ≥200 % of federal poverty line [28]. A prescription drug coverage variable was constructed for every individual as Medicare Part D prescription drug coverage was not enacted until 2006. Prescription drug coverage was computed using third-party payment for prescription drugs, questions pertaining to whether his or her plan offers drug coverage, and receipt of Medicaid. This approach has been used in previously published studies when using data from the MCBS [29].
Physical health status included perceived health (excellent, very good, good, fair or poor) and functional status [defined using the reported number of limitation in activities of daily living (ADLs): none, 1–2 and 3–6]. Depression was identified on the basis of receipt of a depression diagnosis using the ICD-9-CM codes [30]. Lifestyle risk factors consisted of smoking and obesity measured with body mass index (BMI). Smoking status was classified into three different groups: (1) never smoked; (2) past smoker; and (3) current smoker. BMI was categorized into three different classes: (1) underweight or normal (BMI <25 kg/m2); (2) overweight (BMI ≥25–29.9 kg/m2); and (3) obese or morbidly obese (BMI ≥30 kg/m2) [31].
For the post-regression non-linear decomposition analysis, all of the independent variables were combined according to specific domains, which included demographic (age, race/ethnicity, marital status, metropolitan residence), economic (education, poverty status, prescription drug coverage), physical health status (perceived health, functional status), depression and lifestyle risk factors (BMI categories and smoking status), to understand to what extent these specific domains were able to explain the gender difference in statin use.
2.3 Statistical Methods
Chi-square (χ2) tests were used to test for statistically significant differences in characteristics between women and men. To understand the unadjusted association between statin use and gender, significant group differences were tested for each level of individual-level variables. For example, the relationship between statin use and gender was examined among White individuals. Similar methods have been used to test subgroup differences in other published work [31–34]. To examine the association between statin use and gender, after controlling for all individual-level variables, adjusted logistic regressions were conducted separately for men, women and the two combined (women and men). To examine the extent to which individual-level variables explained the gender difference in statin use, a post-regression non-linear decomposition technique was used [35].
2.3.1 Decomposition Technique
As indicated in Sect. 1, previous work has often used gender as one of the independent variables within a multivariate framework and has not examined how much of the total gender difference in statin use was explained by different independent variables included in the model(s). The advantage of a decomposition technique lies in identifying which characteristics accounted for how much of the gender differences in statin use. The technique uses the parameter estimates (beta coefficients) from the regression and differences in individual characteristics between women and men to distinguish total gender difference in statin use into two components: one component that is explained by differences in individual-level variables (e.g. differences in the distribution of demographic characteristics, economic characteristics, physical health status, etc.) among women and men, and another component that is unexplained. The unexplained component could be due to differences in the regression parameter estimates between women and men or unobservable and/or unmeasured independent variables, provider-, organizational- and neighbourhood-level characteristics that were not included in the model.
Since the dependent variable was categorical (use vs. non-use of statins), a non-linear decomposition technique proposed by Fairlie was used [35, 36]. Decomposition techniques were originally used to explain differences in continuous variables such as wages and earnings [37]. Under this approach, the results may vary depending on which group is used as a reference (i.e. women or men), which is often referred to as the ‘index number problem’. For example, one could use parameter estimates obtained from regression among women or men in evaluating the explained component of gender differences. To solve this index number problem, studies have suggested using regression estimates from pooled regressions [38]. Therefore, in the current study a range of estimates using regression coefficients from pooled data, women and men are presented to distinguish between ‘explained’ and ‘unexplained’ portions of the gender difference in statin use.
All analyses controlled for the complex sampling design of MCBS and were conducted using SAS® version 9.2 (SAS Institute Inc., Cary, NC, USA). STATA® statistical software version 10 (Stata Corporation, College Station, TX, USA) was used to perform the non-linear decomposition.
3 Results
Table 1 summarizes the demographic, economic, health status, depression and lifestyle risk characteristics of the study population by gender. Women constituted approximately 56 % (sample n = 5,508) of the study sample. Based on χ2 statistics, all of the characteristics except diabetes mellitus, hyperlipidaemia and area of residence were significantly different between women and men. For example, with regard to lifestyle risk factors, a higher proportion of women than men (26.7 % vs. 22.5 %) were reported to be obese/morbidly obese; a higher proportion of men were current-smokers (11.0 %) than women (7.3 %).
Among women, 47.2 % were statin users and 55.5 % of men were statin users. This translates into an 8.3 percentage point difference in statin use between women and men. Unadjusted logistic regressions for women on statin use with men as the reference category for each level of characteristics were conducted (data not shown). In the unadjusted regressions women were less likely to use statins only in some subgroups (e.g. White race, older age group, no limitations in ADLs, absence of depression), whereas for many subgroups the association between statin use and gender was not significant (e.g. African American race, elderly in the age group 70–74 years, presence of depression).
Table 2 displays the adjusted odds ratios (AORs) and 95 % confidence intervals from separate logistic regressions on statin use among women and men. The table also presents the AORs for women from a logistic regression on the pooled sample, which combined women and men. As seen from the table, after controlling for individual-level variables, women were 21 % less likely to report any use of statins than men. Among women and men, Latino race/ethnicity, lack of prescription drug coverage and greater functional disability were negatively associated with statin use. African American race and low educational status were negatively associated with statin use in men alone. There was a higher likelihood of statin use among both women and men who had fair health status, those who were overweight or obese, and among men who were smokers in the past (but not current smokers). Of these findings, the most striking were African American men (AOR: 0.61; 95 % CI 0.43, 0.86); no prescription drug coverage for women (AOR: 0.68; 95 % CI 0.55, 0.83) and men (AOR: 0.77; 95 % CI 0.64, 0.93); and overweight women (AOR: 1.39; 95 % CI 1.18, 1.65) and men (AOR: 1.29; 95 % CI 1.07, 1.56).
The results from the post-regression non-linear decomposition analysis are summarized in Table 3. Based on pooled weights, of the 8.3 percentage point gender difference in statin use, 2.44 percentage points was explained by individual-level variables. Thus, less than one third (29.5 %) of the gender difference in statin use was explained by the individual-level variables included in our models. More than two thirds (70.5 %) of the gender difference in statin use remained unexplained. Based on the regression weights for women, the individual-level variables included in the current study explained only 1.66 percentage points and nearly 75 % of the overall gender difference in statin use remained unexplained by variables included in the model. Using the regression weights for men, the total explained portion increased to 3.66 percentage points and approximately 56 % of the total gender difference in statin use remained unexplained.
4 Discussion
The current study examined the magnitude of gender difference in statin use and the extent to which the gender difference in statin use can be explained by a comprehensive list of individual-level variables. Using data from pooled regressions, results from this study indicated that approximately 30 % of the gender difference in statin use was associated with gender differences in demographic, economic, prescription drug coverage, health status, functional status, depression and lifestyle risk factors. As discussed below, among all individual-level factors, lifestyle risk factors, such as BMI and smoking, explained the highest proportion of the gender difference in statin use.
More than two thirds of the gender difference in statin use among elderly Medicare beneficiaries remained unexplained. Some of the unexplained gender difference in statin use could be due to patient-, provider- and system-level factors that were not evaluated in this study. Findings from different published studies can be pieced together to speculate plausible reasons for gender differences in statin use. These include gender differences in CVD treatment due to risk perception by providers and individuals, access to specialist care and discontinuation of statin use. Underestimation of CVD risk by providers and patients alike can lead to gender differences in statin use. It has been observed that women were unaware of their CVD risk factors and underestimated their CVD risk [39]; only 13 % of women in the US considered CVD risk to be serious [40] and this may lead to lower rates of statin use by women. Even when actual estimated CVD risk was similar among women and men, preventive therapy recommendation by physicians was less frequent for women than for men, mainly due to a lower perceived CVD risk for women by the physicians [41]. Access to specialist care may also compound this problem. For example, women with CAD or congestive heart failure were less likely to have a cardiologist consultation than men [42]. Such differences in specialist care may also produce gender differences in statin use, because specialists are more likely to prescribe statins than generalists [43]. Even when women use statins, they may be more likely than men to discontinue statins [44]. This may result in lower rates of statin use among women when measured with cross-sectional designs. Based on the results from this study and other published studies, it can be concluded that personalized risks and benefits may account for some of the unexplained gender differences in statin use. To further understand the gender difference in statin use, future research should be directed towards incorporating additional factors such as patient preferences, provider practice patterns and organizational-level factors that may contribute to gender differences and were not measured in this study.
Results from the current study also revealed that when pooled and men’s regression weights were used, lifestyle risk factors, such as BMI and smoking, explained the highest proportion of the gender difference in statin use. Utilizing the pooled weights, nearly 55 % of the differences in statin use among women and men were explained by the differential lifestyle risk profile of women and men. Among both women and men those who were overweight and obese were more likely to be on statins than elderly individuals with underweight/normal weight. Among men, those who reported to be former smokers were more likely to be statin users than those who never smoked. An examination of the differences in the lifestyle risk factors among women and men suggested that women were less likely to be overweight than men and women were more likely to be in the normal/underweight category than men. Similarly, a higher percentage of men than women reported to be former smokers. Thus, if the lifestyle risk profiles of women were the same as men, the gender difference in statin use would be reduced from 8.3 to 7.0 percentage points, based on pooled weights.
The findings on the increased likelihood of statin use among former smokers among men and among both men and women who are overweight or obese could possibly be explained by the additional beneficial effects of statins among these groups. Specifically, a previous study found evidence of greater benefits from statin use among longtime and recent quitters than among current smokers and never-smokers [45]. Similarly, obesity is a major risk factor for CAD, and therefore it is likely that physicians may consider prescribing statins in individuals who are obese [46].
Results from this study also indicated that statin use was less likely among African American men; however, a relationship between African American women and statin use was not found. African American men were 44 % less likely to use statins than White men after controlling for different individual-level variables. This finding is inconsistent with prior research that reported lower rates of statin use among both African American women and men. A review of 311 studies on pharmacotherapeutic disparities by race/ethnicity and gender reported that receipt of prescription drugs was the most frequently found difference. This review summarized 25 articles on gender disparities in CVD. According to this study, both African American women and men were less likely to receive lipid-lowering drugs [47]. Reasons for the lack of gender differences in statin use among African Americans is not known. Further research is warranted.
The strengths and limitations of this study need to be considered when interpreting findings. This large-sample study was based on nationally representative data on Medicare beneficiaries. The linked Medicare claims and survey data gave us the ability to include a comprehensive list of variables including perceived health status, functional status, obesity and smoking which are generally not available in claims data. However, there were some limitations as well. Prescription drug use and other data were based on self-reports and may be subject to recall bias. However, the special MCBS field procedures, such as interviewing respondents at relatively short intervals and verification of information, including explanation of benefits forms, might help to reduce problems with recall bias. Clinical risk factors such as LDL-C levels and non-clinical factors such as provider perceptions in prescribing statins and patient preferences in using statins that may have explained gender differences were not available. As with any other cross-sectional study, this study also can point only to association but cannot establish the cause–effect relationship between statin use and individual-level variables.
5 Conclusions
Despite these limitations, the current study estimated the magnitude of gender differences in statin use among elderly who are at risk for cardiovascular complications (i.e. those with diabetes, hyperlipidaemia or heart disease). The unique contribution of this study lies in examining the extent to which individual-level variables explained gender differences in statin use. Findings from this study confirmed the existence of gender difference in statin use, and nearly 30 % of the gender difference in statin use was explained by differences in individual-level characteristics. Further research needs to focus on patient preferences, provider practices and organizational-level factors that may explain some of the gender differences in statin use.
References
Braga MB, Langer A, Leiter LA. Recommendations for management of dyslipidemia in high cardiovascular risk patients. Exp Clin Cardiol. 2008 Summer;13(2):71–4.
Walsh JM, Pignone M. Drug treatment of hyperlipidemia in women. JAMA. 2004;291(18):2243–52.
LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA. 1999;282(24):2340–6.
Mills EJ, Rachlis B, Wu P, et al. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. J Am Coll Cardiol. 2008;52(22):1769–81.
Miettinen TA, Pyorala K, Olsson AG, Musliner TA, Cook TJ, Faergeman O, et al. Cholesterol-lowering therapy in women and elderly patients with myocardial infarction or angina pectoris: findings from the Scandinavian Simvastatin Survival Study (4S). Circulation. 1997;96(12):4211–8.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360(9326):7–22.
Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, PROSPER study group. PROspective Study of Pravastatin in the Elderly at Risk, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623–30.
Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, Coordinating Committee of the National Cholesterol Education Program, et al. A summary of implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Arterioscler Thromb Vasc Biol. 2004;24(8):1329–30.
LaRosa JC. Outcomes of lipid-lowering treatment in postmenopausal women. Drugs Aging. 2002;19(8):595–604.
Stagnitti MN. Statin use among persons 18 and older in the U.S. civilian noninstitutionalized population reported as receiving medical care for the treatment of high cholesterol, 2002. MEPS Statistical Brief #95. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st95/stat95.pdf. Accessed 27 Jul 2011.
Pambianco G, Lombardero M, Bittner V, et al. Control of lipids at baseline in the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial. Prev Cardiol. 2009 Winter; 12(1):9–18.
Franks P, Tancredi D, Winters P, et al. Cholesterol treatment with statins: who is left out and who makes it to goal? BMC Health Serv Res. 2010;10(1):68.
Segars LW, Lea AR. Assessing prescriptions for statins in ambulatory diabetic patients in the United States: a national, cross-sectional study. Clin Ther. 2008;30(11):2159–66.
Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42(9):1208–15.
Cooke CE, Hammerash WJ Jr. Retrospective review of sex differences in the management of dyslipidemia in coronary heart disease: an analysis of patient data from a Maryland-based health maintenance organization. Clin Ther. 2006;28(4):591–9.
Akhter N, Milford-Beland S, Roe MT, Piana RN, Kao J, Shroff A. Gender differences among patients with acute coronary syndromes undergoing percutaneous coronary intervention in the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). Am Heart J. 2009;157(1):141–8.
Enriquez JR, Pratap P, Zbilut JP, Calvin JE, Volgman AS. Women tolerate drug therapy for coronary artery disease as well as men do, but are treated less frequently with aspirin, beta-blockers, or statins. Gend Med. 2008;5(1):53–61.
Cho L, Hoogwerf B, Huang J, Brennan DM, Hazen SL. Gender differences in utilization of effective cardiovascular secondary prevention: a Cleveland clinic prevention database study. J Womens Health (Larchmt). 2008;17(4):515–21.
Setoguchi S, Glynn RJ, Avorn J, et al. Ten-year trends of cardiovascular drug use after myocardial infarction among community-dwelling persons ≥65 years of age. Am J Cardiol. 2007;100(7):1061–7.
Robinson JG, Booth B. Statin use and lipid levels in older adults: National Health and Nutrition Examination Survey, 2001 to 2006. J Clin Lipidol. 2010;4(6):483–90.
Vimalananda VG, Miller DR, Palnati M, et al. Gender disparities in lipid-lowering therapy among veterans with diabetes. Womens Health Issues. 2011;21(4 Suppl):S176–81.
Lloyd-Jones D, Adams R, Carnethon M, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009 Jan 27;119(3):e21–181. Epub 2008 Dec 15. Erratum in: Circulation. 2010;122(1):e11.
Kung HC, Hoyert DL, Xu J, et al. Deaths: final data for 2005. Natl Vital Stat Rep. 2008;56(10):1–120.
Centers for Disease Control and Prevention (CDC). Health data interactive. Data sources. Medicare Current Beneficiary Survey (MCBS). http://www.cdc.gov/nchs/data_access/hdi/hdi_data_sources.htm. Accessed 20 Jul 2011.
Eppig FJ, Chulis GS. Matching MCBS (Medicare Current Beneficiary Survey) and Medicare data: the best of both worlds. Health Care Financ Rev. 1997 Spring;18(3):211–29.
Pollak VE, Lorch JA. Effect of electronic patient record use on mortality in end stage renal disease, a model chronic disease: retrospective analysis of 9 years of prospectively collected data. BMC Med Inform Decis Mak. 2007;7:38.
Perez A, Anzaldua M, McCormick J, Fisher-Hoch S. High frequency of chronic end-stage liver disease and hepatocellular carcinoma in a Hispanic population. J Gastroenterol Hepatol. 2004;19(3):289–95.
US Department of Health and Human Services. Prior HHS poverty guidelines and Federal Register references. http://aspe.hhs.gov/poverty/figures-fed-reg.shtml. Accessed 10 Aug 2011.
Sambamoorthi U, Akincigil A, Wei W, et al. National trends in out-of-pocket prescription drug spending among elderly medicare beneficiaries. Expert Rev Pharmacoecon Outcomes Res. 2005;5(3):297–315.
Crystal S, Sambamoorthi U, Walkup JT, Akincigil A. Diagnosis and treatment of depression in the elderly medicare population: predictors, disparities, and trends. J Am Geriatr Soc. 2003;51(12):1718–28.
Centers for Disease Control and Prevention (CDC). Healthy weight – it’s not a diet, it’s a lifestyle! About BMI for adults. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Accessed 14 Aug 2011.
Johnson RW, Sambamoorthi U, Crystal S. Gender differences in pension wealth: estimates using provider data. Gerontologist. 1999;39(3):320–33.
Sambamoorthi U, Olfson M, Walkup JT, et al. Diffusion of new generation antidepressant treatment among elderly diagnosed with depression. Med Care. 2003;41(1):180–94.
Tseng CL, Sambamoorthi U, Rajan M, et al. Are there gender differences in diabetes care among elderly Medicare enrolled veterans? J Gen Intern Med. 2006;21 Suppl 3:S47–53.
Fairlie RW. An extension of the Blinder–Oaxaca decomposition technique to logit and probit models. J Econ Soc Meas. 2005;30(4):305–16.
Fairlie RW. The absence of the African American owned business: an analysis of the dynamics of self-employment. J Labor Econ. 1999;17(1):80–108.
Oaxaca R. Male-female wage differentials in urban labor markets. Int Econ Rev. 1973;14(3):693–709.
Neumark D. Employers’ discriminatory behavior and the estimation of wage discrimination. J Hum Resour. 1988;23(3):279–95.
Oliver-Mcneil S, Artinian NT. Women’s perceptions of personal cardiovascular risk and their risk-reducing behaviors. Am J Crit Care. 2002;11(3):221–7.
Mosca L, Ferris A, Fabunmi R, American Heart Association. Tracking women’s awareness of heart disease: an American Heart Association national study. Circulation. 2004;109(5):573–9.
Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111(4):499–510.
Cook NL, Ayanian JZ, Orav EJ, Hicks LS. Differences in specialist consultations for cardiovascular disease by race, ethnicity, gender, insurance status, and site of primary care. Circulation. 2009;119(18):2463–70.
McAlister FA, Majumdar SR, Eurich DT, Johnson JA. The effect of specialist care within the first year on subsequent outcomes in 24,232 adults with new-onset diabetes mellitus: population-based cohort study. Qual Saf Health Care. 2007;16(1):6–11.
Ellis JJ, Erickson SR, Stevenson JG, Bernstein SJ, Stiles RA, Fendrick AM. Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19(6):638–45.
Keddissi JI, Younis WG, Chbeir EA, et al. The use of statins and lung function in current and former smokers. Chest. 2007;132(6):1764–71.
Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, American College of Cardiology; American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina), et al. ACC/AHA 2002 guideline update for the management of patients with chronic stable angina–summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina). J Am Coll Cardiol. 2003;41(1):159–68.
Hall-Lipsy EA, Chisholm-Burns MA. Pharmacotherapeutic disparities: racial, ethnic, and sex variations in medication treatment. Am J Health Syst Pharm. 2010;67(6):462–8.
Acknowledgments
Mr Bhattacharjee received research assistance and Dr Sambamoorthi was partially supported for infrastructure from the West Virginia Collaborative Health Outcomes Research of Therapies and Services (WV CoHORTS) Center (Morgantown, WV, USA). The authors would also like to thank Dr Joel Halverson for his inspiration and encouragement in conducting this study. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhattacharjee, S., Findley, P.A. & Sambamoorthi, U. Understanding Gender Differences in Statin Use among Elderly Medicare Beneficiaries. Drugs Aging 29, 971–980 (2012). https://doi.org/10.1007/s40266-012-0032-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-012-0032-1