Abstract
Insulin degludec/liraglutide (Xultophy®), a fixed-ratio combination of an ultra-long-acting insulin analogue and a glucagon-like protein-1 (GLP-1) receptor agonist, is available in the EU for the management of inadequately controlled type 2 diabetes. Once-daily subcutaneous insulin degludec/liraglutide as add-on therapy to oral antidiabetics was effective and generally well tolerated in adults with inadequately controlled type 2 diabetes in several well designed 26-week phase III trials. In insulin-naive patients, add-on insulin degludec/liraglutide provided significantly greater improvements in glycated haemoglobin (HbA1c) levels than add-on insulin degludec, liraglutide or placebo, or unchanged GLP-1 receptor agonists (i.e. liraglutide or exenatide). In the extension of one of these trials, the efficacy of add-on insulin degludec/liraglutide was maintained for a total of 52 weeks. In insulin-experienced patients, add-on insulin degludec/liraglutide was significantly more effective with regard to improvements in HbA1c levels than add-on insulin degludec (at equivalent doses) or ongoing insulin glargine therapy. Add-on insulin degludec/liraglutide was associated with a lower incidence of confirmed hypoglycaemia than add-on insulin degludec in insulin-naive patients or ongoing insulin glargine in insulin-experienced patients, and a lower initial rate of nausea than add-on liraglutide. Thus, once-daily subcutaneous insulin degludec/liraglutide is a useful add-on therapy option for adult patients with inadequately controlled type 2 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Fixed-ratio combination of an ultra-long-acting insulin analogue (insulin degludec) and a glucagon-like protein-1 (GLP-1) receptor agonist (liraglutide) |
As add-on therapy in insulin-naive patients, provides better glycaemic control than add-on insulin degludec, liraglutide or placebo, or unchanged GLP-1 receptor agonists |
In insulin-experienced patients, provides better glycaemic control than add-on insulin degludec or ongoing insulin glargine |
Associated with significantly favourable changes in bodyweight compared with add-on insulin degludec or ongoing insulin glargine |
Generally well tolerated, with a tolerability profile that is consistent with its individual components |
Lower risk of hypoglycaemia than with add-on insulin degludec in insulin-naive patients or ongoing insulin glargine in insulin-experienced patients |
1 Introduction
Type 2 diabetes is a chronic disease that is characterized by decreased insulin secretion, hyperglucagonaemia, elevated hepatic glucose output, and insulin resistance, which ultimately results in hyperglycaemia [1, 2]. As the disease progresses, treatment intensification is often required to achieve and maintain adequate glycaemic control [1, 3].
Basal insulin analogues (e.g. insulin degludec, insulin detemir and insulin glargine) are designed to provide continuous, stable insulin exposure, with minimal variability in glucose-lowering effect to reduce the risk of hypoglycaemia [3, 4]. Gut-derived incretin hormones, including glucagon-like protein-1 (GLP-1) and gastric inhibitor polypeptide, are released after a meal and act in glucose-dependent manner to stimulate insulin secretion and suppress glucagon production [5, 6]. GLP-1 receptor agonists (e.g. liraglutide and exenatide) improve glycaemic control by decreasing fasting plasma glucose (FPG) and postprandial glucose (PPG) levels, and are associated with a low risk of hypoglycaemia [7]. When used in combination, basal insulins and GLP-1 receptor agonists display complementary mechanisms of action with regard to improving glycaemic control, which may offset their individual limitations [8].
Insulin degludec/liraglutide (Xultophy®) is a fixed-ratio combination of an ultra-long-acting basal insulin analogue and a GLP-1 receptor agonist that is available for the treatment of adults with inadequately controlled type 2 diabetes in the EU [9]. This article reviews the pharmacological, therapeutic efficacy and tolerability data relevant to the use of subcutaneous once-daily insulin degludec/liraglutide as add-on therapy in these patients. Where required, results were converted to SI units using established conversion factors.
2 Pharmacodynamic Properties of Insulin Degludec/Liraglutide
Insulin degludec and liraglutide have complementary mechanisms of action, which, when combined as fixed-ratio insulin degludec/liraglutide, provide sustained lowering of FPG levels and PPG levels after all meals, thereby improving glycaemic control [9]. This stable glucose-lowering profile allows for once-daily administration of insulin degludec/liraglutide without regard for food [9].
Insulin degludec is an ultra-long-acting basal insulin analogue that binds to insulin receptors on muscle and fat cells, acting as a full agonist to facilitate glucose uptake and inhibit hepatic glucose output [9, 10]. Liraglutide is an analogue of human GLP-1 that binds to and activates G protein-coupled GLP-1 receptors on the surface of pancreatic β-cells [9, 11]. When blood glucose levels are high, liraglutide causes dose-dependent insulin release and simultaneously lowers inappropriately elevated glucagon secretion [9, 11]. As blood glucose levels decrease, liraglutide reduces insulin secretion and no longer inhibits glucagon release [9]. As well as further lowering blood glucose through a slight delay in gastric emptying, liraglutide acts to reduce hunger and lower energy intake, thereby decreasing bodyweight and body fat mass [9, 11].
In a substudy of the DUAL-I trial (Sect. 4.1.1), 260 insulin-naive patients with inadequately controlled type 2 diabetes (despite metformin ± pioglitazone treatment) underwent a 4-h standardized meal test at baseline and 26 weeks [12]. After 26 weeks’ treatment, insulin secretion during the meal test was significantly (p = 0.048) higher in the insulin degludec/liraglutide than the insulin degludec group (33.8 vs. 25.7 pmol/mmol); however, the difference in insulin secretion between the insulin degludec/liraglutide and liraglutide groups was not significant. Postprandial glucagon levels with add-on insulin degludec/liraglutide were significantly (p = 0.003) lower than with add-on liraglutide [estimated between-group difference (BGD) −1.54 pmol/L], but were not significantly different to those observed with add-on insulin degludec [12].
In the DUAL-I trial, add-on insulin degludec/liraglutide for 26 weeks resulted in reductions in mean systolic blood pressure (BP) of 1.8 mmHg from baseline in insulin-naive patients, compared with 0.7 mmHg for add-on insulin degludec and 2.7 mmHg for add-on liraglutide [9]. In the DUAL-II trial in insulin-experienced patients with inadequately controlled type 2 diabetes (Sect. 4.2.1), reductions in mean systolic BP were significantly (p = 0.0028) greater with add-on insulin degludec/liraglutide (5.4 mmHg) than add-on insulin degludec (1.7 mmHg) [9]. At week 26 in DUAL-I, there was a significantly (p < 0.0001) greater mean increase in pulse rates from baseline with add-on insulin degludec/liraglutide than add-on insulin degludec (estimated BGD 3.2 beats/min), although there was no significant difference between the insulin degludec/liraglutide and liraglutide groups (estimated BGD −0.2 beats/min) [13].
Pharmacodynamic interaction studies with insulin degludec/liraglutide have not been carried out; however, there are a number of medications that influence glucose metabolism which may require dosage adjustment of the fixed-ratio combination [9].
3 Pharmacokinetic Properties of Insulin Degludec/Liraglutide
Insulin degludec/liraglutide has a pharmacokinetic profile that is consistent with once-daily dosing, with steady-state concentrations of insulin degludec and liraglutide being reached after 2–3 days of administration [9]. The bioequivalence of insulin degludec/liraglutide and its individually administered components was established in a single-dose study in healthy volunteers [14]. In a population pharmacokinetic analysis of data from the DUAL-I trial in type 2 diabetic patients (Sect. 4.1.1) [n = 1549], there were no clinically relevant changes in dose proportionality for the individual components of insulin degludec/liraglutide, and the effects of covariates (e.g. bodyweight) on exposure were consistent with previous data for insulin degludec and liraglutide [14].
After subcutaneous injection, insulin degludec forms a depot of soluble multihexamers in the subcutaneous tissue, from which insulin degludec monomers are slowly and continuously absorbed into the circulation [9, 10]. Similarly, liraglutide self-associates after subcutaneous administration into a heptameric structure that delays its absorption and prevents enzymatic degradation by neutral endopeptidase and dipeptidyl peptidase-4 (DPP-4) [9, 11]. After subcutaneous injection, liraglutide has an absolute bioavailability of ≈55 % and an apparent volume of distribution of 11–17 L [15]. Following intravenous administration, liraglutide has a mean volume of distribution of 0.07 L/kg [15]. Both insulin degludec and liraglutide are highly bound (>98 %) to plasma proteins [9].
Insulin degludec is metabolized in a similar fashion to human insulin, with all metabolites being inactive [9]. It has an elimination half-life (t½) of ≈25 h, which is independent of dose and determined by the rate of absorption from subcutaneous tissue [16]. The metabolism of liraglutide is similar to that of large proteins, with no specific organ identified as the major elimination route [9]. In the 24 h after administration of radiolabelled liraglutide in healthy volunteers, the major plasma component was unchanged drug, with two minor metabolites being detected (≤5 and ≤9 % of total plasma radioactivity exposure) [9]. The parent drug was not detected in the urine or faeces; however, during the 6–8 days after dosing, a small proportion of the radiolabelled dose was excreted in the urine (6 %) and faeces (5 %) that corresponded to three minor liraglutide metabolites [15]. The mean clearance of liraglutide after a single subcutaneous dose is ≈1.2 L/h, and the plasma t½ is ≈13 h [15], which is prolonged compared with that of endogenous GLP-1 (1.5–2 min) [11].
In population pharmacokinetic analyses, age, gender and ethnicity had no clinically relevant effect on the pharmacokinetics of insulin degludec/liraglutide [9]. Studies with the fixed-ratio combination in paediatric patients have not been performed [9]. Although the pharmacokinetics of insulin degludec are not significantly affected by renal or hepatic impairment [10], liraglutide exposure was reduced in patients with renal or hepatic impairment compared with healthy individuals [9]. Insulin degludec/liraglutide is not recommended in patients with moderate or severe renal impairment, including those with end-stage renal disease, and clinical experience in patients with hepatic impairment is currently too limited to recommend its use in these patients [9].
Drug interaction studies with insulin degludec/liraglutide have not been performed; however, in vitro studies indicate a low potential for pharmacokinetic drug interactions related to cytochrome P450 or plasma protein binding for both insulin degludec and liraglutide [9]. Although liraglutide is associated with a minor delay in gastric emptying which may affect the absorption of concomitantly administered oral medications, studies have demonstrated no clinically relevant delays in absorption of these drugs. A clinically relevant interaction between insulin degludec/liraglutide and warfarin or other coumarin derivatives cannot be excluded, and more frequent monitoring of the international normalized ratio is recommended after initiation of insulin degludec/liraglutide in patients receiving these agents [9].
4 Therapeutic Efficacy of Insulin Degludec/Liraglutide
The therapeutic efficacy of once-daily subcutaneous insulin degludec/liraglutide as add-on therapy to oral antidiabetic drugs (OADs) in adult patients (aged ≥18 years) with type 2 diabetes was established in five 26-week, randomized, multinational, treat-to-target, phase III trials (DUAL-I [13], -II [17], -III [18], -IV [19] and -V [20]), as well as a 26-week extension of the DUAL-I trial [21]. Data from the DUAL-III, -IV and -V trials are from abstract presentations.
The trials were conducted in insulin-naive (DUAL-I [13], -III [18] and -IV [19]; Sect. 4.1) and -experienced (DUAL-II [17] and -V [20]; Sect. 4.2) patients. Patients had glycated haemoglobin (HbA1c) levels of 7–10 [13, 20], 7.5–10 [17] or 7–9 % [18, 19], a body mass index (BMI) of ≤40 kg/m2 [13, 22–24] or ≥27 kg/m2 [17], and had been receiving previous antidiabetic treatment for ≥90 days before study entry [13, 17, 22–24]. Where specified, patients in each trial had a mean age of 55–60 years and a mean disease duration of 7–11 years [13, 17–19]. In all trials, the primary endpoint was the change from baseline in HbA1c levels after 26 weeks of therapy [13, 17–19, 24]. Where specified, efficacy analyses were based on data from the full analysis set [13, 17–19].
4.1 Insulin-Naive Patients
4.1.1 Compared with Add-on Insulin Degludec or Liraglutide
In the open-label DUAL-I trial in patients with inadequately controlled diabetes, once-daily insulin degludec/liraglutide, insulin degludec or liraglutide was added to background therapy with metformin (±pioglitazone) [13].
After 26 weeks’ treatment, add-on insulin degludec/liraglutide produced a significantly greater reduction in mean HbA1c levels from baseline than add-on insulin degludec or liraglutide (Table 1), reaching mean HbA1c levels of 6.4 % with add-on insulin degludec/liraglutide vs. 6.9 and 7.0 % with add-on insulin degludec and add-on liraglutide [13]. The criteria for noninferiority to add-on insulin degludec [upper 95 % confidence interval (CI) margin of 0.3 %] and superiority to add-on liraglutide (lower 95 % CI margin of 0 %) for this endpoint were met. Given the treat-to-target design of this study, glycaemic control was expected to be similar with add-on insulin degludec/liraglutide and add-on insulin degludec, and superiority analysis for this comparison was considered to be inappropriate. As the dosage of add-on insulin degludec/liraglutide was capped at 50 dose steps and add-on insulin degludec had no upper dosage limit, noninferiority of insulin degludec/liraglutide to insulin degludec was tested [13].
At week 26, a significantly greater proportion of patients in the insulin degludec/liraglutide group achieved HbA1c targets of <7.0 and ≤6.5 % than in the insulin degludec or liraglutide groups (Table 1), with 81 and 70 % of add-on insulin degludec/liraglutide recipients achieving these HbA1c targets vs. 65 and 47 % of add-on insulin degludec and 60 and 41 % of add-on liraglutide recipients [13].
There were significantly greater decreases in mean FPG levels from baseline to week 26 with add-on insulin degludec/liraglutide than add-on liraglutide, while the BGD between the fixed-ratio combination and insulin degludec groups was not significant (Table 1) [13]. Based on the nine-point self-monitored blood glucose (SMBG) profile at week 26, the reduction in the overall mean plasma glucose level was significantly (p ≤ 0.01) greater with add-on insulin degludec/liraglutide than either add-on insulin degludec or liraglutide. The reduction in mean plasma 90 min-PPG increment after all main meals was significantly (p < 0.0001) greater with add-on insulin degludec/liraglutide than add-on insulin degludec (estimated BGD −0.45 mmol/L); however, the difference in reductions in mean plasma 90 min-PPG increment between the fixed-ratio combination and liraglutide groups was not significant [13].
At week 26, changes in mean bodyweight from baseline significantly favoured add-on insulin degludec/liraglutide over add-on insulin degludec (BGD −2.22 kg); however, there were significantly lower reductions in mean bodyweight from baseline with add-on insulin degludec/liraglutide than with add-on liraglutide (BGD 2.44 kg) (Table 1) [13].
The proportion of patients who achieved each of the six composite endpoints of an HbA1c target of <7.0 or ≤6.5 % without experiencing bodyweight gain and/or hypoglycaemia was significantly (p < 0.0001) higher with add-on insulin degludec/liraglutide than add-on insulin degludec [13]. For example, the most stringent composite endpoint of an HbA1c target of ≤6.5 % without bodyweight gain or hypoglycaemia was achieved by 32 % of patients in the insulin degludec/liraglutide group compared with 9 % of patients in the insulin degludec group (p < 0.0001) [13].
Significantly (p < 0.0001) more patients in the insulin degludec/liraglutide than the liraglutide group achieved HbA1c levels of ≤6.5 % without hypoglycaemia (52 vs. 40 %) [13]. Conversely, significantly (p ≤ 0.01) more patients in the liraglutide than the insulin degludec/liraglutide group achieved HbA1c levels of <7.0 % without bodyweight gain (54 vs. 46 %) and without bodyweight gain or hypoglycaemia (52 vs. 36 %). No significant difference was observed between the insulin degludec/liraglutide and liraglutide groups in the rates of the other three composite endpoints [13].
At week 26, the mean daily insulin dose was 28 % lower in patients receiving add-on insulin degludec/liraglutide than add-on insulin degludec (38 vs. 53 U; p < 0.0001), and the mean daily liraglutide dose was 1.4 and 1.8 mg in the insulin degludec/liraglutide and liraglutide groups [13].
In the 26-week DUAL-I extension, the efficacy of add-on insulin degludec/liraglutide was maintained over 52 weeks’ treatment [21]. Add-on insulin degludec/liraglutide recipients had significantly greater reductions in mean HbA1c levels from baseline to week 52 than those receiving add-on insulin degludec or liraglutide, and the proportion of patients who achieved HbA1c levels of <7.0 and ≤6.5 % at study end was significantly higher in the insulin degludec/liraglutide group than the other treatment groups (Table 1). At week 52, the proportion of patients in each group who achieved the six composite endpoints of an HbA1c target of <7.0 or ≤6.5 % without bodyweight gain and/or hypoglycaemia were generally similar to those observed after 26 weeks’ treatment [21].
Add-on insulin degludec/liraglutide was associated with twofold greater reductions in mean FPG levels from baseline at week 52 compared with add-on liraglutide, although there was no significant difference in mean FPG reductions between add-on insulin degludec/liraglutide and add-on insulin degludec recipients (Table 1) [21]. The overall mean nine-point SBGM profiles were reduced in all treatment groups after 52 weeks’ treatment, and remained significantly (p < 0.01) lower with add-on insulin degludec/liraglutide than add-on insulin degludec or liraglutide. Add-on insulin degludec/liraglutide was associated with significantly greater reductions in mean bodyweight than add-on insulin degludec after 52 weeks’ treatment; however, patients receiving add-on liraglutide had significantly greater reductions in mean bodyweight than those receiving the fixed-ratio combination as add-on therapy (Table 1). In patients receiving add-on insulin degludec/liraglutide, the mean daily dose of insulin degludec at week 52 was 37 % lower than in those receiving add-on insulin degludec (39 vs. 62 U; p < 0.0001), and the mean daily liraglutide dose remained 22 % lower than those receiving add-on liraglutide (1.4 vs. 1.8 mg) [21].
In post hoc analyses at week 52, significantly (p < 0.01) greater reductions in HbA1c levels were observed with add-on insulin degludec/liraglutide than add-on insulin degludec or liraglutide across all baseline HbA1c categories (≤7.5, >7.5 to ≤8.5, >8.5 to ≤9.0 and >9.0 %) (abstract presentation) [25]. For example, among patients in the baseline HbA1c >9.0 % category, add-on insulin degludec/liraglutide recipients achieved a mean HbA1c level of 7.0 % at week 52 compared with mean HbA1c levels of 7.6 and 7.7 % for add-on insulin degludec and add-on liraglutide recipients. These reductions in HbA1c levels were independent of disease duration [25] and baseline BMI (abstract presentation) [26]. Significantly (p < 0.01) more patients in the insulin degludec/liraglutide group achieved targets for HbA1c (< 7.0 %) and FPG (≤7.2 mmol/L) at earlier timepoints (weeks 8 and 12 for HbA1c and weeks 4, 8 and 12 for FPG) than patients in the insulin degludec or liraglutide groups (abstract presentation) [27]. Add-on insulin degludec/liraglutide was associated with significantly (p < 0.0001) greater reductions in least-squares mean HbA1c from baseline than add-on insulin degludec at weeks 4, 8 and 12, and add-on liraglutide at weeks 8 and 12. Mean bodyweight reductions from baseline were also significantly (p < 0.0001) greater with add-on insulin degludec/liraglutide than add-on insulin degludec as early as 4 weeks after starting therapy; however, bodyweight reductions were significantly (p < 0.0001) greater with add-on liraglutide than add-on insulin degludec/liraglutide [27]. Patients in the insulin degludec/liraglutide group were more likely (p < 0.01) to achieve target pre-meal and 90 min-PPG levels (≥3.9 to ≤7.2 and <9 mmol/L, respectively) for all meals than patients in the insulin degludec or liraglutide groups (abstract presentation) [28]. In a 72-h continuous glucose monitoring substudy (n = 260), the mean interstitial glucose (IG) profile with add-on insulin degludec/liraglutide was significantly (p < 0.0001) lower than add-on liraglutide, but not significantly different from that of add-on insulin degludec (abstract presentation) [29]. Conversely, IG fluctuations and 90 min-PPG increments across all meals with add-on insulin degludec/liraglutide were significantly (p < 0.05) lower than add-on insulin degludec, but not significantly different from those of add-on liraglutide. The day-to-day IG variability remained low and not significantly different across all treatment groups [29].
4.1.2 Compared with Unchanged GLP-1 Receptor Agonists
In the open-label DUAL-III trial, patients with inadequately controlled diabetes on maximum dose GLP-1 receptor agonists (i.e. once-daily liraglutide or twice-daily exenatide) were switched to add-on insulin degludec/liraglutide once daily or continued unchanged GLP-1 receptor agonists in addition to background therapy with metformin (±pioglitazone ± sulfonylurea) [18].
After 26 weeks’ treatment, add-on insulin degludec/liraglutide provided significantly greater mean reductions in HbA1c from baseline than unchanged GLP-1 receptor agonists (Table 1) [18]. Add-on insulin degludec/liraglutide had superior efficacy to unchanged GLP-1 receptor agonists, with an HbA1c estimated treatment difference (ETD) at week 26 of −0.94 % (95 % CI −1.11 to −0.78) [18]. A significantly greater proportion of add-on insulin degludec/liraglutide recipients achieved HbA1c targets of <7.0 and ≤6.5 % at week 26 than unchanged GLP-1 receptor agonist recipients (Table 1), with both HbA1c targets being achieved by more than twice as many add-on insulin degludec/liraglutide vs. unchanged GLP-1 receptor agonist recipients [18].
At week 26, there were significantly greater reductions in mean FPG levels from baseline with add-on insulin degludec/liraglutide than unchanged GLP-1 receptor agonist therapy (Table 1) [18]. Mean nine-point SMBG profiles were also significantly (p < 0.001) lower with add-on insulin degludec/liraglutide than unchanged GLP-1 receptor agonists after 26 weeks’ treatment. However, add-on insulin degludec/liraglutide was associated with significantly greater increases in mean bodyweight from baseline at week 26 than unchanged GLP-1 receptor agonist therapy (Table 1). At week 26, the mean dose of insulin degludec/liraglutide was 43 dose steps (i.e. insulin degludec/liraglutide 43 U/1.55 mg) [18].
At week 26, patient-reported outcomes were generally improved to a greater extent in the insulin degludec/liraglutide than GLP-1 receptor agonist group, as assessed using the Treatment-Related Impact Measure-Diabetes (TRIM-D) questionnaire and the Diabetes Treatment Satisfaction Questionnaire status (DTSQs) (abstract presentation) [30]. At week 26, TRIM-D total and subdomain (i.e. treatment burden, daily life, diabetes management, compliance and psychological health) scores showed significantly (p < 0.05) greater improvements with add-on insulin degludec than unchanged GLP-1 receptor agonists. In add-on insulin degludec/liraglutide recipients, the change in total TRIM-D score from baseline (8.7 vs. 3.1 points with unchanged GLP-1 receptor agonists) was greater than the minimally important difference of 7.8 points. Total DTSQs scores also had significantly (p < 0.001) greater increases from baseline to week 26 with add-on insulin degludec/liraglutide than unchanged GLP-1 receptor agonists. Based on DTSQ findings, the perceived frequency of hyperglycaemia was significantly (p < 0.001) lower with add-on insulin degludec/liraglutide than unchanged GLP-1 receptor agonists, although the perceived frequency of hypoglycaemia was significantly (p = 0.006) higher with add-on insulin degludec/liraglutide [30].
4.1.3 Compared with Add-on Placebo
In the double-blind DUAL-IV trial in patients with inadequately controlled diabetes, once-daily insulin degludec/liraglutide or placebo was added to background therapy with a sulfonylurea (±metformin) [19].
At week 26, add-on insulin degludec/liraglutide was significantly more effective than add-on placebo with regard to decreases in mean HbA1c and FPG levels from baseline and the proportion of patients achieving HbA1c targets of <7.0 and ≤6.5 % (Table 1) [19]. Patients receiving add-on insulin degludec/liraglutide were significantly (p < 0.001) more likely to achieve HbA1c targets of <7.0 and ≤6.5 % than those receiving add-on placebo, with estimated odds ratios of 11.95 and 16.36 for the respective HbA1c targets. Add-on insulin degludec/liraglutide was also associated with significantly greater mean reductions in nine-point SBGM profiles than add-on placebo at week 26, and a post hoc analysis revealed significantly lower blood glucose levels at all measured timepoints (p value not reported). However, there were significantly greater reductions in mean bodyweight from baseline to week 26 in the placebo vs. the insulin degludec/liraglutide group (Table 1). After 26 weeks’ treatment, the mean dose of insulin degludec/liraglutide was 28 dose steps (i.e. insulin degludec/liraglutide 28 U/1 mg) [19].
4.2 Insulin-Experienced Patients
4.2.1 Compared with Add-on Insulin Degludec
The DUAL-II trial was a double-blind study in patients with inadequately controlled diabetes receiving basal insulin plus metformin with or without sulfonylureas or glinides [17]. Patients discontinued all OADs except for metformin and were switched from basal insulin to once-daily add-on insulin degludec/liraglutide or insulin degludec. As this study was designed to evaluate the contribution of liraglutide to the fixed-ratio combination of insulin degludec/liraglutide, the maximum insulin dose for both groups was 50 units [17].
The addition of insulin degludec/liraglutide to ongoing metformin therapy provided superior efficacy to add-on insulin degludec with regard to improvements in HbA1c levels at 26 weeks (Table 1) [17]. The criteria for superiority were met (i.e. 95 % CI for ETD being entirely below 0 %), with an ETD of −1.1 % (95 % CI −1.3 to −0.8; p < 0.0001). Of note, the mean daily insulin degludec dose at this timepoint was identical in both groups (45 U), thereby permitting a valid assessment of the contribution of liraglutide to the fixed-ratio combination. At week 26, there were also significantly greater reductions in mean FPG levels and bodyweight from baseline in the insulin degludec/liraglutide than the insulin degludec group, and more patients in the fixed-ratio combination than the insulin degludec group achieved HbA1c targets of <7.0 and ≤6.5 % (Table 1) [17].
Significantly (p < 0.0001) more patients in the insulin degludec/liraglutide than the insulin degludec group achieved each of the six composite endpoints (i.e. achieving an HbA1c target of <7.0 or ≤6.5 % without experiencing bodyweight gain and/or hypoglycaemia) [17]. For example, the composite endpoint of a target HbA1c level of ≤6.5 % without bodyweight gain or hypoglycaemia was achieved by 30 % of patients in the insulin degludec/liraglutide group compared with 5 % of patients in the insulin degludec group (p < 0.0001) [17].
According to nine-point SMBG profiles at week 26, add-on insulin degludec/liraglutide was associated with significantly (p < 0.05) lower glucose levels than add-on insulin degludec at all timepoints, with an estimated BGD in mean glucose levels of −1.1 mmol/L (p < 0.0001) [17]. Furthermore, the mean prandial increment across meals was significantly (p = 0.026) lower in the insulin degludec/liraglutide than the insulin degludec group (estimated BGD −0.4 mmol/L) [17].
In post hoc analyses, add-on insulin degludec/liraglutide had consistent efficacy with regard to improving glycaemic control irrespective of baseline disease status, with baseline HbA1c category, disease duration and insulin dose (≤30 or >30 U) having no effect on the reduction in HbA1c level with add-on insulin degludec/liraglutide [25]. Addition of the fixed-ratio combination also effectively reduced HbA1c levels independent of baseline BMI [26]. Significantly (p < 0.02) more patients in the insulin degludec/liraglutide group reached HbA1c (<7.0 %) and FPG (≤7.2 mmol/L) targets (at weeks 8 and 12 for HbA1c and weeks 4, 8 and 12 for FPG), and had significantly (p < 0.0001) greater reductions in HbA1c levels and bodyweight from week 4 onwards than those in the insulin degludec group [27]. Pre-meal and 90 min-PPG levels were also more likely (p < 0.01) to be in their respective target ranges with add-on insulin degludec/liraglutide than add-on insulin degludec [28].
4.2.2 Compared with Continuation of Insulin Glargine Regimen
In the open-label DUAL-V trial, patients with inadequately controlled diabetes on insulin glargine were switched to add-on insulin degludec/liraglutide once daily or continued insulin glargine therapy in addition to background therapy with metformin [20].
Add-on insulin degludec/liraglutide was significantly more effective than ongoing insulin glargine therapy with regard to improvements in HbA1c levels at 26 weeks (Table 1), with an ETD of −0.59 % (95 % CI −0.74 to −0.45) [20]. However, reductions in mean FPG levels from baseline at 26 weeks were not significantly different between the insulin degludec/liraglutide and insulin glargine groups (Table 1) [20].
After 26 weeks’ treatment, a significantly greater proportion of add-on insulin degludec/liraglutide than ongoing insulin glargine recipients achieved the HbA1c target of <7.0 % (Table 1), with significantly (p < 0.001) greater proportions of patients in the insulin degludec/liraglutide than in the insulin glargine group achieving the two composite endpoints of an HbA1c target of <7.0 % without hypoglycaemia (54 vs. 29 %) or an HbA1c target of <7.0 % without hypoglycaemia and bodyweight gain (39 vs. 12 %) [20]. Furthermore, add-on insulin degludec/liraglutide was associated with significantly greater reductions in mean bodyweight from baseline at 26 weeks than ongoing insulin glargine (Table 1), and was insulin-sparing, with a significantly (p < 0.001) lower mean daily insulin dose (41 vs. 66 U with insulin glargine) at 26 weeks [20].
5 Tolerability of Insulin Degludec/Liraglutide
Once-daily insulin degludec/liraglutide as add-on therapy to OADs for 26–52 weeks was generally well tolerated in the phase III trials discussed in Sect. 4. The adverse event profile of add-on insulin degludec/liraglutide was mostly consistent with those of add-on insulin degludec or add-on liraglutide in the 26-week DUAL-I and -II trials [13, 17]. In these trials, ≤2 % of patients in both the insulin degludec/liraglutide and insulin degludec groups [13, 17] and 5.8 % of patients in the liraglutide group [13] discontinued treatment because of an adverse event. In the 26-week DUAL-III, -IV and -V trials, the tolerability profile of add-on insulin degludec/liraglutide was generally consistent with the findings of the DUAL-I and -II trials [18–20].
In DUAL-I and -II, at least one treatment-emergent adverse event (TEAE) occurred in 58–63 % of patients receiving add-on insulin degludec/liraglutide or insulin degludec [13, 17] and 73 % of patients receiving add-on liraglutide [13]. In DUAL-III, TEAEs were reported in 66 and 63 % of add-on insulin degludec/liraglutide and unchanged GLP-1 receptor agonist recipients [18]. In DUAL-IV, the overall rates of TEAEs for add-on insulin degludec/liraglutide and placebo were 401.4 and 367.0 events per 100 patient-years of exposure (PYE) [19]. Where reported [13, 18], most TEAEs were considered unlikely to be related to treatment.
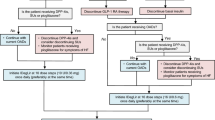
The majority of TEAEs in DUAL-I and -II were of mild or moderate severity, with the most frequently occurring events being headache, nasopharyngitis, gastrointestinal (GI) events and elevated lipase levels (Fig. 1) [13, 17]. In DUAL-IV, the most common TEAEs with add-on insulin degludec/liraglutide were elevated lipase levels (10 vs. 4 % with add-on placebo), nasopharyngitis (9 vs. 8 %), dyslipidaemia (7 vs. 4 %), headache (5 vs. 6 %) and influenza (3 vs. 6 %) [19]. GI events (i.e. nausea, diarrhoea, vomiting and decreased appetite) occurred with a numerically lower frequency with add-on insulin degludec/liraglutide than add-on liraglutide in insulin-naive patients in DUAL-I (Fig. 1a) and its 26-week extension [21], with the highest prevalence of nausea with add-on liraglutide being in the first 10 weeks of treatment [13]. Where reported [17], none of the GI events led to study discontinuation. In a post hoc analysis of DUAL-II and -IV, the odds of experiencing GI adverse effects did not significantly differ between add-on insulin degludec/liraglutide and add-on insulin degludec or placebo (abstract presentation) [31].
Treatment-emergent adverse events occurring with a ≥5 % incidence with add-on insulin degludec/liraglutide, insulin degludec or liraglutide in a insulin-naive [13] and b insulin-experienced [17] adult patients with inadequately controlled type 2 diabetes. Elevated lipase levels defined as >3 × the upper limit of normal. IDeg insulin degludec, LIR liraglutide
In insulin-naive patients in DUAL-I, the rate of confirmed hypoglycaemia was significantly (p = 0.0023) lower in the insulin degludec/liraglutide than insulin degludec group (1.8 vs. 2.6 events/PYE), and a post hoc analysis indicated that the risk of hypoglycaemia was lower for the fixed-ratio combination than insulin degludec irrespective of the end-of-study HbA1c level [13]. Conversely, the rate of hypoglycaemia was significantly (p < 0.0001) higher with add-on insulin degludec/liraglutide than add-on liraglutide (1.8 vs. 0.2 events/PYE) in this trial. Of the five reported episodes of severe hypoglycaemia in DUAL-I, three occurred in the insulin degludec/liraglutide group and two occurred in the insulin degludec group; nocturnal hypoglycaemia occurred in 6, 8 and 1 % of patients in the insulin degludec/liraglutide, insulin degludec and liraglutide groups, respectively [13]. In the DUAL-I extension, the rate of confirmed hypoglycaemia was 37 % lower with add-on insulin degludec/liraglutide than add-on insulin degludec (p < 0.0001), but was significantly (p < 0.0001) higher with add-on insulin degludec/liraglutide than add-on liraglutide [21]. The rate of confirmed hypoglycaemia was also significantly (p < 0.001) higher with add-on insulin degludec/liraglutide than unchanged GLP-1 receptor agonists in DUAL-III (2.82 vs. 0.12 events/PYE) [18] or add-on placebo in DUAL-IV (3.5 vs. 1.4 events/PYE) [19].
In insulin-experienced patients in DUAL-V, the rates of confirmed hypoglycaemia (2.23 vs. 5.05 events/PYE) and nocturnal hypoglycaemia (0.22 vs. 1.23 events/PYE) were significantly (p < 0.001) lower with add-on insulin degludec/liraglutide than ongoing insulin glargine therapy [20]. However, in the insulin degludec/liraglutide and insulin degludec groups in DUAL-II, the rates of confirmed hypoglycaemia (1.5 vs. 2.6 events/PYE) and nocturnal hypoglycaemia (0.22 vs. 0.32 events/PYE) were not significantly different; severe hypoglycaemia occurred in one patient in the insulin degludec/liraglutide group [17].
Where reported [13, 17, 18], the incidence of serious TEAEs in the insulin degludec/liraglutide group was numerically similar to the active comparator groups in insulin-naive (2 vs. 2–3 % with add-on insulin degludec or liraglutide in DUAL-I [13] or unchanged GLP-1 receptor agonists in DUAL-III [18]) and -experienced (4 vs. 6 % with add-on insulin degludec in DUAL-II [17]) patients.
In insulin-naive patients in DUAL-I, three of the 18 cardiovascular events were classified as major; one cardiovascular-related death in the insulin degludec/liraglutide group and one myocardial infarction in the insulin degludec group were both considered unlikely to be treatment-related, while a myocardial infarction in the liraglutide group was considered to be possibly related to treatment [13]. There were two confirmed major cardiovascular events with add-on insulin degludec/liraglutide in DUAL-III (both stroke) [18] and -IV (myocardial infarction and stroke) [19]. In insulin-experienced patients in DUAL-II, three major cardiovascular events were confirmed; one myocardial infarction in the insulin degludec/liraglutide group and a myocardial infarction and a stroke in the insulin degludec group [17].
There were three confirmed neoplasm events in DUAL-III (two with add-on insulin degludec/liraglutide and one with unchanged GLP-1 receptor agonists [18]) and -IV (one with add-on insulin degludec/liraglutide and two events in one add-on placebo recipient [19]). In DUAL-I, four neoplasm events were reported (two with add-on insulin degludec/liraglutide, one with add-on insulin degludec and one with add-on liraglutide) [13]; however, there were no reports of medullary thyroid carcinoma and no confirmed cases of thyroid neoplasm in DUAL-I or -II [13, 17].
At week 26 in insulin-naive patients in DUAL-I, small increases in mean plasma levels of lipase (by 11–15 U/L) were observed with add-on insulin degludec/liraglutide and add-on liraglutide, and mean plasma amylase levels were also slightly elevated in all groups (by 4–9 U/L) [13]. Although most of the 178 episodes of elevated lipase or amylase levels were asymptomatic, 17 episodes were associated with symptoms and suspected as being related to pancreatitis. Across all groups in this trial, there were 18 episodes of suspected or confirmed pancreatitis in 16 patients; acute pancreatitis was confirmed by external adjudication in one patient in the liraglutide group and considered unlikely to be treatment-related [13]. Although elevated plasma lipase levels occurred with numerically higher incidence with add-on insulin degludec/liraglutide than add-on placebo in insulin-naive patients in DUAL-IV (10 vs. 4 %) [19], in insulin-experienced patients in DUAL-II, elevated lipase levels [i.e. >3 × the upper limit of normal (ULN)] occurred in ≤6 % of patients from either treatment group (Fig. 1b) [17]. In DUAL-II, one of these patients from the insulin degludec/liraglutide group also presented with abdominal pain and nausea; however, this event was considered by external adjudication to be unrelated to pancreatitis [17]. In DUAL-II, elevated mean plasma amylase levels (i.e. >3 × ULN) occurred in five patients in the insulin degludec/liraglutide group and two patients in the insulin degludec group, none of whom had symptoms of pancreatitis [17]. There were no confirmed cases of pancreatitis or thyroid-related adverse events in DUAL-II [17], -III [18] or -IV [19].
6 Dosage and Administration of Insulin Degludec/Liraglutide
In the EU [9], the fixed-ratio combination of insulin degludec/liraglutide is indicated for the treatment of adults with type 2 diabetes to improve glycaemic control in combination with OADs when these, alone or in combination with a GLP-1 receptor agonist or basal insulin, do not provide adequate glycaemic control. Insulin degludec/liraglutide is subcutaneously administered once daily at any time (preferably at the same time) of the day by injection in the thigh, upper arm or the abdomen. Injection site rotation within the same region is recommended to reduce the risk of lipodystrophy [9].
Insulin degludec/liraglutide is administered in dose steps, where one dose step contains insulin degludec 1 U and liraglutide 0.036 mg [9]. Individualized dosage adjustment based on FPG levels is recommended for optimization of glycaemic control, with the maximum daily dose being 50 dose steps (i.e. insulin degludec/liraglutide 50 U/1.8 mg). In patients not transferring from a GLP-1 receptor agonist or basal insulin, the recommended starting dosage is ten dose steps (i.e. insulin degludec/liraglutide 10 U/0.36 mg) once daily. Insulin degludec/liraglutide can be added to existing OAD therapy; however, a dosage reduction for concomitantly administered sulfonylureas should be considered. In patients transferring from a GLP-1 receptor agonist or basal insulin, the recommended starting dosage is 16 dose steps (i.e. insulin degludec/liraglutide 16 U/0.6 mg) once daily; this starting dosage should not be exceeded. When transferring from a long-acting GLP-1 receptor agonist (i.e. with once-weekly administration), insulin degludec/liraglutide should be initiated at the same time as the next scheduled dose of long-acting GLP-1 receptor agonist. During and following transfer from a GLP-1 receptor agonist or basal insulin, close glucose monitoring is recommended [9].
Local prescribing information should be consulted for detailed information regarding the use of insulin degludec/liraglutide in special patient populations, warnings and precautions, contraindications and potential drug interactions.
7 Place of Insulin Degludec/Liraglutide in Type 2 Diabetes Management
Type 2 diabetes disease management aims to avoid acute hyperglycaemia and glycaemic instability over time, and prevent/delay the onset of diabetic complications, while maintaining patient health-related quality of life [4]. A target HbA1c level of <7.0 % is recommended for most patients; however, individualization of glycaemic targets and antidiabetic treatment is advised. In patients with inadequate glycaemic control after ≈3 months of lifestyle modifications and first-line therapy with metformin, treatment intensification with sequential addition of other antidiabetics (i.e. a sulfonylurea, thiazolidinedione, DPP-4 inhibitor or a GLP-1 receptor agonist) or basal insulin is recommended [4]. Insulin has the highest efficacy with regard to reducing HbA1c levels [4]; however, in clinical practice, attaining glycaemic targets with insulin is frequently limited by the associated risk of hypoglycaemia and bodyweight gain [2]. GLP-1 receptor agonists are injectable agents that target the incretin system and are widely used as second- or third-line treatment [2, 4]. Although GLP-1 receptor agonists are associated with a reduction in bodyweight and a low risk of hypoglycaemia, their use can be limited by GI adverse events (e.g. nausea and vomiting), particularly in the early phases of treatment [4].
The combination of a basal insulin with a GLP-1 receptor agonist, through their complementary mechanisms of action, may provide patients with improved glycaemic control and fewer limiting side effects than either agent individually [5–7]. When these two agents are used in combination, the GLP-1 receptor agonist appears to reduce insulin-induced hypoglycaemia and bodyweight gain, and improves glycaemic control by minimising PPG variability [2, 6]. Combining a GLP-receptor agonist with basal insulin may additionally allow for an insulin dosage reduction, which could also mitigate insulin-induced hypoglycaemia and bodyweight gain [2]. Furthermore, as GLP-1 receptor agonists do not generally require frequent glucose self-monitoring or ongoing dosage adjustment, combination therapy with a basal insulin may simplify disease management, thereby potentially improving patient adherence compared with intensified insulin therapy and delaying the need to initiate basal plus bolus insulin [7].
Insulin degludec/liraglutide is a fixed-ratio combination that is available as add-on therapy for adults with inadequately controlled type 2 diabetes in the EU [9]. In phase III trials in insulin-naive patients, addition of once-daily subcutaneous insulin degludec/liraglutide for 26 weeks provided significantly greater reductions in mean HbA1c levels from baseline than add-on insulin degludec or liraglutide (DUAL-I; Sect. 4.1.1), unchanged add-on GLP-1 receptor agonists (DUAL-III; Sect. 4.1.2) or add-on placebo (DUAL-IV; Sect. 4.1.3). The glycaemic efficacy of add-on insulin degludec/liraglutide was maintained in the 26-week DUAL-I extension (i.e. 52 weeks’ treatment; Sect. 4.1.1). In insulin-experienced patients, add-on insulin degludec/liraglutide was significantly more effective than add-on insulin degludec (DUAL-II; Sect. 4.2.1) or ongoing insulin glargine (DUAL-V; Sect. 4.2.2) with regard to improvements in HbA1c levels at 26 weeks.
Significantly more patients achieved the end-of-study HbA1c target of <7.0 % with add-on insulin degludec/liraglutide than add-on insulin degludec, add-on liraglutide, unchanged GLP-1 receptor agonists, ongoing insulin glargine or add-on placebo, and the HbA1c target of ≤6.5 % was achieved by significantly greater proportions of add-on insulin degludec/liraglutide recipients than add-on insulin degludec, add-on liraglutide, unchanged GLP-1 receptor agonists or add-on placebo recipients (Table 1). Across trials, the end-of-study HbA1c targets of <7.0 and ≤6.5 % were achieved in 60–81 and 45–70 % of patients receiving add-on insulin degludec/liraglutide (Table 1).
At week 26 in the DUAL-I, -II and -V trials, add-on insulin degludec/liraglutide was associated with significantly favourable changes in mean bodyweight from baseline compared with add-on insulin degludec or ongoing insulin glargine, although significantly greater bodyweight reductions were observed with add-on liraglutide, unchanged GLP-1 receptor agonists or add-on placebo than add-on insulin degludec/liraglutide in DUAL-I, -III and -IV (Table 1). Treatment with add-on insulin degludec/liraglutide was also insulin sparing, requiring significantly lower mean daily insulin doses than add-on insulin degludec in DUAL-I and its 26-week extension (Sect. 4.1.1) and ongoing insulin glargine in DUAL-V (Sect. 4.2.2).
Once-daily subcutaneous insulin degludec/liraglutide in combination with background OADs was generally well tolerated over 26–52 weeks in insulin-naive and -experienced patients, with a tolerability profile that was mostly consistent with those of its individual components (Sect. 5). In insulin-naive patients in DUAL-I and its 26-week extension, the rate of confirmed hypoglycaemia was significantly lower with add-on insulin degludec/liraglutide than add-on insulin degludec (Sect. 5); this was attributed to the lower mean daily insulin dose required with the fixed-ratio combination [13]. However, add-on insulin degludec/liraglutide was associated with a significantly higher rate of confirmed hypoglycaemia than add-on liraglutide, unchanged GLP-1 receptor agonists or add-on placebo (Sect. 5). In insulin-experienced patients, the rate of confirmed hypoglycaemia with add-on insulin degludec/liraglutide was significantly lower than with ongoing insulin glargine in DUAL-V, although it did not significantly differ to add-on insulin degludec in DUAL-II (Sect. 5), where patients in both groups received equivalent daily insulin doses (Sect. 4.2.1).
In insulin-naive patients in DUAL-I, add-on insulin degludec/liraglutide was associated with a numerically lower incidence of nausea than add-on liraglutide, particularly in the first 10 weeks’ treatment (Sect. 5). This was attributed to the lower starting dosage of insulin degludec/liraglutide and more gradual dose increase during the titration phase, combined with a numerically lower mean liraglutide dose in the insulin degludec/liraglutide vs. the liraglutide group near the end of this trial [13]. In insulin-experienced patients in DUAL-II, GI events occurred with a numerically higher frequency in the insulin degludec/liraglutide than the insulin degludec group; however, the overall incidence of each type of event across both groups was ≤6.5 % over 26 weeks [17].
In the absence of head-to-head trials, the relative position of add-on insulin degludec/liraglutide in the management of type 2 diabetes remains to be fully determined. A recent meta-analysis of randomized trials in adults with type 2 diabetes indicated that GLP-1 receptor agonist plus basal insulin combination add-on therapy generally provided improved glycaemic control and bodyweight reductions compared with other antidiabetic treatments, and mitigated the risk of hypoglycaemia associated with basal insulin therapy [2]. Studies comparing insulin degludec/liraglutide with other GLP-1 receptor agonist plus basal insulin combinations (e.g. insulin glargine/lixisenatide) or once-weekly GLP-1 receptor agonists (e.g. exenatide, abligutide and dulaglutide) would be of interest.
Given that insulin degludec/liraglutide has only recently been approved in the EU, no robust pharmacoeconomic analyses for this fixed-ratio combination have been published. As cost is an important factor that determines the choice of antidiabetic therapy in many patients [4], specific cost-effectiveness analyses for the use of insulin degludec/liraglutide in type 2 diabetes would be of interest.
In conclusion, add-on therapy with once-daily subcutaneous insulin degludec/liraglutide is an effective and generally well tolerated emerging option for adult patients with inadequately controlled type 2 diabetes, providing the benefits of improved glycaemic control and bodyweight loss, while decreasing the risk of hypoglycaemia associated with insulin therapy.
Data selection sources:
Relevant medical literature (including published and unpublished data) on insulin degludec/liraglutide was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated 21 July 2015], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Degludec, decludec, NN 1250, Tresiba, liraglutide, Victoza, IDegLira, NN 9068, Xultophy.
Study selection: Studies in patients with type 2 diabetes who received insulin degludec/liraglutide. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Ross SA. Breaking down patient and physician barriers to optimize glycemic control in type 2 diabetes. Am J Med. 2013;126(9 Suppl 1):S38–48.
Eng C, Kramer CK, Zinman B, et al. Glucagon-like peptide-1 receptor agonist and basal insulin combination treatment for the management of type 2 diabetes: a systematic review and meta-analysis. Lancet. 2014;384(9961):2228–34.
Sorli C. New developments in insulin therapy for type 2 diabetes. Am J Med. 2014;127(10 Suppl):S39–48.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35(6):1364–79.
Carris NW, Taylor JR, Gums JG. Combining a GLP-1 receptor agonist and basal insulin: study evidence and practical considerations. Drugs. 2014;74(18):2141–52.
Ahrén B. Insulin plus incretin: a glucose-lowering strategy for type 2-diabetes. World J Diabetes. 2014;5(1):40–51.
Goldenberg R. Insulin plus incretin agent combination therapy in type 2 diabetes: a systematic review. Curr Med Res Opin. 2013;30(3):431–45.
Kumar A. Insulin degludec/liraglutide: innovation-driven combination for advancement in diabetes therapy. Expert Opin Biol Ther. 2014;14(6):869–78.
Novo Nordisk A/S. Xultophy 100 units/mL + 3.6 mg/mL solution for injection: EU summary of product characteristics. 2014. http://www.ema.europa.eu. Accessed 21 Jul 2015.
Keating GM. Insulin degludec and insulin degludec/insulin aspart: a review of their use in the management of diabetes mellitus. Drugs. 2013;73(6):575–93.
Scott LJ. Liraglutide: a review of its use in adult patients with type 2 diabetes mellitus. Drugs. 2014;74(18):2161–74.
Vora J, Linjawi S, Gough SC, et al. Improved postprandial glycaemic control in Type 2 diabetes with a combination of insulin degludec and liraglutide: results from a meal test [abstract no. P113]. Diabet Med. 2014;31(Suppl 1):61.
Gough SC, Bode B, Woo V, et al. Efficacy and safety of a fixed-ratio combination of insulin degludec and liraglutide (IDegLira) compared with its components given alone: results of a phase 3, open-label, randomised, 26-week, treat-to-target trial in insulin-naive patients with type 2 diabetes. Lancet Diabetes Endocrinol. 2014;2(11):885–93.
Kapitza C, Bode B, Ingwersen SH, et al. Preserved pharmacokinetic exposure and distinct glycemic effects of insulin degludec and liraglutide in IDegLira, a fixed-ratio combination therapy. J Clin Pharmacol. 2015. doi:10.1002/jcph.549.
Novo Nordisk A/S. Victoza 6 mg/ml solution for injection in pre-filled pen: EU summary of product characteristics. 2014. http://www.ema.europa.eu. Accessed 21 Jul 2015.
Novo Nordisk A/S. Tresiba 100 units/mL solution for injection in pre-filled pen: EU summary of product characteristics. 2014. http://www.ema.europa.eu. Accessed 21 Jul 2015.
Buse JB, Vilsboll T, Thurman J, et al. Contribution of liraglutide in the fixed-ratio combination of insulin degludec and liraglutide (IDegLira). Diabetes Care. 2014;37(11):2926–33.
Linjawi S, Bode B, Chaykin LB, et al. Efficacy and safety of IDegLira (combination of insulin degludec + liraglutide), in insulin-naive patients with T2D uncontrolled on GLP-1 receptor agonist (GLP-1RA) therapy [abstract no. 1002-P plus poster]. In: American Diabetes Association 75th Scientific Sessions. 2015.
Rodbard HW, Bode B, Harris SB, et al. IDegLira in insulin-naive patients with type 2 diabetes (T2D) inadequately controlled on sulfonylureas (SU) alone or in combination with metformin: the DUAL IV study [abstract no. 1003-P plus poster]. In: American Diabetes Association 75th Scientific Sessions. 2015.
Buse J, Pérez Manghi FC, García-Hernández PA, et al. Insulin degludec/liraglutide (IDegLira) is superior to insulin glargine (IG) in A1c reduction, risk of hypoglycemia, and weight change: DUAL V study [abstract no. 166-OR]. In: American Diabetes Association 75th Scientific Sessions. 2015.
Gough SC, Bode B, Woo VC, et al. One-year efficacy and safety of a fixed combination of insulin degludec and liraglutide in patients with type 2 diabetes: results of a 26-week extension to a 26-week main trial. Diabetes Obes Metab. 2015. doi:10.1111/dom.12498.
US National Institutes of Health. ClinicalTrials.gov identifier NCT01676116. 2012. http://www.clinicaltrials.gov. Accessed 21 Jul 2015.
US National Institutes of Health. ClinicalTrials.gov identifier NCT01952145. 2013. http://www.clinicaltrials.gov. Accessed 21 Jul 2015.
US National Institutes of Health. ClinicalTrials.gov identifier NCT01618162. 2012. http://www.clinicaltrials.gov. Accessed 21 Jul 2015.
Rodbard HW, Buse JB, Woo VC, et al. Novel combination of insulin degludec and liraglutide (IDegLira) is efficacious across the range of disease progression in type 2 diabetes [abstract no. 835]. Diabetologia. 2014;57(Suppl 1):S338–9.
Buse JB, Rodbard HW, Woo VC, et al. Impact of BMI on HbA1c reduction, hypoglycemia rates, and insulin requirements in response to IDegLira in patients with type 2 diabetes (T2D) [abstract no. 66-OR]. Diabetes. 2014;63(Suppl 1):A18.
Vilsboll T, Vora J, Jarlov H, et al. IDegLira, a combination of insulin degludec and liraglutide, enables patients with type 2 diabetes to reach target glycaemic control faster than its individual components alone [abstract no. 836 plus poster]. Diabetologia. 2014;57(Suppl 1):S339.
King A, Philis-Tsimikas A, Langbakke IH, et al. IDegLira, a combination of insulin degludec and liraglutide, improves both pre- and postprandial plasma glucose in patients with type 2 diabetes [abstract no. 243]. Diabetologia. 2014;57(Suppl 1):S108–9.
King AB, Philis-Tsimikas A, Kilpatrick ES, et al. Assessment of glycemic control by CGM in patients with T2D treated with IDegLira [abstract no. 170-OR]. In: American Diabetes Association 75th Scientific Sessions. 2015.
Linjawi S, Brod M, Bode B, et al. In insulin-naive patient with T2DM uncontrolled on GLP-1 receptor agonists (GLP-1RA), IDegLira (novel combination of insulin degludec + liraglutide) resulted in improved patient-reported outcomes vs. unchanged GLP-1RA [abstract no. 1150-P plus poster]. In: American Diabetes Association 75th Scientific Sessions. 2015.
Aroda VR, Jaeckel E, Jarlov H, et al. Incidence of gastrointestinal side effects similar between IDegLira and non-GLP-1RA comparators [abstract no. 1009-P plus poster]. In: American Diabetes Association 75th Scientific Sessions. 2015.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the authors on the basis of scientific and editorial merit. Sarah Greig and Lesley Scott are salaried employees of Adis/Springer.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: S. Linjawi, Coffs Endocrine and Diabetes Services, Coffs Harbour, NSW, Australia; J. E. Thurman, SSM Medical Group—Endocrinology, St. Louis, MO, USA; V. C. Woo, Section of Endocrinology and Metabolism, University of Manitoba, Winnipeg, Manitoba, Canada.
Rights and permissions
About this article
Cite this article
Greig, S.L., Scott, L.J. Insulin Degludec/Liraglutide: A Review in Type 2 Diabetes. Drugs 75, 1523–1534 (2015). https://doi.org/10.1007/s40265-015-0448-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-015-0448-0