Abstract
Acamprosate (Campral®, Aotal®, Regtect®) is one of a limited number of pharmacological treatment options approved as an adjunct to psychosocial interventions to facilitate the maintenance of abstinence in alcohol-dependent patients. It has been used in Europe, the USA and other countries for many years and was recently approved for this indication in Japan. In several randomized, double-blind, placebo-controlled trials (without active comparators), acamprosate in conjunction with psychosocial therapy for 3–12 months was generally significantly better than placebo plus psychosocial interventions in improving various key outcomes, including the proportion of patients who maintained complete abstinence from alcohol (complete abstinence rate), the mean cumulative abstinence duration, the percentage of alcohol-free days and the median time to first drink. Acamprosate as an adjunct to psychosocial interventions also demonstrated efficacy in some randomized, active-comparator trials of similar duration. Although results were not always consistent across individual trials, overall findings were generally favourable for acamprosate in a recent meta-analysis, which showed that alcohol-consumption outcomes were similarly improved with acamprosate or naltrexone. Acamprosate is generally well tolerated, has a low propensity for drug interactions and may be used without dosage adjustment in patients with mild to moderate hepatic impairment, although dosage adjustments or contraindications are recommended in patients with renal impairment. Thus, the use of acamprosate as an adjunct to psychosocial interventions in alcohol-dependent patients provides modest but potentially valuable improvements in alcohol-consumption outcomes and is generally well tolerated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Approved in numerous countries as an adjunct to psychosocial interventions for the maintenance of abstinence in alcohol dependence |
Mechanism of action may involve restoration of the imbalance between neuronal excitation and inhibition that occurs in chronic alcohol exposure by modulating glutamate and GABA neurotransmission |
Does not undergo hepatic metabolism and is eliminated unchanged in urine |
Improves various alcohol-consumption outcomes, as shown in several placebo-controlled and some active-comparator trials, although results not always positive |
Beneficial effects on alcohol-consumption outcomes similar to those of naltrexone in a recent large meta-analysis |
Generally well tolerated (diarrhoea is the most common adverse event) |
1 Introduction
Alcohol misuse includes the full spectrum from drinking above recommended limits to alcohol dependence [1]. It is responsible for ≈3.3 million deaths worldwide each year (5.9 % of all deaths) and is a causal factor in more than 60 major types of diseases and injuries, including cardiovascular disease, liver disease, mental health disorders, social problems, accidents, pancreatitis and various types of cancer [2, 3]. In particular, for persons 15–49 years of age, alcohol is the leading risk factor for death and disability worldwide [2]. Alcohol can also have harmful effects that reach deep into society, often adversely affecting the well-being and health of friends and family members of those who misuse it [2]. In the USA alone, the economic cost of alcohol misuse is estimated in the hundreds of billions of dollars annually, and it ranks among the top three preventable causes of morbidity and mortality [1, 3, 4].
Alcohol dependence develops after repeated alcohol use and is characterized by a strong desire to consume alcohol, difficulties in controlling its use, persisting in its use despite harmful consequences, increased tolerance to its effects, a greater priority given to alcohol consumption than to other activities and obligations, and the development of a physiological withdrawal state when alcohol use is decreased or discontinued [2, 5]. The lifetime prevalence rates of alcohol dependence in men and women in the USA have been estimated at ≈17 and 8 %, respectively [1]. Alcohol dependence is a chronic relapsing medical disorder that is treatable with psychosocial therapy and appropriate adjunctive pharmacotherapy [4–7]. In general, clinical outcomes are poor when drug therapy is not used to enhance the effects of psychosocial interventions, with up to 70 % of patients resuming alcohol consumption within 1 year [4].
Among the limited adjunctive pharmacological treatment options available for the maintenance of abstinence from alcohol in patients with alcohol dependence is acamprosate (Campral®, Aotal®, Regtect®), which has been available for many years in the EU, USA and other countries, and more recently was approved for this indication in Japan. This article provides an overview of the pharmacology of acamprosate and reviews its clinical efficacy and tolerability profile as an adjunct to psychosocial interventions in patients with alcohol dependence.
2 Overview of Pharmacological Properties
2.1 Pharmacodynamics
Acamprosate is a synthetic compound with a chemical structure related to that of taurine and γ-aminobutyric acid (GABA) [8, 9]. The mechanism of action of acamprosate in the maintenance of alcohol abstinence has not been fully elucidated, in part, because the complex neurobiology of alcohol dependence is also not completely understood [8, 10]. Nevertheless, a body of preclinical evidence suggests that acamprosate may interact with (excitatory) glutamate and (inhibitory) GABA neurotransmission to restore the imbalance between neuronal excitation and inhibition that occurs in chronic alcohol exposure [9, 10]. In particular, acamprosate may modulate glutamatergic transmission via effects on N-methyl-d-aspartic acid (NMDA) receptors and metabotropic glutamate receptor 5 (mGlu5) [10–16], and it may also have indirect modulatory effects on GABAA receptor transmission [10]. Acamprosate has been shown to attenuate hyperglutamatergic activity and reduce ethanol consumption in mice that were drinking excessive quantities of ethanol [17, 18], and it reduced glutamate levels (assessed by magnetic resonance spectroscopy) in the brains of alcohol-dependent patients who had been detoxified [19]. Also of interest is a recently reported series of experiments that challenges previous research in this area, suggesting that the pharmacodynamic activity of acamprosate may be related to the calcium salt of acamprosate, which is marketed as acamprosate calcium [20, 21].
Various studies in mice and rats have shown that acamprosate reduces alcohol consumption in rodents that have an extended history of alcohol exposure or are alcohol dependent [8, 15]. These preclinical findings have translated into reductions in alcohol intake in a large number of clinical trials in patients with alcohol dependence (Sect. 3).
Acamprosate suppressed alcohol-induced place preference in mice with alcohol physical dependence [22]. Animal studies have also shown that acamprosate reduces some of the adverse behavioural and neurochemical events associated with alcohol withdrawal, such as hyperactivity and anxiety-like behaviour, as well as attenuation of elevated glutamate levels during the early stages after withdrawal [8]. In a murine model used to evaluate the pharmacodynamic effects of antidepressant agents (tail suppression test), acamprosate produced an antidepressant-like effect that was dependent on NMDA and mGlu5 receptor blockade [23]. In addition, a randomized, double-blind, polysomnographic trial in alcohol-dependent patients showed that acamprosate improved sleep continuity and sleep architecture parameters typically disturbed in this population [24].
Acamprosate was not associated with the development of tolerance or dependence in animal studies, nor has it produced any withdrawal symptoms in patients receiving therapeutic doses in clinical trials [9]. There is also no evidence of acamprosate abuse or dependence from postmarketing studies [9].
2.2 Pharmacokinetics
The absolute bioavailability of acamprosate following oral administration is ≈11 % [9, 25]. Peak plasma concentrations (Cmax) at steady state are achieved between 3 and 8 h after administration of a 666 mg dose [9]. Mean Cmax was 350 ng/mL at steady state in subjects who had received acamprosate 666 mg three times daily for ≥5 days. When taken with food, Cmax is reduced by ≈42 % and area under the plasma concentration-time curve (AUC) is reduced by ≈23 %, but this decrease in acamprosate exposure is not considered clinically significant and no dosage adjustment is necessary [9] (see also Sect. 6).
The estimated volume of distribution of acamprosate following intravenous administration is 72–109 L (≈1 L/kg) and plasma protein binding is negligible [9].
Following oral administration and absorption of the drug into the systemic circulation, acamprosate does not undergo metabolism and is excreted unchanged in the urine as acamprosate [9, 25]. The terminal elimination half-life (t½) of acamprosate is ≈18–33 h [9, 25, 26].
The pharmacokinetic properties of acamprosate are similar between healthy subjects and alcohol-dependent patients [9]. Although the pharmacokinetics of acamprosate have not been evaluated in elderly patients (except in Japan), it is likely that plasma acamprosate concentrations would be higher than in younger adults because renal function diminishes in the elderly and acamprosate undergoes renal elimination. Following single-dose administration of acamprosate 666 mg, Cmax was increased by 2- and 4-fold in subjects with moderate or severe renal impairment, respectively, compared with healthy subjects. Corresponding increases in t½ were 1.8- and 2.6-fold. Dosage adjustments of acamprosate are recommended in patients with moderate renal impairment and the drug is not recommended for use in individuals with severe renal impairment (see Sect. 6). Dosage adjustments are not necessary in patients with mild to moderate hepatic impairment [9].
In healthy male Japanese subjects who received single doses of acamprosate 333–1998 mg in the fasting state, Cmax was achieved 4.4–6.8 h after administration and t½ values ranged from 14.9 to 20.4 h [27]. The pharmacokinetics were linear in that both Cmax and AUC increased proportionally with dose. Cmax and AUC were reduced by one-third and one-half, respectively, when a single dose of acamprosate 666 mg was administered with food compared with the fasting state. Following repeated administration of acamprosate 666 mg three times daily in healthy Japanese males, steady state was achieved within 2 days. Cmax and AUC values were 2- and 2.3-fold higher, respectively, in older (67–80 years of age) compared with younger (22–29 years of age) healthy Japanese subjects who received a single dose of acamprosate 666 mg in the fasting state [27].
Acamprosate has a low propensity for interactions with other drugs, including those likely to be administered as concomitant drugs in alcohol-dependent patients, including alcohol, diazepam, disulfiram or naltrexone [9, 25, 26]. In vitro studies indicate that acamprosate does not induce cytochrome P450 (CYP) 1A2 or 3A4 isoenzymes, nor does it inhibit the metabolism of drugs that are substrates for CYP1A2, 2C9, 2C19, 2D6, 2E1 or 3A4 [9].
3 Therapeutic Efficacy
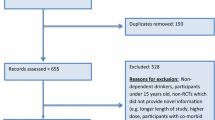
Acamprosate has been available in some markets (e.g. the EU) for more than two decades [8], and a large body of evidence supports its use as an adjunct to psychosocial interventions (e.g. cognitive behavioural therapy, motivational enhancement therapy, 12-step programmes, such as Alcoholics Anonymous [1]) in patients with alcohol dependence. For example, a recent systematic review and meta-analysis of pharmacotherapy for alcohol use disorders in outpatient settings included 22 placebo-controlled trials with acamprosate [28]. The current article is a narrative review, and this section focuses on larger (n ≥ 100), well-designed, fully published clinical trials of ≥12 weeks’ duration with acamprosate in the management of adults with alcohol dependence. These studies are divided into randomized placebo-controlled trials without active comparators (Sect. 3.1.1) and randomized trials comparing acamprosate with one or more active comparators (including combination regimens), which in some cases also included a placebo arm (Sect. 3.1.2). Findings from recent meta-analyses are presented in Sect. 3.1.3. A brief discussion of other potential uses of acamprosate (e.g. in the management of pathological gambling) is included in Sect. 3.2.
Although the main goal of therapy in the management of patients with alcohol dependence is complete abstinence, which was the primary endpoint of several studies discussed in Sect. 3.1, treatment may be beneficial even if complete abstinence is not achieved [1]. Therefore, a number of other outcome measures have been evaluated in the trials, such as the effects of acamprosate on the mean cumulative abstinence duration, the percentage of alcohol-free days and the median time to first drink, as well as its effects on complications of alcohol dependence, including sleep disorders and depression.
Across studies, acamprosate and other pharmacological interventions were used in conjunction with psychosocial interventions, usually starting after detoxification (or a brief but sustained period of abstinence). Alcohol consumption was self-reported, but in many studies was validated by breath alcohol concentration, γ-glutamyltransferase levels and/or collateral informant interviews. Several studies also included follow-up periods after drug treatment was discontinued to assess longer-term efficacy after a pre-defined drug treatment period. Primary efficacy analyses, where specified, were based on the intent-to-treat population, and the majority of study participants were men. Patients with serious co-existing diseases or concomitant psychiatric disorders were typically excluded from the studies. With respect to baseline patient characteristics, treatment groups were generally well matched.
3.1 Treatment of Alcohol Dependence
3.1.1 Placebo-Controlled Studies
In randomized, double-blind, placebo-controlled, multicentre trials (without active comparators), acamprosate 1332–1998 mg/day in conjunction with psychosocial therapy for 3–12 months was generally more effective than placebo for key outcomes, including the proportion of patients who remained completely abstinent, the mean cumulative abstinence duration and the median time to first drink, in patients with alcohol dependence (Table 1) [29–40]. However, results were not always consistent between trials. For example, for primary or co-primary endpoints in short- to medium-term trials of ≈3–6 months’ duration, acamprosate was not significantly different from placebo for the percentage of alcohol-free days in a large (n = 592) ≈6-month study [34] or in a smaller (n = 100) ≈3-month trial [29], nor was there a statistically significant treatment effect on complete abstinence rate in a large (n = 581) 6-month trial [30]. Of note is that the 6-month trial in 592 patients evaluated acamprosate 2 g/day and a higher exploratory dose of 3 g/day, and post hoc analysis controlling for baseline variables and treatment exposure showed that both regimens were statistically superior to placebo for percentage of alcohol-free days (58.2 and 62.7 vs. 52.3 %; p = 0.01 for linear dose effect) [34]. A separate post hoc analysis of this trial showed that acamprosate also had a beneficial effect on sleep disturbances (a common problem in alcoholism), which was mainly, although not entirely, related to the effect of the drug on abstinence [41]. Primary outcomes were significantly better with acamprosate than placebo in several other short- to medium-term studies, including the mean cumulative abstinence duration in a smaller (n = 188) 3-month trial [35] and in various larger (n = 262–330) 6-month studies [31, 32, 37], as well as complete abstinence rates in 3- and 6-month trials [35–37] and median time to first drink in a 6-month study [37]. In addition, in short- to medium-term studies where these outcomes were considered secondary endpoints, acamprosate was also statistically superior to placebo for mean cumulative abstinence duration in a 6-month study [36] and median time to first drink in 3- and 6-month trials [35, 36] (Table 1).
Also of interest are findings of a 6-month, randomized, double-blind, placebo-controlled trial with acamprosate 1998 mg/day conducted at 34 medical institutions in Japan [33]. The study was designed to accommodate usual clinical practices in Japan and included 327 patients with alcohol dependence. Patients were hospitalized for about 2 months for treatment of withdrawal symptoms and rehabilitation therapy, and were then randomized to acamprosate or placebo on the day of hospital discharge. For the primary endpoint of complete abstinence rate throughout the ≈6-month treatment period, acamprosate was statistically superior to placebo (47.2 vs. 36.0 %; p < 0.05). Mean cumulative abstinence duration and percentage of alcohol-free days were not significantly different between treatment groups (Table 1).
In longer-term placebo-controlled trials of ≈11–12 months’ duration (n = 272–538), the complete abstinence rate (a primary or co-primary endpoint in all three studies [38–40]) was significantly greater with acamprosate than placebo at the end of the study treatment period in two trials [39, 40]. In the third study, which randomized patients to placebo or two different dosage regimens of acamprosate, the complete abstinence rate was numerically greater with either acamprosate regimen than placebo after 12 months, and an interim analysis at 6 months showed both regimens were significantly better than placebo [38] (Table 1). One of the trials also showed a statistically significant advantage for acamprosate over placebo for a co-primary endpoint of mean cumulative abstinence duration (225 vs. 162 days; p < 0.001) and a numerical advantage for median time to first drink (131 vs. 45 days; p-value not reported), which was also a co-primary endpoint [39]. In addition, acamprosate was associated with statistically significant advantages over placebo for the mean cumulative abstinence duration in longer-term trials where this endpoint was considered a secondary outcome [38, 40].
Four of the short- to medium-term trials included a 3- to 6-month follow-up period during which active drug therapy was not administered [31, 33, 36, 37]. In one of these trials, patients who were randomized to acamprosate had a significantly higher rate of complete abstinence (43 vs. 30 %) and a significantly higher mean cumulative number of abstinence days (168 vs. 120) than placebo (both p ≤ 0.05) during the treatment plus follow-up period [36]. Similar results for the respective treatment groups were reported for complete abstinence rates (38 vs. 29 %; not statistically significant) and mean cumulative abstinence duration (155 vs. 127 days; p < 0.05) at the end of follow-up in another trial [37]. The third study included findings only for the complete abstinence rate at the end of follow-up, which was 11 % for acamprosate compared with 5 % for placebo, but the between-group difference was not statistically significant [31]. Similarly, the fourth (Japanese) trial included results only for the time to first relapse at the end of follow-up, and the between-group difference did not achieve statistical significance [33].
The longer-term studies included follow-up periods of 6–12 months’ duration during which active drug therapy was not administered [38–40]. Complete abstinence rates and mean cumulative abstinence duration through the treatment plus follow-up periods consistently favoured acamprosate over placebo, although not all between-group differences achieved statistical significance. One of the trials showed a significant advantage for acamprosate over placebo for complete abstinence rate (40 vs. 17 %; p < 0.01) and mean cumulative abstinence duration (387 vs. 251 days; p < 0.001) at the end of follow-up [39]. Both of the other trials also showed a statistically significant advantage for acamprosate (albeit only with the higher dosage in one study [38]) over placebo for mean cumulative abstinence duration at the end of follow-up [38, 40].
3.1.2 Active Comparator-Controlled and Combined Treatment Studies
Several randomized studies have compared the efficacy of acamprosate with that of active comparators and/or evaluated the efficacy of acamprosate in combination with other drug therapy in adults with alcohol dependence (Table 2) [42–48]. Most were also double-blind, placebo-controlled trials [42, 43, 45, 47, 48], although two studies used an open-label design, in part, because patients in one of the treatment arms received disulfiram, and patients’ awareness that they are taking disulfiram is an important factor in its effectiveness [44, 46]. All of the studies recruited patients from ≥2 centres, aside from one of the open-label trials, which was conducted at a single centre [44]. The studies were ≈3–12 months in duration and evaluated a range of primary or co-primary endpoints, although there was some overlap between trials.
In the largest trial (COMBINE), 1383 patients from 11 US sites were randomized to nine possible treatment groups, of which four included medication without a combined behavioural intervention (CBI), four included medication with CBI and one included only CBI (no pills) [42]. CBI involved intensive counseling delivered by alcoholism treatment specialists. The four medication groups (each with or without CBI) included acamprosate 3 g/day, naltrexone 100 mg/day, both drugs in combination or placebo. For the eight arms that included medication, patients also received medical management, a multi-session intervention delivered by a healthcare professional focusing on enhancing medication adherence and abstinence. Of note, dosages used in this trial were higher than those commonly prescribed or used in most other clinical trials in alcohol dependence. Treatment duration was for 16 weeks, although patients were also evaluated for up to 1 year after treatment. Co-primary endpoints were the percentage of alcohol-free days and the percentage of patients who relapsed to heavy drinking over the 16-week treatment period. The analysis allowed for estimations of the effects of each intervention as monotherapies, as well as comparisons of the effects of two or three combined therapies within a 2 × 2 × 2 factorial design (i.e. acamprosate/placebo × naltrexone/placebo × CBI/no CBI).
Results of the COMBINE study showed substantial reductions in drinking in all groups, including an overall 80 % reduction in alcohol consumption and a tripling of the percentage of alcohol-free days from baseline to the end of the 16-week study period among the eight pill-taking groups [42]. Co-primary outcomes for each treatment arm are presented in Table 2. Analysis of results showed that patients who received medical management with naltrexone, CBI or both had the best drinking outcomes, and no combination provided better efficacy than naltrexone or CBI alone in the presence of medical management. Acamprosate did not show a statistically significant advantage over placebo, either alone or with naltrexone, CBI or both. Interestingly, compared with patients who received CBI alone (no pills or medical management), those who received placebo plus medical management or placebo plus medical management and CBI had significantly higher percentage of alcohol-free days (66.6 vs. 73.8 and 79.8 %; p < 0.001). There were no statistically significant between-group differences at 1 year following treatment.
In contrast to the positive findings for naltrexone in COMBINE, a 12-week, randomized, double-blind trial (PREDICT) conducted in 426 alcohol-dependent patients in Germany showed no statistically significant difference between naltrexone, acamprosate or placebo for the primary outcome of heavy drinking relapse rate (Table 2) [47]. Although the three treatment arms of PREDICT were similar to the corresponding treatment arms of COMBINE, in that both studies included medical management to enhance compliance, the PREDICT investigators note that divergence in results may be attributed to differences in the study populations (e.g. history of heavier drinking in PREDICT) and treatment environments (all patients in PREDICT underwent inpatient medical detoxification treatment prior to randomization compared to a very small percentage of patients in COMBINE) [47].
A smaller (n = 169) randomized trial evaluating the efficacy of acamprosate, naltrexone and placebo for 12 weeks also found no statistically significant between-group differences for various drinking outcomes (Table 2) [48]. However, in a similar 12-week study in 160 patients, acamprosate, naltrexone and the combination of acamprosate plus naltrexone were all statistically superior to placebo for the primary outcome of heavy drinking relapse (Table 2) [45]. The combination of acamprosate plus naltrexone was also significantly more effective than acamprosate alone for preventing heavy drinking relapse.
Three studies involved the use of disulfiram, including the two previously mentioned open-label trials [44, 46], as well as a randomized, double-blind, placebo-controlled study of ≈1 year’s duration (Table 2) [43]. In the placebo-controlled trial (n = 110), patients randomized to acamprosate or placebo were stratified by concomitant voluntary disulfiram use. Approximately one-half of the patients in each group received disulfiram. At the end of the study period, acamprosate with or without disulfiram provided significantly better results than placebo with or without disulfiram for the main outcome of mean cumulative abstinence duration (137 vs. 75 days; p < 0.05) [i.e. 40 vs. 21 % alcohol-free days] [43]. In a 12-week open-label trial (n = 243), the mean time to first episode of heavy (46.6 vs. 17.6 and 22.0 days; p < 0.0001) or any (30.4 vs. 11.4 and 16.2 days; p < 0.001) drinking was significantly longer among patients treated with disulfiram than in those who received either acamprosate or naltrexone [46]. Results also favoured disulfiram over acamprosate in a smaller (n = 100) open-label trial of 8 months’ duration in which 54 % of acamprosate and 12 % of disulfiram recipients had a heavy drinking relapse (p = 0.0001) [44].
3.1.3 Meta-Analyses
Overall, results were generally favourable for acamprosate in a recent systematic review and meta-analysis of pharmacotherapy for alcohol use disorders in outpatient settings that included 22 placebo-controlled trials with acamprosate, 44 with naltrexone and 4 with disulfiram [28]. Both acamprosate and naltrexone 50 mg/day orally were associated with improvements in alcohol-consumption outcomes, whereas results were less robust or equivocal for naltrexone 100 mg/day orally and naltrexone injection. In general, evidence did not support efficacy for disulfiram, except possibly in patients with excellent adherence, although the number of disulfiram-treated patients included in the meta-analysis was relatively small. Not all trials evaluated the same parameters, but most included the outcome of return to any drinking. Also of note regarding the acamprosate trials for the endpoint of return to any drinking is that the I2 value for statistical heterogeneity (80.8 %, p < 0.001) indicates substantial, significant heterogeneity between the trials.
Regarding the findings for acamprosate (16 trials; n = 4847) and orally administered naltrexone 50 mg/day (16 trials; n = 2347), numbers needed to treat (NNTs) to prevent one person to returning to any drinking were 12 and 20, respectively [28]. This reflected a risk reduction of 9 % for acamprosate compared with placebo [risk difference (RD) −0.09; 95 % CI −0.14 to −0.04] and a corresponding risk reduction of 5 % for naltrexone 50 mg/day (RD −0.05; 95 % CI −0.10 to −0.002). Meta-analysis of four head-to-head studies comparing acamprosate with naltrexone (including COMBINE) found no statistically significant differences between the drugs for any of these outcomes. There was also insufficient direct evidence from clinical trials to determine whether acamprosate or other medications improved health outcomes, as very few trials reported on outcomes such as mortality, accidents or injuries, and health-related quality of life or function [28].
The statistical superiority of acamprosate compared with placebo was also shown in a Cochrane review of acamprosate for alcohol dependence published a few years earlier, which included 24 randomized controlled trials with 6915 participants [49]. Acamprosate had a relative risk of 0.86 (95 % CI 0.81–0.91) for return to any drinking, with a corresponding NNT of 9.09 (95 % CI 6.66–14.28).
Another meta-analysis of 64 randomized, placebo-controlled trials with acamprosate or naltrexone for treating alcohol use disorders found that acamprosate had a significantly larger effect size than naltrexone on the maintenance of abstinence, whereas naltrexone had a larger effect size than acamprosate on reducing heavy drinking and craving, although differences in effect size between acamprosate and naltrexone were small [50]. Findings from a longitudinal individual patient meta-analysis of 24 randomized trials that started with an inpatient detoxification period suggest that treatment with acamprosate should be continued for at least 6 months after alcohol withdrawal to achieve clinically relevant effects in this patient population (reported as an abstract) [51]. In another large meta-analysis, there were no statistically significant differences in any measure of acamprosate efficacy (or tolerability) between women and men [52].
Acamprosate reduced the severity of relapse, in particular the overall weekly consumption of alcohol, in an analysis of 15 placebo-controlled trials in which the aim of therapy was complete abstinence [53]. The analysis focused on data from 1010 patients who relapsed during the trials. Among patients who had at least one drink since the previous assessment, acamprosate was associated with significant (p < 0.001) reductions in quantity and frequency of alcohol consumption compared with placebo in each of four follow-up periods, and the between-group difference was greatest for the product of these variables (expressed as overall weekly consumption of alcohol).
To evaluate the efficacy of acamprosate in alcohol-dependent patients with depression, an individual patient data meta-analysis was conducted from 11 trials with a total of 3354 patients, of whom one-third (n = 1120) had concomitant depression [54]. Depressed patients were less compliant with treatment and less likely to achieve complete abstinence than non-depressed patients, although the effect of acamprosate on increasing abstinence relative to placebo was similar in depressed and non-depressed patients. Patients who were depressed at baseline and remained continuously abstinent throughout the trial were 7.58 times more likely to become non-depressed than those who returned to drinking, suggesting that treatment of alcohol dependence is an important first step in managing concurrent depression.
In an effort to assess the effects of acamprosate on sleep disturbances in alcohol-dependent patients, a meta-analysis of 13 randomized trials (n = 3508) was conducted (reported as an abstract) [55]. The majority (61 %) of patients had significant sleep disturbance symptoms at baseline, and the main endpoint of the analysis was the change is Short Sleep Index (SSI) scores from baseline to 6 months (reductions in SSI scores indicated improvement). Mean reductions in SSI scores were 45 % with acamprosate and 26 % with placebo (p < 0.001). The proportion of patients with significant sleep disturbance at baseline who did not have this at 6 months was also significantly higher with acamprosate than placebo (54 vs. 44 %; p < 0.0001). The effect of acamprosate on abstinence accounted for 56 % of its total effect of sleep disturbances.
3.2 Treatment of Other Conditions
Acamprosate has been evaluated in off-label uses for the management of pathological gambling [56, 57], anxiety disorders [58, 59] and tinnitus [60] in small studies with up to 50 patients.
Pathological gambling is a behavioural addiction, and part of the rationale for considering the glutamatergic drug acamprosate in its management is that the excitatory neurotransmitter glutamate is thought to be involved in the pathophysiology of addictive behaviours [61]. Promising results were reported from an 8-week, open-label trial with acamprosate in 26 individuals with a clinical diagnosis of pathological gambling and a recent history of multiple gambling episodes [56]. In participants who received acamprosate 1998 mg/day, a statistically significant improvement was observed over the 8-week study period for scores on the Yale-Brown Obsessive Compulsive Scale modified for pathological gambling (Y-BOCS-PG), which was the primary endpoint. The mean Y-BOCS-PG total score decreased from 21.0 at baseline to 10.5 at 8 weeks (p < 0.001), and statistically significant improvements from baseline were also observed for both (urge/thought and behavioural) subscales of the Y-BOCS-PG [56].
In contrast, neither acamprosate (mean dosage 666 mg/day) nor baclofen (mean dosage 30 mg/day) were deemed to be effective in a 6-month, randomized, investigator-blind trial in 17 men with pathological gambling, although the main outcome was complete abstinence [57] (and therefore more difficult to achieve than improved Y-BOCS-PG scores shown in the other trial). There were also no statistically significant changes in visual analogue scores, Hamilton Rating Scale for Anxiety (HARS) scores or Hamilton Depression Rating Scale scores from baseline to relapse in either treatment group.
Acamprosate has also been investigated as augmentation therapy in the management of anxiety because of its pharmacodynamic effects of restoring pathological imbalances between neuronal excitation by glutamate and neuronal inhibition by GABA [58, 59]. When added to current anti-anxiety medication and psychotherapy, acamprosate significantly improved Clinical Global Impressions-Severity of Illness scale and HARS scores from baseline to endpoint in a 4-month, open-label study in 21 patients with an anxiety disorder [59]. Promising results were also reported in an 8-week, open-label trial with acamprosate 1998 mg/day in 13 patients who were stable but still symptomatic on their current medication of selective serotonin reuptake inhibitors or serotonin-norepinephrine reuptake inhibitors [58]. Among eight evaluable patients with at least two consecutive visits, mean HARS scores improved from 20 at baseline to 8.9 at the end of the study (p < 0.001), and 62 % of patients achieved remission (HARS score ≤7).
The dual effects of acamprosate on the glutamatergic and GABA systems may also be of benefit in the management of tinnitus, as suggested by findings of a randomized, double-blind, placebo-controlled trial in 50 patients with tinnitus of sensorineural origin [60]. Patients were randomized to acamprosate 999 mg/day or placebo for 3 months. The main endpoint was the change from baseline to 3 months in tinnitus score, which was rated from 1 to 10 by patients according to how much they were disturbed by the condition. The proportion of patients with any level of improvement (87 vs. 44 %; p = 0.004) or with ≥50 % improvement (48 vs. 11 %; p = 0.012) in tinnitus score was significantly greater among acamprosate than placebo recipients.
4 Tolerability
Acamprosate has been available in numerous countries for many years and has a well established tolerability profile [9, 62]. US prescribing information states that the most common adverse events with acamprosate are accidental injury, asthenia, pain, anorexia, diarrhoea, flatulence, nausea, anxiety, depression, dizziness, dry mouth, insomnia, paraesthesias, pruritus and sweating [9]. Overall, acamprosate was generally well tolerated in placebo-controlled trials, as any differences in the frequency of these adverse events between acamprosate (n = 2019; all dosages pooled) and placebo (n = 1706) were typically small, aside from diarrhoea, which was the most frequently reported adverse event with acamprosate or placebo (Fig. 1).
Adverse events reported in placebo-controlled trials with acamprosate (n = 2019) and placebo (n = 1706) [9]. Acamprosate groups included 1281 patients treated with 1998 mg/day, 397 patients treated with 1332 mg/day, 258 patients treated with 2000 mg/day and 83 patients treated with 3000 mg/day (the latter two used a different dosage strength and regimen). Pooled data from trials with spontaneously reported adverse events that occurred in any acamprosate treatment group in ≥3 % of patients and at a rate greater than the placebo group. When data for the four acamprosate dosages were pooled (shown in the figure), the rate is ≥2 % and not necessarily greater than the placebo group
The rates of discontinuation because of adverse events with acamprosate and placebo were 8 and 6 %, respectively, in studies ≤6 months in duration and 7 % in both groups in longer studies of up to 1 year, according to pooled data from placebo-controlled trials including a total of >2000 patients who received acamprosate [9]. Diarrhoea was the only adverse event that led to the discontinuation of acamprosate in >1 % of patients (2 % with acamprosate vs. 0.7 % with placebo).
Acamprosate is contraindicated in patients with severe renal impairment [creatinine clearance (CLCR) ≤30 mL/min] (see Sect. 6) and in those who are hypersensitive to the drug or any of its components [9]. In addition, all patients who are alcohol-dependent, including those receiving acamprosate, should be monitored for the development of symptoms of depression or suicidal thinking. Although adverse events of a suicidal nature (suicidal ideation, suicide attempts, completed suicides) were reported in 1.4 % of acamprosate recipients compared with 0.5 % of placebo recipients in clinical trials of ≤6 months’ duration, and in 2.4 versus 0.8 %, respectively, in longer-term trials of ≈1 year, the overall rates of completed suicides were 0.13 % in the pooled acamprosate group (3 of 2272 patients) and 0.10 % in the placebo group (2 of 1962 patients) [9].
In the COMBINE trial (Sect. 3.1.2), there were two serious adverse events possibly related to treatment, including one with acamprosate and one with naltrexone, and the rate of treatment withdrawal because of adverse events was generally similar across treatment groups (1 % with placebo, 3 % with acamprosate, 4 % with naltrexone and 4 % with the combination of acamprosate plus naltrexone) [42]. Overall, there were 12 cases of elevated aspartate aminotransferase or alanine transaminase levels (≥5 times the upper limit of normal), mainly occurring in naltrexone recipients (1 receiving acamprosate, 6 receiving naltrexone and 5 receiving both drugs; p = 0.02 for difference across groups). Other statistically significant differences across groups (placebo, acamprosate, naltrexone, both drugs) were observed for nausea (21, 24, 34 and 42 %; p < 0.001), vomiting (9, 9, 15 and 18 %; p < 0.001), diarrhoea (35, 65, 31 and 56 %; p < 0.001), decreased appetite (13, 19, 21 and 25 %; p = 0.002) and somnolence (24, 31, 37 and 31 %; p = 0.003) [42]. In the recent large meta-analysis (Sect. 3.1.3), naltrexone had a NNT for harm of 48 (95 % CI 30–112) for withdrawal from trials because of adverse events, whereas the risk was not significantly increased for acamprosate [28].
5 Pharmacoeconomic Considerations
Pharmacoeconomic analyses of adjuvant acamprosate therapy in the management of alcohol dependence have consistently shown that acamprosate is dominant (i.e. less costly and more effective) over rehabilitation strategies not involving pharmacotherapy [63–67], as reviewed in detail by Poldrugo et al. [68]. All of the analyses were conducted in Europe in the 1990s and published >10 years ago. Study methodology varied somewhat between analyses in that: (i) most used Markov modeling [63–65, 67], but one collected patient-level cost and outcomes data alongside a prospective, open-label, naturalistic study [66]; (ii) the time horizon was relatively short (1 or 2 years) in some analyses [65, 66] and longer (e.g. lifetime) in others [63, 64, 67]; (iii) some included direct costs only [63–65], whereas others considered both direct and indirect (e.g. lost productivity) costs [66, 67]; (iv) although all analyses included hospitalization, rehabilitation and drug acquisition costs, other types of costs included varied across the analyses; and (v) different clinical trial data were used for estimating or measuring key outcomes. The year of costing ranged from 1995–1997 and the analyses were conducted in Germany [63, 64, 66], Belgium [65] and Spain [67]. All of the analyses have been reported in English, except the Spanish analysis [67], although the latter was reviewed by Poldrugo et al. [68].
All of the analyses showed that the cost of acamprosate was more than offset by reductions in other costs, most notably hospitalization and rehabilitation costs, resulting in an overall cost saving [63–67]. Poldrugo and colleagues [68] adjusted the results of each analysis (except the Spanish analysis, which did not provide specific data) to 2004 values and reported that the savings in direct costs per treated patient attributable to acamprosate use were €1450/life [63] and €983/life [64] in the two German analyses with lifetime horizons, €363/year in the short-term German analysis conducted alongside a prospective clinical study [66], and €291/year in the Belgian analysis with a 2-year time horizon [65]. Sensitivity analyses (of the four modeled analyses) showed that results were most sensitive to changes in abstinence rates [68].
6 Dosage and Administration
Acamprosate is orally administered and used as an adjunct to psychosocial support for the maintenance of abstinence from alcohol in patients with alcohol dependence who are abstinent at treatment initiation. US, EU and Japanese prescribing information recommend that acamprosate be taken after (with) meals [9, 27, 62]. In France, it is preferred to administer acamprosate a (nonspecified) period of time after meals if gastrointestinal tolerance is good [69].
In the USA [9] and Japan [27], the recommended regimen is 666 mg (two 333 mg tablets) taken orally three times daily. The recommended regimen in the EU is 666 mg three times daily with meals in individuals weighing ≥60 kg (i.e. total daily dosage 1998 mg) [62]. In those weighing <60 kg, the total daily dosage of acamprosate should be reduced to 1332 mg (i.e. four tablets) administered as follows: two tablets in the morning, one at noon and one at night [62].
In the EU, the recommended treatment period is 1 year [62]. Treatment with acamprosate should be initiated as soon as possible after the withdrawal period and should be maintained if the patient relapses [62]. US prescribing information states that acamprosate should be initiated as soon as possible after the period of alcohol withdrawal, when the patient has achieved abstinence, and should be maintained if the patient relapses [9]. In Japan, in principle, the administration period is 24 weeks [27]. It is possible to extend the period of administration, but only if therapeutic benefits are observed and sufficient attention is given to safety. In clinical trials in Japan, the efficacy and safety of acamprosate was demonstrated over a treatment period of 24 weeks [27].
Acamprosate may be used without dosage adjustment in patients with mild to moderate hepatic impairment, although dosage adjustments or contraindications are recommended in patients with renal impairment [9, 27, 62]. For example, US prescribing information states that for patients with moderate renal impairment (CLCR 30–50 mL/min), a starting dose of one 333 mg tablet taken three times daily is recommended, and acamprosate is contraindicated in patients with severe renal impairment (CLCR ≤30 mL/min) [9].
The approved dosage regimen of acamprosate and its recommended duration of treatment may vary between countries, and local prescribing information should be consulted. Local prescribing information should also be consulted for additional information on warnings, precautions, contraindications, drug interactions and use in special patient populations.
7 Place of Acamprosate in the Management of Alcohol Dependence
Acamprosate is widely used as an adjunct to psychosocial support for the maintenance of abstinence from alcohol in patients with alcohol dependence. It is available in ≈25 countries, including Japan, where it recently gained approval for this indication [27, 33].
The efficacy of acamprosate in improving alcohol-consumption outcomes has been demonstrated in several placebo-controlled and/or active-comparator controlled trials of 3–12 months’ duration (Sect. 3.1), although results were not always consistent across studies, perhaps in part because of trial heterogeneity (e.g. patient populations, psychosocial co-interventions). Of particular interest are results of a recent trial designed to accommodate usual clinical practices in Japan (e.g. extended inpatient rehabilitation period after detoxification), which showed that acamprosate was statistically superior to placebo for complete abstinence rate over ≈6 months (Sect. 3.1.1). Although comparative studies between acamprosate and naltrexone provided somewhat equivocal or disparate results (Sect. 3.1.2), again perhaps owing in part to trial heterogeneity, findings of a recent meta-analysis indicate that both acamprosate and naltrexone 50 mg/day orally were associated with improvements in alcohol-consumption outcomes compared with placebo (Sect. 3.1.3).
Pharmacological treatment options approved to facilitate the maintenance of abstinence in alcohol-dependent patients are limited and include acamprosate, naltrexone (an opioid antagonist), disulfiram (an aldehyde dehydrogenase inhibitor) and, in some countries, nalmefene (an opioid system modulator for reduction of alcohol consumption rather than abstinence) and sodium oxybate (the sodium salt of γ-hydroxybutyric acid), although other drugs not approved for this indication (e.g. topiramate) have been investigated in clinical trials [1, 4–7, 70–74]. In general, treatment guidelines indicate that acamprosate and oral naltrexone provide similar, modest improvements in alcohol-consumption outcomes when used in conjunction with psychosocial interventions after successful withdrawal from alcohol, and the selection between these agents depends on patient characteristics (e.g. the presence of a condition that may make a drug contraindicated), patient and/or physician preference, tolerability, drug availability and cost or pharmacoeconomic considerations [5–7].
Guidelines from NICE in the UK, which appear to be the most recent guidance available on the management of alcohol dependence, recommend either acamprosate or oral naltrexone as first-line pharmacotherapy [7]. They also state that disulfiram (as an adjunct to psychosocial intervention) may be considered in patients who have a goal of abstinence but for whom acamprosate and oral naltrexone are not suitable or for patients who prefer disulfiram and understand its relative risks (i.e. the interaction between disulfiram and alcohol, and the possibility of hepatotoxicity) [7].
NICE guidelines recommend that treatment with either acamprosate or naltrexone should be started as soon as possible after assisted withdrawal from alcohol [7]. With respect to acamprosate, the guidelines note that it is usually prescribed for up to 6 months, or longer for those benefiting from acamprosate who want to continue with this therapy. The guidelines also suggest that acamprosate should be stopped if drinking persists 4–6 weeks after starting the drug [7].
In general, treatment guidelines do not advocate the use of combination regimens, as there is inadequate evidence to support their use [5–7]. Randomized trials with acamprosate as part of combination regimens generally provided equivocal results (Sect. 3.1.2).
It is noteworthy that acamprosate has also shown useful effects on complications of alcohol dependence, including sleep disturbances (Sects. 2.1, 3.1.1 and 3.1.3) and depression (Sect. 3.1.3). These effects appear to be related, at least in part, to the beneficial effects of acamprosate on reducing alcohol consumption. Also of interest are promising findings from small studies evaluating acamprosate in other conditions, such as pathological gambling (Sect. 3.2).
In conclusion, the use of acamprosate as an adjunct to psychosocial interventions in alcohol-dependent patients provides modest but potentially valuable improvements in alcohol-consumption outcomes and is generally well tolerated.
Data selection sources:
Relevant medical literature (including published and unpublished data) on acamprosate was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated 2 June 2015], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Acamprosate, Alcomed, Aotal, Campral, Regtect, Sobriol, Zulex.
Study selection: Studies in patients with alcoholism who received acamprosate. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Jonas DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol-use disorders in outpatient settings. Comparative effectiveness review no. 134. Agency for Healthcare Research and Quality publication no. 14-EHC029-EF. 2014 May. www.effectivehealthcare.ahrq.gov/reports/final.cfm. Accessed 2015 May 18.
World Health Organization. Global status report on alcohol and health. 2014. http://www.who.int/substance_abuse/publications/global_alcohol_report/msb_gsr_2014_1.pdf. Accessed 2015 May 18.
Centers for Disease Control and Prevention. Alcohol use and your health. http://www.cdc.gov/alcohol/fact-sheets/alcohol-use.htm. Accessed 2015 May 18.
Johnson BA. Update on neuropharmacological treatments for alcoholism: scientific basis and clinical findings. Biochem Pharmacol. 2008;75(1):34–56.
Lingford-Hughes AR, Welch S, Nutt DJ. Evidence-based guidelines for the pharmacological management of substance misuse, addiction and comorbidity: recommendations from the British Association for Psychopharmacology. J Psychopharmacol (Oxf). 2004;18(3):293–335.
US Department of Health and Human Services National Insitutes of Health. Helping patients who drink too much: a clinician’s guide. 2008. www.niaaa.nih.gov/guide. Accessed 2015 May 18.
National Institute for Health and Care Excellence. Alcohol-use disorders: diagnosis, assesment and management of harmful drinking and alcohol dependence. 2011. http://www.nice.org.uk/guidance/cg115. Accessed 2015 May 18.
Mason BJ, Heyser CJ. Acamprosate: a prototypic neuromodulator in the treatment of alcohol dependence. CNS Neurol Disord Drug Targets. 2010;9(1):23–32.
Campral (acamprosate calcium) delayed-release tablets: US prescribing information. 2012. http://pi.actavis.com/data_stream.asp?product_group=1928&p=pi&language=E. Accessed 2015 May 18.
Kalk NJ, Lingford-Hughes AR. The clinical pharmacology of acamprosate. Br J Clin Pharmacol. 2014;77(2):315–23.
Spanagel R, Vengeliene V. New pharmacological treatment strategies for relapse prevention. Curr Top Behav Neurosci. 2013;13:583–609.
De Witte P, Littleton J, Parot P, et al. Neuroprotective and abstinence-promoting effects of acamprosate: elucidating the mechanism of action. CNS Drugs. 2005;19(6):517–37.
Harris BR, Prendergast MA, Gibson DA, et al. Acamprosate inhibits the binding and neurotoxic effects of trans-ACPD, suggesting a novel site of action at metabotropic glutamate receptors. Alcohol Clin Exp Res. 2002;26(12):1779–93.
Rammes G, Mahal B, Putzke J, et al. The anti-craving compound acamprosate acts as a weak NMDA-receptor antagonist, but modulates NMDA-receptor subunit expression similar to memantine and MK-801. Neuropharmacology. 2001;40(6):749–60.
Oka M, Hirouchi M, Tamura M, et al. Acamprosate monocalcium bis(3-acetamidopropane-1-sulfonate) reduces ethanol-drinking behavior in rats and glutamate-induced toxicity in ethanol-exposed primary rat cortical neuronal cultures. Eur J Pharmacol. 2013;718(1-2-3):323–31.
Spanagel R, Kiefer F. Drugs for relapse prevention of alcoholism: ten years of progress. Trends Pharmacol Sci. 2008;29(3):109–15.
Mann K, Kiefer F, Spanagel R, et al. Acamprosate: recent findings and future research directions. Alcohol Clin Exp Res. 2008;32(7):1105–10.
Spanagel R, Pendyala G, Abarca C, et al. The clock gene Per2 influences the glutamatergic system and modulates alcohol consumption. Nat Med. 2005;11(1):35–42.
Umhau JC, Momenan R, Schwandt ML, et al. Effect of acamprosate on magnetic resonance spectroscopy measures of central glutamate in detoxified alcohol-dependent individuals: a randomized controlled experimental medicine study. Arch Gen Psychiatry. 2010;67(10):1069–77.
Spanagel R, Vengeliene V, Jandeleit B, et al. Acamprosate produces its anti-relapse effects via calcium. Neuropsychopharmacology. 2014;39(4):783–91.
Heilig M. Acamprosate: an alcoholism treatment that may not be what we thought. Neuropsychopharmacology. 2014;39(4):781–2.
Kurokawa K, Mizuno K, Shibasaki M, et al. Acamprosate suppresses ethanol-induced place preference in mice with ethanol physical dependence. J Pharmacol Sci. 2013;122(4):289–98.
Pahicha-Poniewiera A, Pilea A. Involvement of mGlu5 and NMDA receptors in the antidepressant-like effect of acamprosate in the tail suspension test. Prog Neuropsychopharmacol Biol Psychiatry. 2012;39:102–6.
Staner L, Boeijinga P, Danel T, et al. Effects of acamprosate on sleep during alcohol withdrawal: A double-blind placebo-controlled polysomnographic study in alcohol-dependent subjects. Alcohol Clin Exp Res. 2006;30(9):1492–9.
Saivin S, Hulot T, Chabac S, et al. Clinical pharmacokinetics of acamprosate. Clin Pharmacokinet. 1998;35(5):331–45.
Scott LJ, Figgitt DP, Keam SJ, et al. Acamprosate: a review of its use in the maintenance of abstinence in patients with alcohol dependence. CNS Drugs. 2005;19(5):445–64.
Nippon Shinyaku. Regtect (acamprosate calcium): Japan prescribing information. 2013.
Jonas DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014;311(18):1889–900.
Berger L, Fisher M, Brondino M, et al. Efficacy of acamprosate for alcohol dependence in a family medicine setting in the United States: a randomized, double-blind, placebo-controlled study. Alcohol Clin Exp Res. 2013;37(4):668–74.
Chick J, Howlett H, Morgan MY, et al. United Kingdom Multicentre Acamprosate Study (UKMAS): a 6-month prospective study of acamprosate versus placebo in preventing relapse after withdrawal from alcohol. Alcohol Alcohol. 2000;35(2):176–87.
Geerlings PJ, Ansoms C, Den Van, Brink W. Acamprosate and prevention of relapse in alcoholics. Results of a randomized, placebo-controlled, double-blind study in out-patient alcoholics in the Netherlands, Belgium and Luxembourg. Eur Addict Res. 1997;3(3):129–37.
Gual A, Lehert P. Acamprosate during and after acute alcohol withdrawal: a double-blind placebo-controlled study in Spain. Alcohol Alcohol. 2001;36(5):413–8.
Higuchi S. Efficacy of acamprosate for the treatment of alcohol dependence long after recovery from withdrawal syndrome: a randomized, double-blind, placebo-controlled study conducted in Japan (Sunrise study). Japanese Acamprosate Study Group. J Clin Psychiatry. 2015;76(2):181–8.
Mason BJ, Goodman AM, Chabac S, et al. Effect of oral acamprosate on abstinence in patients with alcohol dependence in a double-blind, placebo-controlled trial: the role of patient motivation. J Psychiatr Res. 2006;40(5):383–93.
Pelc I, Verbanck P, Le Bon O, et al. Efficacy and safety of acamprosate in the treatment of detoxified alcohol-dependent patients. A 90-day placebo-controlled dose-finding study. Br J Psychiatry. 1997;171:73–7.
Poldrugo F. Acamprosate treatment in a long-term community-based alcohol rehabilitation programme. Addiction. 1997;92(11):1537–46.
Tempesta E, Janiri L, Bignamini A, et al. Acamprosate and relapse prevention in the treatment of alcohol dependence: a placebo-controlled study. Alcohol Alcohol. 2000;35(2):202–9.
Paille FM, Guelfi JD, Perkins AC, et al. Double-blind randomized multicentre trial of acamprosate in maintaining abstinence from alcohol. Alcohol Alcohol. 1995;30(2):239–47.
Sass H, Soyka M, Mann K, et al. Relapse prevention by acamprosate. Results from a placebo-controlled study on alcohol dependence. Arch Gen Psychiatry. 1996;53(8):673–80.
Whitworth AB, Fischer F, Lesch OM, et al. Comparison of acamprosate and placebo in long-term treatment of alcohol dependence. Lancet. 1996;347(9013):1438–42.
Perney P, Lehert P, Mason BJ. Sleep disturbance in alcoholism: proposal of a simple measurement, and results from a 24-week randomized controlled study of alcohol-dependent patients assessing acamprosate efficacy. Alcohol Alcohol. 2012;47(2):133–9.
Anton RF, O’Malley SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–17.
Besson J, Aeby F, Kasas A, et al. Combined efficacy of acamprosate and disulfiram in the treatment of alcoholism: a controlled study. Alcohol Clin Exp Res. 1998;22(3):573–9.
de Sousa A, de Sousa A. An open randomized study comparing disulfiram and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2005;40(6):545–8.
Kiefer F, Jahn H, Tarnaske T, et al. Comparing and combining naltrexone and acamprosate in relapse prevention of alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2003;60(1):92–9.
Laaksonen E, Koski-Jannes A, Salaspuro M, et al. A randomized, multicentre, open-label, comparative trial of disulfiram, naltrexone and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2008;43(1):53–61.
Mann K, Lemenager T, Hoffmann S, et al. Results of a double-blind, placebo-controlled pharmacotherapy trial in alcoholism conducted in Germany and comparison with the US COMBINE study. Addict Biol. 2013;18(6):937–46.
Morley KC, Teesson M, Reid SC, et al. Naltrexone versus acamprosate in the treatment of alcohol dependence: a multi-centre, randomized, double-blind, placebo-controlled trial. Addiction. 2006;101(10):1451–62.
Rosner S, Hackl-Herrwerth A, Leucht S, et al. Acamprosate for alcohol dependence. Cochrane Database Syst Rev. 2010;9:CD004332.
Maisel NC, Blodgett JC, Wilbourne PL, et al. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction. 2013;108(2):275–93.
Lehert P, Rosner S. The impact of treatment duration in alcoholism: an individual patient meta-analysis on acamprosate randomized controlled trials [abstract no. O2.2]. Alcohol Alcohol. 2013;48(Suppl1)(1):i35–i6.
Mason BJ, Lehert P. Acamprosate for alcohol dependence: a sex-specific meta-analysis based on individual patient data. Alcohol Clin Exp Res. 2012;36(3):497–508.
Chick J, Lehert P, Landron F. Does acamprosate improve reduction of drinking as well as aiding abstinence? J Psychopharmacol. 2003;17(4):397–402.
Lejoyeux M, Lehert P. Alcohol-use disorders and depression: results from individual patient data meta-analysis of the acamprosate-controlled studies. Alcohol Alcohol. 2011;46(1):61–7.
Perney P, Lehert P. Effect of acamprosate on sleep disturbances in alcoholism: an individual patient data meta-analysis [abstract no. P28]. Alcohol Alcohol. 2013;48:i47.
Black DW, McNeilly DP, Burke WJ, et al. An open-label trial of acamprosate in the treatment of pathological gambling. Ann Clin Psychiatry. 2011;23(4):250–6.
Dannon PN, Rosenberg O, Schoenfeld N, et al. Acamprosate and baclofen were not effective in the treatment of pathological gambling: preliminary blind rater comparison study. Front Psychiatry. 2011;2:33.
Schwartz TL, Siddiqui UA, Raza S, et al. Acamprosate calcium as augmentation therapy for anxiety disorders. Ann Pharmacother. 2010;44(12):1930–2.
Hertzman M, Patt IS, Spielman LA. Open-label trial of acamprosate as a treatment for anxiety. Prim Care Companion J Clin Psychiatry. 2009;11(5):267.
Azevedo AA, Figueiredo RR. Tinnitus treatment with acamprosate: double-blind study. Braz J Otorhinolaryngol. 2005;71(5):618–23.
Pettorruso M, De Risio L, Martinotti G, et al. Targeting the glutamatergic system to treat pathological gambling: current evidence and future perspectives. Biomed Res Int. 2014;2014:109786.
Campral EC (acamprosate calcium enteric-coated tablets): summary of product characteristics. 2012. http://www.medicines.org.uk/emc/medicine/1042/SPC/Campral+EC/. Accessed 18 May 2015.
Schadlich PK, Brecht JG. The cost effectiveness of acamprosate in the treatment of alcoholism in Germany. Economic evaluation of the Prevention of Relapse with Acamprosate in the Management of Alcoholism (PRAMA) study. Pharmacoeconomics. 1998;13(6):719–30.
Palmer AJ, Neeser K, Weiss C, et al. The long-term cost-effectiveness of improving alcohol abstinence with adjuvant acamprosate. Alcohol Alcohol. 2000;35(5):478–92.
Annemans L, Vanoverbeke N, Tecco J, et al. Economic evaluation of Campral (acamprosate) compared to placebo in maintaining abstinence in alcohol-dependent patients. Eur Addict Res. 2000;6(2):71–8.
Rychlik R, Siedentop H, Pfeil T, et al. Cost-effectiveness of adjuvant treatment with acamprosate in maintaining abstinence in alcohol dependent patients. Eur Addict Res. 2003;9(2):59–64.
Portella E, Ridao M, Carrillo E, et al. El alcohol y su abuso: impacto socioeconomico. Madrid: Editorial Medica Panamericana; 1998.
Poldrugo F, Haeger DA, Comte S, et al. A critical review of pharmacoeconomic studies of acamprosate. Alcohol Alcohol. 2005;40(5):422–30.
Acamprosate (Aotal): French prescribing information. http://www.vidal.fr. Accessed 2015 May 18.
Selincro (nalmefene): summary of product characteristics. 2015. https://www.medicines.org.uk. Accessed 18 May 2015.
National Institute for Health and Care Excellence. Nalmefene for reducing alcohol consumption in people with alcohol dependence. 2014. https://www.nice.org.uk/guidance/ta325/. Accessed 18 May 2015.
Revia (nalrexone hydrochloride) tablets: US prescribing information. 2013. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/018932s017lbl.pdf. Accessed 18 May 2015.
Chan LN, Anderson GD. Pharmacokinetic and pharmacodynamic drug interactions with ethanol (alcohol). Clin Pharmacokinet. 2014;53(12):1115–36.
Keating GM. Sodium oxybate: a review of its use in alcohol withdrawal syndrome and in the maintenance of abstinence in alcohol dependence. Clin Drug Investig. 2014;34(1):63–80.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes based on any comments received were made by the author on the basis of scientific and editorial merit. Greg Plosker is a salaried employee of Adis/Springer.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: M. Pettorruso, Institute of Psychiatry and Psychology, Catholic University of the Sacred Heart, Rome, Italy; A. Yoshimura, National Hospital Organization, Kurihama Medical and Addiction Center, Yokosuka, Japan.
Rights and permissions
About this article
Cite this article
Plosker, G.L. Acamprosate: A Review of Its Use in Alcohol Dependence. Drugs 75, 1255–1268 (2015). https://doi.org/10.1007/s40265-015-0423-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-015-0423-9