Abstract
Introduction
Nalmefene is the first drug to be approved for reducing alcohol consumption in alcohol use disorder (AUD) patients at high drinking risk. In real-world settings, there is a high prevalence of concurrent psychiatric disorders in AUD subjects, with associated increased morbidity and worse prognosis. This study evaluated the use of nalmefene in AUD patients with stabilized psychiatric comorbidity previously treated unsuccessfully for alcohol dependence, and assessed craving reduction and safety.
Methods
Sixty-five AUD outpatients treated with as-needed 18 mg nalmefene for 24 weeks were included. Primary outcome measures were: changes in heavy drinking days (HDDs) and total alcohol consumption (TAC, g/day). Secondary outcome measures were: changes in drinking risk level and craving (obsessive–compulsive drinking scale and visual analogue scale for craving).
Results
Forty-two AUD subjects (64.6%) had one or more stabilized psychiatric comorbidity. There was a significant reduction in HDDs, TAC and craving measures (p < 0.001), with no differences between subjects with and without psychiatric comorbidity. Nalmefene was safe and well tolerated in all patients.
Conclusion
As-needed nalmefene reduced drinking and craving in AUD subjects with and without psychiatric comorbidity. These findings suggest that nalmefene is a valid therapeutic option in real-world clinical settings, where comorbid conditions are common, and has the potential to engage AUD patients who may otherwise not have sought help.
Funding
Lundbeck Italia S.P.A.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol use disorder (AUD) is defined by a cluster of behavioral and physical symptoms, which can include withdrawal, tolerance and craving [1]. It is a common, chronic, relapsing condition, causing substantial morbidity and a threefold increase in early mortality rates [2, 3]. AUD is a major public health problem and represents a huge social and economic burden, with almost 15 million affected individuals in Europe [4,5,6]. Even so, AUD is often underdiagnosed and undertreated [7]; in Europe, only 10% of AUD patients receive treatment [8] and more than two-thirds of treated patients relapse within the first 12 months [9].
Population-based epidemiologic studies have documented a high prevalence of concurrent psychiatric disorders in individuals with AUD, as well as a higher prevalence of AUD among psychiatric patients compared with the general population [10, 11]. There is a high prevalence of AUD in patients diagnosed with schizophrenia, mood disorders, anxiety disorders and personality disorders. Moreover, even when no formal diagnosis (DSM or ICD) can be formulated, the presence of concurrent psychopathological symptoms is the norm rather than the exception, as it is for the dimensions of impulsiveness [12], anhedonia [13] and alexithymia [14].
Despite high comorbidity rates, little attention has been paid to the clinical management of individuals with AUD and psychiatric disorders. To date, most studies have not had a randomized design or included a placebo comparison. In addition, most current studies do not include approved medications for AUD and, specifically, the combination of targeted pharmacotherapies for the psychiatric disorder and for AUD. Preliminary studies have tested the use of topiramate [15], pregabalin [16], oxcarbazepine [17], baclofen [18], acamprosate [19], acetyl-L-carnitine [20], quetiapine [21] and aripiprazole [22, 23], but larger, controlled studies are warranted to confirm these findings. Given comorbid psychiatric conditions are associated with an increased risk of psychopathology, increased suicide risk, poor prognosis, increased morbidity, overall functional decline and worse treatment outcome in subjects with AUD [24,25,26], further research on pharmacological treatments for concurrent AUD and psychiatric disorders is needed.
The goal of treatment in AUD patients has traditionally been to achieve abstinence, prevent relapse and reduce craving [27]. Reduction in alcohol consumption has widely been considered an intermediate goal on the way to full abstinence [28]. Also, reduction in alcohol consumption has been found to be associated with harm reduction and a decreased risk of morbidity and mortality [29,30,31]. However, a subgroup of AUD patients is not inclined to achieve abstinence.
Nalmefene, a 6-methylene derivative of naltrexone, is the first drug to be approved in the European Union for reducing alcohol consumption in AUD adults with a high drinking risk level based on WHO guidelines (total alcohol consumption >60 g/day in men or >40 g/day in women) and who continue to have a high drinking risk level 2 weeks after initial assessment [32]. Nalmefene is a dual-acting opioid system modulator with distinct μ, δ, and k-receptor profile (antagonistic activity at the μ and δ opioid receptors and partial agonistic activity at the k opioid receptor) [33, 34]. Nalmefene given on an as-needed basis has been shown to reduce total alcohol consumption and the number of heavy drinking days (HDDs), to improve liver function and clinical status, and was generally well tolerated in AUD patients in two 6-month studies [35, 36]. Therefore, nalmefene represents a valid treatment option for AUD patients who are unable to significantly reduce their alcohol consumption after an initial abstinence-oriented intervention [37,38,39,40].
AUD patients are often excluded from clinical trials assessing the efficacy of psychiatric medications, and patients with psychiatric comorbidity are usually excluded from clinical trials assessing efficacy of pharmacotherapies for AUD. Given the abovementioned high prevalence of concurrent psychiatric disorders in AUD patients, investigating nalmefene in a sample of AUD subjects with psychiatric comorbidity may better relate to real-world use and have important implications for everyday clinical practice.
This study investigated the use of nalmefene in AUD subjects with stabilized psychiatric comorbidity who had previously been treated unsuccessfully for alcohol dependence. Additional aims were to assess the usefulness of nalmefene in reducing alcohol craving and to determine the safety and tolerability of nalmefene.
Methods
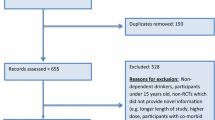
Data were obtained from 65 AUD outpatients admitted to the Day-Hospital of Psychiatry of the University General Hospital “A. Gemelli” in Rome, the Institute of Psychiatry of the “G. d’Annunzio” University in Chieti, the psychiatric clinic “Von Siebenthal” in Rome, and the “Vincent P. Dole” Dual Diagnosis Unit of the Santa Chiara University Hospital in Pisa between January 2014 and December 2016. Participants were evaluated using the Structured Clinical Interviews for DSM-IV [41, 42].
Inclusion criteria were: age 18–65 years; DSM-5 diagnosis of AUD [1]; ≥6 HDDs/month (≥60 g/day for men, ≥40 g/day for women) at baseline; alcohol consumption at least at the WHO high drinking risk level at baseline; ability to speak and write Italian.
Exclusion criteria were: severe cognitive deficits (a Mini-Mental State Examination score <26 [43]); neurological or medical disorders impairing evaluation; pregnancy (positive serum β-HCG test result), lactation, or participation in other trials involving any investigational drug during the 60 days prior to nalmefene administration.
Patients included in the study had taken, over a 6-month period, one tablet of 18 mg nalmefene on each day they perceived a risk of drinking alcohol (as-needed dosing). Data were obtained from measurements and assessments that had been performed at baseline and every 4 weeks. The Timeline Follow-back [44] estimated daily drinking and daily medication intake.
The following psychometric tests had been administered:
-
the brief psychiatric rating scale (BPRS) [45] to assess psychiatric symptomatology.
-
the Hamilton depression and anxiety rating scales [46, 47] and the Young Mania Rating Scale (YMRS) [48] to assess mood and anxiety symptoms.
-
the clinical global impression-severity of illness (CGI-S) [49].
-
the Italian version of the obsessive–compulsive drinking scale (OCDS) [50] and the visual analogue scale for alcohol craving (VASc) [51] to assess craving.
Primary outcome measures were: changes in the number of HDDs and total alcohol consumption (TAC, g/day) from baseline to month 6. Secondary outcome measures were changes (from baseline to month 6) in drinking risk level (DRL), CGI-S score and craving levels. The safety of nalmefene was determined by measurements of mean corpuscular volume (MCV), alanine aminotransaminase (ALAT) and gamma-glutamyl transpeptidase (γ-GT) at baseline and after 12 and 24 weeks of nalmefene treatment.
All participants were provided a continuous psychosocial support focused on treatment adherence and reducing alcohol consumption, consisting of twice a week group sessions according to the BRENDA model [52].
Statistical Analysis
Descriptive data were summarized as the number of patients and percentage (%) or mean ± standard deviation (SD). Comparisons between groups were performed using Independent Samples t test (continuous variables) or Chi square test (dichotomous variables). Time to first event was evaluated using Kaplan–Meier analysis and curves. Subjects with and without comorbidity were compared using the log-rank test. To control whether there was a significant difference between the same variables within group, pre- and post-treatment, Wilcoxon Signed Ranks test was used. To determine the impact of comorbidity on efficacy variables at 6 months, general linear models were used. The dependent variable was the modification of each efficacy variable after 6 months of treatment. The presence of comorbidity was one of the fixed factors. The models were also corrected for the values of the parameters which were significantly different between patients with versus patients without comorbidity at baseline. A significance level of 0.05 was used for each test. All analyses were conducted using IBM SPSS Statistics for Windows, v.20.0.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008. Informed consent was obtained from all patients before being included in the study.
Results
Demographic and Clinical Data
Forty-two AUD subjects (64.6%) had one or more comorbid psychiatric disorders: major depressive disorder (n = 8); bipolar disorder type I (n = 3); bipolar disorder type II (n = 8); bipolar disorder not otherwise specified (n = 2); dysthymia (n = 3); generalized anxiety disorder (n = 2); panic disorder (n = 4); obsessive compulsive disorder (n = 3); bulimia nervosa (n = 1); cocaine use disorder (n = 1); benzodiazepine use disorder (n = 4); gambling disorder (n = 2); dependent personality disorder (n = 2); borderline personality disorder (n = 2).
Twenty subjects (30.8%) were polyabusers: benzodiazepine (n = 4); cannabis (n = 8); cocaine (n = 13). Socio-demographic and baseline clinical characteristics of AUD subjects, overall and in those with and without psychiatric comorbidity, are shown in Tables 1 and 2.
AUD subjects with psychiatric comorbidity had achieved stabilization of the concurrent disorder and were following a naturalistic maintenance pharmacological treatment (Table 3).
Primary Outcome Measures
At the end of the study, patients without comorbidity had received 52.97 ± 17.6 nalmefene tablets (v1 = 16.9 ± 4.4; v2 = 9.5 ± 6.2; v3 = 12.4 ± 3.8; v4 = 5.36 ± 3.1; v5 = 2.7 ± 2.8; v6 = 2.7 ± 2.6), while comorbid subjects had received 74.3 ± 16 nalmefene tablets (v1 = 23 ± 5.1; v2 = 14.6 ± 5.7; v3 = 15 ± 2.8; v4 = 9.5 ± 5.1; v5 = 5.7 ± 4.3; v6 = 5.5 ± 4.6).
The reduction of TAC (g/day) from baseline over time was statistically significant in AUD patients both with and without comorbidity (Z = −6.797; p < 0.001). TAC scores did not significantly correlate with the presence/absence of psychiatric comorbidity (Fig. 1). The cumulative percentage of patients who reach TAC = 0 was 38.5%: 35.7% with and 43.5% without psychiatric comorbidity (χ 2 = 0.378; NS) (Fig. 2). The estimated time to reach TAC = 0 was 20.58 ± 0.6 weeks.
There was a statistically significant reduction in HDDs over time compared with baseline in both comorbid and non-comorbid patients (Z = −6.683; p < 0.001). HDDs did not significantly correlate with the presence/absence of psychiatric comorbidity (Fig. 3). The cumulative percentage of patients who reached HDD = 0 was 42.4%: 35.7% with and 54.5% without psychiatric comorbidity (χ 2 = 2.099; NS) (Fig. 2). The estimated time to reach HDD = 0 was 19.28 ± 0.8 weeks.
Secondary Outcome Measures
After 24 weeks of treatment with nalmefene, the majority of patients had achieved a decrease of at least one risk level (Fig. 4). At the same time, 56 patients (86.1%) showed a decrease in CGI-S score versus baseline (Z = −6.562; p < 0.001). With respect to craving levels, a significant reduction from baseline to month 6 was observed for OCDS scores in both comorbid and non-comorbid AUD patients (OCDS total, non-comorbid: 26.9 ± 7.6 vs. 9.5 ± 2.3, p < 0.001; OCDS total, comorbid: 21.9 ± 6.5 vs. 5.7 ± 3.3, p < 0.001; OCDS obsessive, non-comorbid: 13 ± 2.9 vs. 4.7 ± 1.5, p < 0.001; OCDS obsessive, comorbid: 10.2 ± 3.6 vs. 5.7 ± 3.3, p < 0.001; OCDS compulsive, non-comorbid: 13.9 ± 5 vs. 4.9 ± 1.4, p < 0.001; OCDS compulsive, comorbid: 11.7 ± 3.5 vs. 6.2 ± 3.7, p < 0.001). Similarly, a significant reduction of VASc scores was observed in both groups (non-comorbid: 7.6 ± 2.3 vs. 3.3 ± 2.2, p < 0.001; comorbid: 7.1 ± 1.5 vs. 4.7 ± 2.5, p < 0.001). No significant difference between groups, except for OCDS total and obsessive scores at baseline (higher in non-comorbid patients), was noted (Fig. 5).
Safety and Tolerability
A significant improvement from baseline to 6 months in both comorbid and non-comorbid AUD patients was observed for MCV (non-comorbid: 91.6 ± 6.2 fl vs. 87.4 ± 4.3 fl; comorbid: 94.2 ± 5.7 fl vs. 88.4 ± 6.2; Z = −5.1, p < 0.001), ALAT (non-comorbid: 42.3 ± 16.5 UI/L vs. 18.6 ± 6 UI/L; comorbid: 40.2 ± 14.4 UI/L vs. 28.2 ± 11.3 UI/L; Z = −4.9, p < 0.001) and γ-GT (non-comorbid: 59.3 ± 33.7 UI/L vs. 29.1 ± 15.9 UI/L; comorbid: 46.6 ± 18.1 UI/L vs. 29.9 ± 12.2 UI/L; Z = −5.2, p < 0.001). The reduction in ALAT levels was significantly higher in patients without psychiatric comorbidity (p = 0.021).
During the 6-month treatment period, 24 AUD subjects experienced at least one adverse event from nalmefene. The mean number of adverse events per patient was 0.72 (±1.35), the most commonly reported being dizziness, nausea, headache and insomnia. Most adverse events were transient (3–7 days), occurred within one day from the first dose, and were mild or moderate in intensity.
Discussion
The main finding of our study is that treatment with as-needed 18 mg nalmefene was generally well tolerated and significantly reduced drinking (TAC, HDDs, DRLs) in AUD patients with and without psychiatric comorbidity.
A major clinical issue that complicates AUD treatment is the common co-occurrence of other psychiatric disorders. Literature regarding concurrent AUD and psychiatric disorders has increased in recent years, and comorbidity has been associated with negative effects on symptom severity, treatment and general functioning [24,25,26].
AUD commonly co-occurs with schizophrenia; 33.7% of schizophrenic patients meet criteria for a lifetime AUD diagnosis. Both biological and psychosocial factors are thought to contribute to this co-occurrence. AUD complicates the clinical course and treatment outcome of schizophrenia. AUD is, in fact, correlated with poor concurrent adjustment and predictive of adverse outcomes such as higher rates of homelessness, hospitalization and incarceration [53].
Bipolar disorder (BD) has been reported to be the psychiatric comorbidity most strongly linked with AUD, particularly manic/hypomanic states [54]. A recent meta-analysis confirms this association and indicates that male BD patients have between 2 and 3 times greater risk of lifetime AUD [55]. Patients with concurrent AUD and BD present with a longer duration of withdrawal from alcohol, increased severity of manic and depressive symptoms [56], increased suicide risk, worse treatment response and increased morbidity [57, 58].
Personality disorders are also more prevalent in AUD patients than in the general population; prevalence rates have been reported to be over 70% in several clinical and epidemiological studies [59]. Personality disorders are an important contributing and/or predisposing factor in the pathogenesis and clinical course of AUD and have been found to negatively affect treatment outcome. Literature has focused primarily on antisocial and borderline personality disorders (BPD) [60, 61]. Data from the National Epidemiologic Survey on Alcohol and Related Conditions indicates that 58.3% of individuals with a lifetime diagnosis of BPD also had a lifetime diagnosis of AUD. In the same study, rates of co-occurrence of lifetime BPD in patients with AUD ranged from 9.8 to 14.7%. AUD and personality disorders comorbidity is also associated with poor social functioning, low rates of treatment retention, an increased risk of relapse and a worse prognosis [62].
A high prevalence of comorbid anxiety disorders and alcohol dependence in the general population and in clinical samples has been consistently reported [63]. Phobic disorders (social phobia and agoraphobia) were found to serve as a primary diagnosis in most cases, whereas panic disorder and generalized anxiety disorders are more often diagnosed after the onset of alcohol dependence. Furthermore, high rates of concurrent use of other substances over the past year was reported in AUD individuals. Polysubstance abuse was associated with greater severity and comorbid psychopathology [64].
Despite these high rates of comorbidity, research on treatment of comorbid conditions is lacking and no standard clinical treatment protocols exist [65]. Thus, our study responds to an urgent clinical need, with results suggesting that as-needed nalmefene provides an important new option for use in real-world clinical settings, where comorbid conditions are common [66, 67].
Treatment with nalmefene also significantly reduced craving levels in AUD subjects with and without psychiatric comorbidity. This result sheds further light on the mechanisms by which nalmefene may lead to reduced drinking. Craving is a core feature of addiction in general, and is putatively related to the motivation to consume alcohol [12]. Craving is widely thought to play a crucial role both in the transition from controlled drinking to AUD and in the mechanism underlying relapse [68,69,70]. Furthermore, the efficacy of opioid antagonists in AUD involves opioidergic modulation of the mesolimbic dopaminergic circuitry, with diminished urges to engage in drinking and longer periods of abstinence [34, 71]. Nalmefene is thought to reduce the reinforcing effects of alcohol, thereby helping to decrease alcohol consumption. Therefore, a reduction in craving levels after consuming alcohol has obvious benefits in subjects attempting to curtail or cease their drinking [72].
It is noteworthy that in AUD patients with comorbid psychiatric disorders, reduction in alcohol craving levels was more gradual: AUD patients without comorbidity obtained significantly lower scores on craving scales at the 4-week follow-up visit, while the downward trend in craving levels was comparable in the two groups from week 8 onwards. This finding appears to be consistent with data demonstrating the negative impact of comorbidity on the course of AUD (i.e. prolonged withdrawal symptoms) [73, 74]. This observation may help guide clinicians working in naturalistic treatment settings with comorbid AUD patients, who will likely exhibit a slower treatment response.
Despite the harmful effects of AUD, retention in treatment represents a protective factor against death, suggesting that strategies supporting primary medical and social care may effectively reduce premature mortality [75]. Subjects included in our sample had not responded to previous interventions for alcohol dependence and/or alcohol withdrawal. Nalmefene does not require patients to achieve and maintain complete abstinence, but rather aims at reducing alcohol consumption. Reduction of TAC is associated with reduced risk of morbidity and mortality: any reduction in alcohol consumption for a person who consumes more than 10 g of alcohol per day will reduce the annual and lifetime risk of alcohol-related mortality [31, 76]. The introduction of pharmacologically-supported reduced-risk drinking interventions may ultimately narrow the treatment gap and reduce relapse rates [77]. Also, the as-needed dosing regimen engages AUD patients in active management of their disorder [78, 79]. Treatment with nalmefene thus addresses unmet medical needs in that it represents a possible therapeutic option for individuals with comorbid conditions and has the potential to engage AUD patients in treatment who may otherwise not have sought help [39, 80]. The latter is particularly relevant to AUD patients with comorbidity, who have higher dropout and lower adherence rates.
Limitations of the study are the relatively small sample size and the pharmacological heterogeneity in AUD subjects with comorbidity. However, the study population is as realistic as possible, thus reflecting real-world clinical practice. Future studies should replicate our preliminary results and focus on evaluating treatments that combine pharmacological [81], behavioral and alternative interventions to optimize treatment efficacy in comorbid AUD patients.
Conclusion
Our findings suggest that nalmefene represents a valid therapeutic option in reducing alcohol intake and craving in AUD patients with and without stabilized psychiatric comorbidity. Obtaining a reduction in alcohol consumption might serve as an ‘intermediate’ goal in patients unable to reach complete abstinence, thereby narrowing the treatment gap and reducing relapse rates.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorder. 5th ed. Arlington: American Psychiatric Publishing; 2013.
Roerecke M, Rehm J. Alcohol use disorders and mortality: a systematic review and meta-analysis. Addiction. 2013;108:1562–78.
Shield KD, Rehm J, Gmel G, Rehm MX, Allamani A. Alcohol consumption, alcohol dependence, and related mortality in Italy in 2004: effects of treatment-based interventions on alcohol dependence. Subst Abuse Treat Prev Policy. 2013;8:21.
Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21:655–79.
Laramée P, Kusel J, Leonard S, Aubin HJ, François C, Daeppen JB. The economic burden of alcohol dependence in Europe. Alcohol Alcohol. 2013;48:259–69.
Rehm J, Anderson P, Barry J, et al. Prevalence of and potential influencing factors for alcohol dependence in Europe. Eur Addict Res. 2015;21(1):6–18.
Schuckit MA. Alcohol-use disorders. Lancet. 2009;37:492–501.
Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82:858–66.
Merkx MJ, Schippers GM, Koeter MW, et al. Guidelines for allocating outpatient alcohol abusers to levels of care: predictive validity. Addict Behav. 2011;36:570–5.
Grant B, Stinson F, Dawson D, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16.
Hasin DS, Stinson FS, Ogbum E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Di Nicola M, Tedeschi D, De Risio L, et al. Co-occurrence of alcohol use disorder and behavioral addictions: relevance of impulsivity and craving. Drug Alcohol Depend. 2015;148:118–25.
Hatzigiakoumis DS, Martinotti G, Di Giannantonio M, Janiri L. Anhedonia and substance dependence: clinical correlates and treatment options. Front Psychiatry. 2011;2:10.
Carano A, De Berardis D, Campanella D, et al. Alexithymia and suicide ideation in a sample of patients with binge eating disorder. J Psychiatr Pract. 2012;18:5–11.
Martinotti G, Di Nicola M, De Vita O, et al. Low-dose topiramate in alcohol dependence: a single-blind, placebo-controlled study. J Clin Psychopharmacol. 2014;34:709–15.
Di Nicola M, Martinotti G, Tedeschi D, et al. Pregabalin in outpatient detoxification of subjects with mild-to-moderate alcohol withdrawal syndrome. Hum Psychopharmacol. 2010;25:268–75.
Martinotti G, Di Nicola M, Romanelli R, et al. High and low dosage oxcarbazepine versus naltrexone for the prevention of relapse in alcohol-dependent patients. Hum Psychopharmacol. 2007;22:149–56.
Addolorato G, Leggio L, Ferrulli A, Baclofen Study Group, et al. Dose-response effect of baclofen in reducing daily alcohol intake in alcohol dependence: secondary analysis of a randomized, double-blind, placebo-controlled trial. Alcohol Alcohol. 2011;46:312–7.
Maremmani AG, Bacciardi S, Rovai L, et al. Six-month outcome in bipolar spectrum alcoholics treated with acamprosate after detoxification: a retrospective study. Int J Environ Res Public Health. 2014;11:12983–96.
Martinotti G, Andreoli S, Reina D, et al. Acetyl-l-Carnitine in the treatment of anhedonia, melancholic and negative symptoms in alcohol dependent subjects. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:953–8.
Stedman M, Pettinati HM, Brown ES, Kotz M, Calabrese JR, Raines S. A double-blind, placebo-controlled study with quetiapine as adjunct therapy with lithium or divalproex in bipolar I patients with coexisting alcohol dependence. Alcohol Clin Exp Res. 2010;34:1822–31.
Janiri L, Martinotti G, Di Nicola M. Aripiprazole for relapse prevention and craving in alcohol-dependent subjects: results from a pilot study. J Clin Psychopharmacol. 2007;27:519–20.
Geoffroy PA, Goddefroy G, Rolland B, Cottencin O. Efficacy of aripiprazole in comorbid addiction in bipolar disorder. CNS Neurosci Ther. 2012;18:359–60.
Bischof G, Rumpf HJ, Meyer C, Hapke U, John U. Influence of psychiatric comorbidity in alcohol-dependent subjects in a representative population survey on treatment utilization and natural recovery. Addiction. 2005;100:405–13.
Burns L, Teesson M, O’Neill K. The impact of comorbid anxiety and depression on alcohol treatment outcomes. Addiction. 2005;100:787–96.
Boschloo L, van den Brink W, Penninx BW, Wall MM, Hasin DS. Alcohol-use disorder severity predicts first-incidence of depressive disorders. Psychol Med. 2012;42:695–703.
National Institute for Health and Clinical Excellence: Guidance. European Medicines Agency. Guideline on the development of medicinal products for the treatment of alcohol dependence. 2010.
European Medicines Agency Guidelines: the development of medicinal products for the treatment of alcohol dependence. 2010.
Gastfriend DR, Garbutt JC, Pettinati HM, et al. Reduction in heavy drinking as a treatment outcome in alcohol dependence. J Subst Abuse Treat. 2007;33(1):71–80.
Roerecke M, Gual A, Rehm J. Reduction of alcohol consumption and subsequent mortality in alcohol use disorders: systematic review and meta-analyses. J Clin Psychiatry. 2013;74:1181–9.
Rehm J, Allamani A, Aubin HJ, et al. People with alcohol use disorders in specialized care in eight different European countries. Alcohol Alcohol. 2015;50:310–8.
European Medicines Agency. Selincro (nalmefene): EU summary of product characteristics. 2013.
Biggio G. Neurobiology of alcohol and pharmacological aspects of nalmefene. Riv Psichiatr. 2015;50:19–27.
Rose JH, Karkhanis AN, Steiniger-Brach B, Jones SR. Distinct Effects of nalmefene on dopamine uptake rates and kappa opioid receptor activity in the nucleus accumbens following chronic intermittent ethanol exposure. Int J Mol Sci. 2016;17:E1216.
Gual A, He Y, Torup L, van den Brink W, Mann K. A randomised, double-blind, placebo controlled, efficacy study of nalmefene, as needed use, in patients with alcohol dependence. Eur Neuropsychopharm. 2013;23:1432–42.
Mann K, Bladström A, Torup L, Gual A, van den Brink W. Extending the treatment options in alcohol dependence: a randomized controlled study of as-needed nalmefene. Biol Psychiatry. 2013;73:706–13.
van den Brink W, Aubin H-J, Bladström A, Torup L, Gual A, Mann K. Efficacy of as-needed nalmefene in alcohol-dependent patients with at least a high drinking risk level: results from a subgroup analysis of two randomized controlled 6-month studies. Alcohol Alcohol. 2013;48:570–8.
Soyka M, Mutschler J. Treatment-refractory substance use disorder: focus on alcohol, opioids, and cocaine. Prog Neuropsychopharmacol Biol Psychiatry. 2016;70:148–61.
Mann K, Torup L, Sørensen P, et al. Nalmefene for the management of alcohol dependence: review on its pharmacology, mechanism of action and meta-analysis on its clinical efficacy. Eur Neuropsychopharmacol. 2016; Nov 12 [Epub ahead of print].
Sinclair JM, Chambers SE, Shiles CJ, Baldwin DS. Safety and tolerability of pharmacological treatment of alcohol dependence: comprehensive review of evidence. Drug Saf. 2016;39:627–45.
First MB, Spitzer RL, Gibbon M, Williams BW, Benjamin L. Structured clinical interview for DSM-IV Axis II personality disorders (SCID-II). New York: Biometrics Research Department, New York State Psychiatric Institute; 1990.
First MB, Spitzer RL, Gibbon M, Williams JB. 1995. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P, Version 2.0). Biometrics Research Department, New York State Psychiatric Institute, New York.
Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: RZ Litten, RZ Allen, eds. Measuring alcohol consumption: psychosocial and biological methods. Humana Press. New Jersey: Humana;1 992:41–72.
Overall JE, Gorham DR. The brief psychiatric rating scale. Psycol Rep. 1962;10:799.
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Young R, Biggs J, Ziegler V, Meyer D. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35.
Guy W. ECDEU Assessment Manual for Psychopharmacology. Revised; 1976. DHEW Publication No. (ADM), pp 76–338.
Janiri L, Calvosa F, Dario T, et al. The Italian version of the Obsessive-compulsive drinking scale: validation, comparison with the other versions, and difference between type 1- and type 2-like alcoholics. Drug Alcohol Depend. 2004;74:187–95.
Mottola CA. Measurement strategies: the visual analogue scale. Decubitus. 1993;6:56–8.
Starosta AN, Leeman RF, Volpicelli JR. The BRENDA model: integrating psychosocial treatment and pharmacotherapy for the treatment of alcohol use disorders. J Psychiatr Pract. 2006;12:80–9.
Drake RE, Mueser KT. Co-occurring alcohol use disorder and schizophrenia. Alcohol Res Health. 2002;26:99–102.
Merikangas KR, Herrell R, Swendsen J, Rössler W, Ajdacic-Gross V, Angst J. Specificity of bipolar spectrum conditions in the comorbidity of mood and substance use disorders: results from the Zurich cohort study. Arch Gen Psychiatry. 2008;65:47–52.
Di Florio A, Craddock N, van den Bree M. Alcohol misuse in bipolar disorder. A systematic review and meta-analysis of comorbidity rates. Eur Psychiatry. 2014;29:117–24.
Salloum IM, Cornelius JR, Daley DC, Kirisci L, Himmeloch JM, Thase ME. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2005;62:37–45.
Cardoso BM, Kauer SM, Dias VV, Andreazza AC, Cereser KM, Kapczinski F. The impact of comorbid alcohol use in bipolar patients. Alcohol. 2008;42:451–7.
van Zaane J, van den Brink W, Draisma S, Smit JH, Nolen WA. The effect of moderate and excessive alcohol use on the course and outcome of patients with bipolar disorders: a prospective cohort study. J Clin Psychiatry. 2010;71:885–93.
Moran P. Dangerous severe personality disorder-bad tidings from the UK. Int J Soc Psychiatry. 2002;48(1):6–10.
Trull TJ, Sher KJ, Minks-Brown C, Durbin J, Burr R. Borderline personality disorder and substance use disorders: a review and integration. Clin Psychol Rev. 2000;20:235–53.
Verheul R, Kranzler HR, Poling J, Tennen H, Ball S, Rounsaville BJ. Axis I and Axis II disorders in alcoholics and drug addicts: fact or artifact? J Stud Alcohol. 2000;61:101–10.
Hasin D, Fenton MC, Skodol A, et al. Personality disorders and the 3-year course of alcohol, drug, and nicotine use disorders. Arch Gen Psychiatry. 2011;68:1158–67.
Marquenie LA, Schadé A, van Balkom AJ, et al. Origin of the comorbidity of anxiety disorders and alcohol dependence: findings of a general population study. Eur Addict Res. 2007;13:39–49.
Moss HB, Goldstein RB, Chen CM, Yi HY. Patterns of use of other drugs among those with alcohol dependence: associations with drinking behavior and psychopathology. Addict Behav. 2015;50:192–8.
Jonas DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings. A systematic review and meta-analysis. JAMA. 2014;311:1889–900.
van Amsterdam J, van den Brink W. Reduced-risk drinking as a viable treatment goal in problematic alcohol use and alcohol dependence. J Psychopharmacol. 2013;27:987–97.
Maremmani I, Presta S, Petracca A, et al. Nalmefene: clinical and real world evidence in the treatment of alcohol dependence. J Psychopathol. 2014;20:80–91.
Sinha R, Li CS. Imaging stress- and cue-induced drug and alcohol craving: association with relapse and clinical implications. Drug Alcohol Rev. 2007;26:25–31.
Heinz A, Beck A, Grüsser SM, Grace AA, Wrase J. Identifying the neural circuitry of alcohol craving and relapse vulnerability. Addict Biol. 2009;14:108–18.
Martinotti G, Di Nicola M, Tedeschi D, et al. Craving typology questionnaire (CTQ): a scale for alcohol craving in normal controls and alcoholics. Compr Psychiatry. 2013;54:925–32.
Keating GM. Nalmefene: a review of its use in the treatment of alcohol dependence. CNS Drugs. 2013;27:761–72.
Koob JF. The dark side of emotion: the addiction perspective. Eur J Pharmacol. 2015;753:73–87.
Pettinati HM, O’Brien CP, Dundon WD. Current status of co-occurring mood and substance use disorders: a new therapeutic target. Am J Psychiatry. 2013;170:23–30.
Pettorruso M, De Risio L, Di Nicola M, et al. Allostasis as a conceptual framework linking bipolar disorder and addiction. Front Psychiatry. 2014;5:173.
Morandi G, Periche Tomas E, Pirani M. Mortality risk in alcoholic patients in Northern Italy: comorbidity and treatment retention effects in a 30-year follow-up study. Alcohol Alcohol. 2016;51:63–70.
Nutt DJ, Rehm J. Doing it by numbers: a simple approach to reducing the harms of alcohol. J Psychopharmacol. 2014;28:3–7.
Aubin HJ, Daeppen JB. Emerging pharmacotherapies for alcohol dependence: a systematic review focusing on reduction in consumption. Drug Alcohol Depend. 2013;133:15–29.
Korpi ER, Linden AM, Hytönen HR, et al. Continuous delivery of naltrexone and nalmefene leads to tolerance in reducing alcohol drinking and to supersensitivity of brain opioid receptors. Addict Biol. 2016; Mar 15 [Epub ahead of print].
Soyka M. Nalmefene for the treatment of alcohol use disorders: recent data and clinical potential. Expert Opin Pharmacother. 2016;17:619–26.
Echeverry-Alzate V, Giné E, et al. Nalmefene is effective at reducing alcohol seeking, treating alcohol-cocaine interactions and reducing alcohol-induced histone deacetylases gene expression in blood. Br J Pharmacol. 2016;173:2490–505.
Caputo F, Maremmani AG, Addolorato G, et al. Sodium oxybate plus nalmefene for the treatment of alcohol use disorder: a case series. J Psychopharmacol. 2016;30:402–9.
Acknowledgements
No funding or sponsorship was received for this study. Article processing charges were funded by Lundbeck Italia S.P.A. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosures
Marco Di Nicola, Sergio De Filippis, Giovanni Martinotti, Luisa De Risio, Mauro Pettorruso, Simone De Persis, Angelo Giovanni Icro Maremmani, Icro Maremmani, Massimo di Giannantonio and Luigi Janiri have nothing to disclose.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008. Informed consent was obtained from all patients before being included in the study.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/AC18F06001B81D16.
Rights and permissions
About this article
Cite this article
Di Nicola, M., De Filippis, S., Martinotti, G. et al. Nalmefene in Alcohol Use Disorder Subjects with Psychiatric Comorbidity: A Naturalistic Study. Adv Ther 34, 1636–1649 (2017). https://doi.org/10.1007/s12325-017-0546-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-017-0546-3