Abstract
Mirabegron (YM178, Myrbetriq™, Betanis®, Betmiga™) is a β3-adrenergic receptor agonist approved in several countries for the symptomatic treatment of adults with overactive bladder syndrome. In three 12-week, randomized, double-blind, placebo-controlled, multinational trials in patients with overactive bladder syndrome, oral mirabegron 25 or 50 mg once daily significantly reduced the adjusted mean number of incontinence episodes per 24 h (in patients with incontinence at baseline) and the adjusted mean number of micturition episodes per 24 h (in full trial populations) [coprimary endpoints]. Across trials, mirabegron 50 mg once daily also consistently significantly reduced urgency episodes and increased the volume of urine voided per micturition, generally in association with improved health-related quality of life (HR-QOL) and treatment satisfaction. Based on descriptive analyses from a 12-month trial, once-daily mirabegron 50 mg and tolterodine extended-release (ER) 4 mg were both efficacious in reducing urinary symptoms and improving HR-QOL. Mirabegron was generally well tolerated in the trials. Over 12 weeks, the adverse event rate with mirabegron 50 mg once daily was similar to that with placebo. During 12 months of treatment, 2.8 % of mirabegron 50 mg once daily recipients reported dry mouth compared with 8.6 % with tolterodine ER 4 mg once daily recipients. Mirabegron 50 mg once daily carries a low risk of QT interval prolongation. Thus, mirabegron is an efficacious new treatment for overactive bladder syndrome with a favourable tolerability profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
First β3-adrenergic receptor agonist to be approved for the treatment of overactive bladder syndrome |
Long half-life after oral administration, making it suitable for once-daily dosing |
Well tolerated and more efficacious than placebo in randomized trials in patients with overactive bladder syndrome |
Trials comparing mirabegron with antimuscarinics in overactive bladder syndrome would be of interest |
1 Introduction
The central clinical features of overactive bladder syndrome are urinary urgency, with or without urgency incontinence, usually accompanied by frequency and nocturia, according to an International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on female pelvic floor dysfunction [1]. As these symptoms are non-specific and overlap with other medical conditions, in order to meet the IUGA/ICS definition for overactive bladder syndrome, they must occur in the absence of urinary tract infection or other obvious pathology [1].
Overactive bladder syndrome is a common impairing condition with a negative impact on quality of life and is associated with an increased risk of depression, sleep disturbances, skin infections, falls and fractures [2]. In a 2005 population-based survey of adults aged ≥18 years in Canada and four European countries, 12.8 % of women and 10.8 % of men reported the lower urinary tract symptoms that define overactive bladder syndrome [3]. In an earlier population-based survey conducted in six European countries, 16.6 % of adults aged ≥40 years had symptoms suggestive of overactive bladder syndrome, with symptoms mostly of a chronic nature [4]. The prevalence of these symptoms increased with age, from 3.4 and 8.7 % in men and women aged 40–44 years to 41.9 and 31.3 % in those aged ≥75 years [4]. Approximately two-thirds of respondents with these symptoms reported that their condition affected their daily living [4].
The precise aetiology of overactive bladder syndrome is unknown, but it is thought that a combination of neurogenic, myogenic or unknown factors cause overactivity of the detrusor muscle, producing bladder dysfunction during voiding, although 30–50 % of patients with storage symptoms of overactive bladder syndrome do not exhibit detrusor muscle overactivity when tested in the laboratory [5]. The important efferent neural pathways to the detrusor muscle that are involved in bladder filling and emptying are the parasympathetic nerves, sympathetic nerves and somatic nerves, which mediate conscious control of voiding [5].
Recommended first-line treatments for overactive bladder syndrome include bladder and pelvic floor retraining, dietary modifications, such as reduced fluid and caffeine intake, and antimuscarinics, which are considered the mainstay of medical management [6]. Antimuscarinics (e.g. tolterodine, solifenacin, darifenacin, oxybutynin) increase bladder relaxation through antagonism of muscarinic M2 receptors and reduce bladder contraction through antagonism of M3 receptors [2]. Several meta-analyses of placebo-controlled trials of antimuscarinics in overactive bladder syndrome indicate that they are well tolerated and efficacious in improving symptoms [6]. The meta-analyses also show that there is a substantial placebo response [6]. The most frequently occurring adverse effects of antimuscarinics are dry mouth and constipation, which can lead to drug discontinuation in some patients [6]. More serious adverse effects include cognitive functioning deficits or confusion in the elderly and cardiovascular changes, although the risk of developing these varies according to the receptor selectivity of the individual drug [2, 6].
Several classes of drugs with differing modes of action are under investigation in overactive bladder syndrome, based on an improved understanding of the complexity of bladder filling and emptying [2, 6, 7]. These include β3-adrenergic receptor agonists (e.g. mirabegron, amibegron, solabegron) aimed at relaxing the detrusor muscle; inhibitors of tachykinin-mediated bladder-spinal reflex signaling (e.g. neurokinin-1 receptor antagonists, such as aprepitant); and drugs that desensitize vanilloid-sensitive receptors on afferent C fibres in the bladder (e.g. resiniferatoxin) [2, 6, 7].
Mirabegron (YM178, Myrbetriq™, Betanis®, Betmiga®) (Fig. 1) is the first β3-adrenergic receptor agonist to receive approval for use in overactive bladder syndrome. It is approved in the USA [8] and Japan [9], and more recently in the EU [10] and Canada [11], for the symptomatic treatment of urgency, increased micturition frequency and/or urgency incontinence occurring in adults with overactive bladder syndrome [10]. This article provides a narrative review of the literature on mirabegron, providing first an overview of its pharmacology followed by a detailed discussion of its efficacy and tolerability in patients with overactive bladder syndrome. Phase I–III clinical studies of mirabegron in patients with overactive bladder syndrome have included mirabegron dosages in the range of 25–300 mg/day. The discussion in this article focuses chiefly on the 25 and 50 mg once-daily dosages, although where relevant, data for other mirabegron dosages are also presented.
Sources:
Medical literature (including published and unpublished data) on mirabegron in patients with overactive bladder syndrome was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated 31 May 2013], bibliographies from published literature, clinical trial registries/databases and websites (including those of regional regulatory agencies and the manufacturer). Additional information (including contributory unpublished data) was also requested from the company developing the drug.
Search terms: mirabegron, overactive bladder, urinary bladder, overactive.
Study selection: Studies in patients with overactive bladder syndrome who received mirabegron. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Keywords: Mirabegron, β3-adrenergic receptor agonist, overactive bladder syndrome.
2 Pharmacodynamic Properties
Data in this section are from a review of β3-adrenergic receptors in human detrusor muscle [12], clinical studies [13–15] and a placebo- and active treatment-controlled thorough QT study in healthy adults [16], with supplemental information from the EU Summary of Product Characteristics (SPC) [10].
2.1 Mechanism of Action
Mirabegron is a potent and selective β3-adrenergic receptor agonist [10], providing a contrasting mechanism of action in overactive bladder syndrome to antimuscarinics, which act on parasympathetic nerves [2]. Smooth muscle relaxation during bladder filling is dependent on sympathetic nerve activity and the release of noradrenaline [10]. β1- and β2-adrenergic receptors provide sympathetic supply to the detrusor muscle in most species, whereas β3-adrenergic receptors are the predominant β-adrenergic receptor type present in the human bladder [12]. In animal studies and in isolated human bladder tissue, mirabegron induced relaxation of smooth muscle [10]. Thus, it appears that the positive treatment effects observed with mirabegron result from enhanced detrusor muscle relaxation allowing for a greater bladder capacity and reduced frequency of micturition. Importantly, as demonstrated in rats with partial urethral obstruction and in humans with bladder obstruction (Sect. 2.2), mirabegron does not inhibit bladder emptying, which is predominantly under parasympathetic control [10].
2.2 Urodynamics
The urodynamic effects of oral mirabegron were evaluated in men aged ≥45 years with lower urinary tract symptoms and bladder outlet obstruction (n = 200) [data are available from an abstract [13]]. Patients were randomized to mirabegron 50 or 100 mg/day or placebo for 12 weeks; coprimary endpoints were the change from baseline to 12 weeks in the maximum urinary flow rate (Qmax) and in detrusor muscle pressure at Qmax (PdetQmax) [13].
Mirabegron met prespecified criteria for noninferiority to placebo for both Qmax (lower limit of 95 % CI for the treatment difference of <3 mL/s) and PdetQmax (lower limit of 95 % CI for the treatment difference of <15 cms H2O), indicating that there were no negative effects on voiding. The adjusted mean changes in Qmax (95 % CI for the difference from placebo) were 0.07 (−0.63 to 1.42), 0.30 (−0.43 to 1.68) and −0.33 mL/s in the mirabegron 50 mg/day, mirabegron 100 mg/day and placebo groups, respectively; corresponding PdetQmax values were −3.03 (−13.98 to 2.09), 1.53 (−9.73 to 6.96) and 2.92 cms H2O [13].
There was also no negative effect on bladder contractility, as there were no between-group differences in adjusted mean changes from baseline in the Bladder Contractility Index [13]. In the mirabegron 100 mg/day group, there was a significant (p < 0.05) difference in the change from baseline to 12 weeks in the adjusted mean post-void urine volume [13]; adjusted mean changes were 17.9, 30.8 and 0.6 mL in mirabegron 50 and 100 mg/day and placebo groups, respectively [10].
2.3 Urinary Symptoms in Patients with Overactive Bladder Syndrome
The effects of different dosages of oral mirabegron on urinary symptoms in male and female patients aged ≥18 years with overactive bladder syndrome were evaluated in randomized, double-blind studies, including a proof-of-concept study (n = 255) [14] and a dose-ranging study (n = 919) [15]. In both studies, ≥81 % of included patients were women [14, 15].
In the primary analysis in the proof-of-concept study, mirabegron 100 or 150 mg twice daily for 4 weeks was associated with significantly (p < 0.05) greater reductions in the mean micturition frequency per 24 h than placebo; there was no difference between the mirabegron dosage groups on this endpoint [14]. Mirabegron 100 mg was also associated with significantly greater improvements than placebo on most secondary efficacy endpoints [14].
In the dose-ranging study, after 12 weeks of randomized treatment, the changes from baseline in the mean number of micturitions per 24 h (primary endpoint) were −1.9, −2.1, −2.1 and −2.2 in the mirabegron 25, 50, 100 and 200 mg once-daily dosage groups, respectively, and was −1.4 in the placebo group (p < 0.05 vs. placebo for mirabegron 50, 100 and 200 mg once-daily dosages) [15]. Mirabegron was generally significantly more efficacious than placebo based on changes from baseline in secondary urinary endpoints. For instance, mirabegron 50 mg once daily resulted in significantly greater reductions in incontinence, urgency incontinence and nocturia episodes per 24 h (p < 0.05 or p < 0.01) and a significant (p < 0.001) increase in the mean volume of urine voided per micturition, but not in urgency episodes per 24 h or level of urgency per micturition over 24 h [15]. Dosages of mirabegron 25, 50 and 100 mg once daily were evaluated further in phase III trials (Sect. 4).
2.4 Effects on the QT Interval
In a thorough QT study, healthy adults (n = 317) were administered once-daily oral mirabegron 50, 100 or 200 mg or placebo for 10 days, or moxifloxacin 400 mg as a single dose on day 10, in a two-way crossover design [16]. QT interval changes were assessed using an individual subject-specific correction formula (QTcI) with adaptation for heart rate hysteresis [16].
Higher dosages of mirabegron were associated with greater changes in the time-matched, baseline-adjusted mean QTcI, with a greater effect in females than males [16]. However, at the recommended maximum dosage of 50 mg once daily, or at 100 mg once daily, there was no evidence of QTc interval prolongation with mirabegron [16]. In both men and women at mirabegron dosages of 50 or 100 mg once daily, the upper bound of the one-sided 95 % CI for the change in QTcI was <10 ms at all time points, meeting the International Conference on Harmonization E14 criterion for a negative study. In women, mirabegron 200 mg once daily was associated with QTcI changes that exceeded this criterion, with the upper bound of the 95 % CI generally >10 ms from 0.5 to 6 h post dose and at 10 h post dose. In men, even at these supra-therapeutic dosages, the change in QTcI remained within the E14 criterion [16].
However, caution is needed when administering mirabegron to patients with a history of QT interval prolongation or who are receiving medications that cause QT interval prolongation, as there are no mirabegron studies in such patients [10]. The effects of mirabegron on the QT interval in patients with overactive bladder syndrome are discussed in Sect. 5.2.
3 Pharmacokinetic Properties
The data reported in this section are from the EU SPC [10] and pharmacokinetic studies in healthy adults [17–19], patients with renal or hepatic impairment [20], poor or extensive hepatic cytochrome P450 (CYP) 2D6 metabolizers (available as an abstract [21]) and from drug interaction studies (available as abstracts [22–25]). For illustrative purposes, Table 1 shows values for pharmacokinetic parameters from a randomized, open-label, two-way crossover study in healthy adults aged 18–45 years and ≥55 years, in which subjects received two of three oral mirabegron dosage regimens (25, 50 or 100 mg twice daily on day 1 and then once daily on days 2–7) during two treatment periods [17]. Data shown are for mirabegron 50 mg once daily [17].
3.1 Absorption and Distribution
After oral administration, mirabegron was readily absorbed with a mean time to reach maximum concentration (Cmax) of approximately 3–4 h [10]. The absorption of mirabegron was more than dose proportional. For example, compared with a dose of mirabegron 50 mg, the mean mirabegron Cmax and area under the concentration-time curve (AUC) values during a dosing interval (AUCτ) were 2.9- and 2.6-fold higher after a 100 mg dose and 8.4- and 6.5-fold higher after a 200 mg dose. After continued once-daily administration, steady state was reached within 7 days, with mirabegron plasma exposure approximately twofold higher than after a single dose [10].
Administration of mirabegron 50 mg with a low-fat meal was associated with a 75 % reduction in the mirabegron Cmax and a 51 % reduction in the AUC, whereas administration with a high-fat meal reduced the Cmax by 45 % and the AUC by 17 % [10]. Mirabegron can be taken with or without food, as was the case in the clinical trials that evaluated its efficacy (Sect. 4).
At steady state, the volume of distribution of mirabegron was 1,670 L, indicating that it is widely distributed in the body [10, 19]. Mirabegron is approximately 71 % bound to human plasma proteins and has moderate affinity for albumin and α1-acid glycoprotein [10].
3.2 Metabolism and Elimination
Mirabegron metabolism involves multiple pathways, including amide hydrolysis, glucuronidation, and N-dealkylation or oxidation of secondary amines [10, 18]. Mirabegron metabolites are inactive and mirabegron is the main circulating component, based on evaluation following a single radiolabelled dose of mirabegron [10].
CYP2D6 and CYP3A4 enzymes play a limited role in oxidative metabolism [10]. Based on a pharmacokinetic study in healthy men who were CYP2D6 poor (n = 8) or extensive (n = 8) metabolizers, CYP2D6 polymorphisms are unlikely to be associated with clinically important differences in mirabegron exposure, as there were only slight differences in pharmacokinetic parameters between poor and extensive metabolizers [21]. No dose adjustment is required in CYP2D6 poor metabolizers [10].
The renal and total body clearances of mirabegron from plasma were ≈13 and 57 L/h and the terminal elimination half-life (t½) was ≈50 h [10]. Renal clearance, primarily via active tubular secretion, accounts for nearly 25 % of total clearance and is dose-dependent [10]. After administration of radiolabelled mirabegron, ≈55 % of the radioactivity was recovered in the urine and 34 % in the faeces [18]. Overall, 45 % of the radioactivity detected in the urine was as unchanged drug, with one or more of the mirabegron metabolites making up the remainder of the radioactivity in the urine [18].
3.3 Special Populations
The absorption pharmacokinetics of mirabegron were similar in young and older patients and were unaffected by race, but the mirabegron Cmax and AUC were approximately 40–50 % higher in women than men [10]. However, no mirabegron dosage adjustment on the basis of age or sex or racial background is recommended [10].
In patients with mild renal impairment (estimated glomerular filtration rate based on the abbreviated modification of diet in renal disease formula [eGFR-MDRD] 60–89 mL/min/1.73 m2), there were 6 and 31 % increases in mirabegron Cmax and AUC in comparison with adults with normal renal function [20]. The mirabegron Cmax and AUC were increased by 23 and 66 % in patients with moderate renal impairment (eGFR-MDRD of 30–59 mL/min/1.73 m2) and by 92 and 118 % in patients with severe renal impairment (eGFR-MDRD of 15–29 mL/min/1.73 m2) [20]. There are no studies of mirabegron in end-stage renal disease or in patients requiring dialysis [10]. See Sect. 6 for dose restrictions in patients with renal impairment.
Compared with adults with normal hepatic functioning, after a single dose of mirabegron, the mirabegron Cmax and AUC were increased by 9 and 19 % in patients with mild hepatic impairment (Child-Pugh classification 5–6) and by 175 and 65 % in patients with moderate hepatic impairment (Child-Pugh classification 7–9) [20]. There are no studies of mirabegron in patients with severe hepatic impairment [10]. See Sect. 6 for dose restrictions in patients with hepatic impairment.
3.4 Drug Interactions
In vitro, mirabegron was not associated with clinically relevant inhibition of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19 or CYP2E1 enzymes and did not induce CYP1A2 or CYP3A enzymes [10]. However, mirabegron is a moderate, time-dependent CYP2D6 inhibitor and a weak CYP3A inhibitor [10]. A single dose of mirabegron 100 mg administered to healthy men and women (n = 24) after multiple doses of ketoconazole (a strong CYP3A4 and P-glycoprotein [P-gp] inhibitor) was associated with a 1.4-fold increase in the mirabegron Cmax and a 1.8-fold increase in the AUC from time 0 to infinity, indicating only weak inhibitory effects of ketoconazole on mirabegron clearance [23].
Compared with mirabegron alone, multiple doses of rifampicin (rifampin) [a strong CYP3A4 inducer] followed by a single dose of mirabegron 100 mg in healthy men and women (n = 24) led to 35 and 44 % reductions in the geometric mean ratios of mirabegron Cmax and AUC, indicating a moderate reduction in mirabegron systemic exposure [24]. No dosage reduction is required when mirabegron is coadministered with CYP3A inducers [10].
Coadministration of desipramine (a CYP2D6 substrate) with mirabegron in healthy male and female extensive CYP2D6 metabolizers (n = 28) resulted in 1.8- and 3.4-fold increases in the desipramine Cmax and AUC and prolonged the desipramine t½ [22]. Coadministration of mirabegron with a single dose of metoprolol (also a CYP2D6 substrate) increased the metoprolol Cmax and AUC by 90 and 229 % [10]. These findings are consistent with mirabegron being a moderate inhibitor of CYP2D6. Therefore, caution is needed if mirabegron is to be used concomitantly with CYP2D6 substrates that are individually dose-titrated and with drugs that have a narrow therapeutic window and that are extensively metabolized by CYP2D6 enzymes, including tricyclic antidepressants (e.g. imipramine, desipramine), thioridazine, and type 1C antiarrhythmics (e.g. flecainide acetate, propafenone) [10]. However, no dose adjustment is required when mirabegron is coadministered with other CYP2D6 inhibitors [10].
In preclinical studies, mirabegron was associated with reductions in plasma glucose levels [25]. In healthy men (n = 16) who were administered mirabegron concomitantly with the oral hypoglycaemic metformin, there were no clinically relevant changes in metformin pharmacokinetic parameters or in fasting plasma glucose levels [25].
Caution is required if mirabegron is used concomitantly with drugs such as digoxin and dabigatran that are substrates of P-gp, as mirabegron is a weak inhibitor of P-gp [10]. If digoxin is to be administered concomitantly with mirabegron, it should be initiated at the lowest possible dose and serum digoxin concentrations monitored closely as the digoxin dose is titrated upwards to achieve the desired clinical effect [10].
No clinically important interactions were observed when mirabegron was co-administered with warfarin, solifenacin or tamsulosin at therapeutic dosages, or with the combined oral contraceptive ethinyl estradiol/levonorgestrel [10].
4 Therapeutic Efficacy
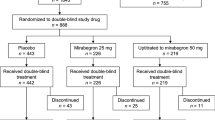
The efficacy of oral mirabegron was evaluated in 12-week, randomized, double-blind, placebo-controlled trials, conducted in Europe and Australia (Study 046) [26], the USA and Canada (Study 047) [27] and Europe, the USA and Canada (Study 074) [28] (Sect. 4.1). A further randomized, double-blind, active treatment-controlled, multinational trial evaluated the safety and efficacy of mirabegron over 12 months, with the evaluation of efficacy being a secondary objective (Study 049) [29] (Sect. 4.2). Further analyses of the placebo-controlled trials include a prespecified pooled analysis of the 12-week trials that included evaluation of the efficacy of mirabegron in patients with or without prior exposure to antimuscarinics [30], a post hoc analysis of Study 046 that included patients who had previously discontinued antimuscarinics because of insufficient benefit (data are from the EU SPC) [10], and a post hoc pooled analysis of the 12-week trials restricted to patients aged ≥65 years (data are from an abstract) [31].
Included patients were men or women aged ≥18 years with symptoms of overactive bladder syndrome for at least 3 months; patients were required to have on average ≥8 micturition episodes per 24 h and ≥3 urgency episodes over a 3-day period [26–29]. Key exclusion criteria were clinically relevant stress incontinence, or mixed stress/urgency incontinence if stress was the predominant factor, mean daily urinary volume >3,000 mL, other specified bladder or pelvic conditions, risk of bladder outflow obstruction, severe hypertension and other relevant medical conditions or laboratory test disturbances. Patients underwent a 2-week, single-blind, placebo run-in [26–29].
Patients meeting inclusion/exclusion criteria after the run-in period were randomized to 12 weeks of treatment with once-daily mirabegron 50 or 100 mg, placebo or tolterodine extended-release (ER) 4 mg (Study 046) [26], mirabegron 50 or 100 mg or placebo (Study 047) [27] and mirabegron 25 or 50 mg or placebo (Study 074) [28]. In Study 049, patients were randomized to once-daily mirabegron 50 or 100 mg or tolterodine ER 4 mg, continued for 12 months [29].
In the 12-week trials, the coprimary endpoints were the changes from baseline in the adjusted mean number of incontinence episodes per 24 h (in patients with incontinence at baseline) and micturition episodes per 24 h, based on a patient-completed, 3-day micturition diary completed at baseline and prior to clinic visits at weeks 4, 8 and 12 [26–28]. Secondary endpoints which are unlikely to be conflated with the coprimary endpoints are also discussed. Analyses were conducted in the full analysis set (all randomized patients who took at least one dose of study drug and who completed the micturition diary at baseline and on at least one occasion post baseline) using last-observation-carried-forward imputation. Analyses included pairwise comparisons with placebo and stratified rank analysis of covariance (ANCOVA) for each pairwise comparison; adjustments for multiple tests were applied for analyses of the coprimary and key secondary endpoints [26–28]. Study 046 was powered to test for differences between the mirabegron and placebo groups; there was no statistical testing of mirabegron versus tolterodine ER [26]. In Study 049, efficacy endpoints were assessed at months 1, 3, 6, 9 and 12; all efficacy data in this study are descriptive, consisting of adjusted mean changes in endpoints from baseline to the final visit, as derived from ANCOVA models [29].
Across trials, 68–76 % of included patients were female and 87–99 % were Caucasian; the majority (60–64 %) were aged <65 years, with a mean age ranging from 58 to 60 years across treatment groups [26–29]. Baseline values for key clinical endpoints are shown in Tables 2 and 4.
4.1 Placebo-Controlled Trials
4.1.1 Urinary Symptoms
In patients with overactive bladder syndrome, oral mirabegron was efficacious in reducing both incontinence and micturition episodes over the 12-week treatment period (coprimary endpoints) [26–28]. Across all three trials, in patients with incontinence episodes at baseline, mirabegron 25 or 50 mg once daily was significantly more efficacious than placebo in reducing the adjusted mean number of incontinence episodes per 24 h from baseline (Table 2). For mirabegron 50 mg once daily, incontinence episodes were reduced by −1.4 to −1.6 per 24 h (vs. −1.0 to −1.1 with placebo). Mirabegron 25 or 50 mg once daily recipients also had significantly greater reductions in the adjusted mean number of micturition episodes than placebo recipients (Table 2). For mirabegron 50 mg once daily recipients, the adjusted mean number of micturition episodes was reduced by −1.6 to −1.9 episodes per 24 h (vs. −1.1 to −1.4 with placebo) [26–28]. In Study 046, there were no significant differences between the tolterodine ER and placebo groups in reductions in incontinence or micturition episodes [26].
Across trials, mirabegron 50 mg once daily recipients, but not 25 mg once daily recipients, had significantly greater increases in the adjusted mean urine volume voided per micturition than placebo recipients (Table 2) [26–28]. Mirabegron 50 mg once daily recipients also had consistently significantly greater reductions than placebo recipients in the adjusted mean number of micturition episodes associated with a grade 3–4 level of urgency per 24 h (Table 2) [26–28]. In Study 046, tolterodine ER 4 mg once daily recipients had significantly greater improvements than placebo recipients in these urine volume and urgency endpoints (Table 2) [26].
Approximately 50 % of patients included in the trials had received previous medications for overactive bladder [30]. Based on pre-specified pooled analyses, mirabegron was generally efficacious regardless of whether or not patients had been treated previously with antimuscarinics, although the magnitude of the mirabegron-placebo difference was less in antimuscarinic-naïve patients because of a higher placebo response in this group [30]. In patients previously treated with antimuscarinics, the adjusted mean differences from baseline (95 % CI) in the number of incontinence and micturition episodes per 24 h were −1.49 (−1.66 to −1.32) and −1.67 (−1.86 to −1.48) in the mirabegron 50 once daily group and −0.92 (−1.09 to −0.75) and −0.93 (−1.12 to −0.74) in the placebo group; the corresponding values in the antimuscarinic-naïve group were −1.50 (−1.71 to −1.29) and −1.84 (−2.04 to −1.64) in the mirabegron 50 mg once daily group and −1.35 (−1.55 to −1.14) and −1.51 (−1.71 to −1.31) in the placebo group [30].
In the post hoc analysis that included patients from Study 046 who had previously discontinued antimuscarinics because of insufficient benefit, mirabegron was an efficacious treatment [32]. For the mirabegron 50 mg once daily group (n = 105–160), the adjusted mean mirabegron-placebo differences (95 % CI) in incontinence and micturition episodes were −0.76 (−1.32 to −0.19) and −0.59 (−1.15 to −0.04) [32]. For the tolterodine ER 4 mg/day group (n = 102–155), the adjusted mean tolterodine ER-placebo differences (95 % CI) in incontinence and micturition episodes were −0.06 (−0.63 to 0.50) and −0.08 (−0.64 to 0.47) [10].
Mirabegron was also efficacious in older patients, based on the post hoc pooled analysis in patients aged ≥65 years; older patients made up ≈38 % of the pooled sample [31]. For the mirabegron 50 mg once daily group (n = 355–499), the adjusted mean differences (95 % CI) versus the placebo group (n = 345–504) were −0.66 (−0.95 to −0.37) for incontinence episodes per 24 h, and −0.62 (−0.94 to −0.30) for micturition episodes per 24 h [31].
4.1.2 Health-Related Quality of Life and Treatment Satisfaction
In general, the mirabegron groups had significantly greater improvements in health-related quality of life (HR-QOL) than the placebo groups [26–28]. Mirabegron 50 mg once daily recipients had significantly greater changes from baseline in adjusted mean Overactive Bladder Questionnaire (OAB-q) symptom bother scores (all studies [26–28]), and in the adjusted mean Patient Perception of Bladder Condition (PPBC) scores (in studies 046 [26] and 047 [27], but not Study 074 [28]) [Table 3]. In addition, in studies 046 and 047, mirabegron 50 mg once daily recipients had significantly (p < 0.05) greater changes than placebo in adjusted mean total OAB-q scores, representing a positive difference in overall HR-QOL (data are from an abstract [33]). In Study 074, there were no significant differences between the mirabegron 25 mg once daily and placebo groups in symptom bother or PPBC scores (Table 3) [28].
Across trials, mirabegron 25 or 50 mg once daily recipients had significantly greater improvements in treatment satisfaction, based on ratings on a visual analogue scale (Table 3) [26–28].
In Study 046, compared with placebo, tolterodine ER 4 mg once daily recipients also had significantly greater improvements in OAB-q symptom bother scores, PPBC scores and treatment satisfaction (Table 3) [26].
4.2 Longer-Term Treatment Over 12 Months
In descriptive analyses of a 12-month trial, oral mirabegron 50 mg once daily and the active treatment control, tolterodine ER 4 mg once daily, were both associated with improvements from baseline in the symptoms of overactive bladder syndrome and in HR-QOL and treatment satisfaction [29]. Across all treatment groups, there were reductions in the adjusted mean numbers of incontinence and micturition episodes and increases in the adjusted mean urine volume voided per micturition (all measured over 24-h time periods) [Table 4]. All groups also had reductions (i.e. improvements) in OAB-q symptom bother and PPBC scores and increases in treatment satisfaction scores (Table 4). Improvements in key symptoms of overactive bladder syndrome were evident from the first assessment at 4 weeks and maintained throughout the 12-month treatment period. As there was no placebo group in this study, it is not possible to rule out that the changes observed were unrelated to treatment [29].
5 Tolerability
The tolerability of oral mirabegron was evaluated in the randomized, controlled trials discussed in Sect. 4. The results reported here are descriptive data from Study 046 [26], which are representative of the findings of the 12-week placebo-controlled trials, and from Study 049 [29], which provides a 12-month comparison with tolterodine ER. Supplemental data are from EU SPC [10] and a pooled analysis of the placebo-controlled trials, which includes data for all mirabegron dosage groups (25, 50 and 100 mg once daily) [30]. Across studies, statistical analyses to assess the significance of between-group differences were not performed.
5.1 General
5.1.1 During 12 Weeks of Treatment
Mirabegron was well tolerated by most patients in the 12-week, placebo-controlled trials. In Study 046, treatment-emergent adverse events (TEAEs) were reported in 43, 40, 43 and 47 % of patients in the once-daily mirabegron 50 and 100 mg, placebo and tolterodine ER 4 mg groups, respectively; most TEAEs were of mild or moderate severity [26]. In the corresponding groups, 5, 3, 3 and 4 % of patients discontinued treatment because of TEAEs [26]. In the pooled analysis, 46, 19 and 4 % of mirabegron recipients (all dosages) had a TEAE, drug-related TEAEs and TEAEs leading to discontinuation, respectively; corresponding adverse event rates were 48, 17 and 3 % in the placebo group [30]. In the mirabegron, placebo and tolterodine ER groups, serious adverse events were observed in 2 % of patients in all groups [30].
Specific TEAEs occurring in ≥2 % of patients in any group in Study 046 are shown in Fig. 2a, including TEAEs of special interest which were generally defined based on results of ancillary investigations such as ECG monitoring [26]. The most common TEAEs, which occurred across the active treatment and placebo groups, were hypertension, headache, nasopharyngitis, dry mouth, influenza and arrhythmia [26]. Apart from dry mouth, which occurred in 10.1 % of tolterodine ER recipients and ≤2.8 % of patients in the mirabegron and placebo groups [26]; there were no striking between-group differences in TEAE rates, based on these numerical data. In the once-daily mirabegron 50 and 100 mg, and tolterodine ER 4 mg groups, 0.2, 0.4 and 0.2 % of patients, respectively, had post-void residual volumes of >300 mL (placebo group rates not reported) [26].
Tolerability of mirabegron in randomized, double-blind, placebo-and active treatment-controlled trials in patients with overactive bladder syndrome [26, 29]. The descriptive data shown are treatment-emergent adverse events (TEAEs) occurring in ≥2 % of patients in at least one treatment group over 12 weeks in Study 046 (a) and over 12 months in Study 049 (b). MIR mirabegron, OSI TEAE of special interest, PL placebo, TOL ER tolterodine extended-release
5.1.2 During Longer-Term Treatment
In Study 049, the tolerability findings for mirabegron followed a similar pattern to those in Study 046 [29]. Over 12 months of treatment, 60, 61 and 63 % of patients reported TEAEs in the once-daily mirabegron 50 and 100 mg and tolterodine ER 4 mg groups, respectively. Across groups, TEAEs were mostly of mild or moderate severity, with ≤6 % of patients in any group having serious adverse events and ≤6 % of patients discontinuing treatment because of TEAEs [29]. There were five deaths during the course of the study (three patients in the mirabegron 50 mg once daily group and two in the tolterodine ER group), but none were considered to be treatment-related [29].
Specific TEAEs occurring in ≥2 % of patients in any group in Study 049 are shown Fig. 2b. TEAEs that occurred in ≥4 % of mirabegron recipients were hypertension, urinary tract infection, hypersensitivity (which encompassed a wide range of allergies), nasopharyngitis, arrhythmia, headache and back pain; these TEAEs occurred at similar rates across all treatment groups [29]. Dry mouth occurred at a numerically higher rate in the tolterodine ER group (8.6 vs. ≤2.8 % in the mirabegron groups) [29].
Urinary retention as an adverse event was reported in 0.1 % of mirabegron 50 and 100 mg once daily recipients and 0.4 % of tolterodine ER 4 mg once daily recipients. Across groups, there were no reports of urinary retention as a serious adverse event; no mirabegron 50 mg once daily recipients had acute urinary retention, but one patient each in the once daily mirabegron 100 mg and tolterodine ER 4 mg groups required bladder catheterization for acute urinary retention [29].
5.2 Cardiovascular
Patients in the clinical trials were closely monitored for treatment-emergent cardiovascular events, changes in vital signs and ECG abnormalities [26, 27, 29, 34]. Table 5 shows cardiovascular adverse events of interest in patients enrolled in studies 046 [26] and 049 [29]. Despite the older age of patients in these study populations (mean age ≈60 years), cardiovascular adverse event rates were generally low across groups, with no indication of an increased rate in mirabegron recipients relative to placebo or tolterodine ER [26, 29].
In the 12-month trial, hypertension event rates were 11.0, 10.1 and 10.6 % in the once-daily mirabegron 50 or 100 mg and tolterodine ER 4 mg groups, respectively [29]; in the absence of a placebo group, the clinical significance, if any, of these data is uncertain.
In the 12-week, placebo-controlled trials, 1.2 % of mirabegron 50 mg once daily recipients had tachycardia and 0.1 % discontinued treatment because of tachycardia [10]. Compared with placebo, in mirabegron recipients, small reversible changes in pulse rate (≈1 beat per min difference) and BP (≈1 mmHg or less difference) were noted [10].
After 12 months extended treatment in Study 049, compared with baseline, mirabegron 50 and 100 mg once daily were associated with small changes in the adjusted mean pulse rate of <2 beats per minute and in adjusted mean systolic and diastolic BP of ≤0.4 mmHg [29]. Nevertheless, mirabegron is not recommended for use in patients with severe uncontrolled hypertension, as mirabegron has not been studied in this population [10].
6 Dosage and Administration
In the EU, the recommended mirabegron dosage in patients with overactive bladder syndrome is 50 mg once daily [10]. In the USA, the recommended initial dosage is mirabegron 25 mg administered orally once daily, which can be increased to 50 mg once daily based on efficacy and tolerability [8]. Mirabegron tablets should be swallowed whole with liquids, with or without food [8, 10]. As there are no efficacy or safety data in patients below the age of 18 years, mirabegron is not recommended for use in children [8, 10].
In the EU, in patients with mild or moderate renal impairment who are receiving strong CYP3A inhibitors, the mirabegron dosage should be reduced to 25 mg once daily; in patients with severe renal impairment, mirabegron is not recommended for those who are taking strong CYP3A inhibitors and the dosage is not to exceed 25 mg once daily in those who are not taking strong CYP3A inhibitors [10]. In the US, no dosage adjustment is recommended for patients with mild or moderate renal impairment, whereas in patients with severe renal impairment, the dosage is not to exceed 25 mg once daily [8].
In both the EU and US, mirabegron is not recommended for use in patients with severe hepatic impairment, as it has not been studied in this population [8, 10]. In the EU, mirabegron is not recommended for use in patients with moderate hepatic impairment who are receiving strong CYP3A inhibitors [10]. In patients with mild hepatic impairment receiving strong CYP3A inhibitors, or with moderate hepatic impairment who are not receiving strong CYP3A inhibitors, the dosage should be reduced to 25 mg once daily [10]. In the US, no dosage adjustment is recommended for patients with mild hepatic impairment, whereas in patients with moderate hepatic impairment, the dosage should not exceed 25 mg once daily [8].
Mirabegron is not recommended for use in women who are pregnant or of child-bearing age but not using contraception, as high doses of mirabegron (14- to 22-fold higher than the maximum recommended human dose) have been associated with teratogenic effects in animals [10]. Mirabegron is expressed in the milk of rodents and is likely to be present in human milk; it should not be used by breastfeeding women [10].
Local prescribing information should be consulted for detailed information regarding special warnings and precautions, use in special populations and possible drug interactions. Specific recommendations regarding the use of mirabegron in overactive bladder syndrome may vary outside the EU, the USA and Japan.
7 Current Status of Mirabegron in Overactive Bladder Syndrome
Mirabegron is approved in the USA [8] and Japan [9], and more recently in the EU [10] and Canada [11], for the symptomatic treatment of urgency, increased micturition frequency and/or urgency incontinence occurring in adults with overactive bladder syndrome [10].
In 12-week, randomized, double-blind, multinational trials, mirabegron 25 or 50 mg once daily was significantly more efficacious than placebo in reducing incontinence episodes and micturition frequency (coprimary endpoints). Mirabegron 50 mg once daily was also efficacious in reducing urgency episodes, increasing the volume of urine voided per micturition and improving HR-QOL and treatment satisfaction. In a 12-month randomized trial with tolterodine ER as the active comparator, both once-daily mirabegron 50 mg and tolterodine ER 4 mg were efficacious in reducing urinary symptoms and improving HR-QOL, based on descriptive analyses of changes from baseline.
In descriptive analyses of the 12-week clinical trials, the adverse event rate with mirabegron 50 mg once daily was similar to that with placebo. In a 12-week trial that included a tolterodine ER arm, there were no striking differences in tolerability between once-daily mirabegron 50 mg and tolterodine ER 4 mg, except that mirabegron recipients were less likely to have dry mouth (2.8 vs. 10.1 %). In the trial of 12 months duration, ≤2.8 % of mirabegron recipients reported dry mouth in comparison with 8.6 % of tolterodine ER recipients. Data from clinical trials and a thorough QT study in healthy adults suggest that mirabegron 50 mg once daily carries a low risk of cardiovascular adverse events and QT interval prolongation.
Overall, mirabegron is an efficacious new treatment for overactive bladder syndrome with a favourable tolerability profile. Comparative trials of mirabegron versus antimuscarinics that are in current use for the treatment of overactive bladder syndrome would be of considerable interest.
Recently initiated trials that will further explore the efficacy and tolerability of mirabegron, include a phase III, 12-week, randomized comparison of mirabegron with the antimuscarinic solifenacin in patients with overactive bladder syndrome who have previously been treated with antimuscarinics but who are not satisfied with treatment because of lack of efficacy [35] and a phase IV, 16-week, safety study of mirabegron as add-on therapy to solifenacin in patients with overactive bladder syndrome who are currently receiving solifenacin [36].
References
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Wagg A, Majumdar A, Toozs-Hobson P, et al. Current and future trends in the management of overactive bladder. Int Urogynecol J. 2007;18(1):81–94.
Irwin DE, Milsom I, Hunskaar S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50(6):1306–15.
Milsom I, Abrams P, Cardozo L, et al. How widespread are the symptoms of overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001;87(9):760–6.
Wein AJ, Chapple C. Overactive bladder in clinical practice. London: Springer; 2012.
Marinkovic SP, Rovner ES, Moldwin RM, et al. The management of overactive bladder syndrome. BMJ. 2012;344(7853):38–44.
Hashim H, Abrams P. Drug treatment of overactive bladder: efficacy, cost and quality-of-life considerations. Drugs. 2004;64(15):1643–56.
Astellas Pharma US, Inc. Myrbetriq™ (mirabegron) extended-release tablets. US prescribing information. 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/202611s000lbl.pdf. Accessed 19 Mar 2013.
Astellas Pharma, Inc. Approval for Betanis® tablet, a treatment for OAB in Japan [media release]. 1 Jul 2011. http://astellas.com/en/corporate/news/detail/approval-for-betanis-tablet-a.html.
European Medicines Agency. Betmiga 25 mg and 50 mg prolonged-release tablets: summary of product characteristics. 2013. http://www.emea.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002388/WC500137309.pdf. Accessed 4 Feb 2013.
Astellas Pharma Canada, Inc. Astellas Pharma Canada, Inc. receives a Notice of Compliance from Health Canada for Myrbetriq™ (mirabegron) [media release]. March 8 2013. http://www.cmastellas.ca/uploads/pdf/FINAL%20-%20Myrbetiq%20NOC.pdf.
Yamaguchi O. B3-adrenoreceptors in human detrusor muscle. Urology. 2002;59(5 Suppl. 1):25–9.
Nitti V, Rosenberg S, Mitcheson D, et al. Urodynamic safety of the potent and selective beta3-adrenoceptor agonist, mirabegron, in males with lower urinary tract symptoms and bladder outlet obstruction [abstract no. POD-03.05]. Urology. 2012;80(3 Suppl. 1):S10.
Chapple CR, Amarenco G, López Aramburu MA, et al. A proof-of-concept study: mirabegron, a new therapy for overactive bladder. BLOSSOM Investigator Group. Neurourol Urodyn. 2013. doi:10.1002/nau.22373.
Chapple CR, Dvorak V, Radziszewski P, et al. A phase II dose-ranging study of mirabegron in patients with overactive bladder. Int Urogyneco J. 2013. doi:10.1007/s00192-013-2042-x.
Malik M, van Gelderen EM, Lee JH, et al. Proarrhythmic safety of repeat doses of mirabegron in healthy subjects: a randomized, double-blind, placebo- and active-controlled thorough QT study. Clin Pharmacol Ther. 2012;92(6):696–706.
Krauwinkel W, van Dijk J, Schaddelee M, et al. Pharmacokinetic properties of mirabegron, a Β3-adrenoceptor agonist: results from two phase I, randomized, multiple-dose studies in healthy young and elderly men and women. Clin Ther. 2012;34(10):2144–60.
Takusagawa S, van Lier JJ, Suzuki K, et al. Absorption, metabolism and excretion of [14C]mirabegron (YM178), a potent and selective Β3-adrenoceptor agonist, after oral administration to healthy male volunteers. Drug Metab Dispos. 2012;40(4):815–24.
Eltink C, Lee J, Schaddelee M, et al. Single dose pharmacokinetics and absolute bioavailability of mirabegron, a Β3-adrenoceptor agonist for treatment of overactive bladder. Int J Clin Pharmacol Ther. 2012;50(11):838–50.
Dickinson J, Lewand M, Sawamoto T, et al. Effect of renal or hepatic impairment on the pharmacokinetics of mirabegron. Clin Drug Invest. 2012;31(1):11–23.
van Gelderen EM, Li Q, Meijer J, et al. An exploratory comparison of the single dose pharmacokinetics of the beta3-adrenoceptor agonist mirabegron in healthy CYP2D6 poor and extensive metabolizers [abstract no. PIII-65]. Clin Pharmacol Ther. 2009;85 Suppl.:S88.
Krauwinkel WJ, van Gelderen EM, Groen MJ. An open-label, one-sequence crossover study to evaluate the effect of multiple doses of mirabegron on the pharmacokinetics of the CYP2D6 substrate desipramine in healthy subjects [abstract no. PIII-65]. In: 111th Annual Meeting of the American Society for Clinical Pharmacology and Therapeutics; 17-20 Mar 2010; Atlanta.
Sawamoto T, Lee J, Alak A, et al. Phase I, open-label, drug interaction study to evaluate the effect of multiple doses of ketoconazole on single dose mirabegron (YM178) oral controlled absorption system (OCAS) in healthy adult subjects [abstract no. PI-43]. Clin Pharmacol Ther. 2011;89 Suppl.:S21.
Sawamoto T, Lee J, Cao Y, et al. Phase I, open-label, drug interaction study to evaluate the effect of repeat doses of rifampin on the single-dose pharmacokinetics of mirabegron (YM178) in healthy adult subjects [abstract no. PI-44]. Clin Pharmacol Ther. 2011;89 Suppl.:S21–2.
Veltkamp S, van Gelderen M, Schaddelee M, et al. Clinical study into the pharmacokinetic, pharmacodynamic and safety interaction of the novel Β3-adrenoceptor agonist mirabegron and metformin in healthy subjects [abstract no. WP107]. In: 9th Congress of the European Association for Clinical Pharmacology and Therapeutics; 12–15 Jul 2009; Edinburgh.
Khullar V, Amarenco G, Angulo JC, et al. Efficacy and tolerability of mirabegron, a Β3-adrenoreceptor agonist, in patients with overactive bladder: results from a randomised European–Australian phase 3 trial. Eur Urol. 2013;63(2):283–95.
Nitti V, Auerbach S, Martin N, et al. Results of a randomized phase III trial of mirabegron in patients with overactive bladder. J Urol. 2013;189(4):1388–95.
Herschorn S, Barkin J, Castro-Diaz D, et al. A phase III, randomized, double-blind, parallel-group, placebo-controlled, multicentre study to assess the efficacy and safety of the β3 adrenoceptor agonist, mirabegron, in patients with symptoms of overactive bladder. Urology. 2013. doi:10.1016/j.urology.2013.02.077.
Chapple CR, Kaplan SA, Mitcheson D, et al. Randomized double-blind, active-controlled phase 3 study to assess 12-month safety and efficacy of mirabegron, a Β3-adrenoceptor agonist, in overactive bladder. Eur Urol. 2013;63(2):296–305.
Nitti VW, Khullar V, van Kerrebroeck P, et al. Mirabegron for the treatment of overactive bladder: a prespecified pooled efficacy analysis and pooled safety analysis of three randomised, double-blind, placebo-controlled, phase III studies. Int J Clin Pract. 2013;67(7):619–32.
Khullar V, Cambronero J, Angulo J, et al. Age-related efficacy of the B3-adrenoceptor agonist mirabegron for the treatment of overactive bladder (OAB): pooled analysis of three prospective, randomised phase III studies in patients aged ≥65 years [abstract no. 331]. In: 42nd Annual Meeting of the International Continence Society; Oct 15–19 2012; Beijing.
Nitti V, Herschorn S, Khullar V, et al. Efficacy of the selective B3-adrenoceptor agonist, mirabegron, in patients with overactive bladder (OAB) who discontinued prior antimuscarinic therapy due to insufficient effect: pooled analysis of three randomised phase III studies [abstract no. 351]. In: 37th Annual Meeting of the International Urogynecological Association; Sep 4–8 2012; Brisbane.
Nitti V, Herschorn S, Auerbach S, et al. The potent and selective Β3-adrenoceptor agonist mirabegron improves patient-reported outcomes in overactive bladder: results from two phase III studies [abstract no. 68]. Neurourol Urodyn. 2012;31(6):813–5.
van Kerrebroeck P, Barkin J, Castro-Diaz D, et al. Randomised, double-blind, placebo-controlled phase III study to assess the efficacy and safety of mirabegron 25 mg and 50 mg once-daily in overactive bladder (OAB) [abstract no. 359 plus poster]. In: 42nd Annual Meeting of the International Continence Society; 15–19 October 2012; Beijing, China.
Astellas Pharma Europe, Ltd. A double-blind, randomized, parallel group, multicentre study to evaluate the efficacy and safety of mirabegron compared to solifenacin in subjects with overactive bladder (OAB) treated with antimuscarinics and dissatisfied due to lack of efficacy. 2012. http://clinicaltrials.gov/show/NCT01638000. Accessed 7 Feb 2013.
Astellas Pharma, Inc. Post-marketing clinical study of mirabegron: add-on therapy with mirabegron in patients with overactive bladder under treatment with solifenacin. 2012. http://clinicaltrials.gov/ct2/show/NCT01745094. Accessed 7 Feb 2013.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the author on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: M. Cerruto, Department of Surgery, University and AOUI of Verona, Verona, Italy; E.J. Geller, Department of Obstetrics and Gynaecology, University of North Carolina, Chapel Hill, NC, USA; P. van Kerrebroeck, Department of Urology, Maastricht University Medical Center, Maastricht, The Netherlands; A.A. Wagg, Division of Geriatric Medicine, University of Alberta, Edmonton, AB, Canada.
Rights and permissions
About this article
Cite this article
Sanford, M. Mirabegron: A Review of Its Use in Patients with Overactive Bladder Syndrome. Drugs 73, 1213–1225 (2013). https://doi.org/10.1007/s40265-013-0086-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-013-0086-3