Abstract
Introduction
The potential for routine sequence symmetry analysis (SSA) signal detection in health claims databases to detect new safety signals of medicines is unknown.
Objective
Our objective was to assess the potential utility of SSA as a signal detection tool in health claims data for detecting medicines with potential heart failure (HF) adverse event signals.
Methods
We applied the SSA method to all subsidized single-ingredient medicines in Australia. The source of data was the Australian Government Department of Veterans’ Affairs (DVA) administrative claims database using data collected between 2002 and 2011. We used first ever HF hospitalization and frusemide initiation as indicators for HF. A signal was considered to be present if the lower limit of the 95 % confidence interval for the adjusted sequence ratio was greater than one. To identify potential new signals of HF, we excluded medicines where HF or edema was listed in the product information (PI) of that medicine or for any other medicine in the same class. We also excluded medicines that were used in HF treatment and medicines indicated for diseases that may contribute to the development of HF.
Results
We tested 691 medicines. HF signals were detected for 12 % (80/691) using the hospitalization event and 22 % (153/691) using frusemide initiation. Among medicines that did not have HF listed in the PI, SSA found 11 % (44/397) associated with HF hospitalization and 15 % (60/397) associated with frusemide initiation. Of the medicines tested in which no other medicine in the same class had HF or edema in the PI, and where the medicine was not indicated for a disease that is a risk factor for HF, potential new signals were generated for 2–3 % of these medicines tested (12 of 397 medicines using HF hospitalization and 9 of 397 medicines using frusemide initiation).
Conclusion
SSA generated potential new signals of HF for some anti-glaucoma and anti-dyspepsia medicines. For some of the potential signals, the event is biologically plausible and some have pre-marketing and post-marketing case reports to support the finding. Confirmation of these signals using cohort studies is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Prior to this research, the utility of sequence symmetry analysis (SSA) as a signal detection tool to detect new adverse event signals from administrative claims database was unknown. |
Using first ever heart failure hospitalization or initiation of frusemide as proxies for heart failure adverse event signals, SSA identified a positive signal for 2–3 % of medicines tested that did not have heart failure or edema listed in their product information (heart failure hospitalization 12/397, frusemide 9/397). |
Potential new heart failure signals were identified for some anti-glaucoma and anti-dyspepsia medicines given biologically plausibility and pre-marketing and post-marketing case reports. |
SSA could be a feasible tool to identify potential new signals of adverse events of medicines for further investigation. |
1 Introduction
Data mining can be applied to large data for two purposes: to describe the general properties of the data in the database or to generate hypotheses about the data to make predictions [1]. In a pharmaco-surveillance context, the main objective of data mining is to discover potentially clinically relevant medicine–event associations [2]. Health regulators have incorporated computerized data mining techniques to generate safety signals of medicines in adverse event spontaneous reporting databases. The techniques currently applied to spontaneous reporting databases to detect adverse event signals include disproportionality techniques, proportional reporting ratio (PRR), reporting odds ratio (ROR), and Bayesian methods [3–6]. The validity of these methods as a data mining or safety signal detection tool in spontaneous reporting databases has been investigated, and the potential of these methods to detect adverse event signals has been shown to be low to moderate (sensitivity 32 %, positive predictive value 20–44 %) [7, 8].
Data mining in computerized population-based health claims data may have the potential to complement spontaneous reporting systems for the detection of unknown adverse event signals. Health claims data are unlikely to be affected by the under-reporting or reporting bias that may occur in spontaneous reporting systems because claims data are collected routinely and stored electronically [9], thus it may capture all subsidized medicine users and outcomes.
Studies using data mining methods in health claims data have thus far investigated the ability of the method to detect known adverse event signals [10–13], for example non-steroidal anti-inflammatory drug (NSAID)-induced myocardial infarction [10] and cerivastatin-induced rhabdomyolysis [12]. Data mining has also been studied to assess unknown adverse event signals [14–16]. The methods studied include MUTARA (Mining Unexpected Temporal Association Rule) [14], Gamma Poisson Shrinker [16], and Information Component [15]. Sequence symmetry analysis (SSA) has been used to detect known adverse event signals using health claims data [17–19] and also has potential to be used as a signal detection tool for unknown events. SSA has been shown to have moderate sensitivity (61 %) and high specificity (93 %) to detect known adverse event signals in health claims data [20]. The method was also found to be consistent across different databases [21], suggesting that SSA may be a robust method to detect adverse events across databases. However, the utility of SSA as a signal detection tool in health claims data to detect potential clinically relevant and new safety signals has not been explored. In this study, we aimed to explore the utility of SSA as a signal detection tool to identify potential new signals of adverse events. We used the adverse event heart failure (HF) as a test case because it is a clinically important adverse event and HF is potentially preventable.
2 Methods
2.1 Source of Data for Signal Detection
Australian Government Department of Veterans’ Affairs (DVA) health claims data between 1 January 2002 and 31 December 2011 (i.e., 10 years) were used as the data source. The DVA database consists of health claims data for the veteran population who have served in Australia’s armed forces and their eligible dependents and spouses. The DVA database contains information on all medicines and healthcare utilization by veterans for which DVA pay a subsidy. This includes data for all medicines dispensed on the Pharmaceutical Benefits Scheme (PBS) and Repatriation Pharmaceutical Benefits Scheme (RPBS) as well as hospitalizations. The dataset covers a treatment population of 250,000 veterans [22]. Medicines are coded using the World Health Organization (WHO) anatomical and therapeutic chemical (ATC) classification [23] and the Schedule of Pharmaceutical Benefits item codes [24]. Hospitalizations are coded according to the WHO International Classification of Diseases (ICD), 10th revision, Australian modification [25].
2.2 Tested Medicines
A total of 788 subsidized medicines were identified in the database. Only single-ingredient products were tested. After combination products were excluded, a total of 691 single-ingredient products were tested.
The Australian approved product information (PI) for each tested medicine was extracted from the Australian Therapeutic Goods Administration (TGA) website and reviewed to identify whether heart failure was a listed adverse event for each tested medicine (Table 1) [26]. We classified the medicines as having a known HF adverse event if HF was listed as an adverse event in the PI of the medicine. We also included medicines with edema listed as an adverse event in the PI as known heart failure to avoid confounding bias because edema can be a sign of underlying HF or a complication of HF [27]. All selected medicines were reviewed and classified by two clinical researchers (IAW, LKE) as (1) a medicine indicated for diseases with potential to cause HF or (2) a medicine indicated for or used as an adjunct in HF treatment. This is because, in the search for potential new HF signals, independence between the medicine and the outcome of interest, in this case HF, was assumed. Medicines that could be related to the HF outcome, for example medicines indicated for use following myocardial infarction, may have a higher incidence of use amongst people with HF post-myocardial infarction, because the risk of HF increases following myocardial infarction [28]. Thus, HF is not necessarily an adverse event of the medicine itself.
2.3 Signal Detection Method and Adverse Event Outcome to be Identified
SSA [29] was carried out for all 691 medicines. HF was measured in two ways: (1) using the first occurrence of HF hospitalization (ICD-10 code I50.0, I50.1, I50.9) and (2) the first initiation of frusemide dispensing (ATC code C03CA01). SSA has been described in detail previously [30]. SSA is an algorithm that uses administrative claims databases that contain individual prescription or hospital records to make an assessment between a medicine and a potential adverse drug reaction (ADR). The principle behind this method is to determine the ratio of sequences of two medicines or a medicine and an event. One medicine is suspected of causing an ADR, also called the index medicine, and the second medicine is a medicine used to counteract or treat the ADR, for example anti-diarrheal medicines are used to treat diarrhea. The second medicine serves as an indicator for the ADR. The sequence of dispensing of both medicines in the same person is identified in the prescription database: the medicine suspected of causing the ADR may be supplied first and the indicator may be supplied second, or vice versa. The observed sequence ratio is calculated by dividing the number of people with the indicator for the ADR that was dispensed second by the number of people with the indicator for the ADR dispensed first. This is called the crude sequence ratio (CSR). We used a 1-year time period for SSA, as previous analysis had demonstrated this to be an appropriate time span in which to detect adverse events [20]. A run-in period of 1 year was used to ensure incident events were identified.
SSA is robust towards cofounders that remain stable over time because the patient population serves as its own control. However, SSA is sensitive to changing trends over time in the medicine or outcome of interest. To adjust for the trend over time, a null-effect sequence ratio (NSR) was calculated [29]. The NSR estimates the sequence ratio that might be expected due to the trends in medicine use, assuming that the investigated medicine and the outcome are unrelated. The adjusted sequence ratio (ASR) was obtained by dividing the CSR by the NSR. A non-parametric resampling technique was used to create the bootstrapped confidence intervals (CIs) for the NSR. First, the number of observations in the SSA analysis were randomly selected with replacement to obtain a bootstrapped dataset. The ASR was then calculated on this dataset. This was repeated 500 times, and a bootstrap distribution of the ASR estimate was created. A 95 % CI was generated for the bootstrapped ASR distribution using the bootstrapped-t method. A signal was considered to be present when the lower limit of the 95 % CI was greater than one. All analyses were carried out using SAS 9.3 (SAS Institute, Inc., Cary, NC, USA).
2.4 Identification of Potential New Heart Failure Signals
To identify new HF adverse events, we defined adverse event signals where medicines were associated with significant positive SSA signals that (1) did not have HF or edema listed in the PI, (2) other medicines in the same class did not have HF or edema listed as an adverse event in the PI, (3) were not indicated for HF treatment or were not indicated for diseases that have the potential to cause HF.
3 Results
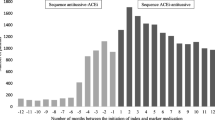
Figure 1 describes the identification of potential new HF signals. Of the 691 tested medicines, 80 (12 %) were associated with HF hospitalization and 153 (22 %) were associated with frusemide initiation.
The list of SSA signals for HF hospitalization and frusemide initiation is provided in Appendices A and B in the Electronic Supplementary Material (ESM). Anti-diabetics, beta-blockers, statins, anti-glaucoma, and NSAIDs were amongst medicines that were associated with excess HF hospitalization and frusemide initiation (Appendix A and B).
After excluding medicines that had edema listed in the PI for the medicine or HF or edema listed as an adverse event for other medicines in the same class and medicines indicated for use in HF treatment or for diseases with potential to cause heart failure, 2–3 % were potentially new HF signals (Fig. 1).
Initially, there were 44 SSA signals for HF hospitalization amongst medicines that did not have HF or edema listed as an adverse event in the PI. Of these, 28 signals were for medicines where HF or edema was listed in the PI for other medicines in the same class (Fig. 1). A further four signals were for medicines indicated for the treatment of HF or indicated for diseases with the potential to cause HF. After excluding these 32 potentially confounded signals, 12 (35) signals remained. Three of the signals were for anti-glaucoma medicines and two were for anti-histamine medicines (Table 1).
Using frusemide initiation as an indicator of HF, 60 signals were identified amongst medicines that do not have HF in the PI. Of these, 34 signals were for medicines where HF or edema was listed in the PI for other medicines in the same class (Fig. 1). A further 17 signals were for medicines indicated for the treatment of HF or indicated for diseases with potential to cause HF (Fig. 1). After excluding these 51 potentially confounded signals, nine new signals remained (Fig. 1). Two of these were anti-glaucoma medicines and two were for anti-dyspepsia medicines (Table 1).
4 Discussion
This study demonstrated the feasibility of using SSA as a signal detection tool for detecting the potential adverse outcome, HF. The method identified a statistically significant ASR for 19 unique medicines where HF was not listed in the PI and where the adverse event was not listed for other medicines in the same class and the medicines were not indicated for diseases with the potential to cause HF or used in HF treatment.
The class of medicine with the strongest potential sign was the prostaglandin anti-glaucoma eye drop. This group of medicines had multiple medicines in the class with positive signals from HF hospitalization or frusemide dispensing (bimatoprost, travoprost, and latanoprost). Only latanoprost had a statistically significant association with both HF hospitalization and frusemide initiation indicators. Travoprost and bimatoprost were associated with excess HF hospitalization but not frusemide initiation. An association between anti-glaucoma prostaglandin analogues (latanoprost, travoprost, and bimatoprost) and HF has not been previously reported; however, there is some evidence to support our finding. In post-marketing experience, the Uppsala Monitoring Centre (UMC) had received 13 spontaneous reports of latanoprost eye drops associated with HF by 2010 [31]. One of these was classified as a definite reaction that occurred upon rechallenge. A pre-marketing clinical trial for travoprost reported one case of edema and three cases of HF in travoprost-treated patients [32]. There were no reports of these adverse events in placebo-treated patients. Latanoprost and travoprost are prostaglandin F2 alpha (PGF2α) analogues that have the potential to cause vasoconstriction to the coronary artery and renal blood vessels [33, 34]. Vasoconstrictor activity of PGF2α on the renal cortical nephron may result in enhanced sodium retention [35]. When considering Bradford Hill criteria [36], this potential signal meets a number of criteria: the SSA result provides evidence of temporality and consistency, with a number of medicines from the same class showing similar results. Further consistency is evident with the pre-marketing and post-marketing case reports of HF. Finally, biological plausibility supports the SSA signal for prostaglandin analogue-associated HF. Collectively, this is suggestive of a potentially new signal that warrants further investigation.
The other group of medicines that featured in the signals generated were the histamine antagonists. Betahistine has weak H1 agonist activity and moderate H3 antagonist activity [37]. A positive signal was found for betahistine for both the hospital event and medication event. Fexofenadine and loratadine, which are H2 antagonists, were both positive for the hospitalization outcome. Two H2 antagonists (famotidine and ranitidine) were also positive. Histamine does have action on the heart, and a number of studies have investigated the role of histamine antagonists on HF and cardiac function, although results are not clear cut [38–41]. With regards to the H2 antagonists, an alternative explanation is that they could have been co-prescribed with NSAIDs to prevent gastric ulcers and that the NSAID could have been the contributor to the observed effect. As this study was a signal detection study, co-prescribing was not assessed and cannot be ruled out as a possible contributor.
The other potential signal of interest was for teriparatide, for which a risk estimate of 5 was observed. Teriparatide is recombinant human parathyroid hormone [42]. Parathyroid hormone has been implicated in HF [43, 44], so this potential signal is also worthy of further investigation. While the above examples are potentially of interest, we cannot rule out false positives. Previous work has identified that SSA has moderate sensitivity and high specificity [20] for known adverse reactions, which suggests the possibility that these signals are false is low.
Similar to other signal detection studies using health claims data, our SSA study generated HF signals for medicines indicated for the treatment of diseases that themselves may be associated with an increased risk of developing HF, including statins (pravastatin, simvastatin) and anti-thrombotic medicines such as dalteparin (Appendices A and B). HF commonly develops after acute coronary syndromes (ACS) such as myocardial infarction [45], and initiation of statins and anti-thrombotic medicines are indicated in patients with ACS. Thus, associations seen for these medicines suggest confounding by indication may have occurred. Confounding by indication could occur when the indication for treatment is related to the risk of future health outcome [46]. The same scenario was shown in other data mining studies in health claims data. In one study, the Bayes Multi-Item Gamma Poisson Shrinkage (MGPS) method was applied to 259 different adverse events for celecoxib and rofecoxib [10]. The study identified only one known adverse event, myocardial infarction, associated with celecoxib, whereas other events that were indicated for and related to celecoxib treatment such as osteoarthritis and rehabilitation were detected [10]. In another Bayesian data mining study performed on 3445 medicines and 5753 events, the potential for detecting indications for use of the medicine or treatment of other underlying diseases related to the medicine was highlighted [47]. In this study [47], the antihypertensive medicine nifedipine was found to be associated with hypertension and diabetes. This study also highlighted the importance of sound clinical interpretation of the results of signal detection studies, so that signals relating to the indication for use of the medicine are not misinterpreted as new adverse events.
A limitation of this study was that we only assessed one outcome, HF, using two different measures. Future work is required to investigate the potential of SSA as a routine signal detection tool for other outcomes in health claims data. Our results are not sensitive to side effects of frusemide causing the examined medicine to be used. If frusemide produces an adverse effect that needs to be treated with the investigated medicines, the results would be biased towards the null. Additionally, some of the frusemide signals may be due to peripheral edema rather than HF.
In this study, we made no adjustments to account for potential multiple false-positive signals that could occur when many medicine–event and medicine–prescription pairs were tested. Since there is no adjustment for multiple testing, 2.5 % of the ASRs are expected to have a 95 % CI >1 by chance alone. However, only few potential new signals were generated in this study after excluding medicines indicated for HF or diseases with potential to cause HF. These potential new signals both for HF hospitalization and frusemide initiation could therefore be prioritized for further investigation. Hence, clinical knowledge should be incorporated into the detection of unknown ADR signals using the SSA method.
5 Conclusion
SSA provides an opportunity to interrogate large claims datasets for the purpose of safety signal detection and may help to complement signal detection tools already in use by medicine regulatory authorities. We identified potential new HF signals for the prostaglandin eye drops, which were biologically plausible and were supported by case reports. Further studies are required to investigate these signals.
References
Han J, Kamber M. Data mining: concepts and techniques. 2nd ed. California: Morgan Kaufman; 2006.
Hauben M, Madigan D, Gerrits CM, Walsh L, Van Puijenbroek EP. The role of data mining in pharmacovigilance. Exp Opin Drug Saf. 2005;4(5):929–48.
Evans SJW, Waller PC, Davis S. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Saf. 2001;10(6):483–6.
Egberts ACG, Meyboom RHB, Van Puijenbroek EP. Use of measures of disproportionality in pharmacovigilance: three Dutch examples. Drug Saf. 2002;25(6):453–8.
Bate A, Lindquist M, Edwards IR, Olsson S, Orre R, Lansner A. A Bayesian neural network method for adverse drug reaction signal generation. Eur J Clin Pharmacol. 1998;54(4):315–21.
Gould AL. Practical pharmacovigilance analysis strategies. Pharmacoepidemiol Drug Saf. 2003;12(7):559–74.
Lindquist M, Stahl M, Bate A, Edwards IR, Meyboom RHB. A retrospective evaluation of a data mining approach to aid finding new adverse drug reaction signals in the WHO international database. Drug Saf. 2000;23(6):533–42.
Lehman HP, Chen J, Gould AL, Kassekert R, Beninger PR, Carney R. An evaluation of computer-aided disproportionality analysis for post-marketing signal detection. Clin Pharmacol Ther. 2007;82(2):173–80.
Virnig BA, McBean M. Administrative data for public health surveillance and planning. Ann Rev Pub Health. 2001;22:213–30.
Curtis JR, Cheng H, Delzell E, Fram D, Kilgore M, Saag K. Adaptation of bayesian data mining algorithms to longitudinal claims data: coxib safety as an example. Med Care. 2008;46(9):969–75.
Schuemie MJ. Methods for drug safety signal detection in longitudinal observational databases: LGPS and LEOPARD. Pharmacoepidemiol Drug Saf. 2011;20(3):292–9.
Brown JS, Kulldorff M, Chan KA, Davis RL, Graham D, Pettus PT, et al. Early detection of adverse drug events within population-based health networks: application of sequential testing methods. Pharmacoepidemiol Drug Saf. 2007;16(12):1275–84.
Brown J, Petronis K, Bate A, Zhang F, Dashevsky I, Kulldorff M, et al. Drug adverse event detection in health plan data using the Gamma Poisson Shrinker and comparison to the Tree-based Scan Statistic. Pharmaceutics. 2013;5(1):179–200.
Jin H, Chen J, He H, Kelman C, McAullay D, O’Keefe CM. Signaling potential adverse drug reactions from administrative health databases. IEEE Trans Knowl Data Eng. 2010;22(6):839–53.
Norén GN, Hopstadius J, Bate A, Star K, Edwards IR. Temporal pattern discovery in longitudinal electronic patient records. Data Min Knowl Discov. 2010;20:361–87.
Coloma PM, Schuemie MJ, Trifirò G, Furlong L, van Mulligen E, Bauer-Mehren A. Drug induced acute myocardial infarction: Identifying ‘prime suspects’ from electronic healthcare records-based surveillances system. PLoS One. 2013;8(8):e72148.
Vegter S, De Jong-Van Den Berg LTW. Misdiagnosis and mistreatment of a common side effect—angiotensin-converting enzyme inhibitor-induced cough. Br J Clin Pharmacol. 2010;69(2):200–3.
Garrison SR, Dormuth CR, Morrow RL, Carney GA, Khan KM. Nocturnal leg cramps and prescription use that precedes them: a sequence symmetry analysis. Arch Intern Med. 2012;172(2):120–6.
Corrao G, Botteri E, Bagnardi V, Zambon A, Carobbio A, Falcone C, et al. Generating signals of drug-adverse effects from prescription databases and application to the risk of arrhythmia associated with antibacterials. Pharmacoepidemiol Drug Saf. 2005;14(1):31–40.
Wahab IA, Pratt NL, Wiese MD, Kalisch LM, Roughead EE. The validity of sequence symmetry analysis (SSA) for adverse drug reaction signal detection. Pharmacoepidemiol Drug Saf. 2013;22(5):496–502.
Pratt N, Andersen M, Bergman U, Choi N-K, Gerhard T, Huang C, et al. Multi-country rapid adverse drug event assessment: the Asian Pharmacoepidemiology Network (AsPEN) antipsychotic and acute hyperglycaemia study. Pharmacoepidemiol Drug Saf. 2013;22(9):915–24.
Australian Government Department of Veterans’ Affairs. Treatment population statistics. Quarterly Report-March 2011; 2011 [cited 2015 May 30]. Available from: http://www.dva.gov.au/aboutDVA/Statistics/Documents/TpopMar2011.pdf.
World Health Organization Collaborating Centre for Drug Statistics Methodology. Anatomical Therapeutic Chemical Code Classification index with Defined Daily Doses 2015; 2015 [cited 2015 May 30]. Available from: http://www.whocc.no/atcddd/.
Australian Government, Department of Health and Ageing. Schedule of Pharmaceutical Benefits. PBS for health professional 2015; 2015 [cited 2015 May 30]. Available from: http://www.pbs.gov.au/info/healthpro/explanatorynotes/section1/Section_1_2_Explanatory_Notes.
National Centre for Classification in Health. International statistical classification of diseases and related health problems, Tenth Revision, Australian Modification (ICD-10-AM). National Centre for Classification in Health, Faculty of Health Sciences, University of Sydney; 2004.
Australian Government. Department of Health and Ageing. Therapeutic Goods Administration. Information about prescription medicines in Australia; 2015 [cited 2015 May 30]. Available from: https://www.ebs.tga.gov.au/.
Watson RDS, Gibbs CR, Lip GYH. ABC of heart failure: clinical features and complications. BMJ. 2000;320(7229):236–9.
Dargie H. Heart failure post-myocardial infarction: a review of the issues. Heart. 2005;91(Suppl 2):ii3–ii6.
Tsiropoulos I, Andersen M, Hallas J. Adverse events with use of antiepileptic drugs: a prescription and event symmetry analysis. Pharmacoepidemiol Drug Saf. 2009;18(6):483–91.
Hallas J. Evidence of depression provoked by cardiovascular medication: a prescription sequence symmetry analysis. Epidemiol. 1996;7(5):478–84.
Uppsala Monitoring Centre. Latanoprost Safety Report 2010.
United States Department of Health and Services. U.S Food and Drug Administration. Drugs@FDA: FDA Approved Drug Products. Travatan; 2015 [cited 2015 May 30]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/nda/2001/21257_Travatan_medr_P1.pdf.
Parker RE, Strandhoy JW. A vasoconstrictor cardiogenic chemoreflex induced by prostaglandin F2 alpha. Am J Physiol Heart Circ Physiol. 1981;240(4):H528–32.
Schror K. Prostaglandin-mediated actions of the renin-angiotensin system. Arzneimittelforschung. 1993;43(2A):236–41.
Castellani S, Paladini B, Paniccia R, Di Serio C, Vallotti B, Ungar A, et al. Increased renal formation of thromboxane A 2 and prostaglandin F 2α in heart failure. Am Heart J. 1997;133(1):94–100.
Hill AB. The environment and disease: association or causation? Proc R Soc Med London. 1965;58:295–300.
Mira E. Betahistine in the treatment of vertigo. History and clinical implications of recent pharmacological researches. Acta Otorhinolaryngol Ital. 2001;21(3 Suppl 66):1–7.
Borow KM, Ehler D, Berlin R, Neumann A. Influence of histamine receptors on basal left ventricular contractile tone in humans: assessment using the H2 receptor antagonist famotidine and the beta-adrenoceptor antagonist esmolol as pharmacologic probes. J Am Coll Cardiol. 1992;19(6):1229–36.
Hilleman DE, Mohiuddin SM, Williams MA, Gannon JM, Mathias RJ, Thalken LJ. Impact of chronic oral H2-antagonist therapy on left ventricular systolic function and exercise capacity. J Clin Pharmacol. 1992;32(11):1033–7.
Malinowska B, Godlewski G, Schlicker E. Histamine H3 receptors: general characterization and their function in the cardiovascular system. J Physiol Pharmacol. 1998;49(2):191–211.
Solomon SD, Wolff S, Jarboe LA, Wolfe MM, Lee RT. Effects of histamine type 2-receptor antagonists cimetidine and famotidine on left ventricular systolic function in chronic congestive heart failure. Am J Cardiol. 1993;72(15):1163–6.
Dobnig H. A review of teriparatide and its clinical efficacy in the treatment of osteoporosis. Expert Opin Pharmacother. 2004;5(5):1153–62.
Hagström E, Ingelsson E, Sundström J, Hellman P, Larsson TE, Berglund L, Melhus H, Held C, Michaëlsson K, Lind L, Arnlöv J. Plasma parathyroid hormone and risk of congestive heart failure in the community. Eur J Heart Fail. 2010;12(11):1186–92.
Patrik A, Erik R, Ronnie W. Primary hyperparathyroidism and heart disease: a review. Eur Heart J. 2004;25(20):1776–87.
Kaul P, Ezekowitz JA, Armstrong PW, Leung BK, Savu A, Welsh RC, et al. Incidence of heart failure and mortality after acute coronary syndromes. Am Heart J. 2013;165(3):379–85.e2.
Walker AM. Confounding by indication. Epidemiol. 1996;7(4):335–6.
Nor GN, Hopstadius J, Bate A, Star K, Edwards IR. Temporal pattern discovery in longitudinal electronic patient records. Data Min Knowl Discov. 2010;20(3):361–87.
Acknowledgments
The authors thank DVA for providing the data used in this study. We would also like to thank the Uppsala Monitoring Centre for providing prostaglandin eye drop ADR reports. The supplied data come from a variety of sources, including both regulated and voluntary sources. The likelihood of a causal relationship is not the same in all reports. The study results, discussion, and conclusion are those of the authors and do not represent the opinion of the World Health Organization.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work is funded by a National Health and Medical Research Centre (NHMRC) Grant, Centre of Research Excellence in post-marketing surveillance of medicines and medical devices GNT 1040938. Nicole Pratt is supported by an NHMRC Early Career Research Fellowship GNT 1035889. Dr. Izyan A. Wahab was supported by a Malaysian Government PhD scholarship.
Conflict of interest
Izyan A. Wahab, Nicole L. Pratt, Lisa Kalisch Ellett, and Elizabeth E. Roughead have no conflicts of interest that are directly relevant to the content of the manuscript.
Statement about prior postings and presentations
The results of the study have not been previously presented at any proceedings or conferences.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wahab, I.A., Pratt, N.L., Ellett, L.K. et al. Sequence Symmetry Analysis as a Signal Detection Tool for Potential Heart Failure Adverse Events in an Administrative Claims Database. Drug Saf 39, 347–354 (2016). https://doi.org/10.1007/s40264-015-0391-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-015-0391-8