Abstract
Status epilepticus (SE) is one of the most frequent neurological emergencies. Despite this, understanding of its pathophysiology and evidence regarding its management is limited. Rapid, effective, and well-tolerated treatment to achieve seizure cessation is advocated to prevent brain damage or potentially lethal outcomes. The last two decades have witnessed an exponential increase in the number of available antiepileptic drugs (AEDs). These compounds, especially lacosamide and levetiracetam, in view of their intravenous formulation, have been increasingly prescribed in SE. These and other newer AEDs present a promising profile in terms of tolerability, with few centrally depressive effects, favorable pharmacokinetic properties, and fewer drug interactions than classical AEDs; conversely, they are more expensive. There is still no clear evidence to suggest a specific beneficial impact of newer AEDs on SE outcome, preventing any strong recommendation regarding their prescription in SE. Further comparative studies are urgently required to clarify their place and optimal use in the armamentarium of SE treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Status epilepticus (SE) is one of the most frequent neurological emergencies. Rapid recognition and control of SE are advocated to prevent brain damage or a fatal outcome. |
Newer antiepileptic drugs show good tolerability, but no significant beneficial impact on outcome has yet been demonstrated in SE. |
Good-quality randomized trials are urgently needed to determine the place of newer AEDs in SE. |
As no high-quality evidence is available for choosing one molecule over another, prescription of AEDs in SE should be tailored to each patient considering the efficacy spectrum, potential of adverse events, pharmacokinetic interactions, and financial impact. |
1 Introduction
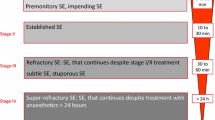
Status epilepticus (SE) is one of the most frequent neurological emergencies, associated with significant morbidity, and a mortality of around 10–20% [1, 2]. While generalized convulsive SE has been classically defined as at least 5 min of continuous seizure, or discrete seizures between which there is incomplete recovery of consciousness [3], the International League Against Epilepsy recently proposed a definition encompassing all SE types, including timing according to different seizure semiologies, and considering the risk of neuronal injury. SE is
“… a condition resulting either from the failure of the mechanisms responsible for seizure termination, or from the initiation of mechanisms, which lead to abnormally, prolonged seizures (after time point t1). It is a condition, which can have long-term consequences (after time point t2), including neuronal death, neuronal injury” [4].
While SE persisting after two antiepileptic drugs (AEDs) is defined as refractory (RSE), SE continuing despite a general anesthetic trial is called super-refractory SE (SRSE) [5]. Of note, evidence regarding neuronal injury essentially relies on animal studies, but rapid recognition and control of SE appears fundamental to improving chances of success and preventing potential complications.
The last two decades have witnessed an exponential increase in AEDs. These are often classified as “traditional” or “newer” according to the year of marketing (typically, before or after 1990, respectively). The newer compounds, especially levetiracetam and lacosamide [6,7,8], have been increasingly prescribed in patients with SE and potentially exhibit better tolerability and fewer pharmacokinetic interactions than traditional AEDs [9].
Current SE treatment guidelines propose a three-stage approach. Benzodiazepines show level A evidence in early SE (stage I). If seizures continue despite benzodiazepines, defining established SE (stage 2); intravenous AEDs such as phenytoin, phenobarbital, valproate, levetiracetam, or lacosamide are proposed. If SE persists despite the first- and second-line treatment, the patient is considered in RSE (stage 3), where general anesthesia and coma induction can be considered [2, 10,11,12]. Currently, as we discuss, there is no high-class evidence to prefer one particular intravenous AED in stage 2 treatment; thus, there is an urgent need for understanding of available information and to outline knowledge gaps.
Historically, phenytoin, valproate, and phenobarbital represent the most used second-line compounds. A recent careful review assessing the relative efficacy of second-line treatments in benzodiazepine-resistant convulsive SE, analyzing 22 studies with a total of more than 700 patients [13], reported that seizure cessation using valproate (75.7%; 95% confidence interval [CI] 63.7–84.8) and phenobarbital (73.6%; 95% CI 58.3–84.8) seemed somewhat better than phenytoin (50.2%; 95% CI 34.2–66.1). Another review based on Indian experience found that, administered as second-line treatment for convulsive SE (but not uniformly after a failed benzodiazepine), valproate was efficacious in 74.1% and phenytoin in only 25% of patients [14]. These broad percentages may orient on the expected efficacy of other compounds, but extreme care is needed when interpreting studies from diverse geographical settings and with markedly different methodological approaches.
The aim of this article is to critically review, without performing a systematic analysis, the current data concerning newer AEDs mostly used as second-line treatment, that are available as intravenous formulations, such as levetiracetam, lacosamide, or brivaracetam, but also as oral compounds, such as pregabalin, topiramate, or perampanel. SE in children and post-anoxic cases are not considered in this review in view of their peculiarities; for the sake of space constraints, we do not focus on alternative approaches (such anti-inflammatory or non-pharmacological therapies). Available literature on each drug is described in descending order of evidence. Table 1 summarizes mechanisms of actions and the typical loading and maintenance doses.
2 Newer Antiepileptic Drugs (AEDs): Intravenous Administration
2.1 Levetiracetam
Levetiracetam was the first newer AED with an intravenous formulation described in SE treatment [15,16,17]. It binds to synaptic vesicle protein 2 (SV2) and presents a broad spectrum of action with limited drug–drug interactions; the intravenous formulation is bioequivalent to the oral and appears generally well tolerated even at high dosages or with rapid infusion rates [18, 19]. Adverse effects were reported at very low rates (< 10%) and were essentially mild and transient [18, 20, 21]. Levetiracetam is the most commonly prescribed newer AED, and a previous assessment by our group showed that it has become the most frequently used AED in SE [6].
The few randomized trials that have investigated the efficacy of levetiracetam versus phenytoin or valproate generally reported comparable results [14, 22,23,24,25]. Two meta-analyses addressed the efficacy of second-line treatment, including intravenous levetiracetam [13, 26]. The latter was compared with intravenous valproate or phenytoin for 144 convulsive SE episodes (generalized or focal) in patients of any age [26]; the authors did not report any significant difference in clinical seizure cessation between levetiracetam and phenytoin (odds ratio [OR] 1.18; 95% CI 0.50–2.79), whereas the limited number of publications prevented an assessment of levetiracetam versus valproate. However, the indirect comparison showed no difference (OR 1.16; 95% CI 0.45–2.97), possibly because of the limited statistical power. This appears to be broadly in line with the aforementioned analysis assessing the relative efficacy of levetiracetam, valproate, lacosamide, phenytoin, and phenobarbital in convulsive SE [13]: levetiracetam (seizures cessation in 68.5%; 95% CI 56.2–78.7) was found to be similar to valproate and phenobarbital but slightly better than phenytoin. A previous systematic review of ten studies (334 patients) described a large efficacy range (44–94%), with higher numbers reported in retrospective assessments [27], suggesting possible information and publication bias, whereas a pooled analysis of 707 patients with various forms of SE found seizure cessation in 70% [20].
A retrospective study from our group comparing the efficacy of levetiracetam, phenytoin, and valproate in 187 adults with various forms of SE questioned the relative efficacy of levetiracetam [28]: failure to control SE occurred in 25.4% of episodes treated with valproate, 41.4% with phenytoin, and 48.3 % with levetiracetam. After adjustment for relevant SE outcome predictors, levetiracetam showed a higher risk of lack of seizure control than valproate (OR 2.69; 95% CI 1.19–6.08), with approximately 17% of treatment failures attributable to levetiracetam. Importantly, however, the prognosis at hospital discharge was comparable. Several other case series have been published since 2007; these may provide some valuable information but unfortunately lack comparisons [15,16,17, 28, 29].
Intravenous levetiracetam has also been considered as first-line treatment [18, 30]. An Indian randomized trial compared it with lorazepam in 79 patients presenting convulsive or subtle SE; these compounds were equally effective in reaching clinical seizure cessation within 10 min of administration (76.3% after levetiracetam vs. 75.6% after lorazepam); the 24-h seizure freedom was also comparable. Lorazepam was nevertheless associated with significantly greater need for artificial ventilation, though no significant difference in mortality was reported [24]. Of note, the studied population included a high proportion of acute symptomatic SE, especially central nervous system (CNS) infections, and 1-week mortality was relatively high (30.3 %), probably reflecting a specific geographical setting and patient selection. A recent French prehospital, randomized controlled study compared clonazepam alone or in addition to levetiracetam at the onset of generalized convulsive SE in 107 patients; convulsions stopped at 15 minutes in 84% of patients receiving clonazepam and in 74% of patients receiving clonazepam plus levetiracetam (relative risk [RR] 0.88, 95% CI 0.74–1.05; p = 0.14) [31]. It has been argued that levetiracetam may take a relatively long time to reach the CNS; this factor might influence its efficacy if assessed early in SE [32].
Levetiracetam is by far the most studied newer AED with available randomized controlled studies and meta-analyses. However, many of these studies are flawed: they have methodological issues, are set in countries with SE profiles and work-ups that differ from those in the Western world—limiting generalizability—and have limited sample sizes, lacking sufficient power to detect statistical differences.
2.2 Lacosamide
Lacosamide acts on the slow inactivation of the sodium channel and has a narrow spectrum of action, presenting a favorable side effects profile, linear pharmacokinetics, a low interaction potential, and the possibility of rapid intravenous administration with the same safety as the oral formulation [33,34,35,36]. Thus, “off-label” utilization of lacosamide in SE has rapidly increased, reaching nearly 40% of SE episodes in 2016 in our previous study [6].
A recent Indian randomized controlled trial compared the efficacy and safety of intravenous lacosamide (400 mg) and intravenous valproate (30 mg/kg) in 66 patients with lorazepam-resistant SE. While 1-h seizure remission was similar between the two groups, the 24-h efficacy was higher in the valproate group (66.6 vs. 45.5 %). However, this trial was retracted because of statistical errors [37, 38]. A review focusing on the period between 2009 and 2012 retrieved 136 RSE episodes treated with lacosamide (50% non-convulsive, 31% focal, and 19% convulsive SE). The overall success rate was 56%; adverse events (mostly mild and transient) were described in 25% of patients, but one subject presented a third-degree atrioventricular block and paroxysmal asystole [39]. A more recent systematic literature review ranging from 2008 to 2016 reported 522 SE episodes in 486 patients of all ages, with a similar overall lacosamide efficacy (57%). The success appeared similar between generalized convulsive (61%) and non-convulsive SE (57%), but, surprisingly, was greater in focal motor SE (92%) [40].
A retrospective comparison between phenytoin and lacosamide in 46 patients reported a similar success rate (33% with lacosamide vs. 40% phenytoin), with 27% side effects in the phenytoin group and none with lacosamide. However, these treatments were applied after failure of benzodiazepines and levetiracetam, thus as an adjunctive second-line treatment [41]. A retrospective cohort study including 111 patients with RSE reported treatment with lacosamide in 53%. Whereas the mean number of AEDs, duration, severity, etiology of SE, and concomitant critical medical conditions did not differ between the patients with and without lacosamide, age tended to be higher, and mechanical ventilation or use of anesthetics tended to be less frequent in the lacosamide group. Lacosamide was considered efficacious in 51%, but without any significant difference between the lacosamide group and other medications (OR 2.34; 95% CI 0.5–10.1). After adjustment for age, mortality was significantly reduced in patients receiving lacosamide (OR 0.34; 95% CI 0.1–0.9; p = 0.035) [42].
In a proof-of-concept observational study in 16 elderly patients with post-stroke non-convulsive SE (NCSE), lacosamide was prescribed as first line due to contraindications to benzodiazepines or phenytoin; it was deemed effective in 50%, with no reported adverse events [43]. A multicentric Spanish prospective study including 34 patients with RSE (mostly symptomatic focal motor SE) reported a 67.4 % lacosamide success rate, with SE termination before 12 h in 50% [44].
Retrospective series (each with more than 30 patients with various types of SE) reported seizure cessation after lacosamide, respectively, in 44% [45], 67% [46], 70% [47], and 88% [48]. All demonstrated a higher SE termination rate when lacosamide was used earlier in the course of treatment. In contrast with these positive results, an observational study in nine patients with RSE reported no response to lacosamide, with one patient developing angioedema [49]. However, the dose range was 100–200 mg (infusion rate not mentioned), appearing much lower (at least by a factor of 2) than that usually given in SE. This might at least partially explain the poorer efficacy.
A prospective observational study including 25 patients reported a significantly higher degree of early response (< 3 h) and a trend towards higher overall response rate in patients treated with 400 mg over 200 mg intravenous lacosamide [50]. Interestingly, a recent assessment by our group, including 40 adults recruited at two centers, showed a responder rate of 40%; however, lacosamide serum levels after loading did not correlate with seizure control [51].
Evidence regarding lacosamide efficacy in SE is still somewhat limited: only retrospective series and small prospective observational studies with few patients are available. This is emphasized by the cited meta-analysis of AEDs in convulsive SE resistant to benzodiazepines, which concluded that data on lacosamide were insufficient [13].
2.3 Brivaracetam
Brivaracetam is the latest approved AED in Europe and the USA, with a considerably higher affinity to the SV2A than levetiracetam [52]. Its favorable safety profile and pharmacokinetic properties, including the ability to cross the blood–brain barrier faster than levetiracetam, suggest it may represent a good alternative in SE [32]. Furthermore, in animal studies, brivaracetam showed a marked synergism with benzodiazepines [53, 54]. However, to date, literature on its prescription in SE is sparse. A German multicenter series including 11 adults with RSE and SRSE described seizure cessation within 24 h after brivaracetam utilization in 27% [55], and an Austrian study of seven patients with RSE reported immediate clinical improvement after brivaracetam administration in two, and immediate electrophysiological improvement in three patients [56].
Brivaracetam is the newest compound and, despite a promising profile, evidence in SE is still needed, as only two retrospective studies (with 18 patients in total) are available.
3 Newer AEDs: Oral Administration
Intravenous administration may not always be mandatory in RSE [57], especially outside an intensive care setting; AEDs administered orally or via nasogastric tube may represent a possible add-on option in some situations. Few newer AEDs have been described in this setting; however, to our knowledge, no comparative studies have been conducted with these compounds, which have essentially been described as additional second-line options.
3.1 Topiramate
Topiramate is a broad-spectrum drug with multiple mechanisms of action, including activity on sodium and calcium channels, carboanhydrase inhibition, and α-amino-3 hydroxy-5 methy-l-4-isoxazole-propionic acid (AMPA) antagonismus [58]; the latter may prove interesting given the pathophysiology of SE (see Sect. 3.3). Several case series have reported successful RSE termination after topiramate administration [59,60,61,62,63]. A more recent study in 17 patients with RSE showed SE cessation in all patients (!) treated with topiramate; while univariate analyses suggest it was more frequently used in younger and healthier patients, topiramate was not independently associated with RSE cessation in the multivariate assessment [64].
3.2 Pregabalin
Pregabalin is an AED that mostly acts through calcium channel modulation and represents an interesting option, especially for polymorbid patients, as it has good oral bioavailability, no drug interactions (together with gabapentin, it is virtually the only AED entirely renally excreted and lacking any metabolism), and can also be titrated quickly in inpatients [59]. A retrospective study including 11 SE episodes, mostly focal RSE, reported a definite electroclinical response in five, and a possible response in three patients at 24 h. No side effects were reported [65]. A more recent study in 21 patients with non-convulsive repetitive seizures or SE described a 52% responder rate after pregabalin; this proved much higher in repetitive seizures (82%) than in SE (18%) [66].
3.3 Perampanel
Imbalance between glutamate excitatory neurotransmission and gamma-aminobutyric acid (GABA) inhibition has been postulated as one of the underlying mechanisms of seizure continuation in SE. In RSE, postsynaptic GABAA receptors are internalized to the cytoplasm, and glutamate receptors are externalized in the synaptic membrane [67, 68]. As a noncompetitive AMPA receptor antagonist, perampanel might be an interesting approach in RSE, as it is more specific than topiramate. However, its extensive hepatic metabolism and high protein binding presents a potentially concerning interaction potential, which may render its use more difficult in patients receiving polymedication [69].
Data for perampanel in SE remain anecdotal; so far, only a few case reports or series are available [70,71,72]. A retrospective study in 12 patients with various RSE types reported a clinical improvement at 24 h in one patient and at 72 h in another (16%); no adverse effects were noted [71]. Retrospective analysis of ten patients with RSE (non-convulsive or focal SE without consciousness impairment) found that perampanel was efficacious in two to six episodes, depending on assessment criteria [70]. It is also interesting to note that perampanel may exert antimyoclonic activity [73, 74]; however, to date, we are unaware of any literature on its use in myoclonic SE.
Evidence of AEDs without intravenous formulations is still anecdotal. However, their pharmacokinetic properties mean they might represent an interesting alternative, especially as additional second-line drugs in elderly or critically ill patients, or in SE forms that do not necessarily require general anesthesia.
4 Other Treatments (Ketogenic Diet, Stiripentol, Allopregnanolone, Ketamine)
In RSE and SRSE, further therapeutic options may be considered. A ketogenic diet, a long-used treatment that is mostly used in pediatric patients with severe pharmaco-resistant epilepsy, also seems promising in adults with SE. As an example, a recent retrospective case review of ten patients described, despite prolonged SE duration, a 90% SE resolution within a median of 3 days [75].
Stiripentol is typically prescribed in conjunction with valproate and benzodiazepines in patients with Dravet syndrome. A retrospective study in five patients with SRSE suggested that it could be of some value in this context [76]. However, despite promising previous experimental animal data, evidence concerning its utilization in human SE is still extremely limited.
Allopregnanolone is a neuro-steroid, a natural metabolite of progesterone, that allosterically enhances the activity of GABA receptors. Despite an encouraging multicenter phase I/II trial, a phase III randomized controlled trial failed to prove its efficacy in SRSE [77, 78].
Ketamine, an N-methyl-D-aspartate (NMDA) antagonist, is also receiving increasing attention in this clinical setting. Its favorable cardiovascular profile, and in view of SE pathophysiology (see Sect. 3.3), means it might represent a useful addition to the anesthetic armamentarium in patients with RSE and SRSE [79, 80].
5 Pearls and Pitfalls of the Use of Newer AEDs in Status Epilepticus
More than two dozen AEDs are available on the market, but evidence regarding SE treatment is still considerably limited. High-class evidence is currently only available for the early stage of SE treatment (i.e., benzodiazepines). In the later SE stages, where newer AEDs are prescribed as second-line treatment (initially, or as additional compounds, as well as adjuncts to general anesthesia), there is only low-level evidence. This clinical situation represents an interesting paradox, where physicians can choose among a large variety of treatments in the absence of rational evidence and even official indications, whereas, at the same time, prospective studies appear extremely difficult to perform. It should also be emphasized that the costs of newer AEDs, although varying across countries, are several times those of traditional AEDs, particularly considering the oral forms (as the reimbursement values of intravenous formulations are generally similar for both newer and traditional compounds). The higher costs of the newer compounds may admittedly have a relatively limited financial impact in well-resourced settings, but could represent an additional, poorly studied burden in resource-limited regions. Table 2 summarizes considerations regarding pros and cons of the use of newer and traditional AEDs.
Data supporting prescription of newer AEDs in SE are, as we have seen, essentially based on case series or mostly low-quality randomized studies. We identified only five randomized controlled trials, all focusing on levetiracetam [22,23,24,25, 31]. Except the French study reporting no advantage after addition of levetiracetam to clonazepam in prehospital convulsive SE [31], these trials present several methodological issues. Levetiracetam was used as first- or second-line treatment, with different doses or infusion rates, different definitions of SE cessation, major population heterogeneity, inclusion of repetitive seizures together with SE, and specific geographic settings where infectious etiology predominates. Furthermore, the sample size was often based on feasibility rather than pre-defined assumptions, leading to insufficient statistical power. Retrospectively assessing the exact time of SE cessation, especially in RSE, is admittedly difficult, and—to this day—no consensus exists on efficacy criteria in this particular field. Many studies did not confirm SE cessation with continuous electroencephalogram (EEG) monitoring, which may have led to misrecognition of non-convulsive SE. A German study nicely illustrates this point, showing markedly different perampanel efficacies according to the chosen criterion [70]. In addition, the studied cohorts are often poorly representative of the general SE population. Authors often state that newer AEDs were prescribed because standard treatment was contraindicated or considered inappropriate, without further details. Outside randomized trials, a selection bias might be present towards prescription of newer AEDs in more severe SE or in older patients with more comorbidities. In addition, in clinical practice, second-line treatments are often given shortly after benzodiazepines to prevent seizure recurrence, which may lead to an overestimation of efficacy in retrospective studies. Furthermore, the loading and maintenance doses vary considerably between and within the studies, greatly limiting their comparability.
It is intriguing that very few severe adverse events are reported after administration of newer AEDs, whereas comparative studies relate a higher rate of relevant treatment-related adverse events with traditional AEDs (especially phenytoin) [41]. This might explain the current tendency to prefer newer AEDs (especially levetiracetam) in SE [6, 7]. Some studies suggest that, despite their supposed “safe” profile, newer AEDs have a possible lower efficacy as a whole [6, 7, 41]. Previous assessments from our group, occurring at different time points, reported associations between newer AEDs and greater disability at hospital discharge and higher rates of refractory SE [6, 7]. This is partly mirrored in a German study, which showed a similar efficacy of lacosamide and phenytoin in controlling RSE; however, patients receiving lacosamide showed a tendency towards higher rates of disability at discharge. Since there was a preferential treatment with phenytoin in patients with convulsive SE and acute etiologies (possibly linked to higher risk of morbidity and mortality), whereas lacosamide was used more frequently in NCSE (supposedly less severe if focal), a selection bias could be argued [41]. One study revealed decreased mortality in RSE treated with lacosamide after adjustment for age, but this might be confounded by the implementation of continuous EEG monitoring 6 months before the first use of lacosamide; furthermore, the use of anesthetics and mechanical ventilation was less frequent in patients with lacosamide [42]. As therapeutic coma has been potentially associated with greater mortality, this might account for the lower fatality rate in the lacosamide group [81,82,83].
Few papers report differences in efficacy between AEDs; however, they usually do not identify differences in mortality or disability, suggesting that “treatable” SE will be controlled by subsequent compounds [24, 28]. These findings underlie the fact that various factors, especially age and etiology, seem to contribute to the SE prognosis more than specific AED choices or dosages [84,85,86,87]. Furthermore, as newer AEDs are not yet officially approved for SE treatment, most studies used them as adjunctive therapy in RSE. This might have led to an underestimation of their efficacy in this setting, as AEDs used later in the succession of drugs are often less effective [67]. For example, as stated, several studies have described a significantly lower success rate for lacosamide with later positioning [41, 44, 46].
6 Conclusion
Despite their promising profile in terms of tolerability, with few centrally depressive effects and a low drug interaction potential, no tangible beneficial impact on outcome has yet been demonstrated for newer AEDs in SE. As most studies on AEDs focus on seizure cessation, very little data on long-term outcomes or morbidity are available. Studies with these endpoints are critically needed to help clinicians choose one compound over another. Of note, pharmacological information regarding tolerability are mostly derived from regulatory randomized trials in patients with pharmaco-resistant epilepsy that are unlikely to be automatically applicable to subjects with SE.
The lack of good-quality randomized trials prevents any strong recommendation regarding the prescription of newer AEDs in SE, which conversely has a definite economic impact (newer AEDs being more expensive than traditional ones). Further studies are thus clearly required to clarify their indication and adequate use in SE. Hopefully, results from the ESETT-trial, an ongoing, adequately powered, and carefully designed, randomized, double-blind study comparing fosphenytoin, levetiracetam, and valproate (unfortunately not lacosamide or brivaracetam), should eventually provide information regarding the relative efficacy and safety of these drugs [88]. For the time being, it is the opinion of the authors that clinicians should tailor the SE treatment strategy to each patient, considering the efficacy spectrum, the potential for adverse events and pharmacokinetic interactions, and financial impact. In several cases, traditional AEDs may still prove more adequate than newer ones.
References
Betjemann JP, Lowenstein DH. Status epilepticus in adults. Lancet Neurol. 2015;14(6):615–24.
Meierkord H, Boon P, Engelsen B, Gocke K, Shorvon S, Tinuper P, et al. EFNS guideline on the management of status epilepticus in adults. Eur J Neurol. 2010;17(3):348–55.
Lowenstein DH, Bleck T, Macdonald RL. It’s time to revise the definition of status epilepticus. Epilepsia. 1999;40(1):120–2.
Trinka E, Cock H, Hesdorffer D, Rossetti AO, Scheffer IE, Shinnar S, et al. A definition and classification of status epilepticus—report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. 2015;56(10):1515–23.
Delaj L, Novy J, Ryvlin P, Marchi NA, Rossetti AO. Refractory and super-refractory status epilepticus in adults: a 9-year cohort study. Acta Neurol Scand. 2017;135(1):92–9.
Beuchat I, Novy J, Rossetti AO. Newer antiepileptic drugs in status epilepticus: prescription trends and outcomes in comparison with traditional agents. CNS Drugs. 2017;31(4):327–34.
Jaques L, Rossetti AO. Newer antiepileptic drugs in the treatment of status epilepticus: impact on prognosis. Epilepsy Behav E&B. 2012;24(1):70–3.
Rossetti AO. Are newer AEDs better than the classic ones in the treatment of status epilepticus? J Clin Neurophysiol. 2016;33(1):18–21.
Glauser T, Ben-Menachem E, Bourgeois B, Cnaan A, Guerreiro C, Kalviainen R, et al. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2013;54(3):551–63.
Brophy GM, Bell R, Claassen J, Alldredge B, Bleck TP, Glauser T, et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23.
Claassen J, Riviello JJ Jr, Silbergleit R. Emergency neurological life support: status epilepticus. Neurocrit Care. 2015;23(Suppl 2):S136–42.
Glauser T, Shinnar S, Gloss D, Alldredge B, Arya R, Bainbridge J, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the Guideline Committee of the American Epilepsy Society. Epilepsy Curr/Am Epilepsy Soc. 2016;16(1):48–61.
Yasiry Z, Shorvon SD. The relative effectiveness of five antiepileptic drugs in treatment of benzodiazepine-resistant convulsive status epilepticus: a meta-analysis of published studies. Seizure J Br Epilepsy Assoc. 2014;23(3):167–74.
Misra UK, Kalita J. A comparison of four antiepileptic drugs in status epilepticus: experience from India. Int J Neurosci. 2016;126(11):1013–9.
Knake S, Gruener J, Hattemer K, Klein KM, Bauer S, Oertel WH, et al. Intravenous levetiracetam in the treatment of benzodiazepine refractory status epilepticus. J Neurol Neurosurg Psychiatry. 2008;79(5):588–9.
Rossetti AO, Bromfield EB. Levetiracetam in the treatment of status epilepticus in adults: a study of 13 episodes. Eur Neurol. 2005;54(1):34–8.
Ruegg S, Naegelin Y, Hardmeier M, Winkler DT, Marsch S, Fuhr P. Intravenous levetiracetam: Treatment experience with the first 50 critically ill patients. Epilepsy Behav E&B. 2008;12(3):477–80.
Ramael S, Daoust A, Otoul C, Toublanc N, Troenaru M, Lu ZS, et al. Levetiracetam intravenous infusion: a randomized, placebo-controlled safety and pharmacokinetic study. Epilepsia. 2006;47(7):1128–35.
Ramael S, De Smedt F, Toublanc N, Otoul C, Boulanger P, Riethuisen JM, et al. Single-dose bioavailability of levetiracetam intravenous infusion relative to oral tablets and multiple-dose pharmacokinetics and tolerability of levetiracetam intravenous infusion compared with placebo in healthy subjects. Clin Ther. 2006;28(5):734–44.
Trinka E. What is the evidence to use new intravenous AEDs in status epilepticus? Epilepsia. 2011;52(Suppl 8):35–8.
Trinka E, Dobesberger J. New treatment options in status epilepticus: a critical review on intravenous levetiracetam. Ther Adv Neurol Disord. 2009;2(2):79–91.
Chakravarthi S, Goyal MK, Modi M, Bhalla A, Singh P. Levetiracetam versus phenytoin in management of status epilepticus. J Clin Neurosci. 2015;22(6):959–63.
Gujjar AR, Nandhagopal R, Jacob PC, Al-Hashim A, Al-Amrani K, Ganguly SS, et al. Intravenous levetiracetam vs phenytoin for status epilepticus and cluster seizures: a prospective, randomized study. Seizure. 2017;49:8–12.
Misra UK, Kalita J, Maurya PK. Levetiracetam versus lorazepam in status epilepticus: a randomized, open labeled pilot study. J Neurol. 2012;259(4):645–8.
Mundlamuri RC, Sinha S, Subbakrishna DK, Prathyusha PV, Nagappa M, Bindu PS, et al. Management of generalised convulsive status epilepticus (SE): a prospective randomised controlled study of combined treatment with intravenous lorazepam with either phenytoin, sodium valproate or levetiracetam—pilot study. Epilepsy Res. 2015;114:52–8.
Brigo F, Bragazzi N, Nardone R, Trinka E. Direct and indirect comparison meta-analysis of levetiracetam versus phenytoin or valproate for convulsive status epilepticus. Epilepsy Behav. 2016;64(Pt A):110–5.
Zelano J, Kumlien E. Levetiracetam as alternative stage two antiepileptic drug in status epilepticus: a systematic review. Seizure. 2012;21(4):233–6.
Alvarez V, Januel JM, Burnand B, Rossetti AO. Second-line status epilepticus treatment: comparison of phenytoin, valproate, and levetiracetam. Epilepsia. 2011;52(7):1292–6.
Eue S, Grumbt M, Muller M, Schulze A. Two years of experience in the treatment of status epilepticus with intravenous levetiracetam. Epilepsy Behav. 2009;15(4):467–9.
De Smedt T, Raedt R, Vonck K, Boon P. Levetiracetam: part II, the clinical profile of a novel anticonvulsant drug. CNS Drug Rev. 2007;13(1):57–78.
Navarro V, Dagron C, Elie C, Lamhaut L, Demeret S, Urien S, et al. Prehospital treatment with levetiracetam plus clonazepam or placebo plus clonazepam in status epilepticus (SAMUKeppra): a randomised, double-blind, phase 3 trial. Lancet Neurol. 2016;15(1):47–55.
Nicolas JM, Hannestad J, Holden D, Kervyn S, Nabulsi N, Tytgat D, et al. Brivaracetam, a selective high-affinity synaptic vesicle protein 2A (SV2A) ligand with preclinical evidence of high brain permeability and fast onset of action. Epilepsia. 2016;57(2):201–9.
Cawello W. Clinical pharmacokinetic and pharmacodynamic profile of lacosamide. Clin Pharmacokinet. 2015;54(9):901–14.
Cawello W, Stockis A, Andreas JO, Dimova S. Advances in epilepsy treatment: lacosamide pharmacokinetic profile. Ann N Y Acad Sci. 2014;1329:18–32.
Chung SS. Lacosamide: new adjunctive treatment option for partial-onset seizures. Expert Opin Pharmacother. 2010;11(9):1595–602.
Kellinghaus C. Lacosamide as treatment for partial epilepsy: mechanisms of action, pharmacology, effects, and safety. Ther Clin Risk Manag. 2009;5:757–66.
Brigo F, Trinka E. Randomized controlled trials in status epilepticus: Size matters. Epilepsia. 2017;58(5):915.
Misra UK, Dubey D, Kalita J. A randomized controlled trial of lacosamide versus sodium valproate in status epilepticus. Epilepsia. 2017.
Hofler J, Trinka E. Lacosamide as a new treatment option in status epilepticus. Epilepsia. 2013;54(3):393–404.
Strzelczyk A, Zollner JP, Willems LM, Jost J, Paule E, Schubert-Bast S, et al. Lacosamide in status epilepticus: systematic review of current evidence. Epilepsia. 2017;58(6):933–50.
Kellinghaus C, Berning S, Stogbauer F. Intravenous lacosamide or phenytoin for treatment of refractory status epilepticus. Acta Neurol Scand. 2014;129(5):294–9.
Sutter R, Marsch S, Ruegg S. Safety and efficacy of intravenous lacosamide for adjunctive treatment of refractory status epilepticus: a comparative cohort study. CNS Drugs. 2013;27(4):321–9.
Belcastro V, Vidale S, Pierguidi L, Sironi L, Tancredi L, Striano P, et al. Intravenous lacosamide as treatment option in post-stroke non convulsive status epilepticus in the elderly: a proof-of-concept, observational study. Seizure. 2013;22(10):905–7.
Miro J, Toledo M, Santamarina E, Ricciardi AC, Villanueva V, Pato A, et al. Efficacy of intravenous lacosamide as an add-on treatment in refractory status epilepticus: a multicentric prospective study. Seizure J Br Epilepsy Assoc. 2013;22(1):77–9.
Kellinghaus C, Berning S, Immisch I, Larch J, Rosenow F, Rossetti AO, et al. Intravenous lacosamide for treatment of status epilepticus. Acta Neurol Scand. 2011;123(2):137–41.
Santamarina E, Toledo M, Sueiras M, Raspall M, Ailouti N, Lainez E, et al. Usefulness of intravenous lacosamide in status epilepticus. J Neurol. 2013;260(12):3122–8.
Garces M, Villanueva V, Mauri JA, Suller A, Garcia C, Lopez Gonzalez FJ, et al. Factors influencing response to intravenous lacosamide in emergency situations: LACO-IV study. Epilepsy Behav. 2014;36:144–52.
Hofler J, Unterberger I, Dobesberger J, Kuchukhidze G, Walser G, Trinka E. Intravenous lacosamide in status epilepticus and seizure clusters. Epilepsia. 2011;52(10):e148–52.
Goodwin H, Hinson HE, Shermock KM, Karanjia N, Lewin JJ 3rd. The use of lacosamide in refractory status epilepticus. Neurocrit Care. 2011;14(3):348–53.
Legros B, Depondt C, Levy-Nogueira M, Ligot N, Mavroudakis N, Naeije G, et al. Intravenous lacosamide in refractory seizure clusters and status epilepticus: comparison of 200 and 400 mg loading doses. Neurocrit Care. 2014;20(3):484–8.
Perrenoud M, Andre P, Alvarez V, Stahli C, Decosterd LA, Rossetti AO, et al. Intravenous lacosamide in status epilepticus: correlation between loading dose, serum levels, and clinical response. Epilepsy Res. 2017;135:38–42.
Gillard M, Fuks B, Leclercq K, Matagne A. Binding characteristics of brivaracetam, a selective, high affinity SV2A ligand in rat, mouse and human brain: relationship to anti-convulsant properties. Eur J Pharmacol. 2011;664(1–3):36–44.
Niquet J, Suchomelova L, Thompson K, Klitgaard H, Matagne A, Wasterlain C. Acute and long-term effects of brivaracetam and brivaracetam-diazepam combinations in an experimental model of status epilepticus. Epilepsia. 2017;58(7):1199–207.
Wasterlain CG, Baldwin R, Naylor DE, Thompson KW, Suchomelova L, Niquet J. Rational polytherapy in the treatment of acute seizures and status epilepticus. Epilepsia. 2011;52(Suppl 8):70–1.
Strzelczyk A, Steinig I, Willems LM, Reif PS, Senft C, Voss M, et al. Treatment of refractory and super-refractory status epilepticus with brivaracetam: a cohort study from two German university hospitals. Epilepsy Behav. 2017;70(Pt A):177–81.
Kalss GRA, Leitinger M, Georg P, Novak H, Neuray C, Kreidenhuber R, Höfler J, Kuchukhidze G, Trinka E. Intravenous Brivaracetam in Status epilepticus—a retrospectie single centre study. Epilepsia. 2018 (in press).
Novy J, Logroscino G, Rossetti AO. Refractory status epilepticus: a prospective observational study. Epilepsia. 2010;51(2):251–6.
Garnett WR. Clinical pharmacology of topiramate: a review. Epilepsia. 2000;41(Suppl 1):S61–5.
Bensalem MK, Fakhoury TA. Topiramate and status epilepticus: report of three cases. Epilepsy Behav. 2003;4(6):757–60.
Hottinger A, Sutter R, Marsch S, Ruegg S. Topiramate as an adjunctive treatment in patients with refractory status epilepticus: an observational cohort study. CNS Drugs. 2012;26(9):761–72.
Stojanova V, Rossetti AO. Oral topiramate as an add-on treatment for refractory status epilepticus. Acta Neurol Scand. 2012;125(2):e7–11.
Synowiec AS, Yandora KA, Yenugadhati V, Valeriano JP, Schramke CJ, Kelly KM. The efficacy of topiramate in adult refractory status epilepticus: experience of a tertiary care center. Epilepsy Res. 2012;98(2–3):232–7.
Towne AR, Garnett LK, Waterhouse EJ, Morton LD, DeLorenzo RJ. The use of topiramate in refractory status epilepticus. Neurology. 2003;60(2):332–4.
Madzar D, Kuramatsu JB, Gerner ST, Huttner HB. Assessing the value of topiramate in refractory status epilepticus. Seizure. 2016;38:7–10.
Novy J, Rossetti AO. Oral pregabalin as an add-on treatment for status epilepticus. Epilepsia. 2010;51(10):2207–10.
Swisher CB, Doreswamy M, Husain AM. Use of pregabalin for nonconvulsive seizures and nonconvulsive status epilepticus. Seizure. 2013;22(2):116–8.
Chen JW, Wasterlain CG. Status epilepticus: pathophysiology and management in adults. Lancet Neurol. 2006;5(3):246–56.
Naylor DE, Liu H, Wasterlain CG. Trafficking of GABA(A) receptors, loss of inhibition, and a mechanism for pharmacoresistance in status epilepticus. J Neurosci. 2005;25(34):7724–33.
Patsalos PN. The clinical pharmacology profile of the new antiepileptic drug perampanel: a novel noncompetitive AMPA receptor antagonist. Epilepsia. 2015;56(1):12–27.
Redecker J, Wittstock M, Benecke R, Rosche J. Efficacy of perampanel in refractory nonconvulsive status epilepticus and simple partial status epilepticus. Epilepsy Behav. 2015;45:176–9.
Rohracher A, Hofler J, Kalss G, Leitinger M, Kuchukhidze G, Deak I, et al. Perampanel in patients with refractory and super-refractory status epilepticus in a neurological intensive care unit. Epilepsy Behav. 2015;49:354–8.
Rosche J, Kampf C, Benecke R. Possible effect of perampanel on focal status epilepticus after generalized tonic-clonic status epilepticus. Acta Neurol Belg. 2014;114(3):243–4.
Santamarina E, Sueiras M, Lidon RM, Guzman L, Baneras J, Gonzalez M, et al. Use of perampanel in one case of super-refractory hypoxic myoclonic status: Case report. Epilepsy Behav Case Rep. 2015;4:56–9.
Steinhoff BJ, Bacher M, Kurth C, Staack AM, Kornmeier R. Add-on perampanel in Lance-Adams syndrome. Epilepsy Behav Case Rep. 2016;6:28–9.
Thakur KT, Probasco JC, Hocker SE, Roehl K, Henry B, Kossoff EH, et al. Ketogenic diet for adults in super-refractory status epilepticus. Neurology. 2014;82(8):665–70.
Strzelczyk A, Kortland LM, Knake S, Rosenow F. Stiripentol for the treatment of super-refractory status epilepticus. Acta Neurol Scand. 2015;132(6):435–9.
Rosenthal ES, Claassen J, Wainwright MS, Husain AM, Vaitkevicius H, Raines S, et al. Brexanolone as adjunctive therapy in super-refractory status epilepticus. Ann Neurol. 2017;82(3):342–52.
Erstad BL, Patanwala AE. Ketamine for analgosedation in critically ill patients. J Crit Care. 2016;35:145–9.
Gaspard N, Foreman B, Judd LM, Brenton JN, Nathan BR, McCoy BM, et al. Intravenous ketamine for the treatment of refractory status epilepticus: a retrospective multicenter study. Epilepsia. 2013;54(8):1498–503.
Litt B, Wityk RJ, Hertz SH, Mullen PD, Weiss H, Ryan DD, et al. Nonconvulsive status epilepticus in the critically ill elderly. Epilepsia. 1998;39(11):1194–202.
Marchi NA, Novy J, Faouzi M, Stahli C, Burnand B, Rossetti AO. Status epilepticus: impact of therapeutic coma on outcome. Crit Care Med. 2015;43(5):1003–9.
Sutter R, Marsch S, Fuhr P, Kaplan PW, Ruegg S. Anesthetic drugs in status epilepticus: risk or rescue? A 6-year cohort study. Neurology. 2014;82(8):656–64.
Logroscino G, Hesdorffer DC, Cascino G, Annegers JF, Hauser WA. Short-term mortality after a first episode of status epilepticus. Epilepsia. 1997;38(12):1344–9.
Rossetti AO, Alvarez V, Januel JM, Burnand B. Treatment deviating from guidelines does not influence status epilepticus prognosis. J Neurol. 2013;260(2):421–8.
Towne AR, Pellock JM, Ko D, DeLorenzo RJ. Determinants of mortality in status epilepticus. Epilepsia. 1994;35(1):27–34.
Rossetti AO, Hurwitz S, Logroscino G, Bromfield EB. Prognosis of status epilepticus: role of aetiology, age, and consciousness impairment at presentation. J Neurol Neurosurg Psychiatry. 2006;77(5):611–5.
Bleck T, Cock H, Chamberlain J, Cloyd J, Connor J, Elm J, et al. The established status epilepticus trial 2013. Epilepsia. 2013;54(Suppl 6):89–92.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to prepare this manuscript.
Conflict of interest
I. Beuchat, J. Novy, and A.O. Rossetti have no conflicts of interest that are directly related to the content of this manuscript.
Rights and permissions
About this article
Cite this article
Beuchat, I., Novy, J. & Rossetti, A.O. Newer Antiepileptic Drugs for Status Epilepticus in Adults: What’s the Evidence?. CNS Drugs 32, 259–267 (2018). https://doi.org/10.1007/s40263-018-0509-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-018-0509-5