Abstract
Parkinson’s disease (PD) is the second most common neurodegenerative disorder, after Alzheimer’s disease, affecting the elderly worldwide. Current therapy for PD is largely based on prescription of drugs that act as either dopamine precursors, dopamine agonists or agents that inhibit key enzymes in the dopamine catabolic pathways. Most of these drugs are administered in tablet or capsule form and can involve multiple daily doses in complex dosing regimens, which contributes to sub-optimal compliance amongst patients. There is evidence to suggest that non-compliance with medications results in perceived poor response to therapy and may ultimately increase direct and indirect health care costs. Medication compliance in PD assumes a particularly important role, given that PD is a progressive, debilitating condition, and once medication is instituted for ameliorating the symptoms of PD, it is lifelong. We included nine research studies in our review of the medical literature, which report the prevalence of significant medication non-compliance in PD, using standard definitions, varies between 10 and 67 %. This variation partly reflects differences in defining what clinically significant medication adherence is, the methods used to estimate the scale of the problem and the underlying population heterogeneity. Nevertheless, medication adherence is related to health costs and to the quality of life of patients affected by PD and, indirectly, their carers. Educating patients and their carers is one method of improving patient adherence to therapy. Simplifying drug regimens can also aid in this effort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Medication adherence or compliance is sub-optimal in a significant proportion of patients with Parkinson’s disease. |
Non-compliance with prescribed anti-parkinsonian therapy is associated with a greater disease burden and higher overall health care costs. |
The predictors of non-compliance are longer disease duration, poor knowledge of Parkinson’s disease, risk behaviours (alcohol, novelty seeking) and complex drug regimens. |
Drug regimens that are simpler and that have fewer daily doses offer the prospect of better therapy adherence. |
1 Introduction
‘Medication compliance’ or ‘medication adherence’—two terms with similar meanings in this context—is a hotly debated topic across the spectrum of human chronic diseases, including Parkinson’s disease (PD), and several research groups have analysed this problem.
When compliance is being assessed, the main issues are that compliance should be defined clearly, distinguishing between the various forms of non-compliance; that the methods of measuring compliance should be explicit and robust; and that a clear explanation of the impact of non-compliance on the patient and overall on society is provided, such that the problem can be adequately addressed [1].
Compliance can be defined as the extent to which a patient acts in accordance with the recommended intervals and doses of a drug regimen prescribed by a health care provider [2]. Non-compliance, in the broadest terms, can therefore be defined as any deviation from the recommended timings or dosages of a prescribed regimen. On the basis of this definition, non-compliance can include several subtypes, including overuse and abuse, forgetting to take medications, and alteration of medication schedules and doses [3].
Dose compliance (the doses of medication taken, compared with the doses prescribed) can be estimated in several ways, including patient self-reporting, use of visual analogue scales, a simple tablet count at refills by the person dispensing the medication and electronic monitoring of medication bottle opening. The last of these methods is preferred in clinical trials, as it can be used to monitor not only daily compliance (the percentage of days on which the correct number of doses are taken) but also timing compliance (the percentage of doses taken at the correct time interval). Self-reporting is insensitive in detecting sub-optimal PD medication intake, as there is considerable under-reporting by patients; therefore, objective methods such as electronic monitoring systems are also preferred to estimate the burden of the problem in the community [4].
Measurement of therapy adherence over more prolonged periods makes use of the medication possession ratio (MPR). MPR can be estimated as the number of days’ supply of medication dispensed during a specified follow-up period (e.g. 1 year) divided by the number of days from the first dispensing to the end of the follow-up period [10]. The definition and methods of estimation of MPR, though, have not been uniform across studies, and other measures of compliance have also been used. Various terms—such as ‘adherence ratio’, ‘refill adherence’, ‘compliance rate’, ‘adherence index’, ‘compliance ratio’ and ‘compliance index’—have been used for this purpose in different studies, hindering direct comparisons between studies [5].
It is generally considered that sub-optimal compliance becomes clinically significant when <80 % of prescribed medication is taken (MPR <0.8), but this level is somewhat arbitrary. However, comparison of the 80 % level with an exploratory level of 70 % did not affect the interpretation of the findings in one study in PD [6].
The aims of this review are to summarize the clinical and demographic factors associated with medication non-adherence in patients with PD, discuss the cost implications of non-compliance and assess evidence for intervention strategies to remedy the problem.
2 Literature Search Methodology
We identified relevant studies of the prevalence of medication adherence in PD by searching Medline (from 1946 to 31 July 2014), Embase (from 1947 to 31 July 2014) and the Cochrane Library (from 1946 to 31 July 2014), by combining the two Medical Subject Heading (MeSH) terms ‘medication adherence’ and ‘Parkinson’s disease’ with the Boolean operator ‘AND’. Separate searches were conducted combining the two MeSH terms ‘medication compliance’ and ‘Parkinson’s disease’ with the Boolean operator ‘AND’. The search strategies that were used limited the search to human studies and papers published in the English language, and duplicate entries that came up were then removed from the database searches. Hand searches were performed using the references provided in the papers obtained from the electronic search. The abstracts that were identified were read, examined and matched to pre-defined inclusion and exclusion criteria. The inclusion criteria were pre-defined as those studies that involved community-dwelling patients with idiopathic PD, specifically assessed medication adherence or compliance in PD, and involved ten or more subjects with PD. Abstracts as conference proceedings only, letters to the editor, case reports and case series involving fewer than ten subjects were excluded, as were studies assessing patients with Parkinson-plus syndromes, secondary parkinsonism, vascular parkinsonism or drug-induced parkinsonism. As there is a recent systematic review on this topic [7], we did not replicate that methodology and thereby restricted the scope of this paper. This is a broader narrative review of the topic.
3 Literature Search Results
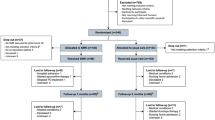
There were 41 abstracts identified by the electronic search strategy that was employed, combining the MeSH terms ‘medication adherence’ and ‘Parkinson’s disease’. An analogous electronic search strategy combining the MeSH terms ‘medication compliance’ and ‘Parkinson’s disease’ came up with 22 abstracts. Eight papers that met the inclusion criteria are included here, plus one additional paper that was identified during manual searches, making a total of nine studies in the review (Fig. 1; Table 1).
3.1 Epidemiology of Drug Compliance in PD
The reported prevalence of non-compliance or non-adherence to prescribed therapy in PD shows a lot of variation, depending upon the methodology that is employed to estimate the problem. In a recent systematic review of medication adherence in PD, six studies were identified [4, 8–12], each of which used a different methodology [7]. The rates of reported non-compliance range from 0 % according to patient self-reporting in clinical trials [4] to as high as 60–70 % according to pharmacy refill data and pill counts amongst community-dwelling patients, but this partly depends on the definition of adherence and the cut-off values used for defining significant non-adherence [9].
3.2 Predictors of Non-Compliance
The predictors of non-compliance in a large population-based study [13] included older age (≥65 years), the presence of multiple comorbidities and the occurrence of multiple changes in the patient’s anti-parkinsonian therapy. Surprisingly, in some studies, non-compliance has been greater in younger patients than in the elderly [11]. Factors such as knowledge of the disease, complexity of posology, stage of disease, disease comprehension, cognitive function and family support can also influence compliance [14] (Table 2).
Several medications can be prescribed for ameliorating the motor symptoms of PD, often in combination in the mid- to late stages of PD, and these have different administration and dosing schedules. Compliance with a single daily dose of a long-acting preparation of a dopamine agonist in the early stages of PD (e.g. prolonged-release ropinirole or pramipexole) may be straightforward, but in the later stages of PD when symptom control requires prescription of more than one drug with several daily doses, the resulting regimen complexity can make it difficult for patients to remain compliant with treatment [11].
Viewing non-adherence in the context of PD brings many of the pertinent factors into focus. First, polypharmacy is exceedingly common, with over half of patients taking at least two anti-parkinsonian drugs in addition to multiple prescriptions for non-motor manifestations of PD and other comorbidities [15]. Furthermore, dopaminergic drugs are often taken 3–4 times daily, with advanced PD patients taking as many as 6–10 doses per day. Greater regimen complexity is strongly correlated with non-adherence in PD [11, 16]. Once-daily drugs for PD have significantly better adherence than drugs prescribed more frequently [1]. This is consistent with the findings of a systematic review of chronic diseases in which adherence to therapy amongst patients was greatest in those prescribed once-daily formulations, compared with those prescribed twice-daily or thrice-daily formulations. For studies comparing once-daily and twice-daily dosing, patients receiving once-daily dosing had 2–44 % more adherent days than those receiving twice-daily dosing. For studies comparing once-daily and thrice-daily dosing, patients receiving once-daily dosing had 22–41 % more adherent days than those receiving thrice-daily dosing, with most studies clustering around 13–26 % [17].
3.3 Drug-Specific Adherence Issues in PD
Levodopa is considered the gold standard for treating the dopamine deficiency state in PD. However, the levodopa plasma half-life is very short, requiring multiple daily doses to keep plasma levels therapeutic. Further, this multiple daily dosing results in marked plasma drug concentration fluctuations, which are matched, as the disease progresses, to swings in the therapeutic response (‘wearing off’ phenomena) [18]. After 5–10 years, the majority of patients suffer fluctuations, dyskinesia or loss of efficacy [19]. This can create problems with drug adherence. Few studies have compared adherence according to drug class or formulation. Several studies pre-dated the emergence of prolonged-release (once-daily) formulations of dopamine agonists, such as ropinirole and pramipexole, which are now often used first line in place of the immediate-release, thrice-daily equivalents [20, 21]. The use of long-acting, prolonged-release, once-daily preparations of dopamine agonists can theoretically increase patient adherence by simplification of the drug regimen. There is evidence of higher therapy compliance rates with cabergoline, another longer-acting, once-daily dopamine agonist, which was used in the past before the emergence of fibrotic reactions as a serious side effect came to light [11, 12]. In a multi-centre, European, prospective study involving 112 patients, compliance amongst all drug classes was greatest with cabergoline (n = 8). This was better than the compliance observed amongst those on thrice-daily dopamine agonists (n = 68) and levodopa (n = 90).
Another study using MPRs found greater compliance for once-daily rasagiline than for all other drug classes (all p < 0.001) but did not distinguish between dopamine agonists, comparing once-daily or more frequently administered formulations [22]. In this retrospective US database study of patients receiving a new PD drug between 1 March and 31 May 2007, of the 19,510 patients included, the greatest mean number of persistent days of treatment (147.5) was reported for rasagiline, followed by levodopa/carbidopa/entacapone (146.9); persistence for both of these drugs was significantly greater than persistence for the comparator medications (rasagiline versus levodopa/carbidopa: p = 0.002; rasagiline versus pramipexole: p = 0.003; rasagiline versus catechol-O-methyltransferase (COMT) inhibitors, ropinirole and selegiline: all p < 0.001; levodopa/carbidopa/entacapone versus levodopa/carbidopa: p = 0.005; levodopa/carbidopa/entacapone versus pramipexole: p = 0.006; levodopa/carbidopa/entacapone versus COMT inhibitors, ropinirole and selegiline: all p < 0.001).
In addition to the oral agents, rotigotine, used as a transdermal patch for once-daily application, may be beneficial to aid therapy compliance. In a large population-based study (n = 863), the majority of the patients either never or very rarely (1–2 times per month) forgot to apply the patch (97.3 %) or deviated by more than 4 h from the chosen application time (94.4 %) [23].
The concept of continuous dopaminergic stimulation is particularly relevant to the issues of therapy compliance in PD. In its ideal form, a drug with a very long half-life (or a drug administered by a continuous delivery mechanism) would maintain therapeutic pharmacokinetic levels 24 hours a day, thereby mimicking natural dopamine release. A lower incidence of dyskinesia and wearing off is associated with use of dopamine agonists, which have a much longer half-life than levodopa. Current evidence suggests that these motor complications in later stages of PD are associated with a non-physiological pulsatile release of dopamine or stimulation of dopamine receptors. In normal human brains, dopamine neurons fire continuously, striatal dopamine concentrations are relatively constant and there is continuous stimulation of dopamine receptors. In the dopamine-depleted state of PD, levodopa or other short-acting dopaminergic drugs induce altered neuronal firing patterns in basal ganglia neurons, leading to motor complications [24]. Continuous dopaminergic replacement not only limits their development in experimental models of PD but also partially reverses these complications in parkinsonian patients. Thus, pharmaceutical approaches that provide relatively continuous dopamine receptor stimulation might confer both prophylactic and palliative benefit for parkinsonian patients [25].
3.4 Optimizing Medication Intake in PD
Optimizing oral medication intake has a potential role in maximizing the therapeutic response in PD. For patients with PD, there is growing evidence to suggest that sub-optimal compliance is a contributing factor to the variable response to dopamine replacement therapy [26]. For example, a multi-centre, European study found that non-compliance with PD treatment was significantly associated with poor motor scores [on the Unified Parkinson’s Disease Rating Scale (UPDRS)], more daily ‘off’ time (from UPDRS part 4) and worse mobility [within the Parkinson’s Disease Quality Of Life Score (PDQ39)] in comparison with patients who demonstrated satisfactory compliance [12]. Further, non-compliance has been found to be associated with higher rates of depression and reduced quality of life [11].
3.5 Complications of Non-Compliance in PD
Non-compliance is common and can prove costly. The consequences of non-compliance for the individual patient may include withdrawal symptoms, which, in severe cases (with total cessation of therapy), can lead to Parkinson hyperpyrexia syndrome [27]. However, partial omission of therapy is much more common in PD patients than complete abandonment of therapy [12]. On the other hand, overdosing as a manifestation of non-compliance with prescribed therapy can lead to dyskinesia or psychiatric complications, such as hallucinations and psychosis, and is a key component of dopamine dysregulation syndrome [28].
3.6 Costs of Non-Compliance in PD
The impact of non-compliance in PD may extend beyond the detrimental effects on individual patients. Non-compliance is associated with an increased burden on health care systems because of greater resource usage in comparison with the compliant population [29], but it has not been shown that improvement of compliance translates into sustained health improvement and ongoing lower health care costs. It remains possible that sub-optimal adherence in patients with worse parkinsonian symptoms is, at least in part, inherent in the stage or type of PD, combined with the degree of their therapy responsiveness, i.e. it cannot be concluded that poor therapy adherence in PD is easily remediable.
Although the total mean drug costs will be higher for compliant patients than for non-compliant patients (driven mainly by the cost of PD medications), the mean costs associated with emergency room and inpatient visits are higher for patients who are less compliant with their prescribed medication. Overall, the total mean all-cause annual health care costs are lower for compliant patients than for non-compliant patients [29]. This finding has been replicated in a large population-based study of PD patients (n = 3,119) within a national database of US managed care plans of patients, which found that patients who were non-compliant with prescribed therapy had significantly higher rates of yearly hospitalizations, outpatient visits to physicians and ancillary care visits, with higher total medical costs despite lower prescription drug costs. The total mean health care costs, including both medical and pharmacy utilization, were $18,511 and $13,082 among non-adherers and adherers, respectively (p < 0.0001) [30]. On the other hand, it has been shown that greater adherence to PD medications (a higher MPR) and a longer duration of use of these medications are associated with lower all-cause health care utilization and lower total health care expenditure [31].
3.7 Aids to Improve Compliance in PD
Several interventions have been applied generally to patients with chronic diseases, in an attempt to improve patient compliance, and these can be applied to cases with PD. These methods include development of an individualized treatment plan that simplifies the complex drug regimen as far as possible [32]; clearly explaining beforehand about the possibility of side effects that can otherwise be surprising and off-putting to the patient [33]; providing compliance aids, such as medication calendars, or dispensing systems, such as blister packs/dosette boxes [32]; and tying the medication-taking process to other daily routines to improve timing compliance [34]. Problems with swallowing pills are prevalent in the elderly population, especially in patients with dysphagia [35], and alternative routes, such as transdermal delivery systems (for rotigotine), may help in this instance, just as they are useful in the peri-operative setting when patients are fasting [36]. However, the requirements of multiple drug classes in more advanced PD usually leave no option other than multiple daily dosing of the medications, taken orally. Educating patients and their carers, e.g. about the continuous dopaminergic hypothesis (to encourage regular medicine intake), has a modest effect in some patients, but it is not known if this is sustained [37]. Adherence therapy (AT) is a cognitive–behavioural therapy approach and has been implemented in patients with PD. Modifying beliefs and exploring ambivalence towards medication are key components of this approach. In a randomized, controlled trial involving 76 patients with PD (active:control ratio 1:1) and 46 spouses/carers, after 12 weeks, AT had significantly improved adherence (60.5 % of the active group improved in adherence, versus 15.8 % of the controls), compared with routine care (odds ratio 8.2; 95 % confidence interval 2.8–24.3) [38].
Addressing comorbidities that may contribute to non-adherence in PD is also of interest. Psychiatric and cognitive problems in PD are common in the later stages of PD [39, 40]. Patients with depression are three times more likely to have poor adherence than non-depressed patients [41], and PD patients with comorbid depression are more likely to have increased health service utilization than those without depression [42]. However, it has not been shown whether treatment of depression and other psychiatric comorbidities restores therapy adherence to higher levels.
Cognitive impairment can also influence medicine-taking behaviour. Cognitive impairment challenges patients’ ability to adhere to complex medication regimens, such as those typically prescribed in PD, particularly in older adults.
Finally, the very important contribution that carers of PD patients make to their wellbeing is recognized in supporting adherence to an appropriate medication prescription schedule [43], but, despite the best efforts to improve compliance for long-term care—including combinations of more convenient care, information, reminders, self-monitoring, reinforcement, counselling, family therapy, psychological therapy, crisis intervention, manual telephone follow-up and supportive care—one must recognize the inconvenient truth that sometimes these interventions may not lead to as huge improvements in adherence and treatment outcomes as one expects [44].
4 Conclusion
Adherence to therapy, medication dosage and timing is vital in the management of PD patients. Treatments that require fewer daily doses may have the potential to improve compliance, which, in turn, could reduce the economic burden associated with PD. Considering dopaminergic therapy as a ‘replacement’ treatment and attempting to mimic its tonic physiological release underpins the concept of good therapy adherence, both for total doses and for accurate medication timing in PD.
References
Hughes DA, et al. Accounting for noncompliance in pharmacoeconomic evaluations. Pharmacoeconomics. 2001;19(12):1185–97.
Cramer JA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7.
Salzman C. Medication compliance in the elderly. J Clin Psychiatry. 1995;56(Suppl 1):18–22 discussion 23.
Grosset KA, et al. Measuring therapy adherence in Parkinson’s disease: a comparison of methods. J Neurol Neurosurg Psychiatry. 2006;77(2):249–51.
Andrade SE, et al. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15(8):565–74 discussion 575–7.
Offord S, et al. Impact of oral antipsychotic medication adherence on healthcare resource utilization among schizophrenia patients with medicare coverage. Community Ment Health J. 2013;49(6):625–9.
Daley DJ, et al. Systematic review on factors associated with medication non-adherence in Parkinson’s disease. Parkinsonism Relat Disord. 2012;18(10):1053–61.
Valldeoriola F, et al. Socio-demographic and clinical factors influencing the adherence to treatment in Parkinson’s disease: the ADHESON study. Eur J Neurol. 2011;18(7):980–7.
Kulkarni AS, et al. Medication adherence and associated outcomes in Medicare health maintenance organization-enrolled older adults with Parkinson’s disease. Mov Disord. 2008;23(3):359–65.
Leopold NA, Polansky M, Hurka MR. Drug adherence in Parkinson’s disease. Mov Disord. 2004;19(5):513–7.
Grosset KA, Bone I, Grosset DG. Suboptimal medication adherence in Parkinson’s disease. Mov Disord. 2005;20(11):1502–7.
Grosset D, et al. Adherence to antiparkinson medication in a multicenter European study. Mov Disord. 2009;24(6):826–32.
Wei YJ, et al. Antiparkinson drug use and adherence in Medicare Part D beneficiaries with Parkinson’s disease. Clin Ther. 2013;35(10):1513–25 e1.
Sesar A, Arbelo JM, del Val JL. Treatment of Parkinson disease, time and dosage: “does simple dosage facilitate compliance and therapeutic goals?”. Neurologist. 2011;17(6 Suppl 1):S43–6.
Leoni O, et al. Drug prescribing patterns in Parkinson’s disease: a pharmacoepidemiological survey in a cohort of ambulatory patients. Pharmacoepidemiol Drug Saf. 2002;11(2):149–57.
Grosset KA, Reid JL, Grosset DG. Medicine-taking behavior: implications of suboptimal compliance in Parkinson’s disease. Mov Disord. 2005;20(11):1397–404.
Saini SD, et al. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22–33.
Contin M, Martinelli P. Pharmacokinetics of levodopa. J Neurol. 2010;257(Suppl 2):S253–61.
Marsden CD. Problems with long-term levodopa therapy for Parkinson’s disease. Clin Neuropharmacol. 1994;17(Suppl 2):S32–44.
Stocchi F, et al. Ropinirole 24-hour prolonged release and ropinirole immediate release in early Parkinson’s disease: a randomized, double-blind, non-inferiority crossover study. Curr Med Res Opin. 2008;24(10):2883–95.
Hametner EM, Seppi K, Poewe W. Role and clinical utility of pramipexole extended release in the treatment of early Parkinson’s disease. Clin Interv Aging. 2012;7:83–8.
Tarrants ML, et al. Drug therapies for Parkinson’s disease: a database analysis of patient compliance and persistence. Am J Geriatr Pharmacother. 2010;8(4):374–83.
Schnitzler A, Leffers KW, Hack HJ. High compliance with rotigotine transdermal patch in the treatment of idiopathic Parkinson’s disease. Parkinsonism Relat Disord. 2010;16(8):513–6.
Olanow CW, Obeso JA, Stocchi F. Continuous dopamine-receptor treatment of Parkinson’s disease: scientific rationale and clinical implications. Lancet Neurol. 2006;5(8):677–87.
Chase TN. The significance of continuous dopaminergic stimulation in the treatment of Parkinson’s disease. Drugs. 1998;55(Suppl 1):1–9.
Grosset D. Therapy adherence issues in Parkinson’s disease. J Neurol Sci. 2010;289(1–2):115–8.
Newman EJ, Grosset DG, Kennedy PG. The parkinsonism–hyperpyrexia syndrome. Neurocrit Care. 2009;10(1):136–40.
O’Sullivan SS, Evans AH, Lees AJ. Dopamine dysregulation syndrome: an overview of its epidemiology, mechanisms and management. CNS Drugs. 2009;23(2):157–70.
Richy FF, et al. Compliance with pharmacotherapy and direct healthcare costs in patients with Parkinson’s disease: a retrospective claims database analysis. Appl Health Econ Health Policy. 2013;11(4):395–406.
Davis KL, Edin HM, Allen JK. Prevalence and cost of medication nonadherence in Parkinson’s disease: evidence from administrative claims data. Mov Disord. 2010;25(4):474–80.
Wei YJ, et al. Antiparkinson drug adherence and its association with health care utilization and economic outcomes in a Medicare Part D population. Value Health. 2014;17(2):196–204.
Bond WS, Hussar DA. Detection methods and strategies for improving medication compliance. Am J Hosp Pharm. 1991;48(9):1978–88.
Galloway R, McGuire J. Determinants of compliance with iron supplementation: supplies, side effects, or psychology? Soc Sci Med. 1994;39(3):381–90.
Berger BA. Assessing and interviewing patients for meaningful behavioral change: part 1. Case Manager. 2004;15(5):46–50 quiz 51.
Llorca PM. Discussion of prevalence and management of discomfort when swallowing pills: orodispersible tablets expand treatment options in patients with depression. Ther Deliv. 2011;2(5):611–22.
Korczyn AD, et al. Rotigotine transdermal system for perioperative administration. J Neural Transm. 2007;114(2):219–21.
Grosset KA, Grosset DG. Effect of educational intervention on medication timing in Parkinson’s disease: a randomized controlled trial. BMC Neurol. 2007;7:20.
Daley DJ, et al. Adherence therapy improves medication adherence and quality of life in people with Parkinson’s disease: a randomised controlled trial. Int J Clin Pract. 2014;68(8):963–71.
Rojo A, et al. Depression in Parkinson’s disease: clinical correlates and outcome. Parkinsonism Relat Disord. 2003;10(1):23–8.
Riedel O, et al. Cognitive impairment in 873 patients with idiopathic Parkinson’s disease: results from the German Study on Epidemiology of Parkinson’s Disease with Dementia (GEPAD). J Neurol. 2008;255(2):255–64.
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–7.
Qureshi SU, et al. Anxiety disorders, physical illnesses, and health care utilization in older male veterans with Parkinson disease and comorbid depression. J Geriatr Psychiatry Neurol. 2012;25(4):233–9.
Campbell NL, et al. Medication adherence in older adults with cognitive impairment: a systematic evidence-based review. Am J Geriatr Pharmacother. 2012;10(3):165–77.
Haynes RB, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;2:CD000011.
Elm JJ, Kamp C, Tilley BC, Guimaraes P, Fraser D, Deppen P, Brocht A, Weaver C, Bennett S; NINDS NET-PD Investigators and Coordinators. Self-reported adherence versus pill count in Parkinson's disease: the NET-PD experience. Mov Disord. 2007;22(6):822–7.
Funding
No external funding was received for the preparation of this article. Naveed Malek and Donald G. Grosset are full-time employees of the UK National Health Service.
Conflict of Interest Declarations
Naveed Malek has no relevant conflicts of interest to declare. Donald G. Grosset has previously received research support from Merz Pharma; consultancy fees from AbbVie and Civitas; and honoraria from AbbVie, GE Healthcare and UCB Pharma.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malek, N., Grosset, D.G. Medication Adherence in Patients with Parkinson’s Disease. CNS Drugs 29, 47–53 (2015). https://doi.org/10.1007/s40263-014-0220-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-014-0220-0