Abstract
Purpose
For controlling symptoms in Parkinson’s disease (PD) together with treating additional comorbidities, patients often face complex medication regimens, with suboptimal adherence, drug-related problems, and diminished therapy efficacy as a common consequence. A medication review could potentially tackle these issues, among others by optimizing drug treatment. Even if no change in clinical outcomes is observed, this intervention might decrease health care costs by reducing drug-related problems and hospital admissions. This study aimed to gain more insight in the health benefits and costs of a structured medication review (SMR) in PD.
Methods
A cost-utility analysis was performed, based on a multicenter randomized controlled trial with 202 PD patients with polypharmacy. The intervention group received an SMR, whereas the control group received usual care. The intervention effect after 6 months of follow-up was presented as incremental quality-adjusted life years (QALY) using the EQ-5D-5L questionnaire. Costs were based on real-world data. Missing data was imputed using multiple imputation techniques. Bootstrapping was used to estimate the uncertainty in all health and economic outcomes.
Results
The QALY gain in the intervention group compared to the control group was − 0.011 (95% CI − 0.043; 0.020). Incremental costs were €433 (95% CI − 873; 1687). When adapting a willingness-to-pay threshold of €20,000/QALY and €80,000/QALY, the probability of SMRs being cost-effective was 18% and 30%, respectively.
Conclusion
A community pharmacist-led SMR in PD patients in the current setting shows no apparent benefit and is not cost-effective after 6 months, compared to usual care.
Trial registration
Netherlands Trial Register, NL4360. Registered 17 March 2014.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is among the most common neurodegenerative disorders worldwide, with an ongoing growth in prevalence [1]. The pathophysiology comprises a complex network of neuropathologic mechanisms, of which eventually dopamine deficiency is a major contributor to motor and non-motor symptoms [1]. These symptoms negatively influence quality of life (QoL). Motor symptoms are characterized by tremor, rigidity, bradykinesia and postural instability, whereas non-motor manifestations cover a wide spectrum of symptoms, of which autonomic dysfunction and mental disturbances are most prevalent. Drug therapy is the first step of treatment aiming to reduce symptoms. With disease progression, drug treatment and dosing frequency intensify, often leading to complex medication regimens. This is aggravated by additional drugs due to age-related comorbidities, which might easily lead to reduced therapy adherence with drug-related problems (DRP), reduced treatment effect, and increased health care costs [2,3,4].
A medication review is an intervention that might mitigate these problems. It is defined as “a structured, critical examination of a patient’s medicines aiming to reach an agreement with the patient about therapy, optimizing the impact of medication, minimizing the number of DRPs, and reducing waste,” ranging in magnitude from prescription reviews to patient-centered clinical medication reviews [5]. By identifying DRPs and improving a patients’ knowledge and adherence, a medication review aims to improve quality, safety, and appropriate use of medication [6]. This medication intervention has been studied in multiple health care settings and positive effects where found regarding DRPs [5, 7, 8], and medication appropriateness [5, 9,10,11]. However, data on health outcomes like QoL showed varying results. This might be ascribed to different care settings, patient populations, study designs, and ways of performing medication reviews.
Community pharmacists in the Netherlands use a structured approach for the clinical medication reviews performed as part of standard care (structured medication review; SMR) [12]. A pilot study in PD investigated the effects of multiple pharmacist-led interventions including an SMR and showed potential positive effects on medication adherence and quality of life [13]. Conversely, in a recent randomized controlled trial analyzing the effectiveness of a community pharmacist-led SMR in PD, no improvement of QoL was seen [14]. Therefore, the actual effect of an SMR on QoL in PD is still uncertain. Additionally, optimized drug treatment after an SMR might decrease health care costs, by reducing DRPs and drug-related hospital admissions. To gain more insight in the benefits of an SMR in PD, both in terms of health benefit and costs, a cost-utility analysis was performed regarding a community pharmacist-led SMR in PD patients compared to usual care.
Methods
Study design and patients
In this study, a cost-utility analysis (CUA) was performed based on data of the Medication Review in Parkinson-trial, a multicenter randomized controlled trial assessing the effect of a community pharmacist-led SMR in PD patients with polypharmacy [14, 15]. The study and economic evaluation were performed and reported with due regard to the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) [16].
Details of the protocol and results are published elsewhere [14, 15]. Patients were selected from three Dutch outpatient neurology clinics. Inclusion criteria were the use of ≥ 4 different drugs daily, ≥ 4 drug intake moments daily, expressing motor and non-motor symptoms, living (semi)-independent, and being able to read and write the Dutch language. Exclusion was based on being unable to administer own medication (e.g., when requiring assistance from medical home care), having received a medication review within a year prior to study participation, receiving continuous apomorphine therapy, continuous levodopa-carbidopa gastro-intestinal gel therapy, or a deep brain stimulator within a year prior to study participation, or planned to receive this within 3 months.
Baseline measurement took place after written informed consent. Subsequently, patients were randomly assigned to the SMR or usual care group, in a 1:1 ratio with a blinded blocked randomization (block sizes four and eight). Inclusion was definite after baseline measurements were carried out, and - with regard to the intervention group patients - the SMR was performed. Due to a high withdrawal rate of randomized intervention group patients who did not receive an SMR for various reasons, and after consultation with the Medical Ethical Committee, the randomization process was adapted to a 4:1 ratio (intervention group vs. control group), to timely meet the calculated power.
Drug use and dosing scheme were verified by the patient’s community pharmacist. PD severity was assessed by Hoehn and Yahr (HY) stage (range 0–5) [17], and comorbidity score was assessed by the Rx-Risk comorbidity index (range 0–46) [18].
The study was conducted in agreement with the Declaration of Helsinki principles, in accordance with the Medical Research Involving Human Subjects Act (WMO), and approved by the Medical Ethical Review Board Twente, the Netherlands (NL48661.044.14). The study was registered in the Netherlands Trial Register (NL4360; registration date: 17 March 2014).
Intervention
Community pharmacists performed an SMR at the study start in the intervention group. Beforehand, a training was offered to all cooperating pharmacists, concerning PD, its pharmacological treatment, the study protocol, and a uniform approach for carrying out SMRs. The latter was based on the Dutch Systematic Tool to Reduce Inappropriate Prescribing (STRIP) method, which is part of the multidisciplinary guideline Polypharmacy in the Elderly [12]. This method underlines the patient’s involvement as equal partner in the process and comprises the following six steps: preparation (data collection concerning drug use, medical history and condition, and laboratory results), anamnesis (including a patient’s expectations, views, and beliefs), analysis (reviewing drug use regarding DRPs, which were further subdivided in, e.g., (contra)indications, interactions, ineffective therapy, suboptimal dose, side effects, and practical usage problems), discussion with involved physicians (proposed interventions are discussed), discussion with the patient (including shared decision-making regarding modifications), and evaluation (within 4 months).
All DRPs, proposed and implemented modifications, and recommendations were recorded, as well as the time spent on the SMR by both pharmacist and GP, using a uniform recording document (Online Resource 1). In the usual care group, no SMR was performed during 6 months of follow-up.
Outcome measures
The primary outcome was cost-utility of the SMR after 6 months from a health care payer’s perspective, presented as incremental effect in quality-adjusted life years (QALYs) and as incremental costs in Euros of the SMR group compared to the usual care group [19].
Health outcomes
At baseline and at 3 and 6 months, a set of validated questionnaires was sent to the patients and — if applicable — their care givers. In the Medication Review in Parkinson-study, QoL was measured by two questionnaires. The Parkinson’s Disease Questionnaire-39 (PDQ-39) measured PD-specific QoL (range 0–100), with higher scores representing worse QoL [20]. The EuroQoL 5 Dimensions-5 Levels-questionnaire (EQ-5D-5L) [21] comprises five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) determining general health-related QoL (range −0.446–1). Here, a utility value of 1 represents perfect health, death is commonly assigned a utility value of 0, and negative utility values represent health states worse than death. Utility values were obtained from the EQ-5D-5L using the Dutch tariff [21], and QALYs were calculated as area under the curve following linear interpolation of utility scores over time. Other secondary outcomes — not relevant in this cost-utility analysis — were non-motor symptoms (Non-Motor Symptoms Questionnaire, NMS-Quest) [22], daily life activities and physical disability (AMC Linear Disability Scale, ALDS) [23], health status (EuroQoL Visual Analogue Scale, EQ-VAS) [24], and PD care giver’s QoL (PDQ-Carer) [25]. Also, SMRs documents were evaluated with regard to potential DPRs and suggested drug interventions (whether or not implemented) and descriptively addressed.
Costs
Total costs per patient were based on medication costs, hospital costs, and - in the SMR group - SMR costs. The costs for the accredited PD training were not taken into account, since these were only offered for the purpose of the study to better prepare pharmacists and standardize the execution of the SMR. Costs for regular patient consultations with their GP were not taken into account, since these were unknown.
Medication costs over 6 months were calculated from prescription data, based on 2020 drug prices [medicijnkosten.nl]. Hospital costs during 6 months were collected, with a distinction between outpatient clinic costs and costs of both emergency department visit and hospital admission. SMR costs were calculated based on a previous study assessing the costs of SMRs [26], taking into account the amount of time the pharmacist and GP spent on the SMR. Hospital and SMR costs were adjusted to 2020 Euros based on Dutch consumer price indices [27].
Analysis
The calculated sample size of the Medication Review in PD-study [14] was based on the detection of a clinically important difference in the PDQ-39-score [28]. This difference was assumed to be minimally 1.6. Based on own expectations, a difference of 6 points between our study groups after intervention was assumed. With a standard deviation of 15 [28], 198 patients needed to be recruited in order to detect a clinically relevant difference, with a type I error of 5% and a power of 80%.
Between-group differences in categorical variables were analyzed with a chi-square test or Fisher’s exact test, as appropriate. Between-group differences in continuous variables were analyzed with a t-test or Mann–Whitney test, as appropriate. Normally distributed continuous data were presented as mean with standard deviation (SD) or as median with interquartile range (IQR) in case of non-normal distribution.
A modified intention-to-treat analysis was applied, as acknowledged in the study protocol [15], in order to assess the actual effect of an SMR. With this, randomized intervention group patients needed to obtain an SMR for definite study inclusion and analyses. To properly address missing data, multiple imputation was performed to obtain 10 imputed datasets. Additionally, a complete case analysis was performed. All presented outcome measures are based on multiple imputed data, unless otherwise noted.
Since the SMR pertains to a primary care intervention, no stratification for outpatient clinic was needed. Non-parametric bootstrapping was used to resample both the data completed with multiple imputations and the complete case data 5000 times, to evaluate the uncertainty in all health and economic outcomes [19]. Based on the bootstrap samples, 95% confidence intervals (CIs) of all outcome measures were determined. The results were plotted on an incremental cost-utility plane [29], which graphically shows the uncertainty in incremental costs and QALYs, and in a cost-effectiveness acceptability curve [30]. The probability that SMRs are cost-effective compared with usual care was shown for willingness-to-pay (WTP) thresholds from €0/QALY to €100,000/QALY, which include the Dutch thresholds, ranging from €20,000/QALY to €80,000/QALY, depending on the burden of the disease [31]. The incremental cost-utility ratio, presenting the additional costs per QALY gained, was calculated by dividing the difference in total costs per group by the difference in QALYs per group. A negative ratio represents either cost saving per QALY or decline of one QALY together with higher costs.
Analyses were performed using Microsoft Excel & VBA, version 15.0, and IBM SPSS Statistics version 26.
Results
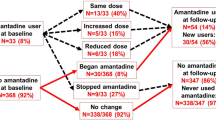
Between May 2014 and December 2018, 240 participants were initially randomized. A total of 37 SMR group patients did not receive an SMR, and 202 patients were definitely included (Fig. 1). The complete case analysis was based on 152 patients, since 31 patients were lost to follow-up, and 19 other patients had incomplete follow-up data. Baseline characteristics as well as questionnaire data are shown in Table 1.
Community pharmacists of 82 pharmacies cooperated in the study, and 99 SMRs were executed, in which they identified 260 potential DRPs (2.6 (± 1.8) per SMR group patient). Of the 260 suggested interventions, 161 were implemented (62%) and led to therapy optimization.
As previously described [14], baseline measurements of all questionnaire data were similar between both groups, and in both groups, all scores were worse after 6 months. No difference was found in change of PDQ-39 scores between the SMR group and usual care group, with a non-significant treatment effect of 2.09 (−0.63; 4.80) in favor of the usual care group. Similarly, non-significant treatment effects were observed for all secondary outcomes (NMS-Quest, ALDS, EQ-VAS and PDQ-Carer).
Effect outcomes and costs
EQ-5D-5L utility values, derived QALYs, and costs during 6 months are presented in Table 2. The incremental QALYs were −0.011 (95% CI −0.043; 0.020) for the SMR group compared to the usual care group. Pharmacists spent on average 101 min (SE 5.76) on an SMR, and GPs 16 min (SE 1.58). With this, the mean SMR costs were €211. Total health care costs per patient in the SMR group were €3371, compared to €2938 in the usual care group, with €433 (95% CI − 873; 1687) incremental costs per patient in the SMR group.
For the complete case analysis, the incremental QALYs for the SMR group compared to the usual care group were −0.010 (95% CI −0.044; 0.025) and incremental costs €368 (95% CI −655; 1373).
Cost-utility analysis
In Fig. 2, the incremental cost-utility plane is presented, with WTP thresholds of €20,000/QALY and 80,000/QALY. Figure 3 shows the cost-effectiveness acceptability curve. When applying a WTP threshold of €20,000/QALY and of €80,000/QALY, the probability of an SMR being cost-effective is 18% and 30%, respectively. In comparison, based on the complete case analysis, this would be 21% and 34%, respectively. The incremental cost-utility ratio is € −38,478/QALY and in the complete case analysis € −37,002/QALY. However, given the very small difference in QALYs (i.e., the denominator of this ratio), these values are not very informative and should be interpreted with caution.
Discussion
In this study, a community pharmacist-led SMR in PD patients is not of apparent benefit compared to usual care. When adapting a WTP threshold of €20,000/QALY and of €80,000/QALY, the probability of SMRs being cost-effective has shown to be 18% and 30%, respectively. This is predominantly based on higher costs (€433 (−873; 1687) during 6 months in patients receiving an SMR, while health outcomes in the SMR and usual care group remained almost similar. The probability of SMRs in this setting being cost-effective is therefore low.
Regarding health effects, no improvement in QoL was found after an SMR based on QALYs. QALYs within 6 months can range between 0 and 0.5. With this, a worsening of 0.011 (−0.043; 0.020) in QALYs after an SMR compared to the usual care group is only small, and its relevance is questionable.
Even though no clinical effect was found, we hypothesized health care costs would be lower in the intervention group, since optimized drug treatment might lead to less health care use and hospital admissions [32]. However, our results showed the opposite. Much of the difference in costs between both groups is explained by the SMR costs. The mean incremental costs were €211, of which €181 was associated with pharmacist costs, based on the time spent to perform an SMR. Besides, costs in the SMR group could have even been higher when taking into account the training for pharmacists, although our main aims with this training were to involve pharmacists in our study and to obtain a uniform approach of the SMR execution. We were not able to analyze whether this training might also have contributed to the quality of SMRs in PD, and we did not include training costs.
To our knowledge, this is the first study to evaluate the cost-utility of a community pharmacist-led SMR in PD. In previous literature, economic evaluations after a medication review have been performed in different health care settings and with different clinical endpoints. In terms of cost-effectiveness, studies showed conflicting results [32,33,34,35,36,37,38,39]. Two studies found positive effects of a medication review in nursing home patients with regard to inappropriate prescribing, but only one was cost-effective [34, 40]. Desborough et al. reported higher health care costs in the intervention group [34]. Also, a medication review at hospital discharge in elderly led to a reduced amount of DRPs, but to higher costs and health care utilization [35], in accordance with our results. Intervention costs in these studies did not seem to justify the health care costs, and Van der Heijden et al. proposed that since the quality of usual pharmacist care in the Netherlands is already high, the beneficial effect of an extended intervention might be difficult to demonstrate [35]. In the same setting, Pacini et al. reported a low probability of a medication review being cost-effective, based on a small, non-significant gain in QoL, with an increase in hospital admissions [36]. Lastly, an in-hospital pharmacist intervention did not seem cost-effective, with higher costs in the intervention group and a rather small gain of QoL [37].
Specifically within primary care, a medication review in patients at risk of drug misuse showed positive outcomes regarding adverse events, severity of illness and costs, although no difference on QoL was found, whereby the ICER in reducing illness severity and adverse drug events was slightly favorable (AUS$65 and AUS$69, respectively) [38]. Verdoorn et al. analyzed the cost-effectiveness of a clinical medication review in elderly with polypharmacy, with a setting comparable to ours [39]. EQ-5D utility values were slightly reduced after the intervention, but a small improvement on the Visual Analogue Scale was seen. Furthermore, costs were saved. According to Jodar et al., similar positive results regarding cost-effectiveness were found [32].
We did not find cost-savings. This might be explained by several reasons. First, compared to the abovementioned studies, a specific patient population was studied. In a PD population, drug therapy is often finely tuned and highly individualized. Changes in pharmacotherapy might demand extra monitoring by the neurologist. This might explain the higher outpatient costs in the SMR group. Also, the modifications might not have had the expected result or even worsened health status, and more changes needed to follow before optimal treatment was set. In line with this, some DRPs were accepted, since resolving the DRP might do even more harm.
Although medication costs reduced after an SMR, this reduction did not outweigh the SMR costs and hospital costs. One might argue that with longer follow-up, this might also be balanced eventually. However, when dealing with a progressive disease, there is a continuous need for adjusting drug treatment and for medication to be reviewed, whereby we do not expect that a longer follow-up would change the current outcome.
A few changes in the current setting might be suggested: a more specific PD patient selection, probably with a focus on possible existing DRPs; a better cooperation between primary and secondary care; and further specialization of a pharmacist in PD. Positive effects on QoL in PD patients were found after a medication intervention by a pharmacist specialized in PD, with possibilities for direct consultation with the neurologist [13]. However, costs were not taken into account. Although this concerned a pilot study, previously it was found that specialization of health care providers in PD has beneficial effects on health outcomes [41, 42]. This questions whether PD pharmacy care should be more centered, with execution of SMRs by pharmacists specialized in PD. On the other hand, as earlier mentioned, pharmacy care delivered in the Netherlands might be of such a high quality that further, small clinical benefits of interventions are difficult to demonstrate.
Previously, we found an association between the number of comorbidities and QoL, in which also female sex and higher HY score are associated with worse QoL [43]. With regard to our data, the percentage of females and of patients with a higher HY score were both higher in the SMR group, although without significant difference. An additional analysis, with correction for some small imbalances between both groups at baseline, resulted in a smaller incremental QALY difference of −0.002 (data not shown), still in favor of the usual care group.
We found a small difference in outcomes between the multiple imputed analysis and the complete case analysis. Of the patients lost to follow-up regarding EQ-5D-5L scores, costs were known in most cases. These patients had in general higher costs for hospital admissions or other medical conditions, and imputed EQ-5D-5L scores were therefore also lower. However, the final conclusion of both analyses is similar.
Strengths of this study were the multicenter randomized controlled setting, with a large number of PD patients and cooperating community pharmacists. This setting reflects standard SMR care by community pharmacists in the Netherlands and supports the generalizability of the study. Furthermore, standardization of the execution of the SMR was assured by a preceding training offered to all pharmacists.
There are also some limitations. As mentioned before, the pharmacist training may have influenced the cost-utility results, since this is not customary organized. Another possible limitation is that costs for regular consultations with their GP by the patients were missing, since these data were unknown. However, one could hypothesize that after an SMR, a consultation with the neurologist might take place more often than with a GP, and all (extra) consultations with the neurologist are already taken into account within the outpatient hospital costs. It is therefore expected that the GP consultation costs would not have a high impact on the total costs. Another limitation is that home care or nursing home costs have not been taken into account for the same reason. This is an important limitation, since by offering the most optimized multidisciplinary care for home-dwelling PD patients, an admission to a nursing home might eventually be postponed. This could save a substantial amount of health care costs. As part of this integrated PD care, an SMR might be a meaningful contribution, although this assessment is beyond the scope of this paper.
Furthermore, the proportion of missing data (25%) is substantial. We adjusted for this by use of multiple imputation. Missing data was similarly distributed between both groups. Besides, based on similar baseline characteristics and flowchart course in both groups, we have no indication that selective dropout took place.
Altogether, the results of our study point towards an SMR not being cost-effective. Since we do not doubt the importance of periodic medication optimization in complex diseases or high risk patients, the future focus should be on either improving the current setting of SMRs in PD or search for other strategies in which this can be achieved.
Conclusions
The results of our study indicate that SMRs executed by community pharmacists in PD patients is not of apparent benefit. Taking into account both the pharmacist’s effort and additional costs when performing an SMR in the current setting, the valuable time of a pharmacist could better be spent on more (cost-)effective interventions. The multidisciplinary PD care regarding optimization of pharmacotherapy should be organized differently, and additional research is warranted to optimize the setting, for example, either by a different PD patient selection, better cooperation between health care providers, or further specialization of pharmacists in PD.
Availability of data and material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Bloem BR, Okun MS, Klein C (2021) Parkinson’s disease. Lancet 397:2284–2303. https://doi.org/10.1016/S0140-6736(21)00218-X
Schröder S, Martus P, Odin P, Schaefer M (2011) Drug-related problems in Parkinson’s disease: the role of community pharmacists in primary care. Int J Clin Pharm 33:674–682. https://doi.org/10.1007/s11096-011-9526-x
Kulkarni AS, Balkrishnan R, Anderson RT et al (2008) Medication adherence and associated outcomes in Medicare health maintenance organization-enrolled older adults with Parkinson’s disease. Mov Disord 23:359–365. https://doi.org/10.1002/mds.21831
Malek N, Grosset DG (2015) Medication adherence in patients with Parkinson’s disease. CNS Drugs. https://doi.org/10.1007/s40263-014-0220-0
Clyne W, Blenkinsopp A, Seal R (2008) A guide to medication review. National Prescribing Centre NHS, Liverpool. https://www.cff.org.br/userfiles/52%20-%20CLYNE%20W%20A%20guide%20to%20medication%20review%202008.pdf. Accessed 17 Sep 2022
Blenkinsopp A, Bond C, Raynor DK (2012) Medication reviews. Br J Clin Pharmacol 74:573–580. https://doi.org/10.1111/j.1365-2125.2012.04331.x
Viswanathan M, Kahwati LC, Golin CE et al (2015) Medication therapy management interventions in outpatient settings: a systematic review and meta-analysis. JAMA Intern Med 175:76–87. https://doi.org/10.1001/jamainternmed.2014.5841
Vinks TH, Egberts TC, de Lange TM, de Koning FH (2009) Pharmacist-based medication review reduces potential drug-related problems in the elderly: the SMOG controlled trial. Drugs Aging 26:123–133. https://doi.org/10.2165/0002512-200926020-00004
Scheifes A, Egberts TCG, Stolker JJ et al (2016) Structured medication review to improve pharmacotherapy in people with intellectual disability and behavioural problems. J Appl Res Intellect Disabil 29:346–355. https://doi.org/10.1111/jar.12183
Hurmuz MZM, Janus SIM, van Manen JG (2018) Changes in medicine prescription following a medication review in older high-risk patients with polypharmacy. Int J Clin Pharm 40:480–487. https://doi.org/10.1007/s11096-018-0602-3
Cooper JA, Cadogan CA, Patterson SM et al (2015) Interventions to improve the appropriate use of polypharmacy in older people: a Cochrane systematic review. BMJ Open 5:e009235. https://doi.org/10.1136/bmjopen-2015-009235
NHG/NVKG/FMS (2021) Richtlijn Polyfarmacie bij ouderen (Guideline Polypharmacy in the elderly). The Netherlands. https://richtlijnendatabase.nl/richtlijn/polyfarmacie_bij_ouderen/polyfarmacie_bij_ouderen_-_korte_beschrijving.html. Accessed 17 Sep 2022
Stuijt C, Karapinar-Çarkit F, van den Bemt B, van Laar T (2018) Effect of pharmacist-led interventions on (non)motor symptoms, medication-related problems, and quality of life in Parkinson disease patients: a pilot study. Clin Neuropharmacol 41:14–19. https://doi.org/10.1097/WNF.0000000000000260
Oonk NGM, Movig KLL, Van Der Palen J et al (2022) The effect of a structured medication review on quality of life in Parkinson’s disease. J Parkinsons Dis 12:1295–1306. https://doi.org/10.3233/JPD-213021
Oonk NGM, Movig KLL, Munster EM et al (2018) The effect of a structured medication review on quality of life in Parkinson’s disease: the study protocol. Contemp Clin Trials Commun 13:100308. https://doi.org/10.1016/j.conctc.2018.100308
Husereau D, Drummond M, Petrou S et al (2013) Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Pharmacoeconomics 31:361–367. https://doi.org/10.1007/s40273-013-0032-y
Goetz CG, Poewe W, Rascol O et al (2004) Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations The Movement Disorder Society Task Force on rating scales for Parkinson’s disease. Mov Disord 19:1020–1028. https://doi.org/10.1002/mds.20213
Vitry A, Wong SA, Roughead EE et al (2009) Validity of medication-based co-morbidity indices in the Australian elderly population. Aust N Z J Public Health 33:126–130. https://doi.org/10.1111/j.1753-6405.2009.00357.x
Zorginstituut Nederland (Dutch Institute National Health Care) (2016) Richtlijn voor het uitvoeren van economische evaluaties in de gezondheidszorg. The Netherlands. https://www.zorginstituutnederland.nl/over-ons/publicaties/publicatie/2016/02/29/richtlijn-voor-het-uitvoeren-van-economische-evaluaties-in-de-gezondheidszorg. Accessed 17 Sep 2022
Jenkinson C, Fitzpatrick R, Peto V et al (1997) The Parkinson’s Disease Questionnaire (PDQ-39): development and validation of a Parkinson’s disease summary index score. Age Ageing 26:353–357. https://doi.org/10.1093/ageing/26.5.353
Versteegh MM, Vermeulen KM, Evers SMAA et al (2016) Dutch tariff for the five-level version of EQ-5D. Value Heal 19:343–352. https://doi.org/10.1016/j.jval.2016.01.003
Chaudhuri KR, Martinez-Martin P, Schapira AH et al (2006) International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov Disord 21:916–923. https://doi.org/10.1002/mds.20844
Holman R, Weisscher N, Glas CA et al (2005) The Academic Medical Center Linear Disability Score (ALDS) item bank: item response theory analysis in a mixed patient population. Health Qual Life Outcomes 3:83. https://doi.org/10.1186/1477-7525-3-83
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343. https://doi.org/10.3109/07853890109002087
Morley D, Dummett S, Kelly L et al (2013) The PDQ-Carer: development and validation of a summary index score. Parkinsonism Relat Disord 19:448–449. https://doi.org/10.1016/j.parkreldis.2012.11.018
Koster L, Hoeben T, Peeters C, Plu R (2014) Generieke kosten medicatiebeoordeling. Royal Dutch Pharmacists Association (KNMP). https://www.knmp.nl/sites/default/files/2022-01/Significant%20-%20Rapport%20Generieke%20kosten%20medicatiebeoordeling%20-%20Definitief.pdf. Accessed 17 Sep 2022
CBS Statline (Statistics Netherlands). Jaarmutatie consumentenprijsindex; vanaf 1963 (Annual rate of change Consumer Price Index). https://opendata.cbs.nl/statline/#/CBS/nl/dataset/70936ned/table?ts=1535353425460. Accessed 17 Sep 2022
Peto V, Jenkinson C, Fitzpatrick R (2001) Determining minimally important differences for the PDQ-39 Parkinson’s disease questionnaire. Age Ageing 30:299–302. https://doi.org/10.1093/ageing/30.4.299
Black WC (1990) The CE Plane: a graphic representation of cost-effectiveness. Med Decis Mak 10:212–214. https://doi.org/10.1177/0272989X9001000308
Fenwick E, O’Brien BJ, Briggs A (2004) Cost-effectiveness acceptability curves - facts, fallacies and frequently asked questions. Health Econ 13:405–415. https://doi.org/10.1002/hec.903
Raad voor de Volksgezondheid en Zorg (Counsil of Public Health and Care) (2006) Advies Zinnige en duurzame zorg. Zoetemeer. https://www.raadrvs.nl/binaries/raadrvs/documenten/publicaties/2006/06/07/zinnige-en-duurzame-zorg/Advies_-_Zinnige_en_duurzame_zorg.pdf. Accessed 17 Sep 2022
Jódar-Sánchez F, Malet-Larrea A, Martín JJ et al (2015) Cost-utility analysis of a medication review with follow-up service for older adults with polypharmacy in community pharmacies in Spain: the conSIGUE program. Pharmacoeconomics 33:599–610. https://doi.org/10.1007/s40273-015-0270-2
Patterson SM, Hughes CM, Cardwell C et al (2011) A cluster randomized controlled trial of an adapted U.S. model of pharmaceutical care for nursing home residents in Northern Ireland (Fleetwood Northern Ireland Study): a cost-effectiveness analysis. J Am Geriatr Soc 59:586–593. https://doi.org/10.1111/j.1532-5415.2011.03354.x
Desborough JA, Clark A, Houghton J et al (2020) Clinical and cost effectiveness of a multi-professional medication reviews in care homes (CAREMED)†. Int J Pharm Pract 28:626–634. https://doi.org/10.1111/ijpp.12656
van der Heijden AAWA, de Bruijne MC, Nijpels G, Hugtenburg JG (2019) Cost-effectiveness of a clinical medication review in vulnerable older patients at hospital discharge, a randomized controlled trial. Int J Clin Pharm 41:963–971. https://doi.org/10.1007/s11096-019-00825-3
Pacini M, Smith RD, Wilson ECF, Holland R (2007) Home-based medication review in older people: is it cost effective? Pharmacoeconomics 25:171–180. https://doi.org/10.2165/00019053-200725020-00008/FIGURES/2
Wallerstedt SM, Bladh L, Ramsberg J (2012) A cost-effectiveness analysis of an in-hospital clinical pharmacist service. BMJ Open. https://doi.org/10.1136/bmjopen-2011-000329
Sorensen L, Stokes JA, Purdie DM et al (2004) Medication reviews in the community: results of a randomized, controlled effectiveness trial. Br J Clin Pharmacol 58:648. https://doi.org/10.1111/j.1365-2125.2004.02220.x
Verdoorn S, van de Pol J, Hövels AM et al (2020) Cost-utility and cost-effectiveness analysis of a clinical medication review focused on personal goals in older persons with polypharmacy compared to usual care: economic evaluation of the DREAMeR study. Br J Clin Pharmacol. https://doi.org/10.1111/bcp.14421
Patterson SM, Cadogan CA, Kerse N et al (2014) Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008165.pub3
Ypinga JHL, de Vries NM, Boonen LHHM et al (2018) Effectiveness and costs of specialised physiotherapy given via ParkinsonNet: a retrospective analysis of medical claims data. Lancet Neurol 17:153–161. https://doi.org/10.1016/S1474-4422(17)30406-4
Bloem BR, Rompen L, de Vries NM et al (2017) ParkinsonNet: a low-cost health care innovation with a systems approach from the Netherlands. Health Aff 36:1987–1996. https://doi.org/10.1377/hlthaff.2017.0832
Oonk NGM, Movig KLL, van der Palen J et al (2021) The impact of non-dopaminergic medication on quality of life in Parkinson’s disease. Clin Drug Investig 41:809–816. https://doi.org/10.1007/s40261-021-01064-z
Acknowledgements
The authors would like to thank all patients and involved health care providers, especially the cooperating pharmacists, for their effort and contribution.
Funding
This work was supported by the Royal Dutch Pharmacists Association (Koninklijke Nederlandse Maatschappij ter bevordering der Pharmacie, KNMP). This funding had no role in the analysis or interpretation of the results in this study.
Author information
Authors and Affiliations
Contributions
Study conception and design: NO, LD, AB, JP, KM, HK. Acquisition of data: NO, LD, AB, HN, MK. Analysis and interpretation of data: NO, LD, AB, JP, KM, HK. Drafting of the manuscript: NO, AB, JP, HK. Critical revision: LD, KM, HN, MK. All authors reviewed the manuscript and gave final approval of the manuscript to be published.
Corresponding author
Ethics declarations
Ethics approval and informed consent
Ethical approval for this study was provided by the Medical Ethical Review Board Twente, the Netherlands (reference number NL48661.044.14). Written informed consent was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oonk, N.G.M., Dorresteijn, L.D.A., van den Berg, A.D. et al. Cost-utility analysis of a structured medication review compared to usual care in Parkinson’s disease. Eur J Clin Pharmacol 79, 289–297 (2023). https://doi.org/10.1007/s00228-022-03438-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03438-4