Abstract
Pregabalin (Lyrica®), a well established anxiolytic agent, has been approved in the EU for the treatment of generalized anxiety disorder (GAD) in adults. It has a distinct mechanism of action relative to other anti-anxiety agents (α2δ binding at presynaptic voltage dependent calcium channels leading to inhibition of excitatory neurotransmission), a rapid onset of effect (typically ≤1 week) and broad spectrum activity against both the psychic and somatic symptoms of GAD. In long-term studies, pregabalin maintained improvements in anxiety symptoms that occurred in response to short-term treatment and delayed the time to relapse of GAD compared with placebo. Common comorbidities of GAD, such as insomnia, gastrointestinal symptoms and subsyndromal depression, have no effect on the anxiolytic efficacy of, and moreover are specifically improved by, pregabalin. Treatment with pregabalin is generally well tolerated; the drug has an adverse event profile that includes dizziness, somnolence and weight gain. The potential for abuse of pregabalin is low; the risk of withdrawal symptoms is generally low when the drug is discontinued gradually (over 1 week). Alongside selective serotonin reuptake inhibitors (SSRIs) and serotonin-noradrenaline reuptake inhibitors (SNRIs), pregabalin is considered a first-line agent for the long-term treatment of GAD by the World Federation of Societies of Biological Psychiatry. It should be stressed, however, that definitive head-to-head studies comparing pregabalin with SSRI/SNRIs, including in patients with GAD and co-morbid major depressive disorder, are currently lacking. Recently, a study of SSRI/SNRI augmentation with pregabalin yielded positive results, while another study of switching from long-term benzodiazepine therapy to pregabalin was inconclusive; further investigations on these topics are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Efficacy and tolerability demonstrated in numerous short- and long-term clinical trials in patients with moderate to severe GAD |
Faster onset of action than selective serotonin reuptake inhibitors (SSRIs) and serotonin-noradrenaline reuptake inhibitors (SNRIs) |
Broad spectrum activity against both psychic and somatic symptoms of GAD |
Effective in elderly patients |
Low potential for drug–drug interactions |
Low potential for abuse |
Minimal withdrawal symptoms and rebound anxiety when tapered off over a 1-week period |
Sexual dysfunction not a prominent adverse event, in contrast to SSRIs/SNRIs |
1 Introduction
Generalized anxiety disorder (GAD) is characterized by excessive generalized worrying and marked symptoms of hypervigilance, hyperarousal and nonspecific anxiety that is persistent (i.e. lasts more than a few months). These psychological symptoms are frequently accompanied by physical (somatic) complaints, such as muscular tension, palpitations, abdominal complaints, sweating, nausea and dry mouth [1–3]. It is a chronic, fluctuating illness that is commonly encountered in community and clinical settings [4].
GAD has a high human burden in terms of impairments in role functioning and health-related quality of life (which are similar in magnitude to those experienced by patients with major depressive disorder [MDD]) and a considerable economic burden owing to high medical resource use (e.g. while diagnosing the disease) and lost work productivity [5]. Moreover, GAD is often co-morbid with other mood and anxiety disorders, such as MDD [2]. In one European community study [6], ≈60 % of patients with GAD (Diagnostic and Statistical Manual of Mental Disorders Volume IV [DSM-IV] criteria) also fulfilled the criteria for MDD; 56 % fulfilled the criteria for another anxiety disorder. Comorbid GAD and MDD results in greater disability compared with the co-occurrence of GAD with other psychiatric conditions [7]. Additionally, it may increase the risk of suicide [8], as both GAD [9] and MDD [10] are independent predictors of this eventuality.
The overall aims of GAD therapy are to improve—and ideally achieve complete relief from—symptoms (thereby restoring functioning) and to prevent their recurrence; following an initial (acute) phase, treatment usually needs to be continued on a long-term basis, due to the chronic nature of the disease [2, 11]. Therapeutic options include psychological interventions (of which cognitive behavioural therapy [CBT] is the best studied and most widely used) and drug therapies [3, 12, 13]. As regards which modality to use and when, drug therapy should be initiated if symptoms cause significant functional impairment (as is usually the case when GAD is diagnosed) [3], while CBT can be used as an alternative to initial drug therapy or to augment the effects of drug therapy [14, 15]. According to the most recent (2008) guidelines issued by the World Federation of Societies of Biological Psychiatry [13, 16], recommended first-line pharmacological treatments for GAD include selective serotonin reuptake inhibitors (SSRIs; e.g. escitalopram, paroxetine, sertraline), serotonin-noradrenaline reuptake inhibitors (SNRIs; e.g. venlafaxine and duloxetine) and the gabapentinoid, pregabalin (Lyrica®) [13].
The current article focuses on the use of pregabalin in the treatment of GAD in adults, an indication for which it has been approved in the EU since 2006 [3, 17, 18]. Pregabalin is also approved in the EU for the treatment of peripheral and central neuropathic pain in adults and as adjunctive therapy for partial seizures with or without secondary generalization in adults with epilepsy [17]; however discussion of these additional indications is beyond the scope of the present review.
2 Pharmacological Properties
Pregabalin is the active (S)-enantiomer of 3-(aminomethyl)-5-methylhexanoic acid. The pharmacodynamics properties of the drug have been reviewed and/or summarized previously [3, 18–21], as have its pharmacokinetic properties [3, 17–20, 22, 23]. Accordingly, only a very brief overview is provided here. The comparative pharmacological properties of pregabalin and gabapentin (the other gabapentinoid in clinical use, albeit not for GAD) have been reviewed elsewhere [22].
2.1 Mechanism of Anxiolytic Action
Pregabalin is a structural analogue of GABA that nonetheless does not interact with GABA(A) or (B) receptors, does not get converted to GABA or a GABA agonist, and does not alter GABA uptake or degradation. Instead, it is thought to exert its anxiolytic and other therapeutic effects by binding selectively and with high affinity to α2δ auxillary subunits—in particular the α2δ type 1 (α2δ-1) subunit—of P/Q-type voltage-dependant calcium channels (VDCCs) in hyperexcited neurones [21, 24, 25]. Binding of pregabalin to presynaptically-localized α2δ-1 reduces the action potential-induced influx of calcium through VDCCs and, consequently, reduces the release of several excitatory neurotransmitters from the nerve terminal, including glutamate and monoaminergic neurotransmitters, which are specifically implicated in pathological anxiety [18, 19, 21].
Within the CNS, the highest levels of pregabalin binding are observed in the cortex, olfactory bulb, hypothalamus, amygdala, hippocampus, cerebellum and dorsal horn of the spinal cord; the α2δ-1 subunit is the primary target, except in the cerebellum, where the α2δ type 2 subunit is the primary target [21]. Although further research is required, available data suggest that pregabalin binding to α2δ is localized to regions that are coextensive with neural circuits that underlie anxiety symptoms and behaviours [21].
Preclinical in vivo data supporting the suggestion that the anxiolytic effect of pregabalin is mediated by α2δ binding include the demonstration that pregabalin analogues with higher affinity for α2δ have more potent effects in animal models of anxiety [26] and the observation that pregabalin lacks anxiolytic activity in transgenic mice with specific point mutations in α2δ-1 [27]. It remains to be determined whether, and to what extent, other observed (calcium influx-independent) effects of gabapentinoids, namely inhibition of excitatory synaptogenesis and inhibition of VDCC trafficking from the endoplasmic reticulum to the cell surface, contribute to the anxiolytic activity of pregabalin [21].
2.2 Pharmacokinetic Properties
The key pharmacokinetic properties of pregabalin are summarized in Table 1. Briefly, pregabalin, a substrate of the L-type amino acid transporter 1, is rapidly absorbed from the gastrointestinal tract after oral administration and readily penetrates the blood–brain barrier [19, 20]. Pregabalin demonstrates linear (dose-proportional) pharmacokinetics over the recommended dose range (150–600 mg/day given in either two or three divided doses; see Sect. 6), and there is no need to routinely monitor plasma concentrations of the drug [17, 23].
Pregabalin undergoes negligible hepatic metabolism and is eliminated almost entirely by renal excretion in the form of unchanged drug (Table 1). Accordingly, dose adjustments are not required in patients with hepatic impairment, but are necessary in patients with renal impairment (including elderly patients with age-related compromised renal function) and those undergoing haemodialysis [17, 28] (see Sect. 6).
Pregabalin has a very low potential for drug–drug interactions, as it is neither bound to plasma proteins nor metabolized and, furthermore, does not affect the cytochrome P450 system at therapeutic doses [17, 19, 22] (see Table 1). In in vivo studies, no clinically relevant pharmacokinetic interactions were observed between pregabalin and commonly used antiepileptic agents (e.g. phenytoin, carbamazepine and valproic acid) or other CNS-influencing medical products (lorazepam, oxycodone and ethanol), albeit pregabalin may enhance the effects of the latter [17, 19, 20].
3 Therapeutic Efficacy
Key inclusion and exclusion criteria for studies discussed in this section are summarized in Table 2. The mean age of trial participants ranged from 36 to 46 years [30–38], except in one study that exclusively enrolled elderly patients (mean age 72 years) [39]. Most (≈50–75 %) patients were women [30–36, 39] and most (≥70 %) were Caucasians [30–39].
3.1 Acute Treatment
This section discusses the results of short-term, randomized, double-blind, active comparator- and/or placebo-controlled, multicentre studies that have evaluated the efficacy of pregabalin:
-
as monotherapy for the treatment of patients with GAD who were not currently receiving antianxiety therapies [30–33, 35, 39–41] (Sect. 3.1.1);
-
as adjunctive therapy for patients with GAD who were not optimally responding to existing therapies [36] (Sect. 3.1.2); and
-
in facilitating taper off long-term benzodiazepine therapy [34] (Sect. 3.1.3).
All of the studies have been published in full, with the exception of study 1008-025 [41], in which neither pregabalin, nor lorazepam, demonstrated significant anxiolytic efficacy compared with placebo (and thus should be considered a failure [42]). Results from 1008-025 are, however, available from a European Medicines Agency (EMA) review of pregabalin in GAD [42].
3.1.1 Monotherapy
Study participants received pregabalin dosages in the range 150–600 mg/day (administered in two or three divided doses) for 4–6 weeks in six fixed-dose studies [30–32, 35, 40, 41] and for 8 weeks in two flexible-dose studies [33, 39]. In the fixed-dose studies, the starting dosage was up-titrated to the target dosage (if higher) over a period of ≤1 week [30–32, 35, 40, 41]. In the flexible-dose studies, pregabalin was started at a dosage of 150 mg twice daily for the first week [33] or up-titrated from an initial dosage of 50 mg/day to 150 mg/day during the first week [39]; thereafter, the dosage was adjusted, based on clinical response and tolerability (patients were maintained on the same dosage from weeks 6 to 8 in one study [39]). Active comparators included lorazepam (6 mg/day [30, 31, 41]), alprazolam (1.5 mg/day [32]) and venlafaxine (75–225 mg/day [33, 35]).
The primary efficacy parameter in these trials was the change from baseline to endpoint (i.e. week 4 [30, 31] or 8 [39] or last-observation-carried-forward [LOCF] endpoint [30–33, 35, 39, 40]) in the Hamilton Anxiety Rating Scale (HAM-A) total score in the active treatment group(s) compared with placebo. All efficacy analyses were performed on the intent-to-treat (ITT) population, defined as all patients who received at least one dose of study medication and had at least one post-baseline efficacy assessment [30–33, 35, 39–41].
Various aspects of the efficacy of pregabalin in the short-term treatment of GAD have been examined in post hoc pooled analyses of four or more of the afore-mentioned studies; results are available from full publications [43–49], abstracts [50–53] or a previous review [54].
3.1.1.1 Comparisons with Placebo
Treatment with fixed or flexible dosages of pregabalin in the range 150–600 mg/day demonstrated efficacy in the short-term treatment of GAD (Tables 3, 4). Excluding the ‘failed’ study 1008-025 [41] from consideration, the improvement in anxiety symptoms, as reflected by the change in HAM-A total score was, with one exception, significantly (p < 0.05) greater in patients receiving pregabalin than in those receiving placebo [30–33, 35, 39, 40]. The exception was the improvement in HAM-A total score in patients receiving a fixed dosage of pregabalin 150 mg/day in one study in which the difference did not attain statistical significance [31] (Table 3).
Results for key secondary endpoints, including the HAM-A psychic and somatic subscales (factors) and responder rates based on HAM-A and Clinical Global Impression of Improvement (CGI-I) criteria (see Table 3 for definitions), were generally consistent with the primary endpoint, particularly for fixed dosages of pregabalin in the range 200–600 mg/day (Tables 3, 4).
Pregabalin demonstrated a dose-response effect on anxiety symptoms that appeared to plateau at dosages of 300 mg/day, according to a pooled analysis of all six fixed-dose studies (n = 1,149 pregabalin and 484 placebo recipients) [47]. Higher dosages of pregabalin (300–600 mg/day) were consistently and similarly effective in reducing the HAM-A total score and HAM-A psychic and somatic factor scores versus placebo, in contrast to a lower dosage (150 mg/day) [47]. The authors of this analysis did not apply a curve-fitting procedure to their data, in contrast to the author of a smaller pooled analysis of five of the six fixed-dose studies [46]. Consistent with the results of an even smaller pooled analysis of four studies [49], the pooled five-study analysis [46] concluded that the dose-response curve for pregabalin on HAM-A total score reached a peak somewhere between 200 and 450 mg/day, with no additional effectiveness at 600 mg/day. According to the pooled five-study analysis [46], the treatment effect on psychic anxiety symptoms reached a peak at ≈400 mg/day, with a reduction in efficacy beyond this dosage. In contrast, the treatment effect on somatic anxiety symptoms continued to increase with increasing dosages of pregabalin up to 600 mg/day.
The results of other analyses suggest that pregabalin at dosages in the range 150–600 mg/day exerts a greater effect against psychic anxiety symptoms than somatic anxiety symptoms [47, 48]. The overall placebo-controlled effect sizes of pregabalin in reducing HAM-A total score (across seven studies; n = 1,352) and HAM-A psychic and somatic factor scores (across four studies; n = 913 patients) were 0.364, 0.349 and 0.239, respectively (all p < 0.001 vs. placebo) [48].
As regards the time to onset of anxiolytic activity, all dosages of pregabalin were associated with a significant improvement in the HAM-A total score within the first week of treatment. In pooled five-study analyses [52, 53], 44–54 % of pregabalin 150–600 mg/day recipients, as compared with 29–30 % of placebo recipients, had a ≥30 % improvement on the HAM-A total score by week 1. In the pooled six-study analysis [47], the proportions of patients achieving early and sustained improvement on the HAM-A psychic and somatic factors (defined as a ≥30 % reduction in HAM-A psychic and somatic factor scores by week 1 and sustained at that level or greater until endpoint) were significantly greater versus placebo with pregabalin 300–450 and 600 mg/day (all p < 0.001), but not 150 mg/day. In the flexible-dose study that exclusively enrolled elderly patients, pregabalin demonstrated a significant anxiolytic effect from the second week of treatment onwards (p < 0.01 vs. placebo) [39].
Pregabalin at fixed dosages in the range 200–600 mg/day demonstrated anxiolytic efficacy across a range of clinically relevant patient groups, based on the results of a pooled five-study analysis [50]. HAM-A responder rates were significantly (p < 0.02) higher in pregabalin (n = 868) than placebo (n = 414) recipients among males (56 vs. 39 %), females (51 vs. 32 %), elderly patients (55 vs. 27 %), patients with severe anxiety (baseline HAM-A total score ≥26; 61 vs. 39 %), patients with subsyndromic depression (baseline Hamilton Depression Rating Scale [HAM-D] total score ≥15; 49 vs. 31 %), patients with severe somatic symptoms (baseline HAM-A somatic factor score ≥12; 57 vs. 35 %) and patients with severe insomnia (60 vs. 37 %) [50]. A pooled six-study analysis [54] provided further evidence of the effectiveness of pregabalin, particularly at dosages of 300–600 mg/day, in subgroups of patients with moderate (baseline HAM-A total score 20–25) or severe anxiety [54].
Additional analyses assessing comorbidities in GAD suggested that concurrent depressive [51], gastrointestinal (GI) [43] and insomnia [44] symptoms had no effect on the anxiolytic efficacy of pregabalin and, moreover, were improved by treatment with pregabalin. Treatment with fixed dosages of pregabalin in the range 200–600 mg/day was consistently associated with significant (p < 0.05 vs placebo) improvements in HAM-A total scores, regardless of whether or not patients with GAD presented with subsyndromic depression (baseline HAM-D total score >15) [51], clinically significant levels of GI symptoms (baseline HAM-A item 11 [GI] score ≥3 [maximum = 4]) [43] or high levels of insomnia (baseline HAM-D sleep disturbance factor score ≥3 [maximum = 6]) [44].
Trial participants receiving pregabalin 150–600 mg/day also experienced significant (p < 0.05 vs. placebo) improvements in concurrent depressive symptoms, as measured by the HAM-D [45, 54] or Bech melancholia factor [45, 51]; mostly similar results were seen in subgroups of patients with subsyndromic depression (baseline HAM-D total score ≥15 or Bech melancholia factor score of ≥8) [45, 54]. Treatment with pregabalin 300–600 mg/day was, almost without exception, associated with significant (p ≤ 0.04 vs. placebo) improvements in GI symptoms, as measured by the HAM-A item 11 [43], or insomnia symptoms, as measured by the HAM-D sleep disturbance factor [44], irrespective of whether or not these concurrent symptoms were prominent at presentation. Only the improvement in GI symptoms in the subgroup of patients who presented with prominent GI symptoms and received pregabalin 600 mg/day did not attain statistical signficance [43].
3.1.1.2 Comparisons with Benzodiazepines
The efficacy of pregabalin, particularly at dosages in the range 300–600 mg/day, was apparently similar to that of benzodiazepines (alprazolam 1.5 mg/day [32] and lorazepam 6 mg/day [30, 31, 41]) in short-term studies that were not designed as formal head-to-head comparisons. In terms of the improvement in HAM-A total score, only one statistically significant between-group difference (favouring lorazepam over pregabalin 150 mg/day [30]) was observed across all four studies (Table 3).
These results were confirmed in the pooled six-study analysis [47] in which the mean improvements in endpoint HAM-A total scores and LOCF endpoint HAM-A psychic and somatic factor scores in benzodiazepine recipients were consistent with those seen in pregabalin 300–450 and 600 mg/day recipients [47]. Of note, treatment with pregabalin 300–450 mg/day was associated with significant improvements on 13 of the 14 individual HAM-A items (i.e. all except the intellectual psychic item), while that with pregabalin 600 mg/day was associated with significant improvements on 10 items (all except the intellectual psychic item, and the somatic sensory, genitourinary and autonomic somatic items). In contrast, treatment with benzodiazepines was associated with significant improvements in only five items (anxious mood, tension and insomnia psychic items, and somatic muscular and cardiovascular somatic items) [47].
The improvement in HAM-A total score at week 1 significantly (p < 0.05) favoured pregabalin 300 or 600 mg/day over alprazolam [32]. Overall, however, the rate of onset of anxiolytic activity appeared to be similar for pregabalin and benzodiazepines [54]. In the pooled six-study analysis [47], early and sustained improvement on the HAM-A psychic and somatic factors was achieved by ≈50 % of benzodiazepine and pregabalin 300–450 or 600 mg/day recipients.
3.1.1.3 Comparisons with Venlafaxine
The efficacy of pregabalin was apparently similar to that of venlafaxine (immediate-release [IR] [35] and extended-release [XR] [33] formulations) in short-term studies of GAD that were not designed as formal head-to-head comparisons. Treatment with pregabalin (either flexible dosages in the range 300–600 mg/day or fixed dosages of 400 or 600 mg/day) significantly improved HAM-A total score versus placebo in both studies [33, 35] (Table 4). In comparison, treatment with a fixed dosage of venlafaxine IR 75 mg/day significantly improved HAM-A total score compared with placebo in one study [35], unlike treatment with flexible dosages of venlafaxine XR 75–225 mg/day, which did not significantly improve HAM-A total score compared with placebo in the other study [33] (Table 4).
The onset of anxiolytic activity occurred earlier with pregabalin than with either the IR or XR formulations of venlafaxine [33, 35]. At week 1 (first assessment), the mean improvement in HAM-A total score was significantly greater with pregabalin 400 and 600 mg/day versus placebo (−7.0 and −7.7 vs. −4.8; p < 0.01 and p < 0.001), but not venlafaxine IR versus placebo (−4.6 vs. −4.8) [35]. In post hoc direct comparisons, both dosages of pregabalin demonstrated significantly (p ≤ 0.005) greater improvement in HAM-A total score at week 1 compared with venlafaxine IR [35].
Similarly, the least squares mean change (decrease) in HAM-A total score was significantly greater in pregabalin recipients than venlafaxine XR and placebo recipients, both on day 4 (−5.3 vs. −2.9 and −3.4; p = 0.001 and p = 0.008) and day 7 (−7.9 vs. −5.6 and −5.4; p = 0.005 and p = 0.002) [33]. By day 4, a ≥20 % improvement from baseline in HAM-A total score was achieved by significantly more pregabalin than venlafaxine XR and placebo recipients (36.3 vs. 18.3 and 20.3 %; p = 0.008 and p = 0.002) [33]. Pregabalin was also associated with significantly greater improvements than venlafaxine XR and placebo on the 100 mm Global Anxiety Visual Analog Scale (GA-VAS; 0 = ‘not at all anxious’ to 100 = ‘extremely anxious’), a patient-rated measure designed to capture early onset of symptom improvement, both at day 4 (−11.3 vs. −5.2 and −4.3; p = 0.01 and p = 0.002) and day 7 (−15.3 vs. −8.6 and −5.2; p = 0.01 and p < 0.0001) [33].
Like venlafaxine IR, pregabalin was effective in reducing secondary depressive symptoms, as measured by both the HAM-D (all dosages; see Table 4) [33, 35] and the Hospital Anxiety and Depression Scale (HADS) depression subscale (400 mg/day dosage only; p ≤ 0.02 vs. placebo) [35]. In addition, pregabalin was also effective in reducing symptoms of insomnia, as measured by the Medical Outcomes Study-Sleep factors (p ≤ 0.002 vs. placebo) [33].
3.1.2 Adjunctive Therapy
Of the 744 patients originally enrolled in this study, 356 had a suboptimal (i.e. partial) response at the end of 8 weeks of open-label therapy with escitalopram, paroxetine or venlafaxine XR. These partial responders were subsequently randomized to 8 weeks of double-blind treatment with either flexible dosages of pregabalin in the range 150–600 mg/day or placebo, in addition to the fixed dosage of SSRI or SNRI that they were already receiving. For patients who had not initiated GAD treatment prior to enrollment, a partial response was defined by meeting the following three criteria: (1) HAM-A total score ≥16, (2) <50 % reduction in HAM-A, and (3) CGI-I change rating ≤3. For those who had initiated GAD treatment prior to enrollment, a partial response was defined as some improvement in anxiety by physician assessment and HAM-A total score ≥16 [36].
The primary endpoint was the change in HAM-A total score from the double-blind baseline to the end of the double-blind phase. Baseline HAM-A total scores in either treatment arm were ≈21. Efficacy analyses were performed on the ITT population (all patients who received at least one dose of double-blind study medication) [36].
Adjunctive pregabalin improved anxiety symptoms in patients who had previously experienced an inadequate response to established treatments. Combination therapy with pregabalin plus an SSRI or SNRI was significantly more effective than placebo plus an SSRI or SNRI with respect to the primary endpoint (Fig. 1) and several secondary endpoints, including responder rates based on HAM-A criteria (47.5 vs. 35.2 %; p = 0.015) and CGI-S criteria (score ≤2 [‘normal’ to ‘borderline ill’], 43.8 vs. 31.8 %; p = 0.01). In the week-by-week analysis, the reduction in HAM-A total score significantly favoured adjunctive pregabalin over placebo at week 1 (p < 0.01) and, thereafter, at weeks 3 and 4 (both p < 0.05). Additionally, a significant improvement in anxiety symptoms occurred by week 1 of adjunctive treatment with pregabalin versus placebo on two patient-rated measures designed to capture early onset of symptom improvement, namely the GA-VAS (−6.7 vs. −2.4; p = 0.014) and the Daily Assessment of Symptoms-Anxiety Scale (p = 0.02) [36]. The time-to-sustained HAM-A improvement (defined as a ≥50 % reduction from baseline in HAM-A total score that was sustained through week 8) significantly favoured adjunctive pregabalin over placebo (p = 0.014); the between-group difference in the median time-to-sustained HAM-A improvement was estimated to be 1 week [36].
Efficacy of adjunctive pregabalin in the short-term treatment of generalized anxiety disorder. Least squares mean change in Hamilton Anxiety Rating Scale total score from baseline after 8 weeks of double-blind treatment [36]. HAM-A Hamilton Anxiety Rating Scale, PL placebo, PGB pregabalin, SNRI serotonin-noradrenaline reuptake inhibitor, SSRI selective serotonin reuptake inhibitor, *p = 0.012 vs. PL
3.1.3 Switching From Long-Term Benzodiazepine Therapy
Study participants (n = 138), all of whom who had previously received a benzodiazepine for between 8 and 52 weeks, initially entered a 2-week, open-label, alprazolam stabilization phase; those who had received a benzodiazepine other than alprazolam were first switched to the equivalent dose of alprazolam over a 2-week period before entering the 2-week stabilization phase. Thereafter, patients who continued to meet eligibility criteria (n = 106) were randomized to 12 weeks of double-blind treatment with either flexible dosages of pregabalin in the range 150–600 mg/day or placebo while undergoing a gradual alprazolam taper at a rate of 25 % per week. Patients were permitted up to 6 weeks to complete the alprazolam taper; only those who were successful continued to receive pregabalin or placebo for a further 6 weeks, after which they entered a 1-week study medication taper period [34].
The primary outcome was the proportion of patients who remained benzodiazepine-free from the end of the alprazolam taper phase until the end of the 6-week ‘benzodiazepine-free’ phase. Secondary outcome variables included an assessment of benzodiazepine-like withdrawal symptoms using the 20-item Physician Withdrawal Checklist (PWC-20; scores range from 0 to 60, with higher scores indicating more symptoms), the Clinical Global Impression-Severity scale (CGI-S; scores range from 1 = ‘normal’ to 7 = ‘extremely ill’) and the Patient Global Impression-Improvement scale (PGI-I; scores range from 1 = ‘very much better’ to 7 = ‘very much worse’). Efficacy analyses were performed on the ITT population (all patients who received at least one dose of study medication) [34].
Only 30 (53.6 %) and 19 (38.0 %) of the 56 and 50 patients randomized to pregabalin and placebo, respectively, completed the study; this high attrition rate reduced the power of the study to detect a significant difference on the primary outcome. Thus, while numerically favouring pregabalin over placebo, the between-group difference in the proportion of patients who remained benzodiazepine-free at the end of the 6-week ‘benzodiazepine-free’ phase (51.4 vs. 37.0 %), did not attain statistical significance [34].
However, pregabalin, as compared with placebo, significantly (p ≤ 0.04) reduced the severity of withdrawal symptoms, as assessed at the alprazolam taper endpoint (PWC total score: 6.8 vs. 12.6), week 6 of the ‘benzodiazepine-free’ phase (2.4 vs. 5.5) and the LOCF endpoint of the ‘benzodiazepine-free’ phase (6.5 vs. 10.3). Additionally, at the LOCF endpoint, pregabalin was associated with a significant reduction in anxiety symptoms compared with placebo, as well as significant improvements on the CGI-I (change rating: 2.6 vs. 3.5; p = 0.01), PGI-I (change rating: 2.7 vs. 3.7; p = 0.01) and CGI-S (change from baseline: −0.4 vs. +0.3; p = 0.003) [34].
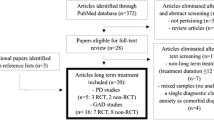
3.2 Long-Term Treatment
Data regarding long-term treatment of GAD with pregabalin monotherapy are available from two 6-month, randomized, double-blind, active comparator- and/or placebo-controlled, multicentre studies [37, 38] (see Table 2 for main inclusion criteria and notable exclusion criteria), and a 1-year, open-label, multicentre, safety trial [55].
The main aim of one controlled trial [38] was to evaluate the efficacy of pregabalin in preventing relapse in patients with GAD who responded to acute treatment (Sect. 3.2.1). The other controlled trial [37] examined the efficacy of pregabalin in maintaining the improvement in anxiety symptoms in patients with GAD who responded to acute treatment (Sect. 3.2.2). Since this second study was primarily designed to assess discontinuation effects following cessation of short- and long-term treatment with pregabalin (see Sect. 4.1.2), it is hereafter referred to as the ‘maintenance/discontinuation study’. The open-label safety trial [55] (Sect. 3.2.3) was an extension study that included, among others, patients with GAD who had previously completed one of two short-term studies of pregabalin monotherapy [35, 39].
3.2.1 Relapse Prevention Study
Of the 624 patients originally enrolled in the relapse prevention study, 339 had a clinical response (i.e. [1] HAM-A total score ≤11 and [2] ≥50 % reduction in HAM-A at ≥2 of the last 3 visits) at the end of 8 weeks of open-label therapy with a fixed dosage of pregabalin 450 mg/day. These responders were subsequently randomized to double-blind treatment with either the same dosage of pregabalin or placebo for up to 6 months or until patients relapsed or otherwise discontinued treatment [38]. The primary endpoint was the time to (protocol-defined) relapse. Secondary outcome variables included the Sheehan Disability Scale (SDS), which assesses functional impairment associated with anxiety. Efficacy analyses were performed on the ITT population (all patients who received at least one dose of double-blind study medication and had at least one post-double-blind baseline efficacy assessment) [38].
The time to relapse of GAD was significantly (p < 0.0001) longer in pregabalin-treated patients compared with placebo-treated patients. At the end of the 6-month double-blind phase, 71 (42.3 %) of 168 pregabalin recipients, as compared with 111 (65.3 %) of 168 placebo recipients, met the study definition of relapse. Relapse was evident in 25 % of pregabalin recipients by day 25; in contrast, 25 % of placebo recipients had relapsed by day 14, and 50 % had relapsed by day 23 [38].
In addition, 6 months of treatment with pregabalin was more effective than placebo in maintaining the reduction in anxiety symptoms that occurred during short-term treatment with pregabalin (e.g. HAM-A total scores: 25.3 vs. 25.1 at open-label baseline; 5.9 vs. 5.5 at double-blind baseline; and 7.2 vs. 11.8 [p = 0.0001] at LOCF endpoint of the double-blind phase), as well as maintaining the reduction in depressive symptoms that occurred during short-term treatment with pregabalin (HAM-D total scores: 14.7, vs. 14.0 at open-label baseline; 4.8 vs. 4.5 at double-blind baseline; and 6.0 vs. 8.7 [p < 0.0002] at LOCF endpoint) [38]. Long-term treatment with pregabalin was also more effective than placebo in maintaining the improvements in functional status that occurred during short-term treatment (SDS work, social and family subscale scores: 5.7 vs. 5.7, 5.9 vs. 5.8 and 5.8 vs. 5.6, respectively, at open-label baseline; 2.0 vs. 2.1, 2.0 vs. 2.1 and 2.3 vs. 2.2, respectively, at double-blind baseline; and 1.4 vs. 2.4 [p = 0.003], 1.7 vs. 2.4 [p = 0.017] and 1.5 vs. 2.4 [p = 0.003], respectively, at LOCF endpoint) [38].
3.2.2 Maintenance/Discontinuation Study
This study consisted of two consecutive 12-week treatment periods (periods 1 and 2). At the start of period 1, study participants (n = 615 [mean age 41–43 years; 58–65 % females; 80–85 % Caucasians]) were randomized to receive a flexible dosage of pregabalin (either low [150–300 mg/day] or high [450–600 mg/day]) or lorazepam (3–4 mg/day) for 6 weeks; those who had a response (i.e. CGI-I change rating of ≤2) continued fixed-dose therapy for 6 additional weeks, while non-responders exited the study. At the start of period 2, patients remaining in the study were re-randomized to either continue on the same fixed dosage of pregabalin or lorazepam (75 % of participants) or to switch to placebo (25 %). Patients switching to placebo at the end of period 1 underwent a 1-week double-blind taper and two post-discontinuation assessments, one immediately following the taper and the other 1-week post-taper. Additionally, all patients remaining in the study at the end of period 2 underwent a 1-week double-blind taper and two post-discontinuation assessments, one immediately following the taper and the other 1-week post-taper [37].
The primary efficacy measure was the HAM-A total score; efficacy analyses (which were performed on all randomized patients who had at least one efficacy assessment) used the LOCF approach [37]. Baseline HAM-A total scores across all treatment arms were ≈25.
Both low and high dosages of pregabalin were associated with substantial improvements in anxiety symptoms at the end of the initial 12-week treatment period; these improvements were maintained for patients who continued to receive pregabalin during the second 12-week treatment period (Fig. 2). Results were similar for the active comparator (Fig. 2); however, between-group statistical comparisons were not reported [37]. Marked improvements in anxiety symptoms were maintained among patients who switched from receiving pregabalin or lorazepam during period 1 to receiving placebo during period 2. Mean changes from baseline to week 24 in HAM-A total score were −14.9, −17.5 and −17.5 in patients who tapered off low-dosage pregabalin (n = 37), high-dosage pregabalin (n = 37) and lorazepam (n = 37), respectively [37].
Comparative efficacy of pregabalin and lorazepam in the treatment of generalized anxiety disorder. Mean changes in Hamilton Anxiety Rating Scale total score from baseline to weeks 12 and 24 during double-blind treatment [37]. HAM-A Hamilton Anxiety Rating Scale, LOR lorazepam, PGB pregabalin
Patients who received pregabalin (or lorazepam) experienced a substantial and sustained improvement in illness severity, regardless of whether they received either drug during both treatment periods or tapered off either drug during period 2. A similar outcome was seen with changes in CGI-S scores. Mean changes from baseline to week 24 in CGI-S scores were −2.4, −2.4 and −2.5 in patients who received low dosage pregabalin, high dosage pregabalin and lorazepam, respectively, throughout periods 1 and 2 (baseline CGI-S scores ranged from 4.4–4.7). In comparison, mean changes from baseline to week 24 in CGI-S scores were −2.0, −2.3 and −2.2 in patients who tapered off low-dosage pregabalin, high-dosage pregabalin and lorazepam, respectively (baseline CGI-S score for each taper group was 4.5) [37].
3.2.3 Safety Study
Overall, the subgroup of patients with GAD (n = 330) experienced a sustained improvement in illness severity during 1 year of open-label treatment with flexible dosages of pregabalin in the range 150–600 mg/day [55]. The mean CGI-S score was 3.6 at baseline, 2.5 and 2.3 at the week 27 and week 51 follow-up visits, and 2.6 at LOCF endpoint [55].
The proportion of patients with a CGI-S score of ≤2 (‘normal’ to ‘borderline ill’) was 15.2 % at baseline, 49.1 and 55.9 % at the week 27 and week 51 follow-up visits, and 48.1 % at LOCF endpoint. Almost all (>95 %) of the 330 patients showed no change in CGI-S status (59.5, 51.3 and 57.5 % at week 27, week 51 and LOCF endpoint, respectively) or shifted from being a non-responder (i.e. CGI-S score >2) to a responder (i.e. CGI-S score ≤2) [37.7, 45.3 and 38.1 % at week 27, week 51 and LOCF endpoint, respectively] [55].
4 Tolerability
4.1 General Profile
Short-term treatment with pregabalin at dosages in the range 150–600 mg/day was generally well tolerated, with adverse events being typically mild to moderate in intensity and transient (2–3 weeks) in duration [54, 56]. The most common treatment-emergent and treatment-related adverse events in pregabalin recipients were CNS events, in particular dizziness and somnolence, which were consistently reported to occur significantly more frequently on pregabalin than placebo (p-values not reported) [54, 56]. Dizziness and somnolence were also the two most frequent severe adverse events (reported by 2.3 and 2.6 % of pregabalin recipients, respectively), as well as being the adverse events most often associated with discontinuation of treatment [42] (Table 5).
There was, however, no clear relationship between the incidences of dizziness and somnolence and the dosage of pregabalin (above 150 mg/day), according to a pooled analysis of the six short-term, fixed-dose studies [42, 57]. The incidences of dizziness and somnolence were 13.8 and 23.8 %, respectively, with pregabalin 150 mg/day, 37.4 and 35.2 %, respectively, with pregabalin 300 mg/day, 38.2 and 29.8 %, respectively, with pregabalin 450 mg/day, and 35.1 and 39.2 %, respectively, with pregabalin 600 mg/day [57]. The observation that the incidences of dizziness and somnolence in the study that exclusively enrolled elderly patients [39] were notably lower than those in the GAD safety database [42] (20.3 vs. 31.1 and 13.0 vs. 29.2 %, respectively) may reflect the fact that this study used a flexible dosage schedule [42] (see Sect. 3).
The adverse event profile in the six-study safety database for GAD was qualitatively similar to that seen in larger safety databases that incorporated data from 22 [58] or 38 [59] randomized controlled trials of 4–17 weeks duration evaluating pregabalin in a range of indications. The more recent, smaller analysis (n = 5,802 pregabalin or placebo recipients), controlled for the underlying disease, unlike the earlier, larger analysis (n = 11,918), and concluded that the risk for pregabalin toxicity did not differ across distinct disorders.
In general, the long-term tolerability profile of pregabalin was consistent with its short-term tolerability profile [37, 38, 55]. For example, in the 1-year open-label study [55] (see Sect. 3.2 for further details), dizziness (10.3 %), somnolence (7.0 %), weight gain (4.2 %), insomnia (4.2 %), nausea (3.6 %) and headache (2.7 %) were the most common (incidence >2 %) treatment-related adverse events in the subgroup of 330 patients with GAD, all of whom received pregabalin dosages in the range 150–600 mg/day. Only 3.6 % of the treatment-related adverse events reported by the GAD subgroup were rated as severe [55].
No clinically meaningful changes in laboratory values, vital signs or the results of physical examinations were observed in long-term studies of pregabalin in patients with GAD [37, 38, 55].
According to the pooled analysis of the six short-term, fixed-dose studies [47], the discontinuation rate due to adverse events was lower in patients receiving pregabalin 150 (6.2 %), 300–450 (8.1 %) or 600 (18.0 %) mg/day than in those receiving a benzodiazepine (either alprazolam 1.5 mg/day or lorazepam 6 mg/day) [28.1 %].
Marked discontinuation symptoms were not observed following cessation of short-term [30–32] or long-term [37] treatment with either pregabalin or benzodiazepines in clinical trials. PWC-20 change scores, for example, were consistently low (≤5.2) following a 1-week taper off pregabalin 150–600 mg/day or lorazepam 3–6 mg/day after 4–24 weeks of treatment [30, 31, 37].
Of note, pregabalin 450 mg/day consistently produced less impairment of cognitive and psychomotor function than alprazolam 3 mg/day in a 3-day, randomized, double-blind, placebo-controlled, cross-over study in 24 healthy volunteers [60].
In terms of the comparative tolerability of pregabalin and venlafaxine in short-term studies [33, 35], dizziness and somnolence were reported more often in patients receiving pregabalin (e.g. 20.7 and 9.1 % for pregabalin 150–600 mg/day vs. 9.6 and 4.8 % for venlafaxine-XR 75–225 mg/day [33]), whereas nausea was reported more often in patients receiving venlafaxine-XR (12.4 vs. 25.6 % [33]). The incidence of severe adverse events with pregabalin was not significantly different from placebo (9.1 vs. 7.8 %), in contrast to that with venlafaxine XR (20.0 vs. 7.8 %; p = 0.002) [33]. Additionally, the rate of discontinuations due to adverse events significantly favoured pregabalin 400 mg/day over venlafaxine-IR 75 mg/day (6.2 vs. 20.4 %; p < 0.01) [35].
4.1.1 Weight Gain
Randomized clinical trials have identified weight gain as being a dose-dependent adverse event associated with the use of pregabalin [57, 61]. In the pooled analysis of the six short-term, fixed-dose studies, weight gain was reported as an adverse event by 3.7 % of pregabalin recipients versus 1.2 % of placebo recipients [56, 57]; the mean change in weight was 1.4 kg for pregabalin-treated patients versus 0.4 kg for placebo-treated patients [56]. Regarding the relationship between the incidence of this adverse event and pregabalin dosage, weight gain was reported by 1.4, 1.1, 7.3 and 5.1 % of patients receiving, respectively, pregabalin 150, 300, 450 and 600 mg/day in three divided doses, and by 1.3, 3.8 and 2.7 % of patients receiving, respectively, pregabalin 200, 400 and 600 mg/day in two divided doses [57]. Clinically significant weight gain (i.e. >7 % increase from baseline) occurred in 4.0 and 1.4 % of pregabalin and placebo recipients, respectively [56].
A clinically significant weight gain was experienced by 12.1 % of patients who received pregabalin 450 mg/day for up to 8 months in the relapse prevention study [38] (see Sect. 3.2.1 for further details); the majority of weight gain apparently occurred during the initial 8-week open-label phase of this trial. In the 1-year open-label study [55], ≈19 % of patients in the GAD subgroup reported a clinically significant weight gain at LOCF endpoint; the mean change in weight in this subgroup was 1.8 kg at week 27 and 2.0 kg at LOCF endpoint. These findings are generally consistent with the results of a large, pooled analysis (of 3,187 patients from 41 studies of pregabalin in a range of indications), which indicated that, over a 1-year period, ≈17 % of patients treated with pregabalin 150–600 mg/day experienced a clinically significant weight gain [61].
4.1.2 Potential for Abuse, Dependence and Withdrawal Symptoms
The potential for abuse of pregabalin is low, as the positive psychological effects of the drug are weak and not sustained during long-term treatment [62–64]. During the open-label phase of the relapse prevention study [38], 16.7 % of patients reported experiencing euphoria (median time to onset: on day 1; median duration: 4 days); however, only one patient (0.2 %) reported euphoria as being severe [38].
Additionally, unless stopped abruptly, pregabalin appears to have little risk for physical dependence or withdrawal [1, 3, 54]. Gradual discontinuation of the drug (i.e. tapering off over a ≤1-week period) after 4–24 weeks of treatment with dosages in the range 150–600 mg/day was not associated with clinically significant (benzodiazepine-like) withdrawal symptoms, based on assessment by the PWC-20 [30–32, 37, 38, 40]. PWC-20 change scores with pregabalin, as assessed 1–2 weeks after the start of a 1-week taper period, were low, ranging from 1.1 to 4.7 following cessation of 4–24 weeks of double-blind treatment [30, 31, 37, 40, 42]. A positive PWC-20 change score represents withdrawal symptoms or re-emerging anxiety; change scores in the range 12–25 (which have been reported after abruptly stopping benzodiazepines) are a potentially clinically significant indicator of a withdrawal syndrome [42].
Discontinuation symptoms following cessation of short- or long-term treatment with pregabalin have also been evaluated in the form of discontinuation-emergent signs and symptoms (DESS; defined as those spontaneously reported adverse events that developed or existed prior to, but worsened during, a 2-week period following taper initiation) [37, 38]. In the maintenance/discontinuation study [37] (see Sect. 3.2.2 for further details), DESS were reported by 32.7 and 22.3 % of patients following cessation of 12 and 24 weeks of double-blind treatment with pregabalin 150–300 mg/day, and by 36.2 and 31.2 % of patients following cessation of 12 and 24 weeks of double-blind treatment with pregabalin 450–600 mg/day. The most frequent DESS following cessation of 12 weeks of pregabalin therapy were insomnia (in 7.7 and 10.3 % of patients who stopped treatment with lower and higher dosages), headache (7.7 and 5.2 %) and nausea (5.8 and 6.9 %) [37]. Similarly, the most frequent DESS following cessation of 24 weeks of pregabalin therapy were insomnia (8.5 and 11.9 %), headache (3.2 and 4.6 %) and anxiety (4.3 and 6.4 %) [37]. DESS were reported by 31.0 and 13.3 % of patients who stopped 12 weeks of double-blind treatment with placebo after switching over from receiving lower and higher dosages of pregabalin for 12 weeks [37]. In the relapse prevention study [38], insomnia (3 %), nausea (3 %) and diarrhoea (3 %) were the most common DESS in the pregabalin group, as assessed during the 2-week discontinuation phase that followed the 24-week double-blind treatment phase. No DESS occurred at an incidence of ≥3 % in the placebo group [38].
The incidence of rebound anxiety in the maintenance/discontinuation study was 1.9 and 5.2 % following cessation of 12 weeks of treatment with lower and higher dosages of pregabalin, respectively, and 0 and 3.7 % following cessation of 24 weeks of treatment [37].
5 Pharmacoeconomic Profile
To date, pharmacoeonomic evaluations of pregabalin in GAD have been conducted in three continental European countries (Portugal [65], Spain [66–71] and Sweden [72]) and the UK [73]; several of these studies have been published in full [65–68, 71, 73].
Assuming a threshold value for willingness to pay of €30,000 per quality-adjusted life-year (QALY) gained, pregabalin monotherapy is predicted to be cost-effective relative to venlafaxine XR for the treatment of outpatients with GAD over a 1-year period in Spain [66] and Portugal [65] (Table 6). Similarly, pregabalin, either as monotherapy or adjunctive therapy, was predicted to be cost-effective relative to usual care [68, 69] or SSRI/SNRIs (also given alone or as adjunctive therapy) [67] for the treatment of patients with refractory GAD, including those with benzodiazepine- [67] and duloxetine- [69] refractory GAD, over a 6-month period in Spain (Table 6). Pregabalin-based therapy was associated with higher drug acquisition costs and total direct healthcare costs than the comparator(s) (Table 6). However, the higher overall costs were accompanied by more favourable clinical outcomes in terms of reductions in anxiety symptoms and gains in QALYs; in each case, the base-case incremental cost per QALY gained was below €30,000, the commonly accepted threshold for cost-effectiveness [65–69] (Table 6).
Estimates of the cost-effectiveness of pregabalin were robust to reasonable variations in the key assumptions and parameter values used in the underlying models [65–69]. For example, the incremental cost per QALY gained with pregabalin versus venlafaxine-XR was ≤€30,000 across most scenarios in one-way deterministic sensitivity analyses [65, 66]; it was highest (€58,093 [65] and €67,928 [66] per QALY gained) when the time horizon was the shortest considered (8 weeks).
The UK analysis [73] assessed the cost-effectiveness of pregabalin, three SSRIs (escitalopram, paroxetine and sertraline), two SNRIs (duloxetine and venlafaxine-XR) and ‘no pharmacological treatment’ (placebo); it was undertaken for the National Institute of Health and Clinical Excellence (NICE) guideline on the treatment of GAD [11]. Briefly, clinical evidence considered in the decision-tree model was synthesized using network meta-analytic techniques; cost data were derived from published literature and national sources, supplemented by expert opinion. The perspective adopted was that of the National Health Service and Personal Social Services in the UK, the time horizon was 42 weeks and the year of costing was 2011.
According to this analysis, pregabalin yielded 0.586 QALYs per patient at a total cost of £696 per patient. In comparison, placebo yielded 0.547 QALYs per patient at a total cost of £599 per patient, while sertraline (the most cost-effective drug) yielded 0.588 QALYs per patient at a total cost of £390 per patient [73]. The probability of being cost effective at a willingness-to-pay threshold of £20,000/QALY (i.e. the lower NICE cost-effectiveness threshold) was 0.7 % for pregabalin, 1.2 % for placebo and 75 % for sertraline [73].
Three analyses have examined the cost impact of initiating treatment with pregabalin by comparing total direct healthcare costs over a 6-month period after its introduction with those over a 6-month period before its introduction [70–72]. Two studies that adopted the perspective of the Spanish National Healthcare System (n = 254 [71] and 725 [70] analyzed patients) derived data from ADAN (Amplification of Definition of ANxiety), a 6-month, prospective, observational, cohort study [74]. In both cases, the direct costs considered were the costs of drug therapy, non-pharmacological treatments for GAD, medical visits (primary care, specialists and emergency room) and hospitalizations; the year of costing was 2009 [70, 71]. The third analysis was a retrospective, longitudinal database study from Sweden (n = 149 patients analyzed) [72].
In the Spanish studies, initiating adjunctive therapy with pregabalin significantly reduced total healthcare costs, both in a population of patients who were refractory to benzodiazepine therapy (by €289 vs. before initiation; p = 0.003) [71] and a population of patients who had previously had a partial response to SSRI treatment (by €478 vs. before initiation; p < 0.001) [70]. Furthermore, total healthcare costs after initiating add-on pregabalin were not significantly different from those after initiating add-on SSRI/SNRIs in benzodiazepine-refractory patients (€977 vs. €822) [71] or those after initiating usual care (i.e. switching to a different SSRI or another anxiolytic) in patients who had previously had a partial response to SSRI treatment (€1,565 vs. €1,406) [70], as larger increases in costs associated with drug acquisition (€305 for pregabalin vs. €187 for SSRI/SNRIs [p < 0.001] [71] and €296 for pregabalin vs. €27 for usual care [p = 0.001] [70]) were partially offset by larger reductions in costs associated with medical visits (€566 for pregabalin vs. €485 for SSRI/SNRIs [71] and €660 for pregabalin vs. €471 for usual care [p = 0.013] [70]).
Additionally, some clinical outcomes significantly favoured adjunctive pregabalin over the respective comparator; these included a greater reduction in benzodiazepine use (p < 0.001) versus SSRI/SNRIs in benzodiazepine-resistant patients [71], and greater improvements in anxiety symptoms (p < 0.0001), concomitant depressive symptoms (p < 0.0001) and quality of life (p < 0.001) versus usual care in patients who previously had a partial response to SSRI treatment [70].
Similar results were seen in the Swedish study [72]. Initiating treatment with pregabalin significantly reduced overall healthcare costs (from €7,635 before initiation to €4,802 after initiation; p = 0.0004); the reduction in healthcare costs was more marked in patients who were benzodiazepine users prior to starting pregabalin (from €8,461 before initiation to €4,622 after initiation; p = 0.0001) than in non-users (from €6,000 before initiation to €5,158 after initiation) [year of costing not stated]. The main driver behind the reduction in overall healthcare costs was the reduction in in-patient costs; drug costs were not specified separately [72].
Pharmacoeconomic analyses of pregabalin, in common with all pharmacoeconomic analyses, are subject to a number of limitations. Pharmacoeconomic analyses based on clinical trials extrapolate the results of such trials to the general population; however, patient populations, rates of compliance and major outcomes in clinical trials may differ from those observed in real-life practice. Modelled analyses, such as those presented in this section, rely on a number of assumptions and use data from a variety of sources. Results of pharmacoeconomic analyses may not be applicable to other geographical regions because of differences in healthcare systems, medical practice and unit costs.
6 Dosage and Administration
The recommended dose range of pregabalin in the treatment of GAD in adults is 150–600 mg, administered orally in two or three divided doses; an initial dose of 150 mg may be increased weekly in increments of 150 mg up to the maximum dose of 600 mg, based on individual patient response and tolerability [17].
Renal dysfunction necessitates dose adjustments. Patients with compromised renal function should receive a reduced daily dose based on creatinine clearance, while those receiving haemodialysis should, in addition to their daily dose, receive a (single) supplementary dose immediately after each 4-hour session [17].
Local prescribing information should be consulted for details of contraindications, special warnings and precautions relating to the use of pregabalin.
7 Place of Pregabalin in the Management of Generalized Anxiety Disorder
The relative advantages and disadvantages of drug classes widely used in the treatment of GAD (benzodiazepines, SSRI/SNRIs and pregabalin) have been summarized previously [54]. Benzodiazepines, historically the cornerstone of GAD pharmacotherapy, have a rapid onset of action, unlike SSRI/SNRIs, which have a delayed onset of action (2–3 weeks). However, the adverse event profile of benzodiazepines includes sedation, memory disturbances and psychomotor impairments; while they may be used on a short-term basis (e.g. to augment initial SSRI/SNRI treatment), they are not recommended for long-term use because of the risks for abuse, dependency and withdrawal syndrome upon discontinuation [13, 54]. In comparison, adverse events associated with SSRI/SNRIs include nausea and nervousness; common concerns during longer-term treatment include sexual dysfunction, weight gain, persistent disturbed sleep and the potential for discontinuation symptoms [3, 75]. Also, some SSRI/SNRIs possess moderate to strong cytochrome P450 inhibitory potential, resulting in possible drug–drug interactions [75, 76].
Pregabalin is a well established anxiolytic agent that has gained approval in the EU [17], albeit not in the US [77], for the treatment of GAD. According to the EU summary of product characteristics [17], an initial dosage of 150 mg/day can be increased weekly in increments of 150 mg up to the maximum dosage of 600 mg/day, based on individual patient response and tolerability (Sect. 6). However, recent results from clinical practice suggest that robust responses to short-term treatment can be achieved with lower dosages of pregabalin (i.e. 150–300 mg/day) [78]. Pregabalin can be administered in two or three divided doses (Sect. 6); twice-daily (as opposed to three-times daily) dosing may facilitate improved patient compliance. In terms of current guidelines, pregabalin is considered a first-line agent for the long-term treatment of GAD by the World Federation of Societies of Biological Psychiatry [13] (Sect. 1), but a second-line treatment (behind SSRI/SNRIs) by the NICE in the UK [11].
Several well designed clinical studies have demonstrated the efficacy of the drug in the treatment of moderate to severe GAD in adults, both in the short term (Sect. 3.1) and the long-term (Sect. 3.2). The anxiolytic effect of pregabalin is characterized by a rapid onset (typically ≤1 week) and broad spectrum activity against both the psychic and somatic symptoms of GAD. Additionally, the efficacy of pregabalin extends to patients with severe GAD and the elderly (Sect. 3.1).
Pregabalin demonstrates a dose-response effect on anxiety symptoms that appears to plateau at dosages of 300 mg/day; notwithstanding the effect size is small (i.e. pregabalin reduces the HAM-A total score by ≈2–4 points relative to placebo), it is nonetheless clinically meaningful, as the categorization of illness severity on the HAM-A scale is quite narrow [75]. In terms of the ideal goal of achieving complete symptom relief, reported remission rates after 4–8 weeks of treatment with pregabalin have ranged from 19 to 38 % in short-term clinical trials not considered ‘failures’ (Sect. 3.1.1).
Notably, the anxiolytic efficacy of pregabalin is unaffected by the presence of prominent insomnia or GI symptoms or subsyndromal depressive symptoms; indeed, in clinical trials, the drug specifically improved each of these comorbidities, which are typically encountered in GAD (Sect. 3.1.1.1). Regarding the effect on insomnia, pregabalin improves all forms of this sleep disturbance in patients with GAD; improvements in insomnia have been linked to reductions in functional impairment and improvements in health-related quality of life [79].
Given the chronicity of GAD, long-term treatment for at least 6–12 months is usually required [3, 80]. In long-term studies, pregabalin monotherapy sustained improvements in anxiety symptoms that occurred in response to short-term treatment and delayed the time to relapse of GAD compared with placebo (Sect. 3.2). Patients received pregabalin for 6–12 months in these trials (Sect. 3.2); however, the optimum duration of treatment remains unknown. Further characterization of long-term clinical outcomes with pregabalin (e.g. what proportion of patients responding to short-term treatment progress to remission and what proportion lose their initial response) is also desirable.
In addition to the numerous controlled trials evaluating monotherapy (Sects. 3.1 and 3.2), a large controlled trial has assessed adjunctive therapy with pregabalin in patients with GAD who responded partially (i.e. inadequately) to previous monotherapy with an SSRI or SNRI (Sect. 3.1.2). Almost half of these patients responded to the addition of pregabalin to the SSRI or SNRI that they were already receiving; response rates with pregabalin were significantly greater than those observed with placebo. These data suggest that augmentation with pregabalin is an effective strategy in patients who have not responded optimally to SSRI or SNRI monotherapy; in this regard, almost half of patients with GAD receiving an SSRI or SNRI fail to respond optimally and remain symptomatic [81]. Therefore, in the case of patients responding poorly to initial monotherapy with an SSRI/SNRI, add-on pregabalin can be considered as an alternative to switching to monotherapy with a different SSRI/SNRI.
Apart from its established efficacy, other aspects of pregabalin that favour its use in augmentation strategies, for example in SSRI or SNRI nonresponders, include its distinct mechanism of action relative to other anti-anxiety agents (α2δ binding at VDCCs; Sect. 2.1) and low potential for drug–drug interactions (Sect. 2.2) [36]. The same considerations also make pregabalin a potentially attractive candidate for use in switching strategies [36]; in this respect, switching to pregabalin facilitated successful discontinuation from long-term benzodiazepine therapy in a placebo-controlled trial, albeit this study was underpowered and therefore inconclusive (Sect. 3.1.3). Further studies evaluating the use of pregabalin in augmentation and switching strategies are warranted.
Short-term treatment with fixed or flexible dosages of pregabalin within the recommended range (150–600 mg/day; Sect. 6) was generally well tolerated, including in elderly patients; adverse events were typically mild to moderate in intensity and transient in duration (Sect. 4.1). The most notable CNS-related adverse events associated with pregabalin are dizziness and somnolence (apparently not related to dosage); these are the most common reasons for treatment discontinuation (Sect. 4.1). Due to the possibility that dizziness or somnolence will occur, a cautious approach to the use of pregabalin in patients at risk of falling (e.g. the elderly) is prudent [75]. In general, the long-term tolerability profile of pregabalin was consistent with its short-term tolerability profile (Sect. 4.1). Weight gain is recognized as being a dose-dependent adverse event associated with the use of pregabalin; clinically significant weight gain occurred in approximately one in every five or six patients with GAD who received recommended doses of the drug in long-term clinical trials (Sect. 4.1.1).
The potential for abuse of pregabalin is low (Sect. 4.1.2). Occasional cases of abuse have, however, been reported; caution is advised when prescribing pregabalin to patients with a history of substance abuse or alcoholism [79]. Pregabalin appears to have little risk for physical dependence or withdrawal, unless stopped abruptly (Sect. 4.1.2). When discontinued gradually (i.e. tapered off over a 1-week period), including after a treatment period of 6 months, recommended doses of pregabalin have generally not resulted in clinically meaningful discontinuation symptoms or rebound anxiety (Sect. 4.1.2).
Head-to-head studies sufficiently powered to directly compare the efficacy and tolerability of pregabalin with other drugs used as first-line treatments for GAD are needed, as none of the clinical trials conducted to date have been designed to detect differences between pregabalin and the active comparator (either a benzodiazepine [Sect. 3.1.1.2] or the SNRI venlafaxine [Sect. 3.1.1.3]). Although pooled data from these trials are suggestive of a similar onset of anxiolytic activity for pregabalin and benzodiazepines [56], the onset of action of benzodiazepines is acknowledged to be very fast (within 1 hour) [13], whereas that of pregabalin is recognized to be slower (within 1 week) [82]. The onset of action of pregabalin is, however, more rapid than that with SSRI/SNRIs, as exemplified by venlafaxine (Sect. 3.1.1.3). Furthermore, pregabalin has so far demonstrated the largest effect size of any GAD pharmacotherapy (0.5 as compared with, for example, 0.42 for SNRIs, 0.38 for benzodiazepines and 0.36 for SSRIs), based on indirect comparison [83]. The tolerability profile of pregabalin also appears to differ significantly from that of benzodiazepines (e.g. less sedation, less cognitive and psychomotor impairment, less risk of abuse, dependence and withdrawal) and SSRI/SNRIs (e.g. less GI adverse events and sexual dysfunction; Sect. 4.1; see also reviews by Montgomery [54] and Montgomery and Kasper [56]). Thus, pregabalin combines some of the positive aspects of the anxiolytic activity of both benzodiazepines and SSRI/SNRIs, while simultaneously avoiding some of the long-term limitations of these therapies. Among the clinical considerations that may favour the selection of pregabalin over alternative anxiolytic therapies are: the presence of prominent insomnia, GI or somatic anxiety symptoms; the presence of a comorbid pain syndrome; concerns about sexual dysfunction, drug–drug interactions, drug-related cognitive and psychomotor impairment; and concerns about the development of physical dependence and/or withdrawal symptoms [56].
It should be stressed that patients with MDD were excluded from the GAD trials of pregabalin (Sect. 3). Therefore, given that GAD and MDD often co-occur (Sect. 1), studies of the drug in patients with GAD-MDD comorbidity—ideally with an SSRI or SNRI as an active comparator—are desirable. Comparative studies of pregabalin in patients with other common co-existing conditions who were excluded from clinical trials (e.g. substance abuse and other anxiety disorders) are also warranted.
Cost-effectiveness is an important consideration in the treatment of GAD, given the significant economic burden of the disease on healthcare providers and society [73] (Sect. 1). To date, pharmacoeconomic analyses of pregabalin have been performed in three continental European countries and the UK (Sect. 5). The acknowledged limitations of modelling studies notwithstanding (Sect. 5), and despite being associated with higher drug acquisition and total healthcare costs, pregabalin is predicted to be cost-effective relative to venlafaxine XR in mental healthcare settings in Spain and Portugal. Similarly, pregabalin, either as monotherapy or adjunctive therapy, is predicted to be cost-effective relative to SSRI/SNRIs (alone or as add-on therapy) or usual care for the treatment of patients with refractory GAD (including benzodiazepine- and duloxetine-refractory GAD) in Spain (Sect. 5).
Although sertraline has not been formally approved for use in GAD, it was the most cost-effective among six agents used as first-line therapies in the UK (Sect. 5); on this basis, NICE recommended it as the drug of first choice for the treatment for GAD [11]. However, drug acquisition cost was an important factor in determining the relative cost effectiveness of these agents. Pregabalin had the highest drug acquisition cost at the time the analysis was conducted; had the acquisition cost of pregabalin equalled that of sertraline, it would have dominated escitalopram, paroxetine and venlafaxine-XR [73].
Of note, only direct costs were considered in cost-effectiveness studies; however, additional consideration of indirect costs could be potentially important, given the considerable impact that GAD has in terms of, for example, lost work productivity [73]. In this regard, pregabalin therapy has been shown to reduce the impact of anxiety symptomatology on work [38] (Sect. 3.2.1) and to improve work productivity [32, 84].
Other (cost-impact) studies from Spain suggest that initiating adjunctive therapy with pregabalin does not result in significantly greater total healthcare costs compared with add-on SSRI/SNRIs in benzodiazepine-refractory patients or usual care in patients who have only partially responded to previous SSRI treatment and is associated with some significantly improved clinical outcomes (Sect. 5).
In conclusion, pregabalin is a well established, EU-approved, anxiolytic agent that, along with SSRI/SNRIs, is considered a first-line agent for the long-term treatment of GAD by the World Federation of Societies of Biological Psychiatry. Recently, a study of SSRI/SNRI augmentation with pregabalin yielded positive results, while another study of switching from long-term benzodiazepine therapy to pregabalin was inconclusive; further investigations on these topics are warranted.
Data selection sources:
Relevant medical literature (including published and unpublished data) on pregabalin was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated 24 June 2014], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Pregabalin, GAD, generalised anxiety disorder, generalized anxiety disorder.
Study selection: Studies in adult patients with generalized anxiety disorder who received pregabalin. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Baldwin DS, Ajel K, Masdrakis VG, et al. Pregabalin for the treatment of generalized anxiety disorder: an update. Neuropsychiatr. 2013;9:883–92.
Katzman MA. Current considerations in the treatment of generalized anxiety disorder. CNS Drugs. 2009;23(2):103–20.
Both C, Kojda G, Lange-Asschenfeldt C. Pharmacotherapy of generalized anxiety disorder: focus and update on pregabalin. Expert Rev Neurother. 2014;14(1):29–38.
Brown TA, O’Leary TA, Barlow DH. Chapter 4. Generalized anxiety disorder. In: Barlow DH, editor. Clinical handbook of psychological disorders. 3rd ed. New York: Guilford Press; 2001. p. 154–208. http://commonweb.unifr.ch/artsdean/pub/gestens/f/as/files/4660/21992_121827.pdf. Accessed 28 Apr 2014.
Hoffman DL, Dukes EM, Wittchen HU. Human and economic burden of generalized anxiety disorder. Depress Anxiety. 2008;25(1):72–90.
Carter RM, Wittchen HU, Pfister H, et al. One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depress Anxiety. 2001;13:78–88.
Hunt C, Slade T, Andrews G. Generalized anxiety disorder and major depressive disorder comorbidity in the National Survey of Mental Health and Well-Being. Depress Anxiety. 2004;20(1):23–31.
Aina Y, Susman JL. Understanding comorbidity with depression and anxiety disorders. J Am Osteopath Assoc. 2006;106(5 Suppl 2):S9–14.
Kanwar A, Malik S, Prokop LJ, et al. The association between anxiety disorders and suicidal behaviours: a systematic review and meta-analysis. Depress Anxiety. 2013;30(10):917–29.
Dumais A, Lesage AD, Alda M, et al. Risk factors for suicide completion in major depression: a case–control study of impulsive and aggressive behaviors in men. Am J Psychiatry. 2005;162(11):2116–24.
National Collaborating Centre for Mental Health. Generalized anxiety disorder in adults—the NICE guideline on management in primary, secondary and community care. 2011. http://www.nice.org.uk/nicemedia/live/13314/52667/52667.pdf. Accessed 7 May 2014.
Hoge EA, Ivkovic A, Fricchione GL. Generalized anxiety disorder: diagnosis and treatment. BMJ. 2012;345:e7500. doi:10.1136/bmj.e7500.
Bandelow B, Zohar J, Hollander E, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive–compulsive and post-traumatic stress disorders—first revision. World J Biol Psychiatry. 2008;9(4):248–312.
Hoffman SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized, placebo-controlled trials. J Clin Psychiatry. 2008;69(4):621–32.
Uptodate®. Psychotherapy for generalized anxiety disorder. 2013. http://www.uptodate.com/contents/psychotherapy-for-generalized-anxiety-disorder. Accessed 27 Feb 2014.
Bandelow B, Sher L, Bunevicius R, et al. Guidelines for the pharmacological treatment of anxiety disorders, obsessive–compulsive disorder and posttraumatic stress disorder in primary care. Int J Psychiatry Clin Pract. 2012;16(2):77–84.
Pfizer Limited. Lyrica [25, 50, 75, 100, 200, 225 and 300 mg hard capsules; 20 mg/mL oral solution]: EU summary of product characteristics. 2013. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000546/WC500046602.pdf. Accessed 26 Feb 2014.
Frampton JE, Foster RH. Pregabalin: in the treatment of generalised anxiety disorder. [Erratum appears in CNS Drugs. 2007;21(6):481]. CNS Drugs. 2006;20(8):685–93 (discussion 94–5).
Ben-Menachem E. Pregabalin pharmacology and its relevance to clinical practice. Epilepsia. 2004;45(Suppl 6):13–8.
Tassone DM, Boyce E, Guyer J, et al. Pregabalin: a novel γ-aminobutyric acid analogue in the treatment of neuropathic pain, partial-onset seizures, and anxiety disorders. Clin Ther. 2007;29(1):26–48.
Micó JA, Prieto R. Elucidating the mechanism of action of pregabalin: α2δ as a therapeutic target in anxiety. CNS Drugs. 2012;26(8):637–48.
Bockbrader HN, Wesche D, Miller R, et al. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet. 2010;49(10):661–9.
Bockbrader HN, Radulovic LL, Posvar EL, et al. Clinical pharmacokinetics of pregabalin in healthy volunteers. J Clin Pharmacol. 2010;50(8):941–50.
Field MJ, Cox PJ, Stott E, et al. Identification of the alpha2-delta-1 subunit of voltage-dependent calcium channels as a molecular target for pain mediating the analgesic actions of pregabalin. Proc Natl Acad Sci USA. 2006;103(46):17537–42.
Taylor CP, Angelotti T, Fauman E. Pharmacology and mechanism of action of pregabalin: the calcium channel alpha2-delta (alpha2-delta) subunit as a target for antiepileptic drug discovery. Epilepsy Res. 2007;73(2):137–50.
Bellioti TR, Capiris T, Ekhato IV, et al. Structure-activity relationships of pregabalin and analogues that target the alpha(2)-delta protein. J Med Chem. 2005;48(7):2294–307.
Lotarski SM, Donevan S, El-Kattan A, et al. Anxiolytic-like activity of pregabalin in the Vogel conflict test in alpha2-1 (R217A) and alpha2-2 (R279A) mouse mutants. J Pharmacol Exp Ther. 2011;338(2):615–21.
Randinitis EJ, Posvar EL, Alvey CW, et al. Pharmacokinetics of pregabalin in subjects with various degrees of renal function. J Clin Pharmacol. 2003;43(3):277–83.
Corrigan BW, Pool WF, Posvar EL. Metabolic disposition of pregabalin in healthy volunteers [abstract no. PI-68]. Clin Pharmacol Ther. 2001;69:P18.
Pande AC, Crockatt JG, Feltner DE, et al. Pregabalin in generalized anxiety disorder: a placebo-controlled trial. Am J Psychiatry. 2003;160(3):533–40.
Feltner DE, Crockatt JG, Dubovsky SJ, et al. A randomized, double-blind, placebo-controlled, fixed-dose, multicenter study of pregabalin in patients with generalized anxiety disorder. J Clin Psychopharmacol. 2003;23(3):240–9.
Rickels K, Pollack MH, Feltner DE, et al. Pregabalin for treatment of generalized anxiety disorder: a 4-week, multicenter, double-blind, placebo-controlled trial of pregabalin and alprazolam. Arch Gen Psychiatry. 2005;62(9):1022–30.
Kasper S, Herman B, Nivoli G, et al. Efficacy of pregabalin and venlafaxine-XR in generalized anxiety disorder: results of a double-blind, placebo-controlled 8-week trial. Int Clin Psychopharmacol. 2009;24(2):87–96.
Hadley SJ, Mandel FS, Schweizer E. Switching from long-term benzodiazepine therapy to pregabalin in patients with generalized anxiety disorder: a double-blind, placebo-controlled trial. J Psychopharmacol (Oxf). 2012;26(4):461–70.
Montgomery SA, Tobias K, Zornberg GL, et al. Efficacy and safety of pregabalin in the treatment of generalized anxiety disorder: a 6-week, multicenter, randomized, double-blind, placebo-controlled comparison of pregabalin and venlafaxine. J Clin Psychiatry. 2006;67(5):771–82.
Rickels K, Shiovitz TM, Ramey TS, et al. Adjunctive therapy with pregabalin in generalized anxiety disorder patients with partial response to SSRI or SNRI treatment. Int Clin Psychopharmacol. 2012;27(3):142–50.
Kasper S, Iglesias-Garcia C, Schweizer E, et al. Pregabalin long-term treatment and assessment of discontinuation in patients with generalized anxiety disorder. Int J Neuropsychopharmacol. 2014;17(5):685–95.
Feltner D, Wittchen H-U, Kavoussi R, et al. Long-term efficacy of pregabalin in generalized anxiety disorder. Int Clin Psychopharmacol. 2008;23(1):18–28.
Montgomery S, Chatamra K, Pauer L, et al. Efficacy and safety of pregabalin in elderly people with generalised anxiety disorder. Br J Psychiatry. 2008;193(5):389–94.
Pohl RB, Feltner DE, Fieve RR, et al. Efficacy of pregabalin in the treatment of generalized anxiety disorder: double-blind, placebo-controlled comparison of BID versus TID dosing. J Clin Psychopharmacol. 2005;25(2):151–8.
Pande AC, Crockatt JG, Janney C, et al. Three randomised, placebo-controlled double-blind trials of pregabalin treatment of generalised anxiety disorder (GAD) [abstract no. P.3.025]. Int J Neuropsychopharmacol. 2000;3(Suppl 1):S344.
European Medicines Agency. Product name: LYRICA. Product no. EMEA/H/C00546/II0004. Scientific discussion. 2005. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion_-_Variation/human/000546/WC500046605.pdf. Accessed 7 Mar 2014.
Stein DJ, Bruce Lydiard R, Herman BK, et al. Impact of gastrointestinal symptoms on response to pregabalin in generalized anxiety disorder: results of a six-study combined analysis. Int Clin Psychopharmacol. 2009;24(3):126–32.
Montgomery SA, Herman BK, Schweizer E, et al. The efficacy of pregabalin and benzodiazepines in generalized anxiety disorder presenting with high levels of insomnia. Int Clin Psychopharmacol. 2009;24(4):214–22.
Stein DJ, Baldwin DS, Baldinetti F, et al. Efficacy of pregabalin in depressive symptoms associated with generalized anxiety disorder: a pooled analysis of 6 studies. Eur Neuropsychopharmacol. 2008;18(6):422–30.
Boschen MJ. Pregabalin: dose-response relationship in generalized anxiety disorder. Pharmacopsychiatry. 2012;45(2):51–6.
Lydiard RB, Rickels K, Herman B, et al. Comparative efficacy of pregabalin and benzodiazepines in treating the psychic and somatic symptoms of generalized anxiety disorder. Int J Neuropsychopharmacol. 2010;13(2):229–41.
Boschen MJ. A meta-analysis of the efficacy of pregabalin in the treatment of generalized anxiety disorder. Can J Psychiatry. 2011;56(9):558–66.
Bech P. Dose-response relationship of pregabalin in patients with generalized anxiety disorder. A pooled analysis of four placebo-controlled trials. Pharmacopsychiatry. 2007;40(4):163–8.
Pollack MH, Walsh T, Cohn CK, et al. Pregabalin in GAD: efficacy in clinically-relevant subtypes [abstract no. NR224]. 157th Annual Meeting of the American Psychiatric Association; 1–6 May 2004; New York (NY).
Pollack M. Pregabalin in generalized anxiety disorder: influence of subsyndromic depression [abstract no. P.3.056]. Eur Neuropsychopharmacol. 2003;13(Suppl 4):377.
Montgomery SA, Rickels K, Bielski RJ. Pregabalin in GAD: speed of onset [abstract no. NR775]. 156th American Psychiatric Association Annual Meeting; 17–22 May 2003; San Francisco (CA).
Montgomery SA. Pregabalin in generalized anxiety disorder: speed of onset [abstract no. P.3.054]. Eur Neuropsychopharmacol. 2003;13(Suppl 4):376–7.
Montgomery SA. Pregabalin for the treatment of generalised anxiety disorder. Expert Opin Pharmacother. 2006;7(15):2139–54.
Montgomery S, Emir B, Haswell H, et al. Long-term treatment of anxiety disorders with pregabalin: a 1 year open-label study of safety and tolerability. Curr Med Res Opin. 2013;29(10):1223–30.
Montgomery S, Kasper S. Pharmacotherapy update: pregabalin in the treatment of generalized anxiety disorder. Clin Med Insights Ther. 2010;2:189–202.
Boehm G, Hughes ATD. NDA: 21-446, 21-273, 21-724; drug: pregabalin (Lyrica). Review and evaluation of clinical data: NDA safety review. 2004. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2005/021724s000_MedR_P2.pdf and http://www.accessdata.fda.gov/drugsatfda_docs/nda/2005/021724s000_MedR_P3.pdf. Accessed 5 Apr 2014.
Zaccara G, Perucca P, Gangemi PF. The adverse event profile of pregabalin across different disorders: a meta-analysis. Eur J Clin Pharmacol. 2012;68(6):903–12.
Zaccara G, Gangemi P, Perucca P, et al. The adverse event profile of pregabalin: a systematic review and meta-analysis of randomized controlled trials. Epilepsia. 2011;52(4):826–36.
Hindmarch I, Dawson J, Stanley N. A double-blind, placebo- and positive-internal-controlled (alprazolam) investigation of the cognitive and psychomotor profile of pregabalin in healthy volunteers. Psychopharmacology (Berl). 2005;183:133–43.
Cabrera J, Emir B, Dills D, et al. Characterizing and understanding body weight patterns in patients treated with pregabalin. Curr Med Res Opin. 2012;28(6):1027–37.
Schwan S, Sundstrom A, Stjernberg E, et al. A signal for an abuse liability for pregabalin-results from the Swedish spontaneous adverse drug reaction reporting system. Eur J Clin Pharmacol. 2010;66(9):947–53.
Filipetto FA, Zipp CP, Coren JS. Potential for pregabalin abuse or diversion after past drug-seeking behavior. J Am Osteopath Assoc. 2010;110(10):605–7.
Chalabianloo F, Schjøtt J. Pregabalin and its potential for abuse [Article in Norwegian]. Tidsskr Nor Laegeforen. 2009;129(3):186–7.
Miguel LS, Miguel NS, Inês M. A cost-utility analysis of pregabalin versus venlafaxine XR in the treatment of generalized anxiety disorder in Portugal. Cost Eff Resour Alloc. 2013;2013(11):8.
Vera-Llonch M, Dukes E, Rejas J, et al. Cost-effectiveness of pregabalin versus venlafaxine in the treatment of generalized anxiety disorder: findings from a Spanish perspective. Eur J Health Econ. 2010;11(1):35–44.
De Salas-Cansado M, Olivares JM, Álvarez E, et al. Pregabalin versus SSRIs and SNRIs in benzodiazepine-refractory outpatients with generalized anxiety disorder: a post hoc cost-effectiveness analysis in usual medical practice in Spain. Clinicoecon. 2012;4:157–68.
De Salas-Cansado M, Álvarez E, Olivares JM, et al. Modelling the cost-effectiveness of pregabalin versus usual care in daily practice in the treatment of refractory generalised anxiety disorder in Spain. Soc Psychiatry Psychiatr Epidemiol. 2013;48(6):985–96.
Carrasco JL, Olivares JM, Álvarez E, et al. Cost-effectiveness of pregabalin versus usual care in duloxetine-refractory out-patients with generalized anxiety disorder: an economic evaluation under medical usual practice in mental health centers [poster]. International Society for Pharmacoeconomics and Outcomes Research 12th Annual European Congress; 24–27 Oct 2009; Paris.
Carrasco JL, Olivares JM, Álvarez E, et al. Adjunctive therapy with pregabalin in generalized anxiety disorder patients with partial response to SSRI treatment: a cost-consequences analysis in medical practice in Spain [poster]. International Society for Pharmacoeconomics and Outcomes Research 16th Annual European Congress; 2–6 Nov 2013; Dublin.
Carrasco JL, Álvarez E, Olivares JM, et al. A comparative cost-analysis of initiating pregabalin or SSRI/SNRI therapy in benzodiazepine-resistant patients with generalized anxiety disorder in Spain. Actas Esp Psiquiatr. 2013;41(3):164–74.
Löfroth E, Myrén KJ, Sandelin R. Cost impact of initiating pregabalin treatment in Swedish patients with generalized anxiety disorder [poster]. International Society for Pharmacoeconomics and Outcomes Research 13th Annual European Congress; 6–9 Nov 2010; Prague.
Mavranezouli I, Meader N, Cape J, et al. The cost effectiveness of pharmacological treatments for generalized anxiety disorder. Pharmacoeconomics. 2013;31(4):317–33.
Álvarez E, Carrasco JL, Olivares JM, et al. Broadening of generalized anxiety disorders definition does not affect the response to psychiatric care: findings from the observational ADAN study. Clin Pract Epidemiol Men Health. 2012;8:158–68.
Wensel TM, Powe KW, Cates ME. Pregabalin for the treatment of generalized anxiety disorder. Ann Pharmacother. 2012;46(3):424–9.
Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008;30(7):1206–27.
Parke-Davis Div of Pfizer Inc. Lyrica (pregabalin) capsules, oral solution: US prescribing information. 2013. http://labeling.pfizer.com/ShowLabeling.aspx?id=561. Accessed 24 Jun 2014.
Kasper S, Brasser M, Schweizer E, et al. How well do randomized controlled trial data generalize to ‘real-world’ clinical practice settings? A comparison of two generalized anxiety disorder studies. Eur Neuropsychopharmacol. 2014;24(1):125–32.
Holsboer-Trachsler E, Prieto R. Effects of pregabalin on sleep in generalized anxiety disorder. Int J Neuropsychopharmacol. 2013;16(4):925–36.
Fricchione GL. Generalized anxiety disorder. N Engl J Med. 2004;351(7):675–82.
Samuel M, Zimovetz EA, Gabriel Z, et al. Efficacy and safety of treatments for refractory generalized anxiety disorder: a systematic review. Int Clin Psychopharmacol. 2011;26(2):63–8.
Bandelow B, Wedekind D, Leon T. Pregabalin for the treatment of generalized anxiety disorder: a novel pharmacologic intervention. Expert Rev Neurother. 2007;7(7):769-81.
Hidalgo RB, Tupler LA, Davidson JR. An effect size analysis of pharmacologic treatments for generalized anxiety disorder. J Psychopharmacol. 2007;21(8):864–72.
Taylor TN, Feltner DE, Goodrich J. Pregabalin improves patient-reported work productivity in patients with GAD (abstract no. NR812). American Psychiatric Association 2003 Annual Meeting; 17–22 May 2003; San Francisco (CA).
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the authors on the basis of scientific and editorial merit. James Frampton is a salaried employee of Adis/Springer.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: M. J. Boschen, School of Applied Psychology and Griffith Health Institute, Griffith University, Southport, Australia; J. Carrasco, Department of Psychiatry, Hospital Clínico San Carlos, Madrid, Spain; S. Kasper, Department of Psychiatry and Psychotherapy, Medical University of Vienna, Vienna, Austria; V. G. Masdrakis, Department of Psychiatry, Athens University Medical School, Athens, Greece; J. A. Micó, Department of Neuroscience, Pharmacology and Psychiatry, CIBER of Mental Health, CIBERSAM, Instituto de Salud Carlos III, University of Cádiz, Cádiz, Spain; S. A. Montgomery, Imperial College School of Medicine, University of London, London, UK; K. Rickels, Department of Psychiatry, Mood and Anxiety Disorders Section, University of Pennsylvania School of Medicine, Philadelphia, PA, USA; G. Zaccara, Unit of Neurology, Department of Medicine, Florence Health Authority, Firenze, Italy.
Rights and permissions
About this article
Cite this article
Frampton, J.E. Pregabalin: A Review of its Use in Adults with Generalized Anxiety Disorder. CNS Drugs 28, 835–854 (2014). https://doi.org/10.1007/s40263-014-0192-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-014-0192-0