Abstract
Purpose
To model the cost-effectiveness (CEA) of the use of pregabalin versus usual care (UC) in outpatients with refractory generalised anxiety disorder (GAD) treated in daily practice in mental health settings in Spain.
Methods
This CEA model used data extracted from a 6-month prospective non-interventional trial: the Amplification of Definition of ANxiety (ADAN) study, which was conducted to determine the cost-of-illness in GAD subjects. Refractory subjects were those who reported persistent symptoms of anxiety and showed suboptimal response in the Hamilton-anxiety scale (HAM-A ≥ 16) after a standard dose regimen of anxiolytics other than pregabalin, alone or in combination, over 6 months. The pregabalin arm was documented with data extracted from patients who received pregabalin in the study for the first time, added or replacing the existing therapy. In the UC arm, treatment might include one or more of the following: a serotonin selective reuptake inhibitor, a serotonin–norepinephrine reuptake inhibitor, other anti-depressants, a benzodiazepine or an anti-epileptic drug other than pregabalin. The time horizon of the modelling was 6 months in the base-case scenario, and the National Health System perspective was chosen to calculate costs. Effectiveness was expressed as quality-adjusted life years (QALYs) gained, which were derived using the EQ-5D questionnaire, at baseline and end-of-trial visits. Results of the CEA model was expressed as an incremental cost-effectiveness ratio (ICER) per QALY gained. Probabilistic sensitivity analysis using bootstrapping techniques was also carried out to obtain the cost-effectiveness plane and the corresponding acceptability curve.
Results
Data from a total of 429 subjects per arm (mean HAM-A score 25.7) meeting eligible criteria for inclusion in CEA modelling were extracted from the original trial. Compared with UC, pregabalin (average dose 218 mg/day) was associated with significantly higher QALY gain; 0.1209 ± 0.1030 versus 0.0994 ± 0.0979 (P = 0.003), but increased healthcare costs as well; €1,272 ± 1,240 versus €1,070 ± 1,177 (P < 0.069) and drug costs €525 ± 252 versus 219 ± 211 (P < 0.001), resulting in an ICER of €15,804/QALY (95 % CI 6,661; 37,186) for healthcare costs and €15,165/QALY (7,947; 31,754) when drug costs were considered alone. A total of 94 % of re-samples fell below the threshold of €30,000 per QALY.
Conclusions
This evaluation modelling suggests that pregabalin may be cost-effective in comparison with UC in outpatients with refractory GAD treated in mental healthcare settings in daily practice in Spain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anxiety disorders are one of the most prevalent psychiatric health conditions, with generalised anxiety disorder (GAD) being one of the most common in primary care and mental health settings [1]. The lifetime prevalence of GAD was estimated to be 2.8 % in Europe and 5.7 % in the United States [2, 3]. In a clinical setting, however, GAD prevalence has been estimated at 7.3 % in primary care and mental healthcare settings, which may represent 13 % of the conditions seen in psychiatric outpatient clinics [4, 5]. Subjects with GAD present a higher rate of medical co-morbidities than other patients, seek more medical care, and undergo extensive medical testing (to rule out other pathologies), making GAD a challenging medical condition to diagnose [6, 7].
Psychological complaints usually included uncontrollable persistent worry and tension about daily life events for at least the previous 6 months. GAD is characterised by excessive, uncontrolled, and often irrational and disproportionate concern about daily issues [8]. Patients suffered from somatic anxiety symptoms in addition to agitation, irritability, difficulty concentrating, muscle tension, sleep disorders and fatigue. Generally, subjects with GAD experienced symptoms for 5–10 years before being diagnosed and treated accordingly [9]. Without treatment, only a small percentage of patients achieved a complete remission of their symptoms (the chance of relapse is 0.15 in 1 year and only 0.25 after 2 years) [10]. Given the chronic course of GAD and its low remission rates, normal functioning in people with GAD is substantially impaired [11] and these patients have lower perceived quality of life than non-anxious controls and a lower degree of social functioning than patients with chronic physical condition such arthritis or diabetes [12]. Misdiagnosis or under diagnosis, which is treated inappropriately or late, can lead to a vicious circle of exacerbated existing illness and the development of new illnesses, fostering further anxiety, demoralisation and depression.
The persistent nature of GAD and the vicious circle of medical and psychiatric conditions make GAD an anxiety disorder which considerably impairs, resulting in a high use of healthcare resources [13], a use higher than that of obsessive–compulsive disorder and panic disorder patients, among others [14]. Thus, considerable burden is associated with this disorder, not only for the patient but also for the healthcare system. The use of healthcare resources and subsequent related costs may be different depending on how patients with GAD are treated or how they respond to therapy. Moreover, patient response to therapy may vary in terms of outcome values such as responder rate and/or quality of life. GAD patients not only use healthcare resources related to their anxiety but are also more likely to seek treatment for other somatic diseases, pain, and sleep disorders [15]. However, although this disorder represents 25 % of anxiety consultations, only 30 % of these are successfully diagnosed, and treatment is only suitable for an even smaller number [15].
According to current guidelines [8], the drugs recommended as first-line treatment for GAD are selective reuptake inhibitors (SSRIs) (escitalopram, paroxetine, and sertraline among others), serotonin–norepinephrine reuptake inhibitors (SNRIs) (venlafaxine and duloxetine), and the calcium channel modulator pregabalin. Pregabalin is a third generation anti-epileptic drug (AED) recommended and also licensed for the treatment of GAD in Europe [16–19]. In reality, however, the clinical management of GAD includes a variety of different benzodiazepines, anti-depressants, and anti-epileptics in addition to those mentioned above.
In addition to the clinical evidence of the effectiveness of a drug in daily practice, health policy decision makers should also be aware of the financial aspects that will allow them to determine the efficiency of new treatments and thus make optimal use of the existing limited economic resources. Thus, the aim of the present study was to model the cost-effectiveness of pregabalin versus usual care in refractory outpatients with GAD treated according to daily practice in mental healthcare settings in Spain.
Methods
Data source
The data for this economic analysis modelling the CE of pregabalin versus UC were taken from a 6-month prospective non-interventional cohort trial: the Amplification of Definition of ANxiety (ADAN) study, which was conducted to assess the effect of broadening Diagnostic Statistical Manual (DSM)-IV diagnostic criteria for GAD on the clinical evolution of patients, their use of resources and the corresponding costs [20]. The ADAN study was an open, multicentre, epidemiological, non-interventional and prospective study conducted in 618 Spanish outpatient psychiatric clinics between 2007 and 2008. Trained psychiatrists, with at least 5-year experience in mental health diseases diagnosis, who participated in the study, were asked to select consecutive patients diagnosed of GAD according to DSM-IV criteria [21] and the so-called broad criteria, until the predetermined sample size was obtained. Patients of both genders, aged 18 or above, who had provided their written informed consent to participate in the study, were refractory to previous therapy and without previous exposition to pregabalin were included in the study. For the CEA shown here, we included data from patients with a standard diagnosis of GAD according to DSM-IV criteria only. Refractory was defined as subjects with persistent symptoms/suboptimal response, a Hamilton-anxiety (HAM-A) scale [22, 23] score ≥16 and a Clinic Global Impression (CGI) [24] score ≥3 at baseline, after a standard dose regimen of any anti-anxiety drug, alone or in combination, for at least 6 months, given prior to the baseline study visit. In addition to the main objective, the ADAN study also assessed self-perceived health-related quality-of-life using the EQ-5D questionnaire [25, 26], use of healthcare resources and related costs.
Economic model design and patient data extraction procedure
The CEA is a comparative analysis which has the purpose of estimating the ratio between the relative expenditure (cost) of a health-related intervention and the outcomes (effectiveness) it produces. Cost-effectiveness is typically expressed as an incremental cost-effectiveness ratio (ICER): the ratio between the difference in the costs and health benefits of two interventions. This is a measure of the additional cost per additional unit of health gain produced by one intervention compared to another. The cost-effectiveness threshold is often referred to as society’s willingness to pay for an additional unit of health gain (QALY), i.e. if the ICER for a specific intervention is less than the cost-effectiveness threshold, then society, or its agents, will be considered it affordable and, thus, willing to fund it, and conversely if the ICER is greater than the threshold society will not be willing to fund it. A threshold value is often set by policy makers, who may decide that only interventions within a given ICER threshold range are cost effective, although decisions on funding may be more complex and subject to additional factors. The threshold monetary value usually is different throughout western countries, and it depends on what is considered affordable in every country [27]. In Spain, there is generally no accepted cost-effectiveness threshold value. However, an ICER equal or less than €30,000 per quality-adjusted life year (QALY) gained is usually considered cost-effective [28]. This is also in the range of that used by the NICE in the United Kingdom [29, 30].
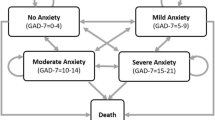
To model this CEA, a nested case–control study methodology was applied to randomly extract the data for analysis from the ADAN trial [21] which included patients who met the DSM-IV criteria for the diagnosis of GAD only. Data from subjects in both cohorts were consecutively selected from the blinded study database in a 1:1 ratio meaning that there was one control for every clinical case. Patients receiving pregabalin (as monotherapy or add-on to the existing treatment) from the baseline visit were the clinical cases and subjects receiving UC, not including pregabalin, were the controls. In the UC arm, treatment might include one or more of the following: a SSRI, a SNRI, other anti-depressants, a benzodiazepine or an anti-epileptic drug other than pregabalin, all of which have an approved indication for treating anxiety symptoms, at the clinical discretion of the physician treating the patients. The design involved a simple decision-tree model representing the data extracted and a final sample of the clinical cases and controls used for the analysis (see Fig. 1).
Resource utilisation and costs
Cost refers to the resources employed for the intervention, usually measured in monetary terms, such as Euros. The cost of each treatment arm is equal to the sum of purchased medical and non-medical resources used (often called “direct costs”) and unpurchased resources, such as patient loss of productivity or unpaid family member/caregiver support (called “productivity costs” or “indirect costs”). For this economic evaluation, we selected a third party payer perspective, that of the Spanish National Healthcare System (NHS), to carry out the CEA. Therefore, only healthcare resource utilisation (HRU) and corresponding costs were computed. The time horizon used in the model was 6 months, as with duration of the ADAN study. Subsequently, no time discounts were applied. HRU was recorded at baseline and end-of-trial visit by means of a HRU questionnaire designed ad hoc for this study. These resources, all related with the GAD condition, included medical visits (primary care, specialists and emergency room visits), days of hospitalisations, drug treatment for GAD symptoms and non-pharmacological treatment for GAD such as physiotherapy, psychotherapy, relaxation techniques, etc. (see Table 1).
The cost of HRU was calculated by multiplying the number of a resource used during the study by its unitary price (Table 1), and was expressed during a 6-month period before the visit when recording took place. Thus, from a cost perspective, the study included two visits: the baseline and the end-of-trial visits. The Spanish Pharmaceutical Drug Catalogue [31] was used for the unit price of drugs, where cost was estimated as retail price + value added tax (VAT) of the cheapest generic medication available, or cheapest pharmaceutical medicinal product when a generic medication or reference price was unavailable. The cost of non-pharmacological treatments, medical visits, and hospitalisations were obtained from the eSALUD [32] healthcare costs database for 2008, updated with the 2008 inflation rate [32]. Finally, some non-pharmacological resources were priced according to expert opinion and/or directly from the vendor/provider.
Effectiveness measures
The measurements used to determine the effectiveness of treatments for this CEA during the 6-month study were derived from the ADAN trial, and were expressed as QALY gained, which was calculated by trapezoidal approximation using utility values from the Spanish version of the EQ-5D questionnaire [33], which was administered twice; at baseline and end-of-trial visits. The EQ-5D is a generic self-reported measure of health-related quality of life, used frequently in clinical and economic evaluations [25, 26]. The degree of impairment is assessed in five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is defined by three health states (no problems = 1 point, some or moderate problems = 2 points, extreme problems = 3 points) completed by the patient in order to assign appropriate utility values to each patient health profile. All possible combinations generate a total of 243 possible health states, which may be transformed using appropriate algorithms to calculate a utility index value ranging from 1 (equivalent to perfect health) to 0 (equivalent to death). The result is an equivalent rate (ET) over time or weighting system that reflected the patient’s preference for all health states generated by the EQ-5D [25, 26].
The other effectiveness measurements were the change in the Spanish version of the HAM-A scale [22], such as responder rate (% of patients with a reduction ≥50 % at end-of-trial in comparison to the baseline intensity of anxiety symptoms assessed with the HAM-A scale) and percentage of subjects without anxiety symptoms at end-of-trial (HAM-A ≤ 9 points). The HAM-A is a 14-item scale, each with a score between 0 (absence) and 4 (severe) that explored the patients’ degree of anxiety [22, 23]. The possible score ranges from 0 to 56 points and allows for a global score and two subscales, one for psychic symptoms and the other for somatic symptoms [21, 22]. In the study, HAM-A scores varied with treatment from patient to patient, with HAM-A scores of ≤9 as “no or minimal anxiety”, 10–15 as “mild anxiety”, 16–24 as “moderate anxiety”, and >24 as “severe anxiety”. While these classifications have not been clinically validated, to the best of our knowledge, they have been previously employed by others [34, 35].
Cost-effectiveness analysis
The CEA was selected because statistically significant differences in effectiveness were observed between both study groups favouring pregabalin. Then, the CEA analysis was expressed as the ICER, i.e. the ratio between the difference in costs between pregabalin and UC and the difference in health benefit also between pregabalin and UC in refractory patients newly diagnosed with GAD. It was calculated by dividing the difference in costs between pregabalin and UC and the difference of their effectiveness: ICER = (costpregabalin − costUC)/(effectivenesspregabalin − effectivenessUC). In accordance with Spanish guidelines for economic evaluation of health technologies [36], the expected mean ICER, with a non-parametric 95 % percentile confidence interval (CI), was estimated using bootstrapping (10,000 re-samples) techniques. These re-samples allowed obtaining the probability values and drawing the cost-effectiveness plane and the ICER acceptability curve for the base-case scenario. This approach enabled us to obtain the percentage of replications that were below €30,000 per QALY gained and therefore could be considered as a cost-effective intervention [28].
Sensitivity analysis
A probabilistic sensitivity analysis was also performed using bootstrapping (10,000 re-samples each time). Univariate sensitivity analyses were carried out in a set of sensitive variables. These analyses included the following variables: healthcare costs (medical visits, hospitalisation, non-pharmacological treatment, and drugs), QALY gained and trial duration (from 6 to 12 months). Each variable was modified ±50 % from the values used in the base-case scenario, and resample techniques were applied to calculate new ICERs with a non-parametric percentile confidence interval.
Statistical analysis
Descriptive statistics were extracted for the continuous variables in the study, including the assessment of central tendency and dispersion statistics with a 95 % CI when possible. The Kolmogorov–Smirnov test was applied to check whether data demonstrated Gaussian distribution. In the study, patients were classified according to the severity of symptoms, with HAM-A scores ≤9 as “no or minimal anxiety”, 10–15 as “mild anxiety”, 16–24 as “moderate anxiety”, and >24 as “severe anxiety”. The percentage of patients without anxiety (HAM-A ≤ 9) and the percentage considered as responder (HAM-A reduction ≥ 50 % compared to baseline score) were also calculated.
For categorical variables, absolute and relative frequencies were calculated. For comparisons, Student’s t test and Chi-square test were used for continuous and categorical variables, respectively. Analysis of covariance (ANCOVA) or binary logistic regression models were carried out comparing pregabalin versus UC groups, adjusting for baseline score, co-morbidities and socio-demographic data. All statistical tests were two-tailed, and a P value inferior to 0.05 was considered as statistically significant. Data were analysed using SPSS version 17.0.
Results
In this CEA modelling, we used data extracted from refractory outpatients with GAD according to DMS-IV criteria, who were pregabalin naïve, but previously treated with at least one drug for anxiety symptoms for 6 months or more, and who had shown a suboptimal response as defined previously. Two balanced groups (Table 2) were formed according to pregabalin exposure during the 6-month period of the original study: the control group was formed with data from 451 patients (mean baseline score of the HAM-A scale: 25.7 ± 7.3 points) who received UC treatment. Treatment could include SSRI/SNRI/other anti-depressants, benzodiazepines, anti-epileptic drugs (other than pregabalin), or a combination of these drugs. The mean number of drugs used during the study was 2.2 (95 % CI 2.1; 2.3) with 85.8 % of controls receiving a benzodiazepine, 82.3 % an anti-depressant, and 11.5 % an anti-epileptic (53 % gabapentin, 42 % topiramate, and 5 % lamotrigine). The group of cases was composed of data from 451 patients (mean baseline score of the HAM-A scale: 26.1 ± 7.1 points) who were treated with flexible doses of pregabalin (≤25 mg/day, 2.6 % of patients; 25–75 mg/day, 28.1 %; 75–150 mg/day, 45.9 %; 150–300 mg/day, 19.5 %; and >300 mg/day, 3.9 %; average dose, 218 mg/day), in monotherapy or as an add-on therapy to the existing treatment at the beginning of the study, and randomly selected from the study cohort as described previously. The mean number of drugs in this group was 2.9 (2.7; 3.0) with 59 (13.1 %) receiving pregabalin in monotherapy and the rest of cases treated concomitantly with benzodiazepines in 68.7 % of patients or anti-depressive drugs in 78.5 %.
Both groups were similar, from a statistical standpoint, with regard to main patient socio-demographic characteristics (Table 2). However, clinical characteristics at baseline presented statistical differences in health scales, such as CGI scores, the scores being higher for the pregabalin group (4.2 ± 0.8 vs. 4.0 ± 0.7; P < 0.001); for the HAM-A score, the percentage of patients in the pregabalin group with severe symptoms of anxiety being higher (64.0 vs. 59.4 %; P < 0.001); and the mean utility value and health status assessed by the EQ-5D questionnaire being lower for the pregabalin group (0.4181 ± 0.3107 vs. 0.5020 ± 0.2936; P < 0.001), meaning that patients included in this group started with a more severe baseline status than the control group (Table 2). In addition, at baseline, the group of patients assigned to pregabalin had been treated with a significantly higher number of anti-depressants than the control group (75.2 vs. 57.4 %; P < 0.001).
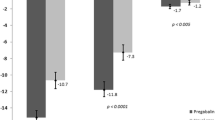
Total healthcare costs and effectiveness values are included in Tables 3 and 4. Compared with UC, pregabalin showed better and statistically significant QALY gain after 6 months of treatment: 0.1209 ± 0.1030 versus 0.0994 ± 0.0979, P = 0.003 after adjusting for sex, age, co-morbidities and baseline values. Moreover, the percentage of patients showing response (HAM-A reduction ≥ 50 %) at end-of-trial was significantly higher in the pregabalin group compared with the control group: 62.9 versus 57.4 %, odds ratio = 1.4 (1.0–1.8), P = 0.044. However, significant differences were not observed in the percentage of subjects without anxiety at the end of the study. Total healthcare costs were higher in the pregabalin group compared with UC: €1,272 ± 1,420 versus €1,070 ± 1,177, showing a tendency towards statistical significance (P = 0.069). This difference was mainly due to the medical visit costs and, as expected, the cost of drugs (Tables 3 and 4), as patients included in the pregabalin group were treated with a significantly higher number of drugs (2.9 vs. 2.2; P < 0.01) as a consequence of adding this drug to the existing therapy in most subjects in this group.
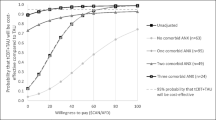
The probabilistic ICER of pregabalin over UC in total healthcare costs was €15,804 per QALY gained (95 % CI 6,661–37,186; Table 4). The cost-effectiveness plane (Fig. 2, graph a) showed that 99.9 % of the re-samples fell in the upper right quadrant (higher healthcare costs and more QALY gained). The cost-effectiveness acceptability curve constructed with those re-samples showed that 94.5 % of them fell under the willingness-to-pay threshold of €30,000 per QALY, with 95 % of them below €30,558 per QALY gained (Fig. 3). In terms of drug costs only, the probability ICER after 10,000 re-samples was €15,165 per QALY gained (95 % CI 7,947–31,754), with 99.5 % of samples in the upper right quadrant (Fig. 2, graph b). In this case, 96.6 % of the samples fell under the willingness-to-pay threshold of €30,000 per QALY gained (Fig. 3), with 95.0 % of samples below €26,034 per QALY gained.
Sensitivity analysis
The sensitivity analysis indicated the ICER to be robust when the main variables of the study were modified ±50 % of the base-case value and after obtaining 10,000 re-samples in each case (Table 5). The percentage of re-samples showing an ICER below €30,000 per QALY gained was above 90 % for most variables modified in the sensitivity analysis, except in 83 % of the samples when drug costs were multiplied by 1.5, and in 88 % of cases when study time horizon increased up to 12 months, which could still be considered cost-effective. Only when QALY gained was multiplied by 0.5 (50 % reduction of the base-case scenario), the willingness-to-pay threshold dropped to 54 %.
Discussion
This paper includes a modelling estimation of the cost-effectiveness of GAD treatment in refractory patients in order to provide insight for future clinical decisions in this population, helping both clinicians and healthcare decision makers in taking clinical decision from an efficiency perspective. The nested case–control design used in this evaluation allowed us to perform the analysis in a set of GAD patients with similar socio-demographic and clinical characteristics and in a sample size of patients large enough to obtain representative samples from the original cohort study. In this population, adding pregabalin alone, or in combination with the existing treatment of such patients, compared with UC, showed that treating subjects with that drug would cost about €152 more per patient in healthcare costs in a 6-month period. However, this incremental cost was accompanied by better results in terms of both better patient response (higher reduction of anxiety symptoms) and higher gain of quality of life as assessed by QALY gain (i.e. lower trade off of years of perfect health), resulting in an affordable incremental cost of €15,804 per QALY gained, which in our healthcare context, and others such is the NICE, is considered to be a cost-effective intervention [28–30]. When this operation was then repeated to obtain 10,000 samples to manage the level of uncertainty, the robustness of the results was confirmed in most scenarios included in the sensitivity analysis carried out; most of the new ICERs felt below the willingness-to-pay threshold of €30,000 per QALY. This indicates that treatment with pregabalin was cost-effective compared to UC therapy in refractory GAD patients in most clinical situations, and thus could be considered affordable by the NHS, except when, as expected, the QALY gain was reduced by 50 %. This possibility, however, was considered highly unlikely.
Compared with the literature on cost-effectiveness studies in anxiety disorders to date, we found eight CEAs published on panic disorder, four on GAD, one on social phobia, one on post-traumatic stress disorder, and another involving several anxiety disorders. Of the four CEA studies focusing on GAD [37–40], only two of them [39, 40] used DSM-IV as diagnostic criteria for GAD (the others used ICD10 as diagnostic criteria), and none of them presented QALY gain as a measure of effectiveness (using treatment success and no relapses). In addition, just one [39] of these previous two studies presented the third party payer’s perspective, although the sample size of each arm was small: 70 and 96 patients only, respectively. This study did not incorporate usual care, but compared diazepam versus venlafaxine [39]. Therefore, in the English literature consulted, we did not find any CEA using DSM-IV as GAD diagnostic criteria, QALY gain as a measurement of effectiveness, with the third party payer’s perspective and comparing the therapeutic alternative with usual care. Our modelling study is therefore the first analysis involving all these perspectives and using a representative sample size of 902 patients, which could be the largest one in a CEA for anxiety disorders. In terms of cost, comparing total healthcare costs as shown by our analysis with the studies cited above, our modelling seems more complete because the cost of all medical visits and hospitalisations, in addition to non-pharmacological treatments, was included. As pointed out by the author of a recently published systematic review in 2009 [41], it would be useful to agree on the measure of effectiveness used in CEA, such as the standard measures of QALY gain, or perhaps DALY avoided, which is recommended in most guidelines for the financial evaluation and assessment of health technologies [42, 43].
Assuming that any analysis of the real situation carries some degree of uncertainty, a sensitivity analysis on 10,000 samples using bootstrapping was carried out to minimise errors and increase certainty of cost estimates, QALY gained or total duration of the study to check the robustness of the analysis and conclusions. However, some limitations of our CEA approach should also be noted. One of them is the observational design of the original cohort source of data, the ADAN study, with its inherent limitations: mainly that it was not a typical randomised clinical trial. Nevertheless, although this could also be considered to be a methodological weakness of our analysis, it could also be accepted as an advantage for payers or the NHS because the study was based on real data which allows health decision makers to draw conclusions from and estimate actual costs and resources utilisation. Secondly, we used a nested case–control design to extract data for CEA modelling. While this kind of design is widely used in morbidity and mortality epidemiological studies, we are not aware of any economic evaluations using this methodology to date. However, we believe that this economic evaluation design enables clinical cases and controls to be compared, and, in fact, subjects included in the analysis were rather similar from the socio-demographic point of view. Nevertheless, subjects included in the pregabalin group presented with slightly more severe cases, which would not favour the results of pregabalin cohort. Thirdly, the patients included in the analysis were refractory to previous treatment and met specific criteria in the ADAN study protocol. Although there was no consensus in the scientific community about how to define refractoriness, the criteria used here seem to fall within the scope of those used by other authors in the literature [8, 44–46]. Moreover, the fact that this CEA modelling focuses on refractory patients only without including other types of GAD patients could be the subject of criticism. However, while this is true, most patients with GAD seen on an outpatient basis in psychiatry clinics in Spain fall in the refractory subtype; the results of this CEA would therefore be applicable to a considerable number of subjects in standard medical practice, in clinics of psychiatry. Another possible limitation was the fact that the perspective of the evaluation was that of the NHS only, and did not include indirect costs resulting from loss of productivity, which could be valuable with regard to this health condition, nor did it include the so-called out-of-pocket costs or resources paid for by the subjects themselves. The main reason for this is that, in our health context, the NHS is more concerned about the resources and costs it funds rather than about cost components which do not fall within its scope of coverage. Moreover, due to the absence of a specific question in the patient diary during the study regarding source of funding, some of the used or prescribed non-pharmacological treatments in this study could have been paid for by the patient, such as some types of massage, acupuncture sessions, yoga/tai chi sessions or naturopathy, among others; a portion of the cost could have therefore been funded by the patients.
Conclusion
In conclusion, despite the limitations of the analysis, this economic modelling suggests that including pregabalin in the treatment of refractory outpatients with GADs may be cost-effective in comparison with the usual care without such drug in daily practice in mental health centres in Spain.
References
Wittchen HU, Kessler RC, Beesdo K, Krause P, Hofler M, Hoyer J (2002) Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry 63(Suppl 8):24–34
Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H et al (2004) Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl 420:21–27
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:593–602
Caballero L, Bobes J, Vilardaga I, Rejas J (2009) Clinical prevalence and reason for visit of patients with generalized anxiety disorder seen in the psychiatry out-patient clinics in Spain. Results of the LIGANDO study. Actas Esp Psiquiatr 37:17–20
Chocron Bentata L, Vilalta Franch J, Legazpi Rodriguez I, Auquer K, Franch L (1995) Prevalence of psychopathology at a primary care center. Aten Primaria 16:586–590
Katon W, Von Korff M, Lin E, Lipscomb P, Russo J, Wagner E, Polk E (1990) Distressed high utilizers of medical care: DMS-III-R diagnoses and treatment needs. Gen Hosp Psychiatr 12:355–362
Kennedy BL, Schwab JJ (1997) Utilization of medical specialists by anxiety disorder patients. Psychosomatics. 38:109–112
Bandelow B, Zohar J, Hollander E, Kasper S, Möller HJ WFSBP Task Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and Post-Traumatic Stress Disoders, Zohar J, Hollander E, Kasper S, Möller HJ, Bandelow B, Allgulander C, Ayuso-Gutierrez J, Baldwin DS, Buenvicius R, Cassano G, Fineberg N, Gabriels L, Hindmarch I, Kaiya H, Klein DF, Lader M, Lecrubier Y, Lépine JP, Liebowitz MR, Lopez-Ibor JJ, Marazziti D, Miguel EC, Oh KS, Preter M, Rupprecht R, Sato M, Starcevic V, Stein DJ, van Ameringen M, Vega J (2008) World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders - first revision. World J Biol Psychiatry 9:248-312
Ballenger JC, Davidson JR, Lecrubier Y, Nutt DJ, Marshall RD, Nemeroff CB, Shalev AY, Yehuda R (2001) Consensus statement of generalized anxiety disorder from the international consensus group on depression and anxiety. J Clin Psychiatry 62(Suppl. 11):53–58
Yonkers K, Warshaw M, Massion A, Keller M (1996) Phenomenology and course of generalised anxiety disorder. Br J Psychiatry 168:308–313
Kessler RC, Wittchen HU (2002) Patterns and correlates of generalized anxiety disorder in community samples. J Clin Psychiatry 63(Suppl. 8):4–10
Katzman MA (2009) Current considerations in the treatment of generalized anxiety disorder. CNS Drugs 23:103–120
McLaughlin TP, Khandker RK, Kruzikas DT, Tummala R (2006) Overlap of anxiety and depression in a managed care population: prevalence and association with resource utilization. J Clin Psychiatry 67:1187–1193
Andlin-Sobocki P, Wittchen HU (2005) Cost of anxiety disorders in Europe. Eur J Neurol 12(Suppl. 1):39–44
Wittchen HU (2002) Generalized anxiety disorder: prevalence, burden, and cost to society. Depression Anxiety 16:162–171
Gee NS, Brown JP, Dissanayake VU, Offord J, Thurlow R, Woodruff GN (1996) The novel anticonvulsant drug, gabapentin (Neurontin), binds to the alpha2delta subunit of a calcium channel. J Biol Chem 271:5768–5776
Fink K, Dooley DJ, Meder WP, Suman-Chauhan N, Duffy S, Clusmann H, Göthert M (2002) Inhibition of neuronal Ca(2+) influx by gabapentin and pregabalin in the human neocortex. Neuropharmacology 42:229–236
Dooley DJ, Donovan CM, Pugsley TA (2000) Stimulus-dependent modulation of [(3)H]norepinephrine release from rat neocortical slices by gabapentin and pregabalin. J Pharmacol Exp Ther 295:1086–1093
Maneuf YP, Hughes J, McKnight AT (2001) Gabapentin inhibits the substance P-facilitated K(+)-evoked release of [(3)H]glutamate from rat caudial trigeminal nucleus slices. Pain 93:91–96
Álvarez E, Carrasco JL, Olivares JM, Perez M, López-Gómez V, Vilardaga I, Rejas J (2010) Broadening of generalized anxiety disorders definition does not affect the response to therapy: findings from the ADAN study. Eur Psychiatr 25(Suppl 1):Abstract PW01-50
The American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn. Text revision: DSM-IV-TR, paper. American Psychiatric Association, Washington, DC. ISBN 0-89042-025-4
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychiatry 32:50–55
Lobo A, Chamorro L, Luque A, Dal-Ré R, Badía X, Baró E (2002) Validación de las versiones en español de la Montgomery-Asberg Depression Scale y la Hamilton Anxiety Rating Scale para la evaluación de la depresión y de la ansiedad. Med Clin (Barc) 118:493–499
CGI (1976) In: Guy W (ed) ECDEU assessment manual for psycopharmacology revised. US Department of Health Education, and Welfare, NIH, Psycopharmacology Research Branch, Rockville, pp 218–222
EuroQoL Group (1990) EuroQoL—a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Badía X, Roset M, Montserrat S, Herdman M, Segura A (1999) The Spanish version of EuroQoL: a description and its applications. European Quality of Life scale. Med Clin (Barc) 112(Suppl 1):79–85
Akehurst R (2002) In Towse A, Pritchard C, Devlin N (eds) Cost effectiveness thresholds: economic and ethical issues. London Kings Fund and Office of Health Economics, p 38
Sacristán JA, Oliva J, Del Llano J, Prieto L, Pinto JL (2002) ¿Qué es una tecnología sanitaria eficiente en España? Gac Sanit 4:334–343
Rawlins MD, Culyer AJ (2004) National Institute for Clinical Excellence and its value judgments. BMJ 329:224–227
Culyer AJ (2002) Introduction. In: Towse A, Pritchard C, Devlin N (eds) Cost effectiveness thresholds: economic and ethical issues. London Kings Fund and Office of Health Economics pp 9–15
Catálogo del Consejo General de Colegios Farmacéuticos de España (2008)
Oblikue (2008) eSALUD. Base de datos de costes sanitarios. In: Social, S.C.d.E.e.E.d.l.S.y.P. (ed) SOIKOS, Barcelona
Brooks R (1996) EuroQoL: the current state of play. Health Policy 37:53–72
Revicki D, Brandenburg M, Matza LS, Morlock R, Hornbrook MC, Feeny D, Clarke G (2006) Relationship between anxiety severity and health utility index scores in generalized anxiety disorder. Collegium of Internationale Neuro-Psycharmacologicum (CINP), Chicago, 9–13 July
Morlock R, Shah H, Feltner D, Brandenburg N, Matza LS, Revicki D (2006) Estimation of health-state utilities for patients with generalized anxiety disorder. Collegium of Internationale Neuro-Psycharmacologicum (CINP), Chicago, 9–13 July
Bastida JL, Oliva J, Antoñanzas F, García-Altés A, Gisbert R, Mar J, Puig-Junoy J (2010) A proposed guideline for economic evaluation of health technologies. Gac Sanit 24:154–170
Heuzenröeder L, Donnelly M, Haby MM, Mihalopoulos C, Rossell R, Carter R, Andrews G, Vos T (2004) Cost-effectiveness of psychological and pharmacological interventions for generalized anxiety disorder and panic disorder. Psychiatry 38:602–612
Issakidis C, Sanderson K, Corry J, Andrews G, Lapsley H (2004) Modelling the population cost-effectiveness of current and evidence-based optimal treatment for anxiety disorders. Psychol Med 34:19–35
Guest JF, Russ J, Lenox-Smith A (2005) Cost-effectiveness of venlafaxine XL compared with diazepam in the treatment of generalized anxiety disorder in the United Kingdom. Eur J Health Econ 6:136–145
Jörgensen TR, Stein DJ, Despiegel N, Drost PB, Hemels ME, Baldwin DS (2006) Cost-effectiveness analysis of escitalopram compared with paroxetine in treatment of generalized anxiety disorder in the United Kingdom. Ann Pharmacother 40:1752–1758
Konnopka A, Leichsenring F, Leibing E, König HH (2009) Cost-of-illness studies and cost-effectiveness analyses in anxiety disorders: a systematic review. J Affect Disord 114:14–31
Weinstein MC, O’Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, ISPOR Task Force on Good Research Practices—Modeling Studies (2003) Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on good research practices—modeling studies. Value Health 6:9–17
National Institute for Clinical Excellence (2004) Guide to the methods of technology appraisal. NICE, Londres
Pollack MH, Otto MW, Roy-Byrne PP, Coplan JD, Rothbaum BO, Simon NM, Gorman JM (2008) Novel treatment approaches for refractory anxiety disorders. Depression Anxiety 25:467–476
Simon NM, Connor KM, LeBeau RT, Hoge EA, Worthington JJ III, Zhang W, Davidson JR, Pollack MH (2008) Quetiapine augmentation of paroxetine CR for the treatment of refractory generalized anxiety disorder: preliminary findings. Psychopharmacology 197:675–681
Pollack MH, Simon NM, Zalta AK, Worthington JJ, Hoge EA, Mick E, Kinrys G, Oppenheimer J (2006) Olanzapine Augmentation of fluoxetine for refractory generalized anxiety disorder: a placebo controlled study. Biol Psychiatry 59:211–215
Acknowledgments
Data collection and analysis were funded by Pfizer España. All authors had complete access to the data, participated in the analysis and/or interpretation of results, and drafted the manuscript.
Conflict of interest
Javier Rejas is full employed by Pfizer España, the body funding the study. M. Belén Ferro was employed by Pfizer España at the time of analysis, although currently is not working for Pfizer, and Marina De Salas-Cansado is an employee of Trial Form Support (TFS), who was paid contractor to Pfizer Inc in the development of the economic modelling. Editorial support was not hired. All other authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Belén Ferro does not currently work for Pfizer.
Rights and permissions
About this article
Cite this article
De Salas-Cansado, M., Álvarez, E., Olivares, J.M. et al. Modelling the cost-effectiveness of pregabalin versus usual care in daily practice in the treatment of refractory generalised anxiety disorder in Spain. Soc Psychiatry Psychiatr Epidemiol 48, 985–996 (2013). https://doi.org/10.1007/s00127-012-0606-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-012-0606-6