Abstract
Attention-deficit hyperactivity disorder (ADHD) is a chronic neurodevelopmental disorder characterized by persistent symptoms of inattention, hyperactivity and/or impulsivity. The proportion of patients diagnosed with ADHD receiving pharmacological treatments has increased enormously in recent years. Despite the well established efficacy and the good safety and tolerability profile, there is concern about the potential for rare but serious cardiovascular adverse events, as well as sudden cardiac death, with pharmacotherapies used for treating ADHD in children, adolescents and adults. The present paper aims to comprehensively and critically review the published evidence on the controversial association between medications approved for treating patients with ADHD and the risk of serious cardiovascular problems, specifically the risk of corrected QT interval (QTc) prolongation, and the risk of sudden cardiac death. A comprehensive search of relevant databases (PubMed, EMBASE and PsychINFO) was conducted to identify studies published in peer-reviewed journals until 21 July 2012. Clinical reports, as well as retrospective or prospective population-based studies with children, adolescents or adults as participants, of pharmacotherapies for ADHD reporting cardiovascular adverse events were included. Stimulant medications for ADHD, including methylphenidate and amphetamine derivatives, are generally safe and well tolerated. Small but statistically significant increases in blood pressure (BP) and heart rate (HR) are among the adverse events of stimulant treatment in all age groups. Similarly, the non-stimulant medication atomoxetine has also been associated with increased HR and BP, although as is the case with stimulants, these are generally minor, time limited and of minor clinical significance in children, adolescents or adults. Growing evidence suggests that these medications do not cause sudden and unexpected cardiac death or serious cardiovascular problems including statistically or clinically significant increases in QTc, at therapeutic doses in ADHD patients across the lifespan. Small decreases in mean systolic BP, diastolic BP and HR have been observed in studies with guanfacine-extended release (-XR) or clonidine-XR, two α2-adrenergic receptor agonists, administered alone or in combination with psychostimulants to children and adolescents with ADHD. There are also no statistically or clinically significant increases in QTc associated with clonidine or guanfacine. There are no reports of torsades de pointes clearly and directly related to medications used for treating ADHD in patients of all age groups. The risk for serious cardiovascular adverse events, including statistically or clinically significant increases in QTc, and sudden cardiac death associated with stimulants, atomoxetine or α2-adrenergic agonists prescribed for ADHD is extremely low and the benefits of treating individual patients with ADHD, after an adequate assessment, outweigh the risks. However, great caution is advised when considering stimulant and non-stimulant medications for patients of any age with a diagnosis of ADHD and a personal or family history or other known risk factors for cardiovascular disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Attention-deficit hyperactivity disorder (ADHD) is a complex and heterogeneous neurodevelopmental disorder characterized by persistent symptoms of inattention, hyperactivity and/or impulsivity [1, 2]. ADHD is the most prevalent psychiatric disorder of childhood, but symptoms persist into adulthood in approximately 60 % of patients [3]. It is associated with significant impairment in psychological, occupational and social functioning in the affected individual across the lifespan [4, 5].
Despite the well established efficacy, overall good safety and tolerability profile, and the long history of use there is concern about the potential for rare but serious cardiovascular adverse events, including sudden cardiac death, of pharmacotherapies for ADHD. Drug-induced sudden death is most commonly caused by torsades de pointes (TdP), a potentially life-threatening, polymorphic, ventricular tachycardia often associated with a QT interval prolongation. The QT interval is an ECG measure that provides an estimate of the time from the earliest ventricular depolarization (the beginning of the QRS complex) to the completion of ventricular repolarization (T wave), thus reflecting the duration of the cardiac action potential [6]. Because the QT interval shortens with increasing heart rates, it is usually corrected for heart rate (HR) [corrected QT interval (QTc)]. Drug-induced QT/QTc prolongation and TdP are relatively rare adverse effects of a wide range of pharmacological agents commonly used in clinical practice [7].
The present paper aims to comprehensively and critically review the published evidence on the controversial association between medications used for treating patients with ADHD and the risk of serious cardiovascular problems, with a particular focus on the risk of QT/QTc prolongation, and the risk of sudden cardiac death in children, adolescents and adults. This is discussed in the context of other factors that may increase the risk of these adverse events in vulnerable individuals. The article may be of particular relevance for researchers and clinicians, both psychiatrists and non-psychiatrists involved in the care of children, adolescents or adult patients with this chronic disorder. The review is limited to licensed medications and therefore those most commonly used for the treatment of children, adolescents and adults diagnosed with ADHD. These include atomoxetine, α2-adrenergic agonists and a number of different immediate-release (IR) and long-acting methylphenidate and amphetamine compounds.
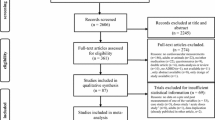
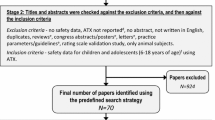
A comprehensive search of relevant databases (PubMed, EMBASE and PsychINFO) was conducted to identify studies published in English in peer-reviewed journals until 21 July 2012, using the following MESH terms and keywords: ‘ADHD’, ‘amphetamine’, ‘atomoxetine’, ‘clonidine’, ‘guanfacine’, ‘lisdexamfetamine’, ‘methylphenidate’, ‘arrhythmia’, ‘cardiac’, ‘cardiovascular’, ‘QT’, ‘sudden death’ and ‘torsade de pointes’. In addition, reference lists were scrutinized to identify and retrieve further relevant reports and studies from additional sources and scientific databases. The literature search included clinical studies/reports, as well as retrospective or prospective population-based studies with children, adolescents or adults as participants, of pharmacotherapies for ADHD reporting cardiovascular adverse events. There were no restrictions on the identification or inclusion of studies in terms of date of publication, publication status and design type. However, abstracts of presentations to specialist meetings and conferences were not included. Titles and abstracts were screened for inclusion/exclusion, and full text versions were retrieved.
A total of 584 records were identified through database searches (233 from EMBASE, 226 from PubMed and 125 from PsychInfo). Titles and abstracts were screened and a total of 447 documents were excluded for not meeting the criteria mentioned above. The remaining 137 documents were considered eligible (51 from EMBASE, 54 from PubMed and 32 from PsychInfo); however, a further 56 duplicate reports were excluded. Therefore, a total of 81 documents identified through database searches were included in the review.
2 Controlled and Open-Label Extension Studies of Medications for Attention-Deficit Hyperactivity Disorder (ADHD) and Serious Cardiovascular Events
2.1 CNS Stimulants
Since the first reports published in 1937 showing beneficial effects of Benzedrine® (Smith, Kline and French), the racemic mixture of levo- and dextro-amphetamine, for hyperactive, inattentive children [8], stimulants have been widely used and remain as first-line pharmacological treatment for ADHD, due to their evidence-based efficacy [4, 8–12]. Stimulants used in the treatment of ADHD include different formulations of IR and long-acting methylphenidate and amphetamines. Methylphenidate is postulated to exert the therapeutic actions in ADHD by blocking noradrenaline (norepinephrine) and dopamine reuptake, while amphetamines also facilitate extracellular release of dopamine and noradrenaline, leading to an increase of noradrenaline and dopamine levels in the prefrontal cortex [13, 14].
Stimulant medications are generally safe and well tolerated in children, adolescents and adults with a diagnosis of ADHD. Appetite suppression and insomnia are the most common adverse effects, but usually mild and manageable without stopping the medication [15, 16]. Small, but statistically significant increases in blood pressure (BP) and HR are among the cardiovascular adverse events of stimulant treatment, in children, adolescents and adults [17–21]. Indeed, in a meta-analysis of the effects of various CNS stimulants in adults with ADHD on several cardiovascular parameters based on data from ten placebo-controlled trials conducted in a pooled sample of 2,665 adults, the use of CNS stimulants, but not of placebo, was associated with a statistically significant increase in mean [standard error] HR (5.0 [0.5] vs. placebo: −0.5 [0.7]), systolic BP (1.2 [0.4] vs. placebo: −0.9 [0.4]) and diastolic BP (1.2 [0.3] vs. placebo: 0.2 [0.4]) [18]. These changes in BP and HR are thought to be mediated by the sympathomimetic, as well as the central and peripheral catecholaminergic effects, of stimulant medications [22, 23]. Several very rare but potentially serious cardiovascular adverse events have been associated with stimulant medications for ADHD (see Sects. 2.1.1 and 2.1.2) [15, 16, 24, 25].
To better characterize the cardiovascular adverse effects, and specifically to evaluate the risks of a prolonged QT/QTc associated with stimulants in children, adolescents and adults with ADHD, methylphenidate- and amphetamine-based formulations were reviewed separately. However, due to the recent publication of a series of large population-based studies assessing the association of medications used for ADHD with the risk of cardiovascular adverse events, this emerging evidence has been reviewed and discussed in a separate section.
2.1.1 Methylphenidate-Based Formulations
Methylphenidate, particularly in its IR formulation, has been used for over 50 years for the treatment of individuals with ADHD, since it first became available in the USA in 1955. Methylphenidate (d,l-threo-methylphenidate) is a racemic mixture of d-methylphenidate and l-methylphenidate. Its active enantiomer, dexmethylphenidate or d-threo-methylphenidate (Focalin®; Novartis Pharmaceuticals), was approved by the US FDA in November 2001 for the treatment of ADHD [26]. Methylphenidate formulations can be IR (Ritalin®; Novartis Pharmaceuticals), with a duration of effect of 3–5 h, and extended release (XR), sustained release (SR), modified release (MR) and controlled delivery (CD) compounds, with a duration of action of up to 8 h (e.g. Equasym XL®; Shire Pharmaceuticals, Medikinet XL®; Flynn Pharma Ltd or Metadate CD®; UCB Pharma Inc.), as well as the Osmotic-controlled Release Oral delivery System (OROS) [Concerta®; Janssen Pharmaceuticals, Inc.], and the XR Spheroidal Oral Drug Absorption System (SODAS) [Focalin XL®; Novartis Pharmaceuticals], with a duration of effect of up to 12 h that allows for once-a-day dosing [2, 12]. The latter is also possible with the methylphenidate transdermal system (Daytrana®; Shire Pharmaceuticals). Although there are significant differences in the absorption rate and other pharmacokinetic parameters between dexmethylphenidate, the methylphenidate transdermal system and the rest of the methylphenidate formulations, they all show similar therapeutic properties and adverse effect profiles [27].
Minor but statistically significant changes in systolic BP (3.3 mmHg), diastolic BP (1.5 mmHg) and HR (3.9 bpm) were observed over a 1-year period in a sample of 432 children with ADHD aged 6–13 years participating in an open-label extension trial of methylphenidate-OROS 18–54 mg [28].
Among adult patients with ADHD, small, but statistically significant increases in systolic BP (3.5 ± 11.8 mmHg), diastolic BP (4.0 ± 8.5 mmHg) and HR (4.5 ± 10.5 bpm) were reported in a randomized, 6-week, placebo-controlled, parallel-design study of methylphenidate-OROS in 141 subjects with ADHD [29]. Similar findings were reported in another 24-week, double-blind, placebo-controlled, multicentre study of methylphenidate-XR (up to 60 mg/day) in 359 adult individuals with ADHD [30]. A statistically significant increase of HR (5 bpm) at week 4 was reported in the methylphenidate-XR group, while an increase in systolic BP was not significant (3 bpm at endpoint) and there was no change in diastolic BP. In a further 7-week, double-blind, placebo-controlled trial of methylphenidate-OROS (up to 108 mg/day) with 226 adult patients with ADHD, no serious treatment-emergent adverse events and no deaths were reported, but in patients receiving methylphenidate-OROS minor increases in HR (+3.6 bpm) and diastolic BP (+1.1 mmHg) and minor decreases in systolic BP (−1.2 mmHg) were documented [31]. In addition, significantly more patients taking methylphenidate-OROS compared with placebo had a HR >100 bpm (7 vs. 2 %) and a diastolic BP >90 mmHg (10 vs. 3 %), and a higher, but non-significant, proportion of patients in the methylphenidate-OROS had a systolic BP >140 mmHg (8 vs. 6 %).
Long-term safety of methylphenidate-OROS in adults (up to 108 mg/day) has been explored in a multicentre, open-label, dose-titration, flexible-dose study in 550 subjects that completed their 6 or 12 months of pharmacological treatment, reporting modest increases from baseline to endpoint in mean systolic (2.6 mmHg) and diastolic (1.9 mmHg) BP and HR (4.1 bpm) [32].
Cardiac arrhythmias have only rarely been reported with methylphenidate treatment. In a study of borderline personality disorder, two of eight patients developed unifocal premature ventricular contractions following intravenous administration of methylphenidate [33]. Neither patient had prior arrhythmias, but these developed within 5–6 min of the onset of methylphenidate infusion. Similarly, the development of ventricular tachycardia (180 bpm) was reported shortly after administration of oral methylphenidate (5 mg twice daily) in a 60-year-old male patient, with no known prior arrhythmia, who was taking the antihypertensive guanethidine [34]. Recently, the development of significant cardiovascular complications has been described in three children taking methylphenidate-OROS for ADHD [35]. Of these three cases, from a clinic of 720 patients, one subject experienced supraventricular tachycardia, whilst the remaining two presented with hypertension and self-limited sinus tachycardia. In contrast, there are no strong data to suggest that methylphenidate increases the QT/QTc. In a small study, concomitant administration of methylphenidate and antipsychotic medication in very young children was not associated with significant alterations of the QT interval [36].
Overdose of methylphenidate may hypothetically result in over-stimulation of the CNS and excessive sympathomimetic effects, which may manifest as tachycardia, palpitations, cardiac arrhythmias and/or hypertension. In a study specifically conducted to assess the effects of methylphenidate overdose on the QT interval, 23 adults who had taken up to 1,500 mg of methylphenidate were identified retrospectively and compared with a control group of subjects, matched for sex and HR, with acetaminophen overdose, a known non-cardiotoxic substance [37]. No arrhythmias were recorded in the individual ECGs, which revealed no significant differences between both groups in mean QT or QRS intervals, therefore suggesting that methylphenidate overdose is unlikely to have substantial effects on the QT interval or to provoke potentially life-threatening arrhythmias. Similarly, in isolated and independent case reports of two adolescent girls taking an overdose of long-acting methylphenidate, no significant cardiovascular adverse events other than slight hypertension, and sinus tachycardia were identified [38, 39]. In addition, in a study that evaluated short- and long-term cardiovascular safety of relatively high doses of methylphenidate-OROS (up to 1.5 mg/kg) in a sample of 114 adolescents with ADHD, 57 of whom completed 6 months of treatment, there were no statistically or clinically significant changes in ECG variables, as well as no serious adverse cardiovascular effects during the study period [40]. Nonetheless, there are reports of ST elevation and myocardial infarction (MI) in isolated cases of methylphenidate overdose [41].
2.1.2 Amphetamine-Based Formulations
Amphetamines include a variety of compounds. Amphetamine itself, first synthesized in 1887, has two stereoisomers, levo- and dextro-amphetamine, the latter one being FDA approved for the treatment of ADHD in IR and SR formulations. Other compounds in this group currently licensed in some countries including the USA, include IR and XR formulations of d-amphetamine sulphate (Dextrostat®; Shire Pharmaceuticals, or Dexedrine® and Dexedrine spansules®; Amedra Pharmaceuticals), and mixed d- and l-amphetamine salts (MAS-XR) [Adderall® and Adderall XR®; Shire Pharmaceuticals], d-methamphetamine salts (Desoxyn®; Ovation Pharmaceuticals) and the long-acting lisdexamfetamine dimesylate (Vyvanse®; Shire Pharmaceuticals), a prodrug of dextroamphetamine.
Despite the growing evidence suggesting that amphetamines do not cause statistically or clinically significant increases in QTc or in sudden and unexpected cardiac death at therapeutic doses [42], amphetamine-class drugs have been involved for decades with serious cardiovascular problems including sudden cardiac death [43]. However, most cases [43–45], but not all [46], refer to problem drug users most commonly abusing amphetamine compounds in combination with other substances, such as alcohol and/or nicotine.
Short- and long-term term cardiovascular effects of MAS-XR have been explored in several randomized placebo-controlled trials. In the first of these studies, that included a 6-month, open-label extension study, cardiovascular effects of MAS-XR were assessed in 327 otherwise healthy adolescents with ADHD [47]. There were no statistically significant differences in mean systolic and diastolic BP and in the QTc at 4 weeks between MAS-XR and placebo groups. No subject had a systolic BP >150 mmHg or a diastolic BP >100 mmHg during the short-term double-blind study, whilst mild but significant HR increases of 5.0 and 8.5 bpm were documented at endpoint with MAS-XR 20 and 50 mg/day, respectively (p ≤ 0.002). During the 6-month follow-up extension study no serious cardiovascular adverse events emerged, with minor but significant increases in systolic BP (1.7 mmHg; p = 0.0252) and HR (4.4 bpm; p < 0.0001) and no changes in diastolic BP (0.6 mmHg). A statistically significant, but negligible decrease in QTc (−4.6 ± 19.9 ms) was also reported; no subject had a QTc >500 ms during long-term treatment. No statistically significant differences in changes in BP, HR and QTc were noticed between children receiving MAS-XR or placebo in another 4-week, double-blind, randomized, controlled study of once-daily MAS-XR with 580 otherwise healthy children [17]. At the end of the 2-year, open-label extension study, which included 568 of the original sample, treatment with MAS-XR was associated with increases in BP (systolic: 3.5 mmHg; diastolic: 2.6 mmHg) and HR (3.4 bpm) that were not clinically significant. In addition, 2 % (11/568) of the sample had a diastolic BP >90 mmHg, and 9 % (50/568) had a systolic BP >130 mmHg at some point during follow-up.
Similarly, in a large, prospective, open-label, non-comparative, community-based study with 2968 children aged 6–12 years followed-up for up to 15 months, once-daily MAS-XR (up to 40 mg/day) was not associated with clinically significant changes in systolic or diastolic BP, or HR [48]. In this study, nine patients (0.3 %) had moderate or serious cardiovascular adverse events, five of which were probably related to MAS-XR, and seven patients (0.2 %) discontinued MAS-XR due to cardiovascular adverse events. In addition, approximately 2.5 % of children had two consecutive systolic or diastolic BP values >95th percentile for age, sex and height, and 3.6 % of the sample demonstrated a HR ≥110 bpm.
The long-term cardiovascular effects of MAS-XR (up to 60 mg/day) have also been specifically assessed in adults with ADHD. In a 24-month open-label study with 223 adult patients, small but statistically significant, albeit not clinically significant, increases in diastolic BP (1.3 ± 9.2 mmHg; p = 0.042), systolic BP (2.3 ± 12.5 mmHg; p = 0.006) and HR (2.1 ± 13.4 bpm; p = 0.019) were reported at endpoint [49]. Additionally, a minor, but significant increase in QTc (7.2 ms; p < 0.001) was observed at 24 months, although no subject had a QTc >480 ms.
2.1.2.1 Lisdexamfetamine Dimesylate
Lisdexamfetamine is a prodrug of dextroamphetamine approved for the treatment of children and adults with ADHD. It is a therapeutically inactive molecule covalently bound to the naturally occurring, essential amino acid lysine, but after oral ingestion it undergoes enzymatic hydrolysis and is activated during first-pass metabolism to dextroamphetamine, which is responsible for its therapeutic actions [50, 51]. This amphetamine-based psychostimulant has a unique pharmacokinetic profile that allows for once-daily dosing and may provide additional safety by reducing abuse potential [50, 52]. The most common adverse events of lisdexamfetamine include appetite suppression, insomnia, upper abdominal pain, dry mouth and headache [52].
Small mean increases in HR (2–3 bpm with lisdexamfetamine vs. 1 bpm with placebo) and negligible changes in BP were reported in a 4-week, placebo-controlled trial of 314 adolescents [53]. Although no overall clinically meaningful trends in ECG changes were noted with lisdexamfetamine, two patients, both taking 70 mg/day, discontinued lisdexamfetamine after 1 week due to increased QTc.
The short-term cardiovascular safety of lisdexamfetamine has been specifically assessed in a 4-week, randomized, controlled, clinical trial in 420 medically healthy adults with ADHD that showed that lisdexamfetamine was associated with limited and modest increases in HR or BP, and no meaningful effects on ECG parameters such as QRS interval or QTc [54]. Compared with placebo, there were no statistically significant differences in systolic or diastolic BP mean changes from baseline to endpoint for each lisdexamfetamine dose group, whilst changes in HR from baseline to endpoint were 0.0, 2.8, 4.2 and 5.2 bpm in the placebo group and lisdexamfetamine 30, 50 and 70 mg/day groups, respectively (p < 0.05, all lisdexamfetamine groups vs. placebo). In post-hoc outlier analyses, 21 subjects in the lisdexamfetamine groups (none in the placebo group) met outlier criteria for HR (HR ≥100 bpm, at clinic visits) at least once during the study (p < 0.05 for lisdexamfetamine 50 mg vs. placebo only). In addition, two subjects receiving placebo, five in the 30 mg/day lisdexamfetamine group, and one in the 70 mg/day group had QTc intervals of 451–480 ms during the study, but there were no QTc interval readings of >480 ms across all study visits and none of the subjects had changes in QTc from baseline of ≥60 ms. Cardiopulmonary effects of lisdexamfetamine were further explored in a 6-month open-label study with 15 adults meeting DSM-IV criteria of ADHD that did not detect any significant changes in cardiac structure and function [55]. Overall, these data highlight the limited cardiovascular adverse events associated with lisdexamfetamine in otherwise healthy adult individuals with ADHD.
2.2 Atomoxetine
Atomoxetine (Strattera®; Eli Lilly and Company) is a selective noradrenaline reuptake inhibitor, originally developed as an antidepressant. Atomoxetine exhibits a high affinity for noradrenaline transporters, leading to the selective inhibition of presynaptic noradrenaline reuptake and an increase of noradrenaline levels in areas of known high distribution of noradrenergic neurons, such as the prefrontal cortex [56, 57]. Following the results of several randomized, placebo-controlled trials showing its efficacy in treating children, adolescents and adults with ADHD [58–60], atomoxetine was the first non-stimulant drug approved for the treatment of ADHD.
Atomoxetine is generally well tolerated in patients with ADHD. The most frequent adverse events of atomoxetine tend to appear early in the course of treatment and subsequently subside. These include dry mouth, nausea, constipation, decreased appetite, dizziness, sweating, dysuria, sexual problems and insomnia [61–64]. Atomoxetine carries a risk of drug-drug interactions due to its cytochrome P450 (CYP) 2D6 metabolism, but it remains to be established how this impacts the overall efficacy, safety and tolerability of the drug. Whilst some studies have reported that atomoxetine (in doses up to 1.8 mg/kg/day) appears to have comparable efficacy and safety in CYP2D6 extensive and poor metabolizers [65], other studies have suggested greater efficacy, greater increases in cardiovascular tone and some differences in tolerability in poor metabolizers compared with extensive metabolizers [66]. Indeed, a pooled analysis of poor and extensive metabolizers from two open-label studies of atomoxetine in children and adolescents with ADHD revealed marginally better efficacy scores and a 4.0 bpm greater increase in mean HR, but otherwise comparable safety profiles, including no differences between groups in changes from baseline in QTc [65]. In contrast, another report found significantly greater reductions in mean symptom severity scores and significantly greater increases in HR and diastolic BP (p < 0.001) at endpoint in poor metabolizers compared with extensive metabolizers (p < 0.05) [66]. Moreover, in a recent placebo-controlled study specifically evaluating the effects of atomoxetine (20 and 60 mg twice daily) on the QT interval in healthy CYP2D6 poor metabolizers [67], although atomoxetine was not associated with a clinically significant change in QTc on day 7 compared with baseline (2.2 and 4.2 ms increase for the 20 and 60 mg twice-daily doses, respectively), there was a statistically significant increase in QTc with increasing atomoxetine plasma concentrations.
Like other non-stimulant drugs with noradrenergic properties [68, 69], atomoxetine may increase HR and BP. Changes in these cardiovascular parameters, albeit statistically significant, are generally small, more likely to occur early in treatment, stabilize over time and gradually decrease on cessation of atomoxetine treatment [42, 59, 61, 62, 70].
In a meta-analysis of six randomized, double-blind, placebo-controlled clinical trials (of 6–9 weeks duration) of atomoxetine in paediatric populations with ADHD, comprising a pooled sample of 280 younger children (aged 6–7 years) and 256 older children (aged 8–12 years), respectively, atomoxetine was associated with a statistically significant increase in mean [SD] HR for both younger (8.7 [12.7] bpm vs. placebo: 1.0 [13.7] bpm; p = 0.001) and older (6.8 [11.7] bpm vs. placebo: 0.6 [11.3] bpm; p < 0.001) children [61]. Similarly, a statistically significant increase in systolic BP (2.1 [9.8] mmHg vs. placebo: 0.3 [8.1] mmHg; p = 0.034) and diastolic BP (2.9 [8.2] mmHg vs. placebo: 0.6 [8.0] mmHg; p = 0.002) was observed for older, but not for younger children. There were no significant differences between the age groups or significant treatment-by-age-group interaction for mean QTc (younger group: atomoxetine, −1.0 [21.1] ms; placebo, 0.7 [16.3] ms; older children: atomoxetine, −0.9 [18.1] ms; placebo, −1.1 [17.5] ms).
With regard to adult patients, atomoxetine was associated with modest increases in BP and HR in two identical randomized, double-blind, placebo-controlled studies conducted concurrently at 17 and 14 outpatient sites in the USA, with 280 (study I) and 256 (study II) adult individuals diagnosed with ADHD, respectively [59]. No serious safety concerns were observed in either study. Atomoxetine was associated with modest increases from baseline in diastolic BP (2.3 [8.1] and 1.2 [9.0] mmHg for atomoxetine vs. 0.5 [7.8] and 0.6 [7.7] mmHg for placebo, in study I and study II, respectively), systolic BP (2.3 [11.1] and 3.5 [10.6] mmHg for atomoxetine vs. −0.8 [9.8] and 0.9 [11.1] mmHg for placebo, in study I and study II, respectively), as well as HR (mean [SD] change in bpm: study I: atomoxetine 6.7 [11.6] vs. placebo −0.5 [9.3] bpm, p < 0.001; study II: atomoxetine = 3.8 [10.2] vs. placebo −0.1[9.6] bpm, p = 0.002).
The potential risk for QT/QTc prolongation and the development of serious cardiac arrhythmias, such as TdP, associated with atomoxetine is controversial. Following post-marketing spontaneous reports of a QT/QTc prolongation in patients taking atomoxetine, the atomoxetine prescribing information was modified to include this reaction, although due to the voluntary nature of the report, the number and characteristics of affected individuals remain uncertain, and a causal relationship to drug exposure cannot be established [71]. However, there is no consistent evidence of a prolonged QT/QTc or other serious cardiovascular problems, as well as no reports of sudden death associated with atomoxetine, at therapeutic doses, as evaluated in large clinical trials [61–63, 70, 72, 73], or in population-based studies [74]. Nonetheless, in a large post-marketing surveillance study with 2544 patients (median age 12 years), conducted to quantify and examine reports of cardiac events during treatment with atomoxetine in the UK, there were 14 patients (0.6 %) with chest pain, 7 patients (0.3 %) with arrhythmia, 22 patients (0.9 %) with tachycardia and 4 patients (0.2 %) with QT prolongation during treatment, whilst one patient (aged 7 years) had a cardiac arrest [75]. Finally, no clinically significant alterations in QT dispersion, systolic and diastolic BP, HR, QTc and left ventricular systolic functions were documented during a prospective 5-week treatment study conducted to assess the changes in cardiovascular functions and QT interval dispersion on the surface ECG of children aged 8–14 years with ADHD without structural cardiac disease [76].
Several case series with 17 [77], 40 [78] and 43 [79] patients of all age groups from poison centre encounters following accidental or intentional atomoxetine overdoses coincided in concluding that no clinically significant cardiovascular effects requiring direct intervention were detected. Furthermore, in these reports, atomoxetine overdoses were not associated with significant arrhythmias beyond transient tachycardia. In contrast, two independent case reports showed a marked QTc prolongation following an acute atomoxetine overdose [80, 81]. However, in both cases, atomoxetine was combined with other complex pharmacotherapies with either inhibitory effects on human Ether-à-Go-Go-Related Gene (hERG) channels or on CYP2D6 activity. Similarly, an isolated case of a massive atomoxetine overdose resulted in CNS and cardiac toxicity as evidenced by tonic-clonic seizures and a QT prolongation of 93 ms without any additional complications and otherwise full recovery within 24 h of hospitalization [82]. These apparently conflicting findings appear to be supported by an experimental study that demonstrated a dose-dependent blockade of the hERG by atomoxetine, therefore providing theoretical cellular explanation of proarrhythmic potential of this ADHD medication [83]. Furthermore, although the risk of atomoxetine-induced QT prolongation may be negligible at therapeutic doses, these data may explain the isolated cases of QT prolongation with atomoxetine overdose. The hERG encodes the α-subunit underlying the delayed rectifier potassium current (I Kr ), which is one of the most important components of cardiac repolarization [84, 85]. Inhibition of the I Kr underlies the cardiac adverse effects of practically all pharmacological agents and may result in drug-induced QT/QTc prolongation and facilitate the development of TdP.
2.3 α2-Adrenergic Agonists
In addition to the primary indication as antihypertensive agents, α2-adrenergic receptor agonists have been investigated and used in the treatment of a variety of childhood and adult psychiatric disorders, including migraine, Tourette’s syndrome, nicotine dependence, opiate withdrawal symptoms and ADHD [86–89]. Although the precise mechanism of action of clonidine and guanfacine in the treatment of ADHD is not fully understood, these α2-agonists are thought to act directly by mimicking noradrenaline effects at α2A-adrenoceptors in the prefrontal cortex, therefore improving prefrontal cortical cognitive functions at the cellular and behavioural levels [90, 91]. Common adverse events of α2-adrenergic agonists, generally transient, include somnolence, dizziness, drowsiness, fatigue and headaches [92]. These drugs are associated with significant cardiovascular effects, such as hypotension, including the risk of orthostatic hypotension, and bradycardia [87]. Guanfacine causes less sedation and is not as potent in decreasing BP than clonidine, probably related to the differences in receptor affinities between both drugs [93]. Whilst guanfacine reportedly binds more preferentially to postsynaptic α2A-adrenergic receptors, clonidine shows high affinity for all three subtypes of α2-receptors (A, B and C), as well as for imidazoline receptors [94]. Following long-term treatment, tolerance to the hypotensive effects develops, and abrupt withdrawal rebound hypertension may occur [19, 95].
2.3.1 Clonidine
Clonidine, as monotherapy or adjunctive therapy, has been used off-label and is reported to be efficacious in treating ADHD symptoms in children and adolescents with or without co-morbidities [92]. To overcome the fluctuating pharmacokinetics of oral clonidine-IR [96], an XR formulation of clonidine (clonidine-XR) [Kapvay®; Shionogi Pharma Inc.] was developed and recently approved by the FDA for the treatment of ADHD in children and adolescents, as monotherapy or as adjunctive therapy to stimulant medications. Clonidine-XR, used alone or in combination with methylphenidate, appears safe and well tolerated in children and adolescents with ADHD as reported in randomized, double-blind, placebo-controlled studies [97, 98]. Furthermore, cardiovascular outcomes appear to be unaffected by clonidine and methylphenidate interactions [99].
ECG changes in QT, QRS and PR intervals, described as lacking clinical significance, were reported in an 8-week, placebo-controlled, fixed-dose trial that evaluated the efficacy and safety of two doses of clonidine-XR (0.2 or 0.4 mg/day) in patients aged 6–17 years with ADHD [97]. Indeed, whilst 14 % of patients in the placebo and clonidine-XR 0.4 mg/day groups and 11 % in the clonidine-XR 0.2 mg/day group had a prolonged QTc during therapy, no patients had a QTc reading ≥500 ms at any time during the study, and no patients in the placebo group, two patients in the clonidine-XR 0.2 mg/day group and one patient in the clonidine-XR 0.4 mg/day group presented with an increase from baseline of QTc >60 ms. The incidence of sinus bradycardia increased from baseline in 5–6 % of patients in the placebo and clonidine-XR 0.2 mg/day groups and in 21 % of patients in the clonidine-XR 0.4 mg/day group. Similar findings were reported in a double-blind controlled trial in children and adolescents with ADHD who were randomized to receive clonidine-XR (up to 0.4 mg/day) or placebo in combination with their baseline stimulant medication [98]. In this study, treatment with clonidine-XR plus a stimulant was well tolerated, and only slight decreases in mean systolic BP (4.7 mmHg), diastolic BP (3.7 mmHg) and HR (5 bpm) were observed in patients in the clonidine-XR plus stimulant group (systolic, 4.7 mmHg; diastolic, 2.6 mmHg), whereas in patients receiving placebo plus a stimulant very small increases in HR (3.1 bpm), and mean systolic (1.6 mmHg) and diastolic BP (0.4 mmHg) were observed. In addition, there were no clinically relevant differences between the placebo plus stimulant and clonidine-XR plus stimulant groups in the number of individuals with increased QTc (using Bazett’s formula or Fridericia’s formula), and no patient had a QTc >450 ms (using Fridericia’s formula) or a QTc 475 ms (using Bazett’s formula).
There have been some safety concerns of clonidine-IR administered concomitantly with methylphenidate from older reports of cases of sudden death associated with clonidine and methylphenidate use [100, 101]. However, children included in these case reports [100, 101] had co-morbidities or other aetiological factors that could explain the deaths, such as the case of sudden death in a child with a congenital cardiac malformation when taking clonidine [102], therefore making it difficult to establish the exact contribution of clonidine to the adverse outcomes. A QT/QTc prolongation (612/601 ms) was also observed in an isolated case report 4 h after addition of lofexidine (an α2-agonist used for opioid detoxification) in an opioid-dependent female patient previously stabilized on 80 mg of methadone [103]. In contrast, in a retrospective study conducted to assess the effects of clonidine, both alone and combined with psychostimulants, on the ECG of 42 children and adolescents with ADHD or tic disorder, while ECG variability was found, it did not appear to be related to any systematic effect of clonidine, either alone or in combination with psychostimulants [104]. In addition, clonidine has been reported to be safe or even confer cardioprotective effects of central origin in an animal model [105]. This α2A-agonist has also been reported to improve HR variability, a predictor of total mortality and sudden cardiac death in patients with congestive heart failure, by increasing the parasympathetic tone [106].
2.3.2 Guanfacine
Guanfacine-XR (Intuniv®; Shire Pharmaceuticals) has been approved by the FDA for the treatment of ADHD as monotherapy and as adjunctive therapy to stimulant medications in children and adolescents aged 6–17 years following the results of large, randomized, double-blind, placebo-controlled studies, showing as well the overall safety of guanfacine in youth diagnosed with ADHD [107, 108]. Dose-dependent, small to modest changes in BP, HR and ECG parameters assumingly lacking clinical significance were observed, with no patient reporting a QRS interval ≥120 ms, a QTc ≥500 ms (using Fridericia’s formula) or a QTc increase from baseline ≥60 ms [107, 108]. Similarly, cardiovascular-related adverse events with guanfacine-XR were considered uncommon in a long-term, open-label extension study, with 240 children, aged 6–17 years, followed up for up to 2 years, conducted to assess the safety profile and effectiveness of guanfacine-XR [109]. Although three subjects in this study had abnormal, clinically significant ECGs possibly related to guanfacine-XR treatment (two with bradycardia and another with junctional escape complexes), none of the ECG abnormalities were determined as serious adverse events.
There are also no reports of serious adverse cardiovascular events when combining guanfacine-XR and psychostimulant medications, as documented in a multicentre, open-label, 9-week study with 75 children and adolescents that evaluated the safety and effectiveness of guanfacine-XR administered in addition to methylphenidate or amphetamine [110]. Changes from baseline screening in QTc (using Fridericia’s formula) ranged from 0.01 to 5.15 ms, and no subject met the ECG outlier criteria (PR interval ≥200 ms, QRS interval ≥120 ms, QTc ≥500 ms or QTc change from baseline ≥60 ms). In an additional multicentre, 9-week, double-blind trial, with 461 children and adolescents aged 6–17 years randomized to receive guanfacine-XR in the morning or in the evening (to a maximum of 4 mg/day) or placebo in association with their stable stimulant medication, mean decreases in HR (5.4–5.8 bpm), systolic BP (1.5–2.9 mmHg) and diastolic BP (1.1–1.2 mmHg) were observed at endpoint in the guanfacine-XR plus stimulant group [111]. In contrast, subjects randomized to receive placebo plus a psychostimulant demonstrated slight decreases in mean HR (2.1 bpm), systolic BP (0.6 mmHg) and diastolic BP (0.0 mmHg). No subjects in any of the treatment groups developed a QTc ≥480 ms (using Fridericia’s formula) or a QTc ≥500 ms (using Bazett’s formula).
In summary, there are no reports of serious cardiovascular adverse events, sudden cardiac death or proarrhythmia associated with clonidine and guanfacine, alone or in combination with psychostimulants in recent, large, multisite, randomized, controlled trials [97–99, 111]. Overall, α2-adrenergic agonists appear to be safe regarding the risk of QT/QTc abnormalities, unless administered concomitantly with other medications known to cause drug-induced long QT/QTc syndrome or in the presence of other aetiological risk factors [92]. Although BP and HR should be monitored prior to initiation of therapy and periodically during clonidine or guanfacine treatment, ECG monitoring is unnecessary, unless there is a personal or family history of cardiac disease, arrhythmias or sudden unexpected death [19].
3 Population-Based Studies of ADHD Medication Use and Serious Cardiovascular Events
Following reports of sudden death in patients treated with ADHD medications, the FDA and Health Canada conducted in February 2006 a review of post-marketing safety data of medications used in the treatment of ADHD in an attempt to better characterize the risk of serious cardiovascular adverse events and sudden cardiac death. As a result, 27 cases of sudden death based on WHO criteria in individuals aged 18 years or less were identified from Adverse Event Reporting System (AERS) data between 1992 and 2004 in individuals taking medications for ADHD. However, when the number of patient-years of prescribed medication was incorporated into the evaluation, the frequency of reported sudden death per year of ADHD therapy with methylphenidate, atomoxetine or amphetamines among children was 0.2, 0.3 and 0.5/100,000 patient-years, respectively [112–115]. Even assuming a 50 % under-reporting rate, the sudden death risk of children on ADHD medications would be below that of children in the general population, which has a median estimated rate of 1.2–1.3/100,000/year [115]. Similarly, the risk of sudden death associated with stimulants or atomoxetine in adults was also much below background general population rates [115].
Several population-based studies, using large population-based datasets have since explored the risk of serious cardiovascular adverse events associated with medications prescribed for ADHD in children and adolescents, as well as in adults. However, due to the period of time covered by these large studies, most of these studies only address the risks of cardiovascular adverse events associated with stimulants, with only a few including atomoxetine [74, 117–119]. Furthermore, none of the studies evaluated the adverse events of recently approved medications guanfacine and clonidine.
3.1 Population-Based Studies in Children and Adolescents
Using the data of all Florida Medicaid beneficiaries who were between 3 and 20 years of age, enrolled between July 1994 and June 2004 (a total of 2,131,953 individuals), the risk for adverse cardiac events associated with methylphenidate and amphetamine salts was compared in individuals with recent diagnoses of ADHD [120, 121]. Rates of cardiac death or of hospitalizations for cardiac reasons were similar in those with ADHD who were prescribed psychostimulants compared with individuals in the general population and there were also no significant differences between those using methylphenidate and amphetamines [121]. There was a 20 % increased risk in cardiac-related emergency room visits among subjects with ADHD who used stimulant medications compared with ADHD patients who did not [120]. However, concurrent use of bronchodilators, antidepressants or antipsychotics, age 15–20 years and a history of cardiac problems were also associated with increased use of the emergency department [121].
A subsequent matched case-control study identified a significant association between sudden unexplained death and the use of stimulants (odds ratio [OR] = 7.4, 95 % CI 1.4, 74.9) [24]. Two matched groups of 564 children and adolescents taking stimulants, aged 7–19 years, identified from mortality data from 1985 to 1996 state vital statistics across the USA were included in the study, one group who had suffered sudden unexplained death, and the other group who had died as passengers in motor vehicle accidents. Ten (1.8 %) of the sudden unexplained death cases were found to be treated with a stimulant at the time of their death, as compared with only two (0.4 %) of the motor vehicle accident victims.
In Europe, a large retrospective cohort study examined the UK General Practice Research Database to identify cases of death in patients aged 2–21 years from 1 January 1993 to 30 June 2006 prescribed methylphenidate, dexamphetamine or atomoxetine for ADHD in an attempt to determine any association between these medications and a greater risk of sudden death [74]. From a cohort of 18,637 patient-years followed from the date of first prescription until whichever came first: date of death, transferred-out date, age >21 years or end of the study period, seven patients died; however, none of them were identified as cases of sudden death. Therefore, no increased risk of sudden death associated with stimulants or atomoxetine was demonstrated in this study.
An additional retrospective study found a very low rate of cardiovascular events and sudden death in a large sample that included all children from two distinct populations aged 3–17 years (n = 241,417) with a prescription for an amphetamine, atomoxetine or methylphenidate and in a matched group of medication-free children [119]. There were no statistically significant differences between medicated and unexposed children in the incidence rate of serious cardiovascular problems, including ventricular arrhythmia (0.06 vs. 0.04 per 10,000 person-years) and sudden cardiac death (0.04 per 10,000 person-years) [hazard ratios of 1.6 (95 % CI 0.19, 13.60) and 0.76 (95 % CI 0.52, 1.12), respectively].
Another recent retrospective study of the use of ADHD medications and the risk of serious cardiovascular events in a cohort of 1,200,438 children and young adults aged 2–24 years and 2,579,104 person-years of follow-up, including 373,667 person-years of current use of ADHD drugs, used data from four large, geographically and demographically diverse US health plans [117]. The study, funded by the Agency for Healthcare Research and Quality (AHRQ) and the FDA, revealed that the incidence of serious cardiovascular events was 3.1 per 100,000 person-years (81 serious cardiovascular events among cohort members), and showed no evidence that current use of an ADHD drug was associated with an increased risk of serious cardiovascular events (sudden death, MI or stroke) [adjusted hazard ratio: 0.75; 95 % CI 0.31, 1.85].
The most recent report published to date examined the possible associations between methylphenidate and mixed amphetamine salts and risk of cardiovascular events and symptoms in children and youth (aged 6–21 years) without known cardiovascular risk factors (n = 171,126) using data from claims records databases (1996–2007) [122]. Compared to no stimulant use, neither current (adjusted OR = 1.18, 95 % CI 0.89, 1.59) nor past stimulant use (adjusted OR = 0.93, 95 % CI 0.71, 1.21) was related to cardiovascular symptoms. Among stimulant users, there were 0.92 new cardiac events and 3.08 new cardiac symptoms per 1,000,000 days of current stimulant use or one event per 890 years of stimulant treatment. Only one incident of a serious cardiovascular event (including sudden death, stroke or acute cerebrovascular events, acute MI and respiratory arrest) was discovered among stimulant users. Considering all of these results, Olfson and colleagues [122] concluded that clinical diagnoses of cardiovascular events and symptoms were rare and not associated with stimulant use.
3.2 Population-Based Studies in Adults
Although several of the population-based studies in children and adolescents included young adults up to 24 years of age [74, 117, 120–122], several recent large reports specifically examined the association of medications prescribed for ADHD and the risk of cardiovascular adverse events in adult patients with ADHD.
The largest study published to date examining whether current use of medications with a labelled indication for the treatment of ADHD was associated with an increased risk of serious cardiovascular events (including MI, sudden cardiac death or stroke) in young and middle-aged adults (aged 25–64 years), compared with matched non-users, used electronic healthcare records from four study sites across the USA [118]. This retrospective study, conducted in parallel with a study of ADHD drug use and serious cardiovascular events in children and young individuals of 2–24 years of age [117]. included a total of 443,198 adults, of whom 150,359 were users of ADHD medications at baseline. No evidence was found of an increased risk of MI, sudden cardiac death or stroke associated with current use compared with nonuse (adjusted rate ratio [RR]: 0.83, 95 % CI 0.72, 0.96) or remote use (adjusted RR: 1.03, 95 % CI 0.86, 1.24) of ADHD medications. There was also little support for an increased risk with any specific medication or with longer duration of current use.
The most recent report, a nonrandomized cohort study, was conducted to determine whether use of methylphenidate in adults was associated with increased rates of serious cardiovascular events (sudden death or ventricular arrhythmias, stroke, MI or composite endpoint scores of stroke or MI) compared to nonusers [123]. A total of 43,999 adult (18 years of age and older) new methylphenidate users and 175,955 matched nonusers from a five-state Medicaid database covering 1999–2003 and a commercial insurance database, covering the period 2001–2006 were included in this study. Whilst no statistically significant difference in risk was found for stroke, MI and a combined endpoint of stroke/MI, there was an increased risk of sudden death or ventricular arrhythmia among methylphenidate users (adjusted hazard ratio: 1.84, 95 % CI 1.33, 2.55). Nonetheless, the authors concluded that the lack of a dose-response relationship between methylphenidate use and risk of sudden death or ventricular arrhythmia did not support a causal relationship.
4 Discussion
Regulatory decisions and scientific statements regarding the management of ADHD have raised questions and doubts about the cardiovascular safety of medications and the need for more complex pretreatment evaluation to determine suitability and appropriateness of approved pharmacological intervention. However, serious cardiovascular events related to ADHD medications leading to sudden unexplained cardiac death are extremely rare [19, 42, 74, 114, 117–119, 124–128].
The data and concerns about serious cardiovascular complications or sudden unexplained death in children, adolescents and adults receiving pharmacological treatment for ADHD cannot be dismissed considering the increases in BP and HR that have been reported associated with stimulants or atomoxetine in clinical trials [18, 42, 61, 114, 126, 129, 130]. However, the majority of randomized, controlled and open-label studies coincide in considering that changes in BP and HR, more commonly seen during the initial titration phase [40], albeit statistically significant, were minor or of negligible clinical significance at typical therapeutic doses in all age groups [28, 40, 64, 129]. The study by Gould et al. [24], the only one to find an association between prescription stimulants and adverse cardiovascular outcomes in children and adolescents, had a series of important limitations that had to be considered. Indeed, the FDA, which partially funded the study, has suggested caution in interpreting the findings from this study, due to methodological considerations, which may have confounded the association [131]. In addition to the limitations inherent in the design of retrospective case–control studies [132], the study had a relatively small sample size, it failed to match on race and geographical region, there was a significant recall bias, parents of 40 % of eligible cases could not be found or would not provide information, and the authors were unable to accurately estimate the rates of ADHD [24, 112, 126, 133, 134].
There is currently not enough evidence of an increased risk for cardiovascular symptoms or cardiovascular disease among adults who were medicated as children for ADHD [19]. To clarify this and to explore whether exposure to stimulant medication was associated with increased HR, systolic or diastolic BP, or BP values in the prehypertension or hypertension range over a 10-year period, a recent report examined data from the MTA (Multimodal Treatment study of ADHD), a 14-month, randomized, controlled, clinical trial in 7- to 9-year-old children that was followed by naturalistic treatment for a cumulative 10-year period of evaluation [135]. No evidence could be found in this study that intensive, sustained and continuous treatment with stimulant medication starting at ages 7–9 years increased the risk for prehypertension or hypertension over the 10-year period of observation. Similarly, stimulants did not increase the risk for tachycardia; however, greater cumulative stimulant exposure was associated with a significantly higher HR at years 3 and 8, possibly explained by the adrenergic effect of stimulants [135]. Based on these data and the recognition that ADHD patients with pre-existing cardiac pathology may be at greater risk, it has been recommended that BP and HR should only be more closely monitored in patients with an underlying medical condition that might be compromised by increases in these parameters [32].
The Committee for Medicinal Products for Human Use of the European Medicines Agency (EMA) conducted a review of the risks of stimulant medications, particularly with regard to cardiovascular safety [125]. It concluded that the benefits of these medicines continue to outweigh their risks, but recommended some changes in the product information with regard to cardiovascular problems suggesting it should contain information stating that before treatment, all patients should be screened for any problems with their BP or HR, the family history of cardiovascular problems should be assessed and any patients with these problems should not be treated without specialist evaluation. It also recommended regular monitoring of BP and HR and any problems that develop should be investigated promptly.
Family history, medical history and physical examination have reportedly low sensitivity for identifying serious cardiac pathology compared with ECG [124]. It may therefore seem reasonable to obtain a baseline ECG for any patient starting pharmacological treatment for ADHD if access to such screening is readily available and not too costly. However, no studies or compelling clinical evidence has demonstrated that the likelihood of sudden death is higher in children receiving medications for ADHD than that in the general population [136], and there is no current evidence suggesting an incremental benefit to ECG assessment of patients prior to initiating pharmacological treatment [137]. Furthermore, the positive predictive value of ECG screening for identifying cardiac disease in otherwise asymptomatic children with ADHD has been reported to be low [138]. A cost-effectiveness evaluation has revealed that relative to current standard of care (performing a history and physical examination with cardiology referral if abnormal), adding pretreatment ECG screening for children with ADHD who are candidates for pharmacological treatment only has borderline cost effectiveness for preventing sudden cardiac death [139]. Considering also the lack of evidence supporting routine ECG during the assessment of ADHD patients before starting medication, it is not surprising that different clinical and consensus-based guidelines, as well as several institutions, including the American Academy of Pediatrics [136], the NICE guideline on diagnosis and management of ADHD in children, young people and adults [11], the multidisciplinary Canadian consensus-based guidelines [112, 127, 128], and more recent European guidelines on managing adverse effects of medication for ADHD [140], or the European Network of Hyperkinetic Disorders and the Association of European Paediatric Cardiology [137], indicated that for people taking stimulant medication and atomoxetine, routine blood tests and ECGs are not recommended unless there is a clinical indication. In contrast, in the recent systematic review from the AHRQ critically examining the effectiveness and adverse events of interventions for ADHD, while acknowledging that cardiovascular concerns remain rare, it was suggested that use of α2-adrenergic agonists may require greater monitoring than psychostimulants or atomoxetine [141],
Independently of pharmacological treatment, ADHD itself may be associated with an increased risk of pre-existing cardiovascular conditions and sudden unexplained death, possibly as a result of the highly prevalent physical and psychiatric co-morbidities associated with the disorder [126, 140, 142]. An increased incidence of hypertension has been suggested in children with ADHD [143], and 10.5 % (n = 917) of patients in a retrospective cohort study of privately insured adults with new ADHD treatment episodes had evidence of one or more preexisting cardiovascular condition [142]. In addition, in a recent study analyzing HR variability (HRV) in children with a mean age of 10.8 years, diagnosed with ADHD, prior to (n = 12) or during methylphenidate treatment (n = 19), it was revealed that, compared with a group of 19 age-matched healthy children, children with ADHD showed significant lower values in HRV parameters [144]. These decreases in HRV parameters have been hypothesized to reflect diminished vagal tone, a well known risk factor of sudden cardiac death in adults, and interestingly these values improved in methylphenidate-treated children with ADHD [144]. A significantly higher rate of early repolarization patterns has also been found in ADHD children compared with normal controls, irrespective of stimulant treatment or gender [36]. A greater prevalence of cardiovascular pathology may be seen in subjects with ADHD than in the general population, possibly also associated with the high rate of co-morbid psychiatric disorders, such as depression, anxiety or substance use disorders [124]. In addition, changes in cardiovascular variables observed with stimulant pharmacotherapy in patients with ADHD may also be influenced by polymorphisms in several genes consistently associated with cardiovascular diseases [145].
5 Conclusion
Despite existing controversy, the risk for serious cardiovascular adverse events and sudden cardiac death associated with stimulants, atomoxetine or α2-adrenergic agonists prescribed for ADHD is extremely low and the benefits of treating individual patients with ADHD, after an adequate assessment, outweigh the risks [15, 16, 73, 113, 140, 146]. Health administrative data suggest that neither cardiac events among those aged 20 years and younger nor cerebrovascular accidents in adults are more frequent among those using medications for ADHD than for individuals in the general population [141]. At therapeutic doses, medications used to treat ADHD are not linked to increased risk of heart attack or other serious cardiovascular problems, including an increased QTc, in children, adolescents or adults, as evidenced in several large studies [17, 61, 97–99, 111, 122, 123], including two recent reports from the Effective Health Care Program of the AHRQ [117, 118]. It is important to note that the Bazett correction formula, the most commonly used to calculate QTc, appears to overestimate the prevalence of prolonged QTc in the paediatric population [146, 147]. There are no reports of TdP directly related to medications used for treating ADHD. Nonetheless, great caution is advised when considering stimulants, atomoxetine or any other medication for patients of any age with a diagnosis of ADHD and a personal or family history of cardiovascular disease, or with other risks for cardiovascular events. Similar caution is recommended in the presence of co-prescription with other pharmacotherapies with a known risk of cardiac adverse events.
Future research of children and adolescents as well as in adults with ADHD should focus on the potential clinical impact of the relatively small, but clinically significant increases in HR and BP associated with CNS stimulant treatment [18]. There is need for further studies to address these questions, and to help develop useful and practical clinical recommendations to guide clinicians in these specific situations. Current data are probably insufficient to develop clinical guidelines, considering that the currently available evidence has not been specifically designed to evaluate cardiovascular adverse effects or the risk of sudden cardiac death of pharmacotherapies for ADHD, making it difficult to draw firm conclusions [42]. In addition, an extremely large sample would be required to adequately estimate whether the risk is above the base rate in the general population in light of the rare occurrence of these serious complications.
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
Biederman J, Faraone SV. Attention-deficit hyperactivity disorder. Lancet. 2005;366:237–48.
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36:159–65.
Kooij SJ, Bejerot S, Blackwell A, et al. European consensus statement on diagnosis and treatment of adult ADHD: the European Network Adult ADHD. BMC Psychiatry. 2010;10:67.
Stein MA. Impairment associated with adult ADHD. CNS Spectr. 2008;13(Suppl. 12):9–11.
Sala M, Lazzaretti M, De Vidovich G, et al. Electrophysiological changes of cardiac function during antidepressant treatment. Ther Adv Cardiovasc Dis. 2009;3:29–43.
Roden DM. Drug-induced prolongation of the QT interval. N Engl J Med. 2004;350:1013–22.
Bradley C. The behavior of children receiving Benzedrine. Am J Psychiatry. 1937;94:577–85.
Banaschewski T, Coghill D, Santosh P, et al. Long-acting medications for the hyperkinetic disorders: a systematic review and European treatment guideline. Eur Child Adolesc Psychiatry. 2006;15:476–95.
Faraone SV, Glatt SJ. A comparison of the efficacy of medications for adult ADHD using meta-analysis of effect sizes. J Clin Psychiatry. 2010;71:754–63.
National Collaborating Centre for Mental Health. Attention deficit hyperactivity disorder: the NICE guideline on diagnosis and management of ADHD in children, young people and adults. National clinical practice guideline number 72. London: Alden Press; 2009.
National Institute of Mental Health. National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: 24-month outcomes of treatment strategies for attention-deficit/hyperactivity disorder. Pediatrics. 2004;113:754–61.
Volkow ND, Wang GJ, Fowler JS, et al. Dopamine transporter occupancies in the human brain induced by therapeutic doses of oral methylphenidate. Am J Psychiatry. 1998;155:1325–31.
Volkow ND, Wang GJ, Fowler JS, et al. Evidence that methylphenidate enhances the saliency of a mathematical task by increasing dopamine in the human brain. Am J Psychiatry. 2004;161:1173–80.
Aagaard L, Hansen EH. The occurrence of adverse drug reactions reported for attention deficit hyperactivity disorder (ADHD) medications in the pediatric population: a qualitative review of empirical studies. Neuropsychiatr Dis Treat. 2011;7:729–44.
Graham J, Coghill D. Adverse effects of pharmacotherapies for attention-deficit hyperactivity disorder: epidemiology, prevention and management. CNS Drugs. 2008;22:213–37.
Findling RL, Biederman J, Wilens TE, et al. Short- and long-term cardiovascular effects of mixed amphetamine salts extended release in children. J Pediatr. 2005;147:348–54.
Mick E, McManus DD, Goldberg RJ. Meta-analysis of increased heart rate and blood pressure associated with CNS stimulant treatment of ADHD in adults. Eur Neuropsychopharmacol (epub 2012 Jul 13).
Vitiello B. Understanding the risk of using medications for attention deficit hyperactivity disorder with respect to physical growth and cardiovascular function. Child Adolesc Psychiatr Clin N Am. 2008;17:459–74.
Wilens TE, Hammerness PG, Biederman J, et al. Blood pressure changes associated with medication treatment of adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2005;66:253–9.
Wilens T, McBurnett K, Stein M, et al. ADHD treatment with once-daily OROS methylphenidate: final results from a long-term open-label study. J Am Acad Child Adolesc Psychiatry. 2005;44:1015–23.
Ballard JE, Boileau RA, Sleator EK, et al. Cardiovascular responses of hyperactive children to methylphenidate. JAMA. 1976;236:2870–4.
Volkow ND, Wang GJ, Fowler JS, et al. Cardiovascular effects of methylphenidate in humans are associated with increases of dopamine in brain and of epinephrine in plasma. Psychopharmacology (Berl). 2003;166:264–70.
Gould MS, Walsh BT, Munfakh JL, et al. Sudden death and use of stimulant medications in youths. Am J Psychiatry. 2009;166:992–1001.
Pilgrim JL, Gerostamoulos D, Drummer OH, et al. Involvement of amphetamines in sudden and unexpected death. J Forensic Sci. 2009;54:478–85.
Moen MD, Keam SJ. Dexmethylphenidate extended release: a review of its use in the treatment of attention-deficit hyperactivity disorder. CNS Drugs. 2009;23:1057–83.
Santosh PJ, Sattar S, Canagaratnam M. Efficacy and tolerability of pharmacotherapies for attention-deficit hyperactivity disorder in adults. CNS Drugs. 2011;25:737–63.
Wilens TE, Biederman J, Lerner M, et al. Effects of once-daily osmotic-release methylphenidate on blood pressure and heart rate in children with attention-deficit/hyperactivity disorder: results from a one-year follow-up study. J Clin Psychopharmacol. 2004;24:36–41.
Biederman J, Mick E, Surman C, et al. A randomized, placebo-controlled trial of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2006;59:829–35.
Rösler M, Fischer R, Ammer R, Ose C, et al. A randomised, placebo-controlled, 24-week, study of low-dose extended-release methylphenidate in adults with attention-deficit/hyperactivity disorder. Eur Arch Psychiatry Clin Neurosci. 2009;259:120–9.
Adler LA, Zimmerman B, Starr HL, et al. Efficacy and safety of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, double-blind, parallel group, dose-escalation study. J Clin Psychopharmacol. 2009;29:239–47.
Adler LA, Orman C, Starr HL, et al. Long-term safety of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: an open-label, dose-titration, 1-year study. J Clin Psychopharmacol. 2011;31:108–14.
Lucas PB, Gardner DL, Wolkowitz OM, et al. Methylphenidate-induced cardiac arrhythmias [letter]. N Engl J Med. 1986;315:1485.
Deshmankar BS, Lewis JA. Ventricular tachycardia associated with the administration of methylphenidate during guanethidine therapy. Can Med Assoc J. 1967;97:1166–7.
Fernández-Fernández MA, Rufo-Campos M, Mateos-Checa R, et al. Cardiovascular side effects secondary to treatment with methylphenidate [in Spanish]. Rev Neurol. 2010;50:573–4.
Nahshoni E, Sclarovsky S, Spitzer S, et al. Early repolarization in young children with attention-deficit/hyperactivity disorder versus normal controls: a retrospective preliminary chart review study. J Child Adolesc Psychopharmacol. 2009;19:731–5.
Hill SL, El-Khayat RH, Sandilands EA, et al. Electrocardiographic effects of methylphenidate overdose. Clin Toxicol (Phila). 2010;48:342–6.
Klampfl K, Quattländer A, Burger R, et al. Case report: intoxication with high dose of long-acting methylphenidate (Concerta®) in a suicidal 14-year-old girl. Atten Defic Hyperact Disord. 2010;2:221–4.
Ozdemir E, Karaman MG, Yurteri N, et al. A case of suicide attempt with long-acting methylphenidate (Concerta). Atten Defic Hyperact Disord. 2010;2:103–5.
Hammerness P, Wilens T, Mick E, et al. Cardiovascular effects of longer-term, high-dose OROS methylphenidate in adolescents with attention deficit hyperactivity disorder. J Pediatr. 2009;155:84–9.
Ruwald MH, Ruwald AC, Tønder N. Methylphenidate induced ST elevation acute myocardial infarction [in Danish]. Ugeskr Laeger. 2012;174:647–8.
Stiefel G, Besag FM. Cardiovascular effects of methylphenidate, amphetamines and atomoxetine in the treatment of attention-deficit hyperactivity disorder. Drug Saf. 2010;33:821–42.
Kalant H, Kalant OJ. Death in amphetamine users: causes and rates. Can Med Assoc J. 1975;112:299–304.
Lora-Tamayo C, Tena T, Rodríguez A. Amphetamine derivative related deaths. Forensic Sci Int. 1997;85:149–57.
Barr AM, Panenka WJ, MacEwan GW, et al. The need for speed: an update on methamphetamine addiction. J Psychiatry Neurosci. 2006;31:301–13.
Sylvester AL, Agarwala B. Acute myocardial infarction in a teenager due to Adderall XR. Pediatr Cardiol. 2012;33:155–7.
Wilens TE, Spencer TJ, Biederman J. Short- and long-term cardiovascular effects of mixed amphetamine salts extended-release in adolescents with ADHD. CNS Spectr. 2005;10(Suppl. 15):22–30.
Donner R, Michaels MA, Ambrosini PJ. Cardiovascular effects of mixed amphetamine salts extended release in the treatment of school-aged children with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007;61:706–12.
Weisler RH, Biederman J, Spencer TJ, et al. Long-term cardiovascular effects of mixed amphetamine salts extended release in adults with ADHD. CNS Spectr. 2005;10:35–43.
Cowles BJ. Lisdexamfetamine for treatment of attention-deficit/hyperactivity disorder. Ann Pharmacother. 2009;43:669–76.
Pennick M. Absorption of lisdexamfetamine dimesylate and its enzymatic conversion to d-amphetamine. Neuropsychiatr Dis Treat. 2010;6:317–27.
Elbe D, Macbride A, Reddy D. Focus on lisdexamfetamine: a review of its use in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2010;19:303–14.
Findling R, Childress A, Cutler A, et al. Efficacy and safety of lisdexamfetamine dimesylate in adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2011;50:395–405.
Adler LA, Weisler RH, Goodman DW, et al. Short-term effects of lisdexamfetamine dimesylate on cardiovascular parameters in a 4-week clinical trial in adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2009;70:1652–61.
Hammerness P, Zusman R, Systrom D, et al. A cardiopulmonary study of lisdexamfetamine in adults with attention-deficit/hyperactivity disorder. World J Biol Psychiatry (epub 2012 May 6).
Garnock-Jones KP, Keating GM. Atomoxetine: a review of its use in attention-deficit hyperactivity disorder in children and adolescents. Pediatr Drugs. 2009;11:203–26.
Zerbe RL, Rowe H, Enas GG, et al. Clinical pharmacology of tomoxetine, a potential antidepressant. J Pharmacol Exp Ther. 1985;232:139–43.
Michelson D, Faries D, Wernicke J, et al. Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose-response study. Pediatrics. 2001;108:E83–91.
Michelson D, Adler L, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo-controlled studies. Biol Psychiatry. 2003;53:112–20.
Spencer TJ, Biederman J, Wilens TE, et al. Novel treatments for attention-deficit/hyperactivity disorder in children. J Clin Psychiatry. 2002;63(Suppl. 12):16–22.
Kratochvil CJ, Milton DR, Vaughan BS, et al. Acute atomoxetine treatment of younger and older children with ADHD: a meta-analysis of tolerability and efficacy. Child Adolesc Psychiatry Ment Health. 2008;2:25.
Simpson D, Plosker GL. Atomoxetine: a review of its use in adults with attention deficit hyperactivity disorder. Drugs. 2004;64:205–22.
Wernicke JF, Kratochvil CJ. Safety profile of atomoxetine in the treatment of children and adolescents with ADHD. J Clin Psychiatry. 2002;63(Suppl. 12):50–5.
Wolraich ML, McGuinn L, Doffing M. Treatment of attention deficit hyperactivity disorder in children and adolescents: safety considerations. Drug Saf. 2007;30:17–26.
Trzepacz PT, Williams DW, Feldman PD, et al. CYP2D6 metabolizer status and atomoxetine dosing in children and adolescents with ADHD. Eur Neuropsychopharmacol. 2008;18:79–86.
Michelson D, Read HA, Ruff DD, et al. CYP2D6 and clinical response to atomoxetine in children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2007;46:242–51.
Loghin C, Haber H, Beasley CM, et al. Effects of atomoxetine on the QT interval in healthy CYP2D6 poor metabolizers. Br J Clin Pharmacol (epub 2012 Jul 16).
Jefferson JW. A review of the cardiovascular effects and toxicity of tricyclic antidepressants. Psychosom Med. 1975;37:160–79.
Wilens TE, Biederman J, Baldessarini RJ, et al. Cardiovascular effects of therapeutic doses of tricyclic antidepressants in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1996;35:1491–501.
Wernicke JF, Faries D, Girod D, et al. Cardiovascular effects of atomoxetine in children, adolescents, and adults. Drug Saf. 2003;26:729–40.
Stratteran® (atomoxetine tablets): US prescribing information. Indianapolis: Eli Lilly and Company; 2011.
Peterson K, McDonagh MS, Fu R. Comparative benefits and harms of competing medications for adults with attention-deficit hyperactivity disorder: a systematic review and indirect comparison meta-analysis. Psychopharmacology. 2008;197:1–11.
Wilens TE, Newcorn JH, Kratochvil CJ, et al. Long-term atomoxetine treatment in adolescents with attention-deficit/hyperactivity disorder. J Pediatr. 2006;149:112–9.
McCarthy S, Cranswick N, Potts L, et al. Mortality associated with attention-deficit hyperactivity disorder (ADHD) drug treatment: a retrospective cohort study of children, adolescents and young adults using the general practice research database. Drug Saf. 2009;32:1089–96.
Dovies M, Cornelius V, Fogg C, et al. A study to examine cardiac events in patients prescribed atomoxetine in England: results of an interim modified prescription event monitoring study. Drug Saf. 2009;32:976–7.
Sert A, Gokcen C, Aypar E, et al. Effects of atomoxetine on cardiovascular functions and on QT dispersion in children with attention deficit hyperactivity disorder. Cardiol Young. 2012;22:158–61.
Lovecchio F, Kashani J. Isolated atomoxetine (Strattera) ingestions commonly result in toxicity. J Emerg Med. 2006;31:267–8.
Spiller HA, Lintner CP, Winter ML. Atomoxetine ingestions in children: a report from poison centers. Ann Pharmacother. 2005;39:1045–8.
Stojanovski SD, Robinson RF, Baker SD, et al. Children and adolescent exposures to atomoxetine hydrochloride reported to a poison control center. Clin Toxicol (Philadelphia). 2006;44:243–7.
Barker MJ, Benitez JG, Ternullo S, et al. Acute oxcarbazepine and atomoxetine overdose with quetiapine. Vet Hum Toxicol. 2004;46:130–2.
Sawant S, Daviss SR. Seizures and prolonged QTc with atomoxetine overdose [letter]. Am J Psychiatry. 2004;161:757.
Kashani J, Ruha AM. Isolated atomoxetine overdose resulting in seizure. J Emerg Med. 2007;32:175–8.
Scherer D, Hassel D, Bloehs R, et al. Selective noradrenaline reuptake inhibitor atomoxetine directly blocks hERG currents. Br J Pharmacol. 2009;156:226–36.
Curran ME, Splawski I, Timothy KW, et al. A molecular basis for cardiac arrhythmia: hERG mutations cause long QT syndrome. Cell. 1995;80:795–803.
Wang Q, Chen Q, Towbin JA. Genetics, molecular mechanisms and management of long QT syndrome. Ann Med. 1998;30:58–65.
Cohen DJ, Young JG, Nathanson JA, et al. Clonidine in Tourette’s syndrome. Lancet. 1979;2(8142):551–3.
Connor DF, Fletcher KE, Swanson JM. A meta-analysis of clonidine for symptoms of attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1999;38:1551–9.
Gourlay S, Forbes A, Marriner T, et al. A placebo-controlled study of three clonidine doses for smoking cessation. Clin Pharmacol Ther. 1994;55:64–9.
Gowing LR, Farrell M, Ali RL, et al. α2-Adrenergic agonists in opioid withdrawal. Addiction. 2002;97:49–58.
Arnsten AF, Scahill L, Findling RL. Alpha-2 adrenergic receptor agonists for the treatment of attention-deficit/hyperactivity disorder: emerging concepts from new data. J Child Adolesc Psychopharmacol. 2007;17:393–406.
Connor DF, Findling RL, Kollins SH, et al. Effects of guanfacine extended release on oppositional symptoms in children aged 6–12 years with attention-deficit hyperactivity disorder and oppositional symptoms: a randomized, double-blind, placebo-controlled trial. CNS Drugs. 2010;24:755–68.
Ming X, Mulvey M, Mohanty S, et al. Safety and efficacy of clonidine and clonidine extended-release in the treatment of children and adolescents with attention deficit and hyperactivity disorders. AHMT. 2011;2:105–12.
Scahill L. Alpha-2 adrenergic agonists in children with inattention, hyperactivity and impulsiveness. CNS Drugs. 2009;23(Suppl. 1):43–9.
Cinnamon Bidwell L, Dew RE, Kollins SH. Alpha-2 adrenergic receptors and attention-deficit/hyperactivity disorder. Curr Psychiatry Rep. 2010;12:366–73.
Jain AK, Hiremath A, Michael R, et al. Clonidine and guanfacine in hypertension. Clin Pharmacol Ther. 1985;37:271–6.
Childress AC, Sallee FR. Revisiting clonidine: an innovative add-on option for attention-deficit/hyperactivity disorder. Drugs Today (Barc). 2012;48:207–17.
Jain R, Segal S, Kollins SH, et al. Clonidine extended-release tablets for pediatric patients with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2011;50:171–9.
Kollins SH, Jain R, Brams M, et al. Clonidine extended-release tablets as add-on therapy to psychostimulants in children and adolescents with ADHD. Pediatrics. 2011;127:e1406–13.
Daviss WB, Patel NC, Robb AS, et al. Clonidine for attention-deficit/hyperactivity disorder: II. ECG changes and adverse events analysis. J Am Acad Child Adolesc Psychiatry. 2008;47:189–98.
Fenichel RR. Combining methylphenidate and clonidine: the role of post-marketing surveillance. J Child Adolesc Psychopharmacol. 1995;5:155–6.
Maloney MJ, Schwam JS. Clonidine and sudden death. Pediatrics. 1995;96:1176–7.
Cantwell DP, Swanson J, Connor DF. Case study: adverse response to clonidine. J Am Acad Child Adolesc Psychiatry. 1997;36:539–44.
Schmittner J, Schroeder JR, Epstein DH, et al. QT interval increased after single dose of lofexidine. BMJ. 2004;329:1075.
Kofoed L, Tadepalli G, Oesterheld JR, et al. Case series: clonidine has no systematic effects on PR or QTc intervals in children. J Am Acad Child Adolesc Psychiatry. 1999;38:1193–6.
Catelli M, Feldman J, Bousquet P, et al. Protective effects of centrally acting sympathomodulatory drugs on myocardial ischemia induced by sympathetic overactivity in rabbits. Braz J Med Biol Res. 2003;36:85–95.
Girgis I, Chakko S, de Marchena E, et al. Effect of clonidine on heart rate variability in congestive heart failure. Am J Cardiol. 1998;82:335–7.
Biederman J, Melmed RD, Patel A, et al. A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics. 2008;121:e73–84.
Sallee F, McGough J, Wigal T, et al. Guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder: a placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2009;48:155–65.
Biederman J, Melmed RD, Patel A, et al. Long-term, open-label extension study of guanfacine extended release in children and adolescents with ADHD. CNS Spectr. 2008;13:1047–55.
Spencer TJ, Greenbaum M, Ginsberg LD. Safety and effectiveness of coadministration of guanfacine extended release and psychostimulants in children and adolescents with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2009;19:501–10.
Wilens TE, Bukstein O, Brams M, et al. A controlled trial of extended-release guanfacine and psychostimulants for attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2012;51:74–85.
Bélanger S, Warren A, Hamilton R, et al. Cardiac risk assessment before the use of stimulant medications in children and youth. Paediatr Child Health. 2009;14:579–92.
Knight M. Stimulant drug therapy for attention deficit disorder (with or without hyperactivity) and sudden cardiac death. Pediatrics. 2007;119:154–5.
Nissen SE. ADHD drugs and cardiovascular risk. N Engl J Med. 2006;354:1445–8.
Villalba L. Follow up review of AERS search identifying cases of sudden death occurring with drugs used for the treatment of attention deficit hyperactivity disorder (ADHD), February 28, 2006 (online). http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4210b_07_01_safetyreview.pdf. Accessed 30 May 2011.
Berger S, Utech L, Hazinski MF. Sudden death in children and adolescents. Pediatr Clin North Am. 2004;51:1653–77.
Cooper WO, Habel LA, Sox CM, et al. ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med. 2011;365:1896–904.
Habel LA, Cooper WO, Sox CM, et al. ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA. 2011;306:2673–83.
Schelleman H, Bilker WB, Strom BL, et al. Cardiovascular events and death in children exposed and unexposed to ADHD agents. Pediatrics. 2011;127:1102–10.
Winterstein AG, Gerhard T, Shuster J, et al. Cardiac safety of central nervous system stimulants in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics. 2007;120:e1494–501.
Winterstein AG, Gerhard T, Shuster J, et al. Cardiac safety of methylphenidate versus amphetamine salts in the treatment of ADHD. Pediatrics. 2009;124:e75–80.
Olfson M, Huang C, Gerhard T, et al. Stimulants and cardiovascular events in youth with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2012;51:147–56.
Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169:178–85.
Elia J, Vetter VL. Cardiovascular effects of medications for the treatment of attention-deficit hyperactivity disorder: what is known and how should it influence prescribing in children? Pediatr Drugs. 2010;12:165–75.
European Medicines Agency, Committee for Medicinal Products for Human Use (CHMP). Elements recommended for inclusion in summaries of product characteristics for methylphenidate-containing medicinal products authorised for the treatment of ADHD in children aged six years and above and adolescents. Wording recommended by the CHMP on 22 January 2009 (online). http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Methylphenidate_31/WC500011184.pdf. Accessed 18 Mar 2011.
Vitiello B, Towbin K. Stimulant treatment of ADHD and risk of sudden death in children. Am J Psychiatry. 2009;166:955–7.
Warren AE, Hamilton RM, Bélanger SA, et al. Cardiac risk assessment before the use of stimulant medications in children and youth: a joint position statement by the Canadian Paediatric Society, the Canadian Cardiovascular Society, and the Canadian Academy of Child and Adolescent Psychiatry. Can J Cardiol. 2009;25:625–30.
Hamilton R, Gray C, Bélanger SA, et al. Cardiac risk assessment before the use of stimulant medications in children and youth: a joint position statement by the Canadian Paediatric Society, the Canadian Cardiovascular Society and the Canadian Academy of Child and Adolescent Psychiatry. J Can Acad Child Adolesc Psychiatry. 2009;18:349–55.
Swanson J, Gupta S, Lam A, et al. Development of a new once-a-day formulation of methylphenidate for the treatment of attention-deficit/hyperactivity disorder: proof-of-concept and proof-of-product studies. Arch Gen Psychiatry. 2003;60:204–11.
Silva RR, Skimming JW, Muniz R. Cardiovascular safety of stimulant medications for pediatric attention-deficit hyperactivity disorder. Clin Pediatr (Phila). 2010;49:840–51.
Kuehn BM. Stimulant use linked to sudden death in children without heart problems. JAMA. 2009;302:613–4.
Hayden GF, Kramer MS, Horwitz RI. The case–control study: a practical review for the clinician. JAMA. 1982;247:326–31.
The U.S. Food and Drug Administration. Communication about an ongoing safety review of stimulant medications used in children with attention-deficit/hyperactivity disorder (ADHD), last updated 04/20/2011 (online). http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm165858.htm. Accessed 25 Mar 2011.
Westover AN, Halm EA. Do prescription stimulants increase the risk of adverse cardiovascular events? A systematic review. BMC Cardiovasc Disord. 2012;12:41.
Vitiello B, Glen R, Elliott GR, et al. Blood pressure and heart rate over 10 years in the Multimodal Treatment Study of children with ADHD. Am J Psychiatry. 2012;169:167–77.
Perrin JM, Friedman RA, Knilans TK, et al. Cardiovascular monitoring and stimulant drugs for attention-deficit/hyperactivity disorder. Pediatrics. 2008;122:451–3.
Hamilton RM, Rosenthal E, Hulpke-Wette M, et al. Cardiovascular considerations of attention deficit hyperactivity disorder medications: a report of the European Network on Hyperactivity Disorders work group, European Attention Deficit Hyperactivity Disorder Guidelines Group on attention deficit hyperactivity disorder drug safety meeting. Cardiol Young. 2012;22:63–70.
Mahle WT, Hebson C, Strieper MJ. Electrocardiographic screening in children with attention-deficit hyperactivity disorder. Am J Cardiol. 2009;104:1296–9.
Denchev P, Kaltman JR, Schoenbaum M, et al. Modeled economic evaluation of alternative strategies to reduce sudden cardiac death among children treated for attention deficit/hyperactivity disorder. Circulation. 2010;121:1329–37.
Graham J, Banaschewski T, Buitelaar J, et al. European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry. 2011;20:17–37.
Charach A, Dashti B, Carson P, et al. Attention deficit hyperactivity disorder: effectiveness of treatment in at-risk preschoolers; long-term effectiveness in all ages; and variability in prevalence, diagnosis, and treatment. Comparative effectiveness review no. 44 (prepared by the McMaster University Evidence-based Practice Center under Contract No. MME2202 290-02-0020). AHRQ publication no. 12-EHC003-EF. Rockville (MD): Agency for Healthcare Research and Quality, October 2011 (online). http://www.effectivehealthcare.ahrq.gov/reports/final.cfm. Accessed 29 Oct 2012.
Gerhard T, Winterstein AG, Olfson M, et al. Pre-existing cardiovascular conditions and pharmacological treatment of adult ADHD. Pharmacoepidemiol Drug Saf. 2010;19:457–64.
Keltikangas-Jarvinen L, Pulkki-Raback L, Puttonen S, et al. Childhood hyperactivity as a predictor of carotid artery intima media thickness over a period of 21 years: the cardiovascular risk in young Finns study. Psychosom Med. 2006;68:509–16.
Buchhorn R, Müller C, Willaschek C, et al. How to predict the impact of methylphenidate on cardiovascular risk in children with attention deficit disorder: methylphenidate improves autonomic dysfunction in children with ADHD. ISRN Pharmacol (epub 5 Mar 2012).
Mick E, McGough JJ, Middleton FA, et al. Genome-wide association study of blood pressure response to methylphenidate treatment of attention-deficit/hyperactivity disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:466–72.
Pliszka SR. Pharmacologic treatment of attention-deficit/hyperactivity disorder: efficacy, safety and mechanisms of action. Neuropsychol Rev. 2007;17:61–72.
Prasad S, Furr AJ, Zhang S, et al. Baseline values from the electrocardiograms of children and adolescents with ADHD. Child Adolesc Psychiatry Ment Health. 2007;1:11.
Acknowledgements
Dr. Jose Martinez-Raga and Dr. Nestor Szerman have received honoraria for being speakers and on advisory boards for Janssen Pharmaceuticals. Dr. Carlos Knecht and Dr. Isabel Martinez report no conflicts of interest that are directly relevant to the content of this manuscript. No sources of funding were used in the preparation, review or approval of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martinez-Raga, J., Knecht, C., Szerman, N. et al. Risk of Serious Cardiovascular Problems with Medications for Attention-Deficit Hyperactivity Disorder. CNS Drugs 27, 15–30 (2013). https://doi.org/10.1007/s40263-012-0019-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-012-0019-9