Abstract
Since the approval of the first direct-acting antiviral agents (DAAs), treatment for hepatitis C virus (HCV) has undergone significant transformation. A new milestone in the treatment of HCV, the approval of the first interferon-free regimens, could be achieved by the end of 2013. For patients with HCV who have absolute or relative contraindications to pegylated-interferon or have failed the currently available treatments, the arrival of new regimens will have a major impact on long-term outcomes. The combinations of DAAs in trials are numerous, and many have demonstrated sustained virologic response rates higher than 90 %. These improvements have also been observed in previous null responders and patients who failed telaprevir- or boceprevir-based regimens. Some specific subpopulations may not be perfectly served by interferon-free regimens, such as patients with genotypes 1a or 3 or cirrhosis, whereas others, such as HIV-infected patients or transplant patients, will definitively benefit from regimens with a lower burden of side effects. This paper reviews the interferon-free regimens currently in phase II or III for which sustained virologic response data are available and discusses the successes and potential pitfalls of these regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hepatitis C virus (HCV) is a disease that affects at least 150 million individuals worldwide [1]. Research on new therapies has progressed slowly for many years but is currently advancing at a remarkable pace. Prior to the discovery of the HCV, interferon (IFN) and its successor pegylated-interferon (PEG-IFN) have been used for the treatment of HCV [2]. Currently, IFN is a component of all treatment regimens for all HCV genotypes. Unfortunately, IFN has been associated with the vast majority of side effects, including flu-like symptoms, depression, anemia, leukopenia, thrombocytopenia, thyroid dysfunction, flare of autoimmune conditions, and several others. A meta-analysis looking at the serious adverse events during PEG-IFN/ribavirin clinical trials reported rates of 7 % [3]. In addition, IFN is contraindicated in certain patient populations, such as organ recipients other than liver, and patients with uncontrolled psychiatric conditions or autoimmune conditions. In combination, these reasons have left many patients without treatment options. For patients in whom IFN is indicated, treatment is often refused due to fear of potential side effects [4]. In the HCV protease inhibitor era, Chen et al. [5] recently looked at reasons for non-initiation of HCV treatment in their genotype 1 population and found that patients had relative or absolute contraindications 51 % of the time and that 23 % of the patients refused the treatment.
Rates of sustained virologic response (SVR) in genotypes 2–3 are 70–85 % with PEG-IFN and ribavirin [6]. For HCV genotype 1 patients previously naive to treatment, the rates have been recently improved to 63–75 % with the introduction of the first direct-acting antiviral agents (DAAs), telaprevir and boceprevir [7, 8]. There still remain a significant number of patients in need of another option. In addition, patients carrying the CT or TT alleles of the recently discovered interleukin (IL)-28B polymorphism are less sensitive to IFN and genetically less likely to achieve SVR with an IFN-based regimen [9]. These alleles are over-represented in the African American population and may partially explain the lower SVR rates typically achieved in this population [9]. For carriers of these negative alleles, regimens without IFN are likely to make a significant difference.
Alternative treatments are needed and are rapidly approaching. Numerous combinations of DAAs are currently in phase III and the New Drug Application (NDA) for the first IFN-free combination was submitted in April 2013 [10]. The aim of this paper is to review more advanced IFN-free trials and to underline the strengths and weaknesses of these types of regimens. A PubMed search was conducted to find preliminary and final results of phase II and III interferon-free trials. Abstracts from the American Association for the Study of Liver Diseases (AASLD), the European Association for the Study of Liver (EASL), the Asia Pacific Association for the Study of the Liver (APASL), and the Conference on Retroviruses and Opportunistic Infections (CROI) were also evaluated. Studies of agents for which the development was stopped or put on hold were not included in this review.
2 Overview of the Direct-Acting Antiviral Agent (DAA) Classes
NS3/NS4 protease inhibitors are the most advanced class, with two agents already approved: telaprevir and boceprevir (Table 1). Simeprevir, faldaprevir, asunaprevir, danoprevir, and ABT-450/r are also under development. Protease inhibitors are characterized by a high potency and a low barrier to resistance. Many of these agents are also associated with a significant number of drug–drug interactions. Telaprevir and boceprevir are administered three times daily and can induce significant adverse events, mainly anemia, rash, and ano-rectal symptoms for telaprevir, and anemia and dysgeusia for boceprevir [7, 8, 11, 12]. Simeprevir and faldaprevir are once-daily drugs [13–15]. Faldaprevir has been associated with photosensitivity, and sunscreen use is recommended during administration [13, 14].
Daclatasvir and ledipasvir are NS5A polymerase inhibitors and are more advanced in their development. In general, NS5A polymerase inhibitors are highly potent, have multi-genotypic coverage, and intermediate barrier to resistance. Daclatasvir has a half-life of 12–15 h, suitable for once-daily dosing [16]. Importantly, daclatasvir and ledipasvir will likely be used in combination with other DAAs. In studies examining daclatasvir in combination with asunaprevir, common adverse events included headache, nasopharyngitis, elevations in alanine aminotransferase (ALT) and aspartate aminotransferase (AST), and diarrhea [17, 18]. In phase I and II studies, ledipasvir was well tolerated, with headaches and fatigue being the most frequent adverse events [19].
Sofosbuvir and mericitabine are NS5B nucleos(t)ide polymerase inhibitors currently under development. NS5B inhibitors commonly have a high barrier to resistance and have pan-genotypic activity. Sofosbuvir is administered once daily and mericitabine will be administered twice daily [6, 20–22]. Both of these drugs have been well tolerated, with fatigue and headache being the most common adverse events [6, 20, 21, 23].
The NS5B non-nucleosidic polymerase inhibitors (NNIs) for which IFN-free trial results are available include deleobuvir (BI207127), GS-9669, ABT-072, and ABT-333. Generally, NNIs have limited genotypic coverage and a low barrier to resistance. NNIs also have an intermediate level of potency. ABT-072 and GS-9669 will likely require daily dosing. Deleobuvir and ABT-333 will be administered twice daily [14, 24].
3 Interferon-Free Regimens: Proof of Principle
The first proof of principle for an IFN-free regimen was presented in 2011 at the International Liver Congress of EASL. In this small, phase IIa study combining daclatasvir and asunaprevir for 24 weeks in previous null responders, 4 of the 11 (36 %) patients achieved SVR24 (Table 2) [17]. The rate of SVR24 may seem small, but these were prior null responders to IFN. In addition to proving that IFN was not required to achieve an SVR, the same study also demonstrated that quadruple therapy (daclatasvir, asunaprevir, PEG-IFN, and ribavirin) could lead to SVR rates of 100 % in null responders [17].
Another key study highlighting this proof of principle was the ELECTRON study. The results for the first arms of the study were presented in 2011 at the Liver Meeting of the AASLD [22]. The study addressed several questions: how many weeks of PEG-IFN are required to achieve SVR, can a single DAA be used in monotherapy, and is an IFN-free combination effective in different genotypes and in patients with different previous treatment responses? The first part of the study included eight arms: sofosbuvir alone, in combination with ribavirin and in combination with PEG-IFN for different durations (4, 8, and 12 weeks) in patients with genotype 2 or 3 and sofosbuvir and ribavirin for 12 weeks in naives and previous null responder patients with genotype 1. Ten patients were included in each arm, except for the genotype 1 naive arm, which included 25 patients. Genotype 2 or 3 patients who were on sofosbuvir monotherapy achieved a SVR rate of 60 %, while 100 % of the patients receiving sofosbuvir/ribavirin with or without PEG-IFN achieved SVR. This suggested that the length of IFN treatment did not have an influence on SVR rates. Importantly, the monotherapy arm suggested that a combination of agents or, more specifically, ribavirin was required. For those with genotype 1, results were satisfying for previously naive (84 %), but not for previous null responders (10 %). In this study, all failures were relapsers and only one patient developed the S282T mutation, the one conferring resistance to sofosbuvir [22].
Based on the results of the ELECTRON study, Gilead developed a phase III program for the combination of sofosbuvir/ribavirin in patients with HCV genotype 2 and 3. FISSION studied treatment-naive patients; FUSION, previously treated patients; and POSITRON, IFN ineligible/intolerant/unwilling patients [6, 21]. FISSION was a non-inferiority trial comparing 12 weeks of sofosbuvir and ribavirin with 24 weeks of PEG-IFN/ribavirin, the current standard of care for HCV genotype 2 and 3 treatment. The SVR rate was 67 % in both arms, proving non-inferiority. There was an important difference in SVR between the patients with genotype 2 or 3 in the sofosbuvir/ribavirin arm (97 versus 56 %), whereas the difference was smaller in the patients in the PEG-IFN/ribavirin group (78 versus 63 %). This result suggests that genotypes 2 and 3 can no longer be studied in a combined manner when testing IFN-free regimens. The difference was validated in FUSION and POSITRON. FUSION was a blinded trial comparing 12 versus 16 weeks of sofosbuvir/ribavirin and POSITRON was a blinded trial of 12 weeks of sofosbuvir/ribavirin versus placebo. SVR rates were 50 and 73 % for the 12- and 16-week arms of FUSION and 78 % for the active treatment arm of POSITRON. Again, the genotype made a major difference, with SVR rates of 86, 94, and 93 % for genotype 2 and 30, 62, and 62 % for genotype 3. We can also infer from these results that, at least in previously treated patients, 16 weeks of treatment may in part overcome the negative impact of the genotype 3.
The QUANTUM study tested sofosbuvir, GS-0938, and ribavirin in different combinations in naive patients with genotypes 1 through 4 [25]. It confirmed that the combination of sofosbuvir/ribavirin was not ideal for genotype 1 patients (SVR rates of 65 % for genotype 1a and 48 % for genotype 1b in the sofosbuvir/ribavirin arms) [25]. The NDA submitted in April for sofosbuvir proposed its use in combination with PEG-IFN and ribavirin for genotypes 1, 4, 5, and 6, but without PEG-IFN for genotypes 2 and 3 [10]. Of note, GS-0938 demonstrated signs of liver toxicity during QUANTUM, and its development was discontinued.
4 Genotype 1a versus 1b Differences
Historically, genotype 1 has been considered the hardest to treat, and little attention was given to sub-genotype 1a and 1b. This landscape is changing with the DAAs. The difference between genotype 1a and 1b was another element discerned from the initial daclatasvir/asunaprevir study [17]. All the patients who failed the IFN-free part of the trial were genotype 1a [17]. The development of this combination is now continuing only in patients with genotype 1b. In one recently published study, this combination was tested in a phase IIa trial carried out in Japanese genotype 1b previous null responders or IFN-ineligible/intolerant patients [18]. SVR24 was achieved by 90.5 % of the null responders and 63.6 % of the previous IFN ineligible/intolerant [18]. Of note is that virtually all of the HCV in Japan is genotype 1b.
SOUND-C2 combined faldaprevir and deleobuvir with and without ribavirin for different durations (16–40 weeks) and different dosing of deleobuvir [14]. It was a phase IIb study for treatment-naive genotype 1 patients (40 % 1a and 60 % 1b). Around 10 % of the patients included had cirrhosis. SVR12 varied from 39 % for the group receiving twice-daily faldaprevir and deleobuvir without ribavirin for 28 weeks to 68 % for the group receiving twice-daily faldaprevir, deleobuvir, and ribavirin for 28 weeks [14]. The differences in SVR rates between genotype 1a and 1b were very impressive in this trial, ranging from 11–47 % for genotype 1a to 57–83 % for genotype 1b. The sub-genotype had a more important influence on the outcome than IL28B polymorphism. Patients with a genotype 1a and an IL28B CC did worse (75 %) than patients with a genotype 1b but an IL28B CT/TT (84 %) [14]. SOUND-C3 further investigated the interaction between the IL28B polymorphism and the sub-genotype [13]. Faldaprevir, deleobuvir, and ribavirin were combined for 16 weeks. The study included naive patients with either HCV genotype 1a and IL28B CC or with genotype 1b and any IL28B allele group. Only 17 % of the genotype 1a patients achieved SVR12, while 95 % achieved SVR in the patients with genotype 1b. This combination of agents is now in phase III, but only for genotype 1b (HCVerso1, 2 and 3; NCT01732796, NCT01728324, NCT01830127) [26].
A difference between genotype 1a and 1b was also found in the INFORM-SVR trial, a phase IIb study for genotype 1 naive patients with stage F0–F2 [20]. Patients received mericitabine and danoprevir boosted with ritonavir with or without ribavirin for 12 or 24 weeks. The viral load of the patients eligible for the 12-week arms had to be below quantification between weeks 2 and 8 and undetectable by week 10. The 12-week arm with ribavirin and all the placebo arms were discontinued early because of high rates of relapse. SVR12 rate in the remaining 24-week arm with ribavirin was 41 %, but was 26 versus 71 % for genotype 1a versus 1b, respectively [20]. The numbers were small, but seem again to demonstrate a more important impact of the sub-genotype than the IL28B polymorphism. Among the arms of the MATTERHORN study, two were an IFN-free combination of mericitabine, danoprevir boosted with ritonavir, and ribavirin [23]. One was for previous partial responders and the other for previous null responders. They were restricted to genotype 1b patients and led to SVR12 rates of 39 and 56 % for partial and null responders, respectively [23].
5 Successes of Combination Regimens
Although SVR rates with some agents in genotype 1a patients are lower, several combinations have overcome this hurdle. If the drugs combined are potent enough, SVR12 rates near 100 % may be achieved. Daclatasvir and sofosbuvir have been combined in study AI444-040. The first part was designed for treatment-naive patients without cirrhosis [27]. Patients with genotype 2 or 3 were randomized to a lead-in of 7 days with ribavirin followed by 23 weeks of sofosbuvir and daclatasvir or to a 24-week combination of sofosbuvir and daclatasvir from the beginning with or without ribavirin. The same arms were available for genotype 1, and there were also two 12-week arms of sofosbuvir and daclatasvir with and without ribavirin. For genotype 2 and 3, one patient in the lead-in arm relapsed, one had a breakthrough, and one patient in the treatment arm with ribavirin was lost to follow-up, leading to SVR24 rates of 88, 100, and 93 %. All the patients in the 24-week arms for genotype 1 achieved SVR24. Final data are not available yet for the 12-week arms.
The second part of study AI444-040 focused on patients who previously failed telaprevir or boceprevir treatment [28]. Patients with cirrhosis and those who discontinued due to side effects were excluded. Patients were randomized to receive sofosbuvir and daclatasvir with or without ribavirin for 24 weeks. Except for one patient who missed his post-treatment week 12 visit, all patients achieved SVR12. The missing patient achieved SVR24 [28]. This study is an extremely important proof of principle because it is the first study to look at re-treatment with DAAs for patients who previously failed protease inhibitors. Despite only including 41 patients, it suggests that failing one class of agent does not preclude treatment with other classes.
Like the AI444-040 study, the ELECTRON study presented above was later amended to add arms combining sofosbuvir and ribavirin with the NS5A inhibitor ledipasvir [29]. After 12 weeks of treatment, all 25 naive patients and ten null responders achieved SVR12 [29]. Two other arms changed ledipasvir for the non-nucleoside NS5B inhibitor GS-9669. The SVR12 rate of naives was 92 %. For the null responders, all patients achieved SVR4, but results are still pending for SVR12 [29]. The combination of sofosbuvir and ledipasvir is now in phase III trials.
The COSMOS study was also a collaborative effort between Janssen Pharmaceuticals, Inc. and Gilead Sciences. The study combined simeprevir and sofosbuvir with and without ribavirin for 12 or 24 weeks in genotype 1 prior null responders to PEG-IFN/ribavirin and with stage F0–F2 on biopsy [15]. Only preliminary results are available so far. SVR8 rates in the 12-week arms were 96 and 93 % with and without ribavirin, respectively [15]. Simeprevir and sofosbuvir NDAs have both been submitted, and the launch of these drugs may happen by the end of 2013 [10, 30]. Clinicians may then be tempted to order this off-label combination, but the results presented thus far from the COSMOS study are preliminary and only exist for 41 patients [15].
While most drug combinations have usually contained one or two DAAs with or without ribavirin, some regimens include up to four or five drugs. AVIATOR is the most advanced study for which data are available, combining three DAAs and ribavirin [31]. It tested different drug combinations, dosing, and treatment durations for ABT-450/r, ABT-333, ABT-267, and ribavirin in naives and previous null responders. It achieved SVR12 in 85–99 % of naive patients and 89–98 % of previous null responders [31]. Of note, this study was preceded by two smaller studies, PILOT and CO-PILOT. PILOT combined ABT-450/r, ABT-072, and ribavirin and was restricted to genotype 1 naive patients with an IL28B CC genotype [32]. Although the SVR rate was 91 %, the study is mostly known to have reported a late relapse (36 weeks post-treatment). The patient demonstrated a polymerase mutation (Y448H) consistent with resistance to ABT-333 [32]. CO-PILOT reported excellent SVR rates for naive patients (93–95 %) but poor rates for previous non-responders (47 %) while combining ABT-450/r, ABT-333, and ribavirin [24]. The M12-998 study was for genotype 1, 2, or 3 naive patients without cirrhosis. Patients were treated for 12 weeks with ABT-450/r and ABT-267 with and without ribavirin [33]. Like in the Gilead trials, response rates for genotype 3 patients were lower than for genotype 1 patients (arms with ribavirin 100, 80, 50 % for genotype 1, 2, and 3, respectively). Response rates were also lower in the arms without ribavirin (60, 60, and 10 % for genotype 1, 2, and 3) [33].
6 Specific Situations
6.1 Fibrosis and Previous Treatment Response
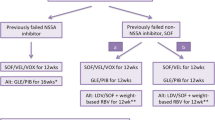
The impact of the number and class of agents combined and the HCV genotype/subtype on SVR rates has been discussed above, but several other factors play a critical role. Cirrhosis clearly predicted a worse prognosis in PEG-IFN-based regimens. Few studies so far have allowed cirrhotic patients and, when included, these patients were under-represented: 10 % in QUANTUM and SOUND-C2 and 20–30 % in the genotype 2–3 sofosbuvir studies [6, 14, 21, 25]. Conclusions cannot be drawn from QUANTUM and SOUND-C2, as the sample size of cirrhotic patients was too small and data were not broken down [14, 25]; however, the negative impact of cirrhosis was clear from FUSION, FISSION, and POSITRON [6, 21]. In the 12-week arm of FUSION, SVR12 rates were 61 % among patients without cirrhosis versus 31 % in those with cirrhosis [6]. Hopefully, increasing the treatment duration to 16 weeks may partly overcome this effect (76 versus 66 % for patients without and with cirrhosis, respectively) [6].
When potent combinations are used, the impact of previous treatment response with IFN-based treatment on IFN-free regimens is less significant. This was well illustrated by the AVIATOR and ELECTRON (ledipasvir arm) studies, and the daclatasvir/asunaprevir studies, where previous null responders achieved SVR rates over 90 % [18, 29, 31]. Similarly, the IL28B polymorphism has less influence on IFN-free combinations although an effect on SVR rates has been detected in some studies [6, 14, 20, 21].
6.2 HIV/Hepatitis C Virus Co-Infected Patients
DAA studies focusing on HIV/HCV co-infected patients are progressing at a much slower pace than studies for HCV mono-infected patients. So far, the only studies for which SVR12 has been presented are the phase II trials for telaprevir and boceprevir [34, 35]. Preliminary SVR12 results for simeprevir were also presented at CROI 2013, whereas on-treatment responses were presented for faldaprevir [36, 37]. These studies combined the protease inhibitors with PEG-IFN and ribavirin. As opposed to lower rates of SVR seen in co-infected patients treated with PEG-IFN and ribavirin, these studies all demonstrated results very similar to those seen in mono-infected patients. In this context, IFN-free regimens may be expected to be effective in co-infected patients, but future studies will be required. Two phase III trials combining sofosbuvir with ribavirin in co-infected patients are currently on-going (NCT01667731 and NCT01783678) [26]. The biggest challenge for treatment of HIV/HCV co-infected patients will be the management of drug–drug interactions. The addition of telaprevir or boceprevir to PEG-IFN and ribavirin has already significantly limited the compatible anti-retrovirals that can be used [38]. With the use of more than one DAA in some combinations, this situation is likely to become a real puzzle and will require strong two-way communication between liver and HIV providers.
6.3 Post-Liver Transplant Patients
The use of IFN is contraindicated post-transplant for most organs except the liver. In liver transplant patients, it can be used with caution in the case of recurrent HCV, but the side effects are significant and success rates are disappointing [39]. DAAs are expected to improve both the safety profile and the rate of SVR; however, similar to observations in HIV-infected patients, drug–drug interactions, especially with calcineurin inhibitors, will be an issue with post-transplant patients and will require careful evaluation. Fontana et al. [39] recently published the first case of IFN-free treatment in a patient with a severe cholestatic HCV recurrence post-transplant. The patient was treated with 24 weeks of sofosbuvir and daclatasvir and achieved SVR36. He did not experience any adverse events on treatment [39]. Studies are currently on-going with sofosbuvir and ribavirin in post-transplant patients with recurrent HCV (NCT01687270) and in pre-transplant patients in order to avoid infection of the transplanted liver (NCT01559844) [26].
7 Conclusion
The pace of development of IFN-free therapies is extremely fast and the first regimen is likely to be approved by the end of 2013 for patients with genotype 2 or 3. Many others will undoubtedly follow, as soon as 2014. The majority of patients will likely be able to achieve SVR with IFN-sparing regimens, but this may not be the case for all patients. Genotypes 1a and 3 seem more difficult to treat with these regimens than the other genotypes, and information is still scant for genotypes 4–6, with only a handful of patients included in QUANTUM. Patients with cirrhosis, as seen in IFN-based regimens, still have lower SVR rates than patients with less advanced fibrosis. New multi-drug combinations may become a solution for patients who have previously failed IFN or even telaprevir or boceprevir, but issues of drug–drug interactions may still arise. Additionally, if patients failing one class of DAA may be treated with another class, treatment options for patients failing a regimen with more than one class are likely to be limited. Resistance testing has not played a major role in treatment decisions for HCV so far, but it may eventually become essential in these patients. Finally, IFN-free regimens may be expensive, and access to treatment may become an important issue, although treatment of HCV is well known to be extremely cost effective because of the consequences of un-treated HCV [40, 41].
References
Hepatitis C. 2013. http://www.who.int/mediacentre/factsheets/fs164/en/ (Accessed 15 Sep 2013).
Hoofnagle JH, Mullen KD, Jones DB, Rustgi V, Di Bisceglie A, Peters M, et al. Treatment of chronic non-A, non-B hepatitis with recombinant human alpha interferon. A preliminary report. N Engl J Med. 1986;315(25):1575–8. doi:10.1056/NEJM198612183152503.
Minami T, Kishikawa T, Sato M, Tateishi R, Yoshida H, Koike K. Meta-analysis: mortality and serious adverse events of peginterferon plus ribavirin therapy for chronic hepatitis C. J Gastroenterol. 2013;48(2):254–68. doi:10.1007/s00535-012-0631-y.
Fusfeld L, Aggarwal J, Dougher C, Vera-Llonch M, Bubb S, Donepudi M, et al. Assessment of motivating factors associated with the initiation and completion of treatment for chronic hepatitis C virus (HCV) infection. BMC Infect Dis. 2013;13(1):234. doi:10.1186/1471-2334-13-234.
Chen EY, Sclair SN, Czul F, Apica B, Dubin P, Martin P, et al. A small percentage of patients with hepatitis C receive triple therapy with boceprevir or telaprevir. Clin Gastroenterol Hepatol. 2013. doi:10.1016/j.cgh.2013.03.032.
Jacobson IM, Gordon SC, Kowdley KV, Yoshida EM, Rodriguez-Torres M, Sulkowski MS, et al. Sofosbuvir for hepatitis C genotype 2 or 3 in patients without treatment options. N Engl J Med. 2013;368(20):1867–77. doi:10.1056/NEJMoa1214854.
Jacobson IM, McHutchison JG, Dusheiko G, Di Bisceglie AM, Reddy KR, Bzowej NH, et al. Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med. 2011;364(25):2405–16. doi:10.1056/NEJMoa1012912.
Poordad F, McCone J Jr, Bacon BR, Bruno S, Manns MP, Sulkowski MS, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364(13):1195–206. doi:10.1056/NEJMoa1010494.
Ge D, Fellay J, Thompson AJ, Simon JS, Shianna KV, Urban TJ, et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature. 2009;461(7262):399–401. doi:10.1038/nature08309.
Gilead Submits New Drug Application to U.S. FDA for Sofosbuvir for the Treatment of Hepatitis C. 2013. http://www.gilead.com/news/press-releases/2013/4/gilead-submits-new-drug-application-to-us-fda-for-sofosbuvir-for-the-treatment-of-hepatitis-c (Accessed 10 June 2013).
Zeuzem S, Andreone P, Pol S, Lawitz E, Diago M, Roberts S, et al. Telaprevir for retreatment of HCV infection. N Engl J Med. 2011;364(25):2417–28. doi:10.1056/NEJMoa1013086.
Bacon BR, Gordon SC, Lawitz E, Marcellin P, Vierling JM, Zeuzem S, et al. Boceprevir for previously treated chronic HCV genotype 1 infection. N Engl J Med. 2011;364(13):1207–17. doi:10.1056/NEJMoa1009482.
Zeuzem S, Dufour J, Buti M, Soriano V, Buynak R, Mantry P, et al. Interferon-free treatment with faldaprevir, BI207127 and ribavirin in SOUND-C3: 95% SVR12 in HCV-GT1b. Hepatol Int. 2013;7(Suppl 1):S445–6.
Zeuzem S, Soriano V, Asselah T, Bronowicki J, Lohse B, Müllhaupt B, et al. SVR4 and SVR12 with an interferon-free regimen of BI201335 and BI207127, +/− ribavirin, in treatment-naive patients with chronic genotype-1 HCV infection: interim results of SOUND-C2. J Hepatol. 2012;56(Supplement 2):S45.
Lawitz E, Ghalib R, Rodriguez-Torres M, Younossi Z, Corregidor A, Jacobson I, et al. COSMOS Study: SVR4 results of a once daily regimen of simeprevir (TMC435) plus sofosbuvir (GS-7977) with or without ribavirin in HCV genotype 1 null responders. 20th Conference on Retroviruses and Opportunistic Infections (CROI); Atlanta; 2013.
Nettles RE, Gao M, Bifano M, Chung E, Persson A, Marbury TC, et al. Multiple ascending dose study of BMS-790052, a nonstructural protein 5A replication complex inhibitor, in patients infected with hepatitis C virus genotype 1. Hepatology. 2011;54(6):1956–65. doi:10.1002/hep.24609.
Lok AS, Gardiner DF, Lawitz E, Martorell C, Everson GT, Ghalib R, et al. Preliminary study of two antiviral agents for hepatitis C genotype 1. N Engl J Med. 2012;366(3):216–24. doi:10.1056/NEJMoa1104430.
Suzuki Y, Ikeda K, Suzuki F, Toyota J, Karino Y, Chayama K, et al. Dual oral therapy with daclatasvir and asunaprevir for patients with HCV genotype 1b infection and limited treatment options. J Hepatol. 2013;58(4):655–62. doi:10.1016/j.jhep.2012.09.037.
Everson GT, Lawitz E, Thompson AJ, Sulkowski MS, Zhu Y, Brainard DM, et al. The NS5A inhibitor GS-5885 is safe and well-tolerated in over 1000 patients treated in phase 2 studies. Hepatology. 2012;56(S1).
Gane E, Pockros S, Zeuzem S, Marcellin P, Shikhman A, Bernaards C, et al. Interferon-free treatment with a combination of mericitabine and danoprevir/r with or without ribavirin in treatment-naive HCV genotype 1-infected patients. J Hepatol. 2012;56(Supplement 2):S555–6.
Lawitz E, Mangia A, Wyles D, Rodriguez-Torres M, Hassanein T, Gordon SC, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368(20):1878–87. doi:10.1056/NEJMoa1214853.
Gane EJ, Stedman CA, Hyland RH, Ding X, Svarovskaia E, Symonds WT, et al. Nucleotide polymerase inhibitor sofosbuvir plus ribavirin for hepatitis C. N Engl J Med. 2013;368(1):34–44. doi:10.1056/NEJMoa1208953.
Jacobson I, Jensen D, Pol S, Foster G, Feld J, Yoshida E, et al. Safety and efficacy of ritonavir-boosted danoprevir (DNVr), peginterferon α-2a (40KD) (P) and ribavirin (R) with or without mericitabine in HCV genotype (G)1-infected treatment-experienced patients with advanced hepatic fibrosis. Hepatology. 2012;56(S1):232A.
Poordad F, Lawitz E, Kowdley G, Everson G, Freilich B, Cohen D, et al. 12-week interferon-free regimen of ABT-450/r + ABT-333 + ribavirin achieved SVR12 in more than 90% of treatment-naive HCV genotype-1-infected subjects and 47% of previous non-responders. J Hepatol. 2012;56(Supplement 2):S549–50.
Lalezari J, Nelson D, Hyland R, Lin M, Rossi S, Symonds W, et al. Once-daily sofosbuvir plus ribavirin given for 12 or 24 weeks in treatment-naïve patients with HCV infection: the QUANTUM study. J Hepatol. 2013;58(Supplement 1):S346.
http://www.clincaltrials.gov (Accessed 8 June 2013).
Sulkowski M, Gardiner D, Rodriguez-Torres M, Reddy K, Hassanein T, Jacobson I, et al. High rate of sustained virologic response with the all-oral combination of daclatasvir (NS5A inhibitor) plus sofosbuvir (nucleotide NS5B inhibitor), with or without ribavirin, in treatment-naive patients chronically infected with HCV genotype 1, 2, or 3. Hepatology. 2012;56(S1):1516–7.
Sulkowski M, Gardiner D, Rodriguez-Torres M, Reddy K, Hassanein T, Jacobson I, et al. Sustained virologic response with daclatasvir plus sofosbuvir ± ribavirin (RBV) in chronic HCV genotype (GT) 1-infected patients who previously failed telaprevir (TVR) or boceprevir (BOC). J Hepatol. 2013;58(Supplement 1):S570.
Gane E, Stedman C, Hyland R, Pang P, Ding X, Symonds W, et al. All-oral sofosbuvir-based 12-week regimens for the treatment of chronic HCV infection: the ELECTRON study. J Hepatol. 2013;58(Supplement 1):S6–7.
New Drug Application has been filed with FDA for Simeprevir (TMC435) for combination treatment of adult patients with genotype 1 chronic hepatitis C; 2013. http://www.medivir.se/v5/en/uptodate/pressrelease.cfm?year=2013&releaseid=758336 (Accessed 27 June 2013).
Kowdley K, Lawitz E, Poordad F, Cohen D, Nelson D, Zeuzem S, et al. Safety and efficacy of interferon-free regimens of ABT-450/r, ABT-267, ABT-333 +/− ribavirin in patients with chronic HCV GT1 infection: results from the AVIATOR study. J Hepatol. 2013;58(Supplement 1):S2.
Lawitz E, Poordad F, Kowdley KV, Cohen DE, Podsadecki T, Siggelkow S, et al. A phase 2a trial of 12-week interferon-free therapy with two direct-acting antivirals (ABT-450/r, ABT-072) and ribavirin in IL28B C/C patients with chronic hepatitis C genotype 1. J Hepatol. 2013. doi:10.1016/j.jhep.2013.02.009.
Lawitz E, Sullivan G, Rodriguez-Torres M, Enayati P, Bennett M, Poordad F, et al. A 12-week trial of interferon-free regimens containing ABT-450/r and ABT-267 +/- ribavirin (RBV) in treatment-naïve patients with HCV genotypes 1-3. Hepatol Int. 2013;7(Suppl 1):S358–9.
Sulkowski MS, Sherman KE, Dieterich DT, Bsharat M, Mahnke L, Rockstroh JK, et al. Combination therapy with telaprevir for chronic hepatitis C virus genotype 1 infection in patients with HIV: a randomized trial. Ann Int Med. 2013. doi:10.7326/0003-4819-159-2-201307160-00654.
Sulkowski M, Pol S, Mallolas J, Fainboim H, Cooper C, Slim J, et al. Boceprevir versus placebo with pegylated interferon alfa-2b and ribavirin for treatment of hepatitis C virus genotype 1 in patients with HIV: a randomised, double-blind, controlled phase 2 trial. Lancet Infect Dis. 2013. doi:10.1016/S1473-3099(13)70149-X.
Dieterich D, Rockstroh J, Orkin C, Gutierrez F, Klein M, Reynes J, et al. Simeprevir (TMC435) with peginterferon/ribavirin in patients co-infected with chronic genotype-1 HCV and HIV-1: week-24 interim analysis of the TMC435-C212 study. 20th Conference on Retroviruses and Opportunistic Infections (CROI); Atlanta; 2013.
Dieterich D, Soriano S, Nelson M, Rockstroh J, Arasteh K, Bhagani S, et al. STARTVerso 4: High rates of early virologic response in HCV genotype 1/HIV-co-infected patients treated with faldaprevir plus pegIFN and RBV. 20th Conference on Retroviruses and Opportunistic Infections (CROI); Atlanta; 2013.
Sulkowski MS. Current management of hepatitis C virus infection in patients with HIV co-infection. J Infect Dis. 2013;207(Suppl 1):S26–32. doi:10.1093/infdis/jis764.
Fontana RJ, Hughes EA, Bifano M, Appelman H, Dimitrova D, Hindes R, et al. Sofosbuvir and daclatasvir combination therapy in a liver transplant recipient with severe recurrent cholestatic hepatitis C. Am J Transplant. 2013;13(6):1601-5. doi:10.1111/ajt.12209.
Camma C, Petta S, Cabibbo G, Ruggeri M, Enea M, Bruno R, et al. Cost-effectiveness of boceprevir or telaprevir for previously treated patients with genotype 1 chronic hepatitis C. J Hepatol. 2013. doi:10.1016/j.jhep.2013.05.019.
Camma C, Petta S, Enea M, Bruno R, Bronte F, Capursi V, et al. Cost-effectiveness of boceprevir or telaprevir for untreated patients with genotype 1 chronic hepatitis C. Hepatology. 2012;56(3):850–60. doi:10.1002/hep.25734.
Acknowledgments
Valérie Martel-Laferrière was funded by the 2012 Grant of the CHUM Foundation.
Disclosures
Valérie Martel-Laferrière and Kian Bichoupan declare no relevant conflicts of interest. Douglas T. Dieterich serves as a paid lecturer, consultant, and is a member on scientific advisory boards of companies that either develop or assess medicines used for the treatment of viral hepatitis. These companies include Gilead Sciences, Boehringer Ingelheim, Novartis, Vertex Pharmaceuticals, Achillion, Tibotec, Idenix, Merck, Kadmon, Bayer Healthcare, Roche/Genentech, and Bristol-Myers Squibb.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martel-Laferrière, V., Bichoupan, K. & Dieterich, D.T. Interferon-Free Regimens for Hepatitis C: Combine and Conquer. BioDrugs 28, 161–169 (2014). https://doi.org/10.1007/s40259-013-0072-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-013-0072-z