Abstract
We present a critical review of the literature that discusses the link between the level of out-of-pocket payments in developed countries and the share of people in these countries reporting that they postpone or forgo healthcare for financial reasons. We discuss the pros and cons of measuring access problems with this subjective variable. Whereas the quantitative findings in terms of numbers of people postponing care must be interpreted with utmost caution, the picture for the vulnerable groups in society is reasonably robust and unsurprising: people with low incomes and high morbidity and incomplete (or non-existent) insurance coverage are most likely to postpone or forgo healthcare for financial reasons. It is more surprising that people with high incomes and generous insurance coverage also report that they postpone care. We focus on some policy-relevant issues that call for further research: the subtle interactions between financial and non-financial factors, the possibility of differentiation of out-of-pocket payments between patients and between healthcare services, and the normative debate around accessibility and affordability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Subjective measures of unmet need show that out-of-pocket payments create financial barriers to healthcare. Social protection of vulnerable groups within the healthcare system must be complemented by broader social policies aiming to improve the economic situation of the poor. |
Policy makers should take into account the subtle interactions between financial and non-financial factors and consider the possibility of differentiation of out-of-pocket payments between patients and between healthcare services. |
Policy makers should also consider the social determination of perceived healthcare needs and distinguish between, on the one hand, limited healthcare use that reflects social constraints and problems of affordability and, on the other hand, limited healthcare use that can be seen as a free choice. |
1 Introduction
Healthcare access is one of the main goals of governments. It is a complex phenomenon, with multiple determinants of who ultimately uses health services and how satisfied these users are. One possible measure of access is to directly question citizens about their postponement of healthcare: given characteristics of the patients and of the health delivery system (organization of healthcare coverage, cost sharing, waiting times, regional distribution and transportation time, quality of care), was there a time when the consumer thought she/he needed a medical intervention but did not receive it or had to postpone it? We summarize this variable as ‘subjective unmet need’ (SUN). It is linked to consumer satisfaction and can therefore be viewed as an outcome indicator.
Many surveys have introduced subjective indicators of postponing or forgoing needed healthcare and have related it to different causes [2, 13,14,15, 39]. One of the main factors contributing to this postponement is the amount patients pay out of pocket (OOP) at their point of access to the system: doctors’ fees, cost of medicines or glasses, hospital bills [13]. We present a critical review of the literature on the impact of OOP payments on subjective unmet healthcare needs.
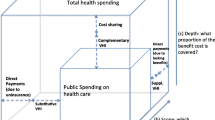
We use OOP payments as a general term covering different phenomena that all relate to what patients must pay at the point of service [1]. In tax-financed systems, the common term is user charges. In insurance systems, the same concept is denoted by co-payments or co-insurance. Deductibles can also be seen as OOP payments, since they imply that patients must pay the full price of the service as long as their expenditures do not reach the threshold amount. Moreover, on top of the official prices, i.e. user charges or co-payments, providers can charge an additional amount to patients, called supplements, balance billing or extra billing. In some countries, informal payments are also an important part of OOP payments [58,59,60,61,62]. Finally, both in tax-financed and in insurance systems, some health-related services are not covered, dental care being a prime example in many countries. Again, patients needing these forms of care must pay for them out of their own pocket. All these different forms of OOP payments have their own specific explanations, their own place in the institutional framework of the healthcare system and their own specific effects. However, from the patient’s viewpoint, what really matters is the combination of all of them: this determines the (financial) price she/he must pay. We therefore focus on overall OOP payments.
OOP payments are often justified by the assumption that they mitigate the problem of moral hazard [63, 64]. This potential advantage must be traded off against the resulting undesirable social effects, interpreted alternatively as a decrease in the insurance protection or as an increase in the inequity of the system. Again, the latter has different aspects. If the price per treatment is not differentiated according to income, OOP payments are a regressive source of healthcare financing even if healthcare needs are equally distributed over all income groups, and a fortiori under the more realistic assumption that poorer individuals have larger healthcare needs [1, 65,66,67]. Potentially even more worrisome is that individuals would forego needed care because they cannot afford to pay its price. This is a direct threat to the ideal of ‘equality of access’. We focus on this latter aspect. A more complete survey of the effects of user charges can be found in Schokkaert and Van de Voorde [1].
In the next section, we discuss the pros and cons of measuring access problems with the subjective variable SUN. The third section presents the main findings linking SUN to OOP payments. Non-financial factors are also important to explain SUN, and we argue in the fourth section that subtle interactions may exist between financial and non-financial factors. The final section concludes and discusses some policy implications.
It should be clear that it is not the aim of this short paper to offer a systematic review of the huge literature on the equity effects of OOP payments. We deliberately restrict ourselves to the effects on SUN, and we try to show what can be learnt (or not be learnt) from the use of this subjective variable. Moreover—largely due to the available results on SUN—we only cover the situation in rich Western countries. We focus on some main insights and on remaining open questions and avenues for further research that we consider to be both scientifically and politically relevant.
2 Subjective Unmet Need as an Indicator of Access Problems
There are clear arguments in favour of using SUN as an indicator of access problems. First, it is not easy to measure the degree of equality of access on the basis of utilization data. Indeed, forgone healthcare is, by definition, unobserved. The economic literature [57] measures socioeconomic inequality in healthcare use, with concentration indices taking into account a correction for ‘needs’, but these needs are usually only measured in an approximate way on the basis of easily observed variables such as age and sex. This may be sufficient to measure inequity at an aggregate level, but it is not sufficient to analyse specific access problems that are related to specific OOP payments. Moreover, nor are differences in quality of treatment observed, as they will not be reflected in utilization measures [2]. Individuals may get an expensive treatment but still (have the feeling that they) are inadequately treated. Patient needs and differences in treatment quality can in some cases be better measured with subjective variables.
Second, subjective indicators are directly related to the satisfaction of the population with the quantity, effectiveness or quality of care received [2]. This subjective satisfaction is a useful indicator of the quality of the relationship of the population with the healthcare system. This can be seen as a value in itself—there is a welfare loss if the presence of OOP payments lowers satisfaction of the population and inequity if this effect on satisfaction differs for different socioeconomic groups.
Third, the results for SUN can offer us a richer picture of the different facets of access problems. People may have financial problems because they have large non-healthcare costs related to their health problems. On the other hand, they may also forgo or postpone needed care because they place relatively little value on health (care) and prefer to spend their income otherwise. In the latter case, one can wonder whether there is any inequity attached to the differences in utilization of different social groups. These factors lead us beyond a consideration of OOP payments in the narrow sense, but there may be important interactions between OOP payments and these other factors.
Fourth, there is a simple pragmatic argument. It is rather easy to collect data on SUN, including for specific small groups of the population and for specific types of healthcare. This may explain why there is such an abundance of data on SUN, at least in high-income countries.
In spite of the clear advantages attached to the use of subjective measures, they also have their drawbacks. First, the results may heavily depend on the design of the questionnaire and the formulation of the question. Legal and Vicard [3] show this convincingly for the postponement of healthcare in a split sample study. Their results are summarized in Table 1. Differences in the formulation of the question may lead to differences of up to 15% in the shares of respondents reporting having postponed healthcare. Adding a filter question (to which respondents must reply positively before they are asked about their reason for postponement of healthcare) or making the question less direct (for instance, by not explicitly mentioning the type of care that is ‘postponed’) reduces considerably the number of respondents who state they have postponed healthcare, other things equal. Given that different formulations of this indicator are used in different surveys even for the same country, and some surveys change the formulation of the question across time, great care must be taken when interpreting the results on the numbers of respondents postponing care. As an example, self-reported unmet need is included in the EU Survey of Income and Living Conditions (EU-SILC), which is aimed at residents in private households aged ≥16 years. The EU-SILC applies a filter: after inquiring whether the respondent postponed healthcare (only medical or dental), she/he is asked in a second stage to indicate the reason(s) for postponement. Perfectly in line with the findings of Legal and Vicard [3], the share of respondents in EU-SILC who report having postponed care is rather low. For Belgium in 2008, the EU-SILC reported that 0.75% of the population postponed healthcare for financial reasons. The Belgian Health Interview Survey, which does not apply a filter, reported for the same year that 12.3% of the population postponed care. Other examples can be given, and it seems fair to conclude that level comparisons over time and between countries are often, if not always, unreliable.
In fact, the specific perception of the questions may also influence respondents’ answers. Some (French) authors point to the polysemy of ‘postponing’, which may lead to interpretational problems if different respondents have a distinct understanding of the concept. In a qualitative study [4], the French word ‘renoncer’ (semantically close to the English word ‘renounce’) was linked by some respondents to a moral–religious context (renoncer à Satan) or seen as necessarily involving choice. In the latter case, individuals argued that when you are not financially capable of getting care, there is no choice and hence no ‘renouncing of care’. Similar interpretational issues are likely to arise in other languages.
However, these problems should not be used to sketch a picture of total disaster. Despite the huge differences in Table 1 following from different formulations of the question, Legal and Vicard [3] detected a robust pattern of inter-individual differences in their data: neither the sociodemographic determinants of postponing healthcare nor the ranking of which kind of care was most frequently postponed depend on the formulation of the question. This implies that one can identify vulnerable groups that are more susceptible to postponing healthcare and identify the types of care for which the problems are most acute. Comparisons of levels should be treated with utmost caution, but differences within a country and within a specific survey are reasonably robust.
This cautious attitude does not solve all problems. Indeed, the importance of psychological and cultural factors goes beyond the influence of the specific formulation of the questions. Reports of SUN will also capture expectations and attitudes towards health and healthcare [4, 51]. These may differ between individuals in different countries as well as between different cultural groups within a country. Expectations with respect to the healthcare system differ, and the same is true for the subjective perception of healthcare needs. ‘Real’ unmet need may be under-reported in the surveys when respondents are unaware of their health problems, and this informational issue may alter for different social and cultural groups. In some cases, the ‘need’ itself is co-determined by cultural factors, screening and dental care being obvious examples (to which we will return). Such cultural differences may lead to biased estimates of inequity or inequality of access and to biased estimates of the effects of OOP payments. As such, all this is not a criticism on the use of SUN. It can equally well be seen as an opportunity for a richer analysis taking up these cultural and psychological phenomena. Yet, it is beyond doubt that caution is needed.
However, with due caution, we believe it is still useful to analyse the effects of OOP payments on healthcare utilization on the basis of a subjective SUN measure. Of course, it is obvious that such an analysis is not a substitute for but rather a complement to a more traditional analysis making use of utilization data.
3 Subjective Unmet Need and Out-of-Pocket Payments
As mentioned, studies on SUN have produced a wide range of numbers for the share of people postponing or forgoing healthcare in different countries and even within a country. Yet, the overall picture coming out of the reviewed literature is clear. OOP payments play a basic role in explaining the degree of SUN in a country, and they also contribute to explaining inter-country differences. To some extent, this is a rather trivial finding. Unmet need for financial reasons can only occur if (1) there is a perceived need and (2) people forgo care because the OOP payment associated with taking up care are seen as representing a too large share in the household budget; this will depend both on the amount of OOP payment and on the size of that budget. The interaction between needs, OOP payments and financial position of the household determines whether there will be SUN, with the important proviso that each of these are influenced by the subjective perception of the respondents.
Striking results are found for the USA, in which individuals who lack insurance coverage tend to postpone healthcare (medical as well as dental care) because of cost more often than insured individuals [5,6,7,8,9,10,11]. The literature also shows that charity care is not an adequate substitute for insurance coverage [6, 7]. Since charity care involves a strong decrease in OOP payments, this suggests that non-financial factors play an important role in SUN. We return to that finding in the following section.
If health insurance is not compulsory, caution is needed in interpreting these results, since there may be a selection issue if taking up health insurance is to some extent a choice. In this respect, Reschovsky et al. [12] made the interesting observation that the type of private insurance affects the use of health services and the (reasons for) unmet needs in a managed care environment. Unmet need (or delayed care) due to cost was significantly lower among people enrolled in health maintenance organizations (HMOs) than among those enrolled in preferred provider organizations (PPOs) and indemnity insurance. On the other hand, HMO enrolees were more likely to perceive problems in provider access. If choosing one’s type of insurance is within one’s own responsibility, this raises questions about how to define ‘equality of access’. We discuss this issue in the following section. In a more recent cross-sectional study, Hong et al. [8] tried to assess the possibly diverse impact of the Affordable Care Act on differently insured individuals. They found that publicly insured people had poorer physical and mental health conditions than uninsured individuals (eligible for Medicaid or for purchasing health plans through the health insurance exchanges) but that the latter were more likely to report unmet healthcare needs. Reported needs may be subjective, and it is possible that uninsured individuals report fewer health problems because they have more undiagnosed health conditions because of restricted access, but the results nevertheless raise questions on the interpretation of ‘needs’ when talking about unmet needs.
The absence of health insurance is an extreme case of large OOP payments. In the less extreme case of countries with (almost) universal coverage (or of the insured individuals in the USA), OOP payments will have an influence on unmet need for individuals with high morbidity (and a high level of utilization of healthcare) if the insurance system reimburses only a fraction of a treatment or medicine. Taking due account of the caveats needed for international comparisons of the level of SUN, it is still interesting to note that the most important explanation for systematic differences in SUN between countries seems to be the share of OOP payments in total healthcare expenditure (with EU-SILC data [13, 14] and with SHARE data [15]). In fact, SUN due to financial reasons has also occurred in very rich countries (Sweden [16], Canada [17] and privately insured populations in the USA [18]) as soon as OOP payments started to increase.
Of course, to explain the occurrence of SUN, the level of OOP payments must be related to the overall budgetary situation of the household. It is mainly the poor who report postponing care in the case of large OOP payments. This implies that important interactions take place between different policy domains. In her analysis of the EU-SILC data for 2012, Israel [14] found not only that the share of OOP payments contributes to the explanation of differences in SUN between different countries but also that a generous system of social allowances has a negative effect on the share of SUN. External shocks to an economy, leading to a deterioration of the general economic situation, may worsen the problem of SUN, even if the rules with respect to OOP payments do not change. A recent example can be found in the effects of the financial crisis in Greece [19, 20]. This leads to the obvious but important policy conclusion that a policy meant to reduce access problems in healthcare should not be restricted to interventions in the insurance system itself but should incorporate broader social policy measures. This is even more important if one does not want to give up OOP payments as an instrument to fight moral hazard.
A specific issue arises if high non-healthcare costs that are caused by the health problems come on top of already high healthcare costs. The former will not appear as OOP payments in a model of healthcare utilization, but for the patients themselves they are definitely seen as health-related expenditures. The problem is especially acute for the chronically ill and for the disabled. As an example, Adams et al. [21] showed that costs related to house maintenance or preparing food constituted an important financial burden for the disabled in Flanders (the northern part of Belgium) and that the amount of these costs had an important influence on SUN for financial reasons.
The disabled are but one example of a vulnerable subgroup. A very large number of studies (mainly for the USA) have looked at the issue of SUN for other subgroups of the population. Many of these studies do not have a direct measure of OOP payments but use indirect measures of the different explanatory factors, such as having insurance or not (private, public or uninsured), utilization of health services (in most countries linked to higher OOP payments) or just a measure of income. The resulting pattern of what constitutes the most vulnerable groups remains remarkably robust. SUN is a more serious issue for the children of the poor (the reader is referred to a systematic review of the literature on children until 2006 [22] and some later studies [23,24,25,26,27,28,29]), for the homeless [30,31,32,33], for chronically ill patients [19, 20, 34,35,36], for the disabled [21, 37, 38], for the sick and poor elderly [39,40,41,42] and for immigrants [43]. Extending insurance coverage for these groups or strengthening social protection measures (lowering OOP payments or increasing their income) should be an obvious target for any policy aiming at improving equity of access.
The picture that has been sketched until now is pretty clear. A high level of OOP payments (in whatever form) can cause the problem of SUN, mainly among vulnerable groups with high morbidity and low incomes. This is an important finding, calling for an adequate social policy reaction that is often missing, but it is not very surprising from a scientific viewpoint. Yet, we certainly did not need data on SUN to derive this conclusion. However, some other findings in the literature on SUN do raise interesting research questions and policy challenges.
A first interesting finding can be derived from the paper by Cylus and Papanicolas [44]. These authors analysed data from the European Social Survey (ESS) for 2008. The question in the ESS differed from that in the other studies, since it captures the uncertainty of accessing healthcare in the next 12 months (not at all likely through to very likely of being able to access care). Yet, the findings described above are also replicated for this indicator: in a comparison between countries, the share of OOP payments in healthcare expenditures is a predictor of access problems, and a significant income effect usually exists within the countries. However, for our purposes, it is more interesting to look more closely at the countries that deviate from the general picture. Countries such as Ukraine, Latvia and Russia have high levels of perceived inability to access care but relatively small differences between individuals with low and high incomes. This may point to access problems unrelated to costs but, at the same time, OOP payments are also high and generally considered a barrier to access. The explanation is that OOP payments provide a way to bypass the difficulties of accessing the legal healthcare system through voluntary and informal payments. In Latvia, for instance, patients prefer to forgo a referral and thus pay higher OOP payments to avoid long waiting times. Therefore, large differences exist between the quality of care (including waiting times) for the poor and for the rich. As mentioned, this is the kind of phenomenon that can be better analysed with subjective measures than with official data on utilization of healthcare.
A second element worth noting is that, even in countries with (near) universal insurance and relatively low OOP payments, there remains a substantial fraction of the population that reports postponing or forgoing healthcare [13,14,15,16,17,18, 44]. The same is true in countries with relatively high OOP payments but an elaborate system of social protection for the poor, an example being Belgium, in which the total amount of co-payments is subject to an income-related cap [68]. A large share of the individuals with SUN are the very poor, and for them the explanation is not too difficult: even ‘relatively low’ OOP payments (or the income-related cap) can still be too high for them, or they may face liquidity problems if they first have to pay the full price of healthcare and are only reimbursed afterwards. Yet, SUN for financial reasons can also be found among middle- and high-income groups and there it is more difficult to explain. Two explanations can be proposed.
First, SUN can be caused by items that are not (fully) covered by the insurance system. These differ between countries, but the usual suspects are dental care, glasses, alternative medicine (homeopathy) and some forms of physiotherapy and mental healthcare. Moreover, items that are covered may incur an additional cost payable on top of the official fee, be it an informal payment or an official supplement. These forms of SUN will be difficult to discover with utilization data but are reflected in subjective measures. For governments confronted with a tight budget constraint in healthcare, this raises the question of the trade-off between the extent of coverage on the one hand, and the level of OOP payments on the other hand. Increasing OOP payments would increase the scope for extending the coverage; restricting the coverage makes it possible to lower the OOP payments for the services that are included.
More generally, this raises the issue of how to differentiate the OOP payments for different services. Smith [45] analysed this question for a decision maker that aims at maximizing health. He found that OOP payments should be lower for interventions with higher price elasticities of demand, mainly among the poor, and that are important in the consumption pattern of the poor. The first of these results is opposite to the traditional result in optimal health insurance that subsidizing healthcare services with a large price elasticity will have severe moral hazard effects. However, its rationale in terms of the objective of equity of access is easily understood: if the price elasticity of a service is large for the poor, this would imply that increasing OOP payments would deter the poor from taking up that service, and hence would lead to SUN.
Second, even fully covered healthcare items are, to some extent, postponed or forgone by insured individuals. This points to the importance of non-financial factors, such as information or trust in the system. At first sight, these non-financial factors may seem largely unrelated to the level of OOP payments. However, as we discuss in the next section, there are important interactions between financial and non-financial considerations.
4 Needs, Preferences, Trust and Information
4.1 The Interaction Between Financial and Non-Financial Factors
It is well-known that non-financial factors are important for explaining postponement or forgoing of healthcare. Leaving aside pure supply-side factors (such as the availability of services), many elements exist at the demand side: trust in healthcare providers, having a long-term relationship with a general practitioner, health beliefs and perceived needs are all codetermined by personal characteristics of the patients and by cultural factors. Personality factors such as self-esteem may also influence SUN [46]. Moreover, the relative social position of patients will have an influence on their personal interaction with the care providers, and this in turn may influence the type and quality of healthcare received [69]. It is obvious that any policy aiming at improving equity in access to healthcare will have to go beyond an OOP payment policy in the narrow sense.
Yet, it would be wrong to simply juxtapose financial and non-financial factors and neglect their interaction. There is a strong correlation between non-financial barriers to access and socioeconomic factors. For both, the overall economic situation of the patients is crucially important. Åhs and Westerling [47] showed that the problem of SUN in Sweden is particularly bad for the unemployed (worse than for those on long-term sick leave) and relate this to the psychological problems associated with unemployment. Other studies have emphasized the importance of the neighbourhood in which people are living, focusing on the level of social capital [48, 49], or point to the specific situation of the homeless [31, 33]. In all these cases, it is clear that just lowering OOP payments will be insufficient to solve the problem of SUN. Yet, there can be no doubt that increasing OOP payments would make the SUN issue more acute. This asymmetry can easily be understood when we reason in a broader economic model in which the ‘perceived price’ of healthcare not only consists of the monetary cost (the OOP payment) but also includes time and psychological costs. When the latter are high, SUN will occur, even if OOP payments are low, but this does not mean that OOP payments can be neglected. In fact, there is an almost perfect overlap between the financially vulnerable groups described in the previous section and the groups facing considerable non-financial barriers to healthcare. A policy aiming to improve access will necessarily have to be a coherent whole of financial and non-financial measures. Importantly, OOP payments will not only have direct financial effects, there may also be an indirect link going through the non-financial factors: raising OOP payments may negatively affect the trust in the system.
Mollborn et al. [50] illustrated how closely financial and non-financial factors may be intertwined in a large US sample of adults who usually see the same physician for their healthcare. They focussed on the effect of fiduciary trust in a physician and distinguished explicitly between different elements of SUN that we have mentioned: in their interpretation, people who do not postpone care can have their needs unmet if the care is of poor quality, whereas those who initially postpone care can eventually receive care that meets their needs. ‘Unmet needs’ and ‘delaying care’ capture two different realities. Mollborn et al. [50] indeed found a negative and statistically significant association between trust and ‘unmet needs’ for all advantaged and disadvantaged subpopulations (except the uninsured). However, while a negative relationship was found between trust and ‘delayed care’ for the advantaged subgroups, this relationship was not found among Blacks, Hispanics, the uninsured or the poor. All of these disadvantaged groups have a higher probability of delaying care, but this higher probability is not associated with a lower level of trust. It is as if ‘for disadvantaged patients, worrying about how much they trust their physicians when making healthcare decisions may be a luxury that they, unlike more advantaged groups, cannot afford’ [50]. We only present this study as one example, and its findings should not be oversold or uncritically extended to other settings. The limitation to respondents with a regular physician certainly introduces some selection bias. Our only point here is to emphasize that complicated interaction effects may exist between OOP payments and financial barriers to care at one side and non-financial demand side barriers at the other side. Again, subjective data are very useful, perhaps even necessary, to analyse these interactions.
The most important non-financial factor is probably the subjective perception and social determination of needs. Desprès [4] found in her qualitative interviews some clear results that are largely confirmed in the quantitative survey studies: less advantaged (lower educated) groups attach a lower weight to dental care but also to some preventive screening measures (such as mammography). They will therefore under-report SUN for these services. Another example is the study by Wiltshire et al. [51] comparing SUN for African American and White women in the USA. Overall, controlling for all other factors, ethnicity was not an important determinant of SUN. Yet, while the level of education did not affect the degree of SUN for White women, it had a strong effect for African American women: for them, higher educational attainment is associated with a higher probability of reporting unmet need. There are no good reasons to believe that this perception reflects differences in objective health problems. Use of the SUN indicator yields an insight that could not easily be obtained with utilization data: under-consumption of healthcare, as measured by these traditional economic approaches, may reflect biased needs perceptions by disadvantaged people.
Non-financial factors are an essential part of the picture if we want to understand the effects of OOP payments on (in)equity of access to healthcare. To some extent, they form barriers on top of the financial barriers formed by OOP payments. We have sketched some obvious interactions, but other less obvious links have remained underexplored in the actual research on the topic. First, consumer prices may act as an informational signal that goes beyond its narrow financial aspects. If the government decides to reimburse a given service (think about screening), this may be seen as an indication that the service is worthwhile. Second, beliefs and perceptions of needs may also be influenced by OOP payments. If a high level of OOP payment makes it impossible or difficult for some individuals to access care, their subjective experiences with the system will differ from those of individuals who do not face that barrier. Well-known mechanisms of cognitive dissonance or the fear of being stigmatized may contribute to the biased perception of needs. ‘If I do not go to the doctor (with my children), this is not because I cannot afford it or prefer to spend my money on other things, it is because there is no real problem.’ More explicit research on such subtle mechanisms would contribute to a more complete picture of the effects of OOP payments.
4.2 Equal Access and Affordability
There is an essential difference between equality of access and equality of (needs-corrected) utilization. Individuals may indeed postpone or forgo care if it is accessible for them. In so far as this reflects their well-informed free choice, one can wonder if there is inequity. The subtle ethical questions on the definition of ‘inequity’ (rather than inequality) in access are well illustrated by looking more carefully at four different groups of individuals. Again, SUN data offer additional information that can be used on top of more traditional utilization data.
A first group of individuals spends a large share of its budget on healthcare, even to such an extent that it must consume less of other necessary commodities. This group would not be picked up by the question about postponing healthcare for financial reasons (nor for that matter by utilization data), while many will agree that it would be fair to redistribute financial means to them to ensure equal access.
A second group would like to consume more healthcare but cannot at all afford to consume less of other products. These are the individuals who are likely to report financial access barriers as presumed in this paper. The co-existence of these two groups raises a major research question. ‘Financial’ indicators, focusing on catastrophic payments for healthcare [70,71,72,73], will capture the first group but not the second. SUN (and utilization) indicators capture the second group, but not the first. To get a coherent picture of the equity problems related to OOP payments, one would need to consider both groups, which seems to require the construction of a notion of well-being integrating health (care) and income (an example of such an approach can be found in Schokkaert et al. [52]).
A third group does consume healthcare but reports SUN because they are not satisfied by its quality or character. As mentioned, it may be seen as an advantage of SUN measures, in contrast to utilization data, that they can discern this kind of situation. However, it is also possible that individuals are dissatisfied, whereas the care they receive is adequate from a purely medical perspective. This raises the ethical issue of the weight to be attached to subjective satisfaction for the evaluation of equity. The answer to this is less straightforward than it may seem. Take an individual who has full access to the traditional healthcare system but prefers alternative medicine, which is not covered by insurance, and therefore reports SUN. Is this an example of inequity?
This brings us to the fourth group: individuals who could ‘afford’ to buy healthcare but systematically choose to consume other goods. If adherents to alternative medicine refuse traditional healthcare, they could also belong in this category. While these individuals may answer ‘yes’ on a question concerning postponement of healthcare, distributing resources to them seems less obvious from an equity perspective. This raises two issues. First, where to draw the boundary between what is ‘affordable’ and what is not? In principle, affordability should refer to the income situation of the individuals, but it is clear that the personal decisions on whether healthcare is affordable also reflect subjective preferences [53, 54]. If one takes the position that individuals are to be held responsible for their preferences but not for their economic situation, how then to empirically distinguish between the two? Second, should individuals really be held responsible for their preferences? It seems natural to accept that they should, if these preferences are authentic and well-informed, but when is this the case? Remember the results described earlier suggesting the strong social determination of subjective healthcare needs or the ethnic differences in trust in the healthcare system.
All these questions are crucial in every analysis of the equity of the financial barriers to access raised by OOP payments. If we see OOP payments as a consumer price, actual utilization will reflect both the income situation of the respondents and their preferences. As soon as we introduce some notion of personal responsibility and freedom in our ethical framework, the question of how to treat preference differences cannot be neglected [55].
This question gets a special twist when the policy maker wants to use differentiated OOP payments as an instrument to steer behaviour, as in the value-based design approach [56]. Behavioural reactions play an essential role here, and it is a priori uncertain that all groups in society have the same price elasticity. This will not always be the case [74, 75]; in some situations vulnerable groups may be more poorly informed or keep more to the status quo. It is then possible that value-based design improves the situation of the well-informed rich but worsens the situation of the less-informed poor. Should the latter be held responsible for their imperfect behavioural reactions?
5 Conclusions and Policy Implications
The literature shows unambiguously that there is a link between the level of OOP payments in a country and the share of people reporting that they postpone or forgo healthcare for financial reasons. This subjective indicator of inequity of access is sensitive to the precise formulation of the question, and the quantitative findings in terms of numbers of people postponing care must be interpreted cautiously. Yet, the picture regarding what are the vulnerable groups in society is reasonably robust: people with low incomes and high morbidity and incomplete (or non-existent) insurance coverage are most likely to postpone or forgo healthcare for financial reasons.
This result is not surprising, but the literature on OOP payments and SUN suggests some more interesting and policy relevant issues that call for further research. First, is the issue of differentiation of OOP payments between patients. Differentiation between individuals seems to necessitate that one has a clear idea about when healthcare is ‘affordable’ to different groups of individuals. The same applies to policies that put an income-related cap on OOP payments. Moreover, it would be misleading to think that problems of SUN due to financial barriers created by OOP payments can only be solved within the healthcare system itself. Social protection of vulnerable groups within the healthcare system must be complemented by broader social policies aimed at improving the economic situation of the poor.
Second, one can also consider differentiation of OOP payments between services. This raises the issue of the trade-off between the level of OOP payments on one hand and the extent of insurance coverage on the other. Moreover, when one aims at differentiating OOP payments to steer behaviour, one should investigate carefully whether different behavioural reactions by different social groups could raise a problem of inequity.
Third, equity of access is also influenced by many non-financial factors related to trust, confidence, social capital and information. There is a tendency to treat financial and non-financial factors as more or less independent. This is wrong; there are many interactions between the two. A coherent policy to improve equity of access to healthcare requires an integrated package of measures directed both at the level of OOP payments and at non-financial factors.
Fourth, all these points confront us with the broader question of how to define equity of access, taking into account personal responsibility. Surely it is difficult to say there is inequity of access if higher-income groups choose not to consume care, either because they prefer to spend their money on other commodities or because they reject traditional care and go for uncovered alternative medicine. Yet, the evidence about the social determination of healthcare needs and about the poor level of information of the socially vulnerable groups in society also suggests that ‘responsibility for revealed preferences’ must be interpreted cautiously. How do we define what are ‘authentic and well-informed’ preferences for which individuals should be held responsible?
Despite its problems, the analysis of SUN can yield interesting insights that could not easily be obtained with utilization data. They can inform us about possible causes or reasons for underutilization. SUN data may contribute to a better understanding of the broader social setting in which utilization decisions are taken, such as the presence (or not) of access barriers unrelated to costs or of non-healthcare costs associated with worse health. Most importantly, they help us to better understand the subtle differences between preferences and needs and they point to the social determinants of the subjective perception of needs. Biased needs perceptions will also influence objective care-seeking behaviour.
References
Schokkaert E, Van de Voorde C. User charges. In: Glied S, Smith P, editors. Oxford handbook on health economics. Oxford: Oxford University Press; 2011. p. 329–53.
Allin S, Grignon M, Le Grand J. Subjective unmet need and utilization of health care services in Canada: what are the equity implications? Soc Sci Med. 2010;70:465–72.
Legal R, Vicard A. Renoncement aux soins pour raisons financières. Doss Solidar Santé. 2015; 28.
Desprès C. Significations du renoncement aux soins: une analyse anthropologique. Sci Soc Santé. 2013;31:71–96.
Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–9.
Cunningham PJ, Kemper P. Ability to obtain medical care for the uninsured: how much does it vary across communities? JAMA. 1998;280:921–7.
Diamant AL, Hays RD, Morales LS, Ford W, et al. Delays and unmet need for health care among adult primary care patients in a restructured urban public health system. Am J Public Health. 2004;94:783–9.
Hong YR, Holcomb D, Bhandari M, Larkin L. Affordable care act: comparison of healthcare indicators among different insurance beneficiaries with new coverage eligibility. BMC Health Serv Res. 2016;16:114.
Malecki K, Wisk LE, Walsh M, McWilliams C, Eggers S, Olson M. Oral health equity and unmet dental care needs in a population-based sample: findings from the survey of the health of Wisconsin. Am J Public Health. 2015;105:S466–74.
Shi DL, Stevens GD. Vulnerability and unmet health care needs. J Gen Intern Med. 2005;20:148–54.
Strunk BC, Cunningham PJ. Treading Water: Americans’ Access to Needed Medical Care, 1997–2001. Tracking Report No. 1. Washington, DC: Center for Studying Health System Change; March 2002.
Reschovsky JD, Kemper P, Tu H. Does type of health insurance affect health care use and assessments of care among the privately insured? Health Serv Res. 2000;35:219–37.
Chaupain-Guillot S, Guillot O. Health system characteristics and unmet care needs in Europe: an analysis based on EU-SILC data. Eur J Health Econ. 2015;16:781–96.
Israel S. How social policies can improve financial accessibility of healthcare: a multi-level analysis of unmet medical need in European countries. Int J Equity Health. 2016;15:41.
Mielck A, Kiess R, von dem Knesebeck O, Stirbu I, Kunst AE. Association between forgone care and household income among the elderly in five Western European countries—analyses based on survey data from the SHARE-study. BMC Health Serv Res. 2009;9:52.
Elofsson S, Unden A-L, Krakau I. Patient charges: a hindrance to financially and psychosocially disadvantage groups seeking care. Soc Sci Med. 1998;46(10):1375–80.
Guend H, Tesseron A-L 2009. Unmet needs for primary care in the context of a universal healthcare system. The case of Québec. Centre—Urbanisation Culture Société (INRS) working paper no. 2009–04. Québec: INRS; 2009.
Himmelstein DU, Woolhandler S. Care denied: US residents who are unable to obtain needed medical services. Am J Public Health. 1995;85:341–4.
Kyriopoulos I-I, Zavras D, Skroumpelos A, Mylona K, Athanasakis K, Kyriopoulos J. Barriers in access to healthcare services for chronic patients in times of austerity: an empirical approach in Greece. Int J Equity Health. 2014;13:54.
Skroumpelos A, Pavi E, Mylona K, Kyriopoulos J. The impact of economic crisis on chronic patients’ self-rated health, health expenditures and health services utilization. Diseases. 2014;2(2):93–105. doi:10.3390/diseases2020093.
Adams M, Augustyns N, Janssens H, Vriesacker B, Van Hal G. What socio-demographic factors influence poverty and financial health care access among disabled people in Flanders: a cross-sectional study. Arch Public Health. 2014;72(1):5.
Skinner AC, Mayer ML. Effects of insurance status on children’s access to specialty care: a systematic review of the literature. BMC Health Serv Res. 2007;7:194.
Gnanasekaran SK, Boudreau AA, Soobader M-J, Yucel R, Hill K, Kuhlthau K. State policy environment and delayed or forgone care among children with special health care needs. Matern Child Health J. 2007;12:739–46.
Hill KS, Freeman LC, Yucel RM, Kuhlthau KA. Unmet need among children with special health care needs in Massachusetts. Matern Child Health J. 2007;12:650–61.
Kane DJ, Zotti ME, Rosenberg D. Factors associated with health care access for Mississippi children with special health care needs. Matern Child Health J. 2005;9:S23–31.
Lehrer JA, Pantell R, Tebb K, Shafer M-A. Forgone health care among U.S. adolescents: associations between risk characteristics and confidentiality concern. J Adolesc Health. 2007;40:218–26.
Lewis C, Robertson AS, Phelps S. Unmet dental care needs among children with special health care needs: implications for the medical home. Pediatrics. 2005;116:e426–31.
Tang MH, Hill KS, Boudreau AA, Yucel RM, Perrin JM, Kuhlthau KA. Medicaid managed care and the unmet need for mental health care among children with special health care needs. Health Serv Res. 2008;43:882–900.
Wisk LE, Witt WP. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 2012;130:1027–37.
Baggett TP, O’Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a National study. Am J Public Health. 2010;100:1326–33.
Hwang SW, Ueng JJM, Chiu S, Kiss A, Tolomiczenko G, Cowan L, Levinson W, Redelmeier DA. Universal health insurance and health care access for homeless persons. Am J Public Health. 2010;100:1454–61.
Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–6.
Lewis JH, Andersen RM, Gelberg L. Health care for homeless women. J Gen Intern Med. 2003;18:921–8.
Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically iii adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94:1782–7.
Ronksley PE, Sanmartin C, Quan H, Ravani P, Tonelli M, Manns B, Hemmelgarn BR. Association between chronic conditions and perceived unmet health care needs. Open Med. 2012;6:e48–58.
Ronksley PE, Sanmartin C, Quan H, Ravani P, Tonelli M, Manns B, Hemmelgarn BR. Association between perceived unmet health care needs and risk of adverse health outcomes among patients with chronic medical conditions. Open Med. 2013;7(1):e21–30.
Horner-Johnson W, Dobbertin K, Lee JC, Andresen EM, the Expert Panel on Disability and Health Disparities. Disparities in health care access and receipt of preventive services by disability type: analysis of the medical expenditure panel survey. Health Serv Res. 2014;49:1980–99.
Michalopoulos C, Wittenburg D, Israel DAR, Warren A. The effects of health care benefits on health care use and health: a randomized trial for disability insurance beneficiaries. Med Care. 2012;50:764–71.
Bremer P. Forgone care and financial burden due to out-of-pocket payments within the German health care system. Health Econ Rev. 2014;4(1):1–9.
Klein D, Turvey C, Wallace R. Elders who delay medication because of cost: health insurance, demographic, health, and financial correlates. Gerontologist. 2004;44:779–87.
Litwin H, Sapir EV. Forgone health care due to cost among older adults in European countries and in Israel. Eur J Ageing. 2009;6:167–76.
Rogowski J, Lillard LA, Kington R. The financial burden of prescription drug use among elderly persons. Gerontologist. 1997;37:475–82.
Lebrun LA, Dubay LC. Access to primary and preventive care among foreign-born adults in Canada and the United States. Health Serv Res. 2010;45:1693–719.
Cylus J, Papanicolas I. An analysis of perceived access to health care in Europe: how universal is universal coverage? Health Policy. 2015;119:1133–44.
Smith P. User charges and priority setting in health care: balancing equity and efficiency. J Health Econ. 2005;24(5):1018–29.
Bazin F, Parizot I, Chauvin P. Original approach to the individual characteristics associated with forgone healthcare. Eur J Public Health. 2005;15:361–7.
Åhs AMH, Westerling R. Health care utilization among persons who are unemployed or outside the labour force. Health Policy. 2006;78:178–93.
Hendryx MS, Ahern MM, Lovrich NP, McCurdy AH. Access to health care and community social capital. Health Serv Res. 2002;37:85–101.
Law M, Wilson K, Eyles J, Elliott S, Jerrett M, Moffat T, Luginaah I. Meeting health need, accessing health care: the role of neighbourhood. Health Place. 2005;11(4):367–77.
Mollborn S, Stepanikova I, Cook KS. Delayed care and unmet needs among health care system users: when does fiduciary trust in a physician matter? Health Serv Res. 2005;40:1898–917.
Wiltshire JC, Person SD, Kiefe CI, Allison JJ. Disentangling the influence of socioeconomic status on differences between African American and white women in unmet medical needs. Am J Public Health. 2009;99:1659–65.
Schokkaert E, Van de Voorde C, Dormont B, Fleurbaey M, Luchini S, Samson A-L, Thébaut C. Equity in health and equivalent incomes. In: Rosa Dias P, O’Donnell O, editors. Health and Inequality (Research on Economic Inequality, vol. 21). Bingley: Emerald; 2013, p. 131–56.
Bundorf K, Pauly M. Is health insurance affordable for the uninsured? J Health Econ. 2006;25(4):650–73.
Glied S. Mandates and the affordability of health care. Inquiry. 2009;46:203–14.
Fleurbaey M, Schokkaert E. Inequity in health and health care. In: Barros P, McGuire T, Pauly M, editors. Handbook of health economics, vol. 2. New York: Elsevier; 2012. p. 1003–92.
Chernew M, Rosen A, Fendrick M. Value-based insurance design. Health Aff. 2007;30:w195–203.
van Doorslaer E, Van Ourti T. Measuring inequality and inequity in health and health care. In: Glied S, Smith P, editors. Oxford handbook on health economics. Oxford: Oxford University Press; 2011. p. 837–69.
Balabanova D, McKee M. Understanding informal payments for health care: the example of Bulgaria. Health Policy. 2002;62:243–73.
Balabanova D, McKee M, Pomerleau JRR, Haerpfer C. Health service utilization in the former Soviet Union: evidence from eight countries. Health Serv Res. 2004;39:1927–50.
Ensor T. Informal payments for health care in transition economies. Soc Sci Med. 2004;58:237–46.
Liaropoulos L, Siskou O, Kaitelidou D, Theodorou M, Katostaras T. Informal payments in public hospitals in Greece. Health Policy. 2008;87:72–81.
Szende A, Culyer A. The inequity of informal payments for health care: the case of Hungary. Health Policy. 2006;75:262–71.
Cutler D, Zeckhauser R. The anatomy of health insurance. In: Culyer A, Newhouse J, editors. Handbook of health economics. New York: Elsevier; 2000. p. 563–643.
McGuire T. Demand for health insurance. In: Barros P, McGuire T, Pauly M, editors. Handbook of health economics, vol. 2. New York: Elsevier; 2012. p. 317–96.
De Graeve D, Van Ourti T. The distributional impact of health financing in Europe: a review. World Econ. 2003;26:1459–79.
Wagstaff A, van Doorslaer E. Equity in health care finance and delivery. In: Culyer A, Newhouse J, editors. Handbook of health economics. New York: Elsevier; 2000. p. 1803–62.
Wagstaff A, van Doorslaer E, et al. Equity in the finance of health care: some further international comparisons. J Health Econ. 1999;18:263–90.
Vrijens F, Renard F, Camberlin C, et al. Performance of the Belgian Health System—Report 2015. KCE Reports 259C. Brussels: Belgian Health Care Knowledge Centre (KCE); 2016.
Ashton C, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med. 2003;18(2):146–52.
van Doorslaer E, O’Donnell O, Rannan-Eliya RP, et al. Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. Lancet. 2006;368:1357–64.
van Doorslaer E, O’Donnell O, Rannan-Eliya RP, et al. Catastrophic payments for health care in Asia. Health Econ. 2007;16:1159–84.
Wagstaff A. Measuring financial protection in health. Policy Research Working Paper 4554. World Bank; 2008.
Xu K, Evans D, Kawabata K, Zeramdini R, Klavus J, Murray C. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–7.
Farfan-Portet M-I, Van de Voorde C, Vrijens F, Vander Stichele R. Patient socioeconomic determinants of the choice of generic versus brand name drugs in the context of a reference price system: evidence from Belgian prescription data. Eur J Health Econ. 2012;13(3):301–13.
Vrijens F, Van de Voorde C, Farfan-Portet M-I, Vander Stichele R. Patient socioeconomic determinants for the choice of the cheapest molecule within a cluster: evidence from Belgian prescription data. Eur J Health Econ. 2012;13(3):315–25.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to the content of the paper. The final version was written by ES.
Corresponding author
Ethics declarations
Conflict of interest
Erik Schokkaert, Jonas Steel and Carine Van de Voorde have no conflicts of interest.
Funding
No external funding was received for the work reported in this study.
Rights and permissions
About this article
Cite this article
Schokkaert, E., Steel, J. & Van de Voorde, C. Out-of-Pocket Payments and Subjective Unmet Need of Healthcare. Appl Health Econ Health Policy 15, 545–555 (2017). https://doi.org/10.1007/s40258-017-0331-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-017-0331-0