Abstract
Introduction
The POPular Genetics trial demonstrated that a CYP2C19 genotype-guided P2Y12 inhibitor strategy reduced bleeding rates compared with standard treatment with ticagrelor or prasugrel without increasing thrombotic event rates after primary percutaneous coronary intervention (PCI).
Objective
In this analysis, we aimed to evaluate the cost effectiveness of a genotype-guided strategy compared with standard treatment with ticagrelor or prasugrel.
Methods
A 1-year decision tree based on the POPular Genetics trial in combination with a lifelong Markov model was developed to compare costs and quality-adjusted life-years (QALYs) between a genotype-guided and a standard P2Y12 inhibitor strategy in patients with myocardial infarction undergoing primary PCI. The cost-effectiveness analysis was conducted from a Dutch healthcare system perspective. Within-trial survival and utility data were combined with lifetime projections to evaluate lifetime cost effectiveness for a cohort of 1000 patients. Costs and utilities were discounted at 4 and 1.5%, respectively, according to Dutch guidelines for health economic studies. Besides deterministic and probabilistic sensitivity analyses, several scenario analyses were also conducted (different time horizons, different discount rates, equal prices for P2Y12 inhibitors, and equal distribution of thrombotic events between the two strategies).
Results
Base-case analysis with a hypothetical cohort of 1000 subjects demonstrated 8.98 QALYs gained and €725,550.69 in cost savings for the genotype-guided strategy (dominant). The deterministic and probabilistic sensitivity analysis confirmed the robustness of the model and the cost-effectiveness results. In scenario analyses, the genotype-guided strategy remained dominant.
Conclusion
In patients undergoing primary PCI, a CYP2C19 genotype-guided strategy compared with standard treatment with ticagrelor or prasugrel resulted in QALYs gained and cost savings.
Trial Registration
Clinicaltrials.gov number: NCT01761786, Netherlands trial register number: NL2872
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A CYP2C19 genotype-guided de-escalation strategy is a reasonable alternative for standard P2Y12 inhibitor therapy according to the latest European Society of Cardiology guidelines for patients with acute coronary syndrome. |
A CYP2C19 genotype-guided strategy compared with standard treatment with potent P2Y12 inhibitors in patients with acute myocardial infarction results in cost savings and improved quality of life. |
These results are based on the prevalence of CYP2C19 loss-of-function alleles in European, mostly Dutch, patients and on Dutch healthcare costs. |
1 Introduction
Patients with myocardial infarction (MI) and patients undergoing percutaneous coronary intervention (PCI) are treated with dual antiplatelet therapy consisting of aspirin (acetylsalicylic acid [ASA]) and a P2Y12 inhibitor. Guidelines favor ticagrelor and prasugrel over clopidogrel in patients with MI because of an associated reduction in thrombotic events [1, 2]. One of the reasons for the reduced effectiveness of clopidogrel compared with the other P2Y12 inhibitors is that clopidogrel must be converted into its active metabolite. The most important enzyme in this process is the cytochrome P450 (CYP) 2C19 enzyme. This enzyme is encoded by the CYP2C19 gene, of which more than 30 different alleles have been identified [3]. Some of these alleles encode for an enzyme that is not functional. The CYP2C19*2 and *3 alleles are the most common loss-of-function alleles, and almost one-third of people in western populations carry one or two of these alleles [4]. Several studies demonstrated that these patients have an increased risk of developing major adverse cardiac events [5]. This prompted the US FDA to add a boxed warning for clopidogrel, stating that the drug might not be effective in patients carrying two loss-of-function alleles [6]. Nevertheless, clopidogrel is still the most frequently prescribed P2Y12 inhibitor, either because of fear of bleeding complications or other side effects when using the stronger P2Y12 inhibitors or for economic reasons (e.g., lower costs of treatment) [7,8,9].
The POPular (Patient Outcomes after primary PCI) Genetics trial showed that, in patients with ST-segment elevation MI (STEMI) undergoing primary PCI, a CYP2C19 genotype-guided P2Y12 inhibitor strategy was noninferior for a net clinical benefit outcome while reducing bleeding outcomes as compared with standard treatment with ticagrelor and prasugrel [10]. Since genetic testing is associated with higher costs, although clopidogrel has a lower price than the other P2Y12 inhibitors, the objective of this study was to assess the cost effectiveness of the genotype-guided strategy compared with a standard treatment strategy with ticagrelor or prasugrel within the context of the Dutch healthcare system.
2 Methods
2.1 Study Design
Details on the methods and results of the POPular Genetics trial have been reported previously [10, 11]. In brief, POPular Genetics was an open-label, randomized, multicenter trial in 2488 patients with STEMI undergoing primary PCI. It evaluated standard treatment with the P2Y12 inhibitors ticagrelor 90 mg twice daily or prasugrel 5 or 10 mg once daily based on the summary of product characteristics approved by the European Medicines Agency compared with a CYP2C19 genotype-guided strategy, where patients without CYP2C19*2 or *3 loss-of-function alleles were prescribed clopidogrel 75 mg once daily and ticagrelor or prasugrel (dosage identical to standard treatment) if they were carriers of such a loss-of-function allele. All patients also received guideline-recommended ASA. Treatment and follow-up duration were 12 months. At 1, 6, and 12 months, all patients received a questionnaire by either post or email. This questionnaire contained the EQ-5D-5L, which was used to calculate health utilities. The cost-effectiveness analysis was prespecified as part of the trial protocol. The trial was approved by the appropriate ethics committees and national authorities. All patients provided informed consent.
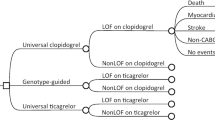
2.2 Model Overview
The current analysis was designed to calculate the cost effectiveness of a CYP2C19 genotype-guided strategy for patients with STEMI undergoing primary PCI. A two-part decision-analytic model was developed that comprised a 1-year decision tree to determine the initial distribution of the cohort over the Markov states (Fig. 1a) and a Markov model to simulate lifelong costs and effects (Fig. 1b). In the 1-year decision tree, all patients could experience minor or major bleeding independent of experiencing any of the other events. At the end of the 1-year decision tree period, patients entered the respective Markov states depending on the experienced event (e.g., event-free, recurrent MI, recurrent stroke, or death). The Markov model structure is identical to previously published trials investigating antiplatelet therapy in similar populations [12], clinically validated, and adjusted to allow for recurrence of stroke and MI. Four disease transient states were included to reflect the lifetime progression of individuals after STEMI, including MI, post-MI, stroke, and post-stroke. Additionally, the model comprised two absorbing states, defined as cardiovascular death and noncardiovascular death. A cohort of 1000 hypothetical subjects was used to simulate the progression through the different disease states. Subjects could switch between disease states or remain in the same disease state based on transition probabilities. In the base-case analysis, a lifetime horizon was used with a cut-off at the age of 100 years.
2.3 Model Assumptions
One of the assumptions underpinning the model was that patients in both groups were treated with ASA monotherapy after the 1-year trial period was finished. Therefore, no difference in bleeding rates was expected in the Markov model. Furthermore, bleeding usually decreases quality of life for only a short period. Hence, bleeding was not included as a separate health state in the Markov model. We assumed that patients could not develop multiple events during the 1-year trial, which was in line with the cost-effectiveness analysis of the PLATO (Platelet Inhibition and Patient Outcomes) trial [12]. In addition, we assumed that recurrent stroke or MI could only happen with a minimum interval of 1 year.
2.4 Population
The intention-to-treat population from the POPular Genetics trial was used for the current decision-analytic model (Table 1). The mean age of the trial population was 61 years, 15% were aged ≥ 75 years, 25% were female, and 10% had a prior history of coronary artery disease. In line with the mean age of the patients in the POPular Genetics trial cohort, all individuals were aged 61 years at the start of the decision tree.
2.5 Model Input Parameters
2.5.1 Transition Probabilities
All model inputs are presented in Table 2. Probabilities for all patients in the 1-year decision tree were based on the results from the POPular Genetics trial [10]. At the end of the decision tree, patients were allocated to their respective health state in the long-term Markov model. Starting from the second year, a Markov state-transition model with yearly cycles was used to simulate disease progression of patients over their lifetime. In each health state, patients could experience an MI, stroke, or death in any year. Patients in the “post-MI” and “post-stroke” health states had a higher risk of subsequent events than patients in the “no event” health state. The transition probabilities of experiencing subsequent events were derived by multiplying the baseline probabilities by the relative risk factors (Table 2) [12]. For mortality, an age-specific mortality rate was used based on the Dutch population lifetables. It was not possible to transition from “post-stroke” to “post-MI”, since the MI health state had a lower risk and was less costly than the stroke health state.
2.5.2 Costs
Cost effectiveness was estimated from the healthcare perspective, so only medical costs were included. Costs were inflated to year 2020 values using the consumer price index inflation from the Dutch Central Bureau of Statistics (Table 2). Costs were based on the Dutch healthcare system and obtained from literature or Dutch governmental agencies. Cost categories were treatment costs (genetic test and different antiplatelet drugs) and costs associated with the different events: minor bleeding, major bleeding, nonfatal MI, nonfatal stroke, post-MI, post-stroke, and death. The costs associated with the use of ASA and other medication were excluded from the analysis, since we assumed this would affect both treatment strategies equally. Costs were discounted using an annual rate of 4% in accordance with existing guidelines for conducting health economic evaluations [23].
2.5.3 Health Utilities
Health utilities, measured in quality-adjusted life-years (QALYs), were dependent on the events experienced by patients (Table 2). Health utility estimates were either derived from the POPular Genetics trial (using the EQ-5D-5L questionnaire) or, if data were not available from the trial, derived from literature focused on the Dutch healthcare system with similar populations. Based on previously published literature, bleeding led to a temporary disutility for the duration of the event during the first year following treatment. QALYs were discounted using an annual rate of 1.5% in accordance with Dutch guidelines for conducting health economic evaluations [23].
2.5.4 Outcomes
The outcome measures used to compare the two strategies in this study were costs, QALYs, and incremental cost-effectiveness ratios (ICERs) presented as cost per QALY gained.
2.5.5 Sensitivity and Scenario Analysis
The base-case analysis was based on the model inputs as shown in Table 2. To accommodate for model uncertainty, univariate deterministic sensitivity analyses and probabilistic sensitivity analyses were conducted. For the sensitivity analyses, the estimated range of each parameter was based on the 95% confidence interval (CI) in the studies. If the 95% CI was not available, ranges were calculated with a standard error of the mean of 25%. For univariate deterministic sensitivity analyses, each of the parameters was varied one by one over the 95% CI to examine the influence of individual parameters on the ICER. In the probabilistic sensitivity analysis, a Monte Carlo simulation was performed (1000 iterations) by varying the parameters simultaneously over their 95% CI. The cost, probability, and utility parameter distributions were varied with a Gamma-, Pert, and Beta distribution, respectively. Outcomes of the sensitivity analysis are presented in a tornado diagram and a cost-effectiveness plane. Four additional scenarios were conducted to capture the effect of the time horizon (1, 5, 10, and 25 years in the Markov model; scenario 1); adjustment of the discount rates to both costs and utilities at 4% (scenario 2); equal drug prices for all three drugs at €0.05/day, to mimic the availability of generic variants in the future (scenario 3); and equal distribution of the cohort over post-MI, post-stroke, and death (both cardiovascular death and noncardiovascular death) at the start of the Markov model for both strategies to account for the uncertainty that a genotype-guided strategy does not result in numerically less stroke and MI as seen in the POPular Genetics trial (scenario 4).
3 Results
3.1 Base-Case Analysis
For a cohort of 1000 patients undergoing primary PCI based on the POPular Genetics trial, the genotype-guided strategy resulted in QALYs gained of 8.98 while saving €725,550.69 (0.009 QALYs gained and €725.56 saved per patient) (Table 3). Cost-saving results for the genotype-guided strategy indicate that this strategy dominates current standard treatment without genotyping. Figure 2 displays the results of the univariate deterministic sensitivity analysis in a tornado diagram. The results demonstrate that, when varying the different model inputs over their CIs, the genotype-guided strategy remains cost saving. Results of the 1000 iterations of the probabilistic sensitivity analysis were plotted on a cost-effectiveness plane (Fig. 3). The genotype-guided strategy was cost saving in each iteration of the Monte Carlo simulation, whereas it increased QALYs in almost all iterations.
One-way sensitivity analysis of a genotype-guided strategy versus standard treatment with ticagrelor or prasugrel. Horizontal bars indicate the range of cost savings obtained when setting each individual variable at its maximum and minimum confidence interval. Since all results remain cost saving, the direction of the bar makes no difference. CV cardiovascular, MI myocardial infarction, NF nonfatal
Results of the probabilistic sensitivity analysis on the cost-effectiveness plane. The scatterplot depicts results of the Monte Carlo analysis (1000 iterations) when all model inputs are randomly varied between their confidence intervals. The black line depicts the willingness to pay €20,000/QALY. A genotype-guided strategy is cost effective if it falls below the black line. QALY quality-adjusted life-year
3.2 Scenario Analyses
In Table 3, results are presented for the varying time horizons (scenario 1), adjustment in discount rates (scenario 2), equal prices for all P2Y12 inhibitors (scenario 3), and an equal distribution of patients amongst health states between the two strategies (scenario 4). In all different scenarios, the genotype-guided strategy remained cost saving and improved QALYs.
4 Discussion
In this prospectively designed cost-effectiveness analysis, based on the POPular Genetics trial data, a CYP2C19 genotype-guided strategy was associated with an increase in QALYs and was cost saving (dominant) as compared with standard treatment with ticagrelor or prasugrel in patients with STEMI undergoing primary PCI. The robustness of this finding was confirmed by various additional sensitivity and scenario analyses. In the Netherlands, the willingness-to-pay threshold varies between €20,000 and 80,000 depending on the intervention, whereas the willingness-to-pay threshold in other European countries also varies but is generally of the same magnitude [24]. Our results are well below the lower end of this range.
The American College of Cardiology (ACC)/American Heart Association (AHA) published a guideline on health economic analyses [25]. According to this guideline, our findings suggest a high value of a genotype-guided strategy as compared with a standard treatment strategy with ticagrelor or prasugrel, since it improved QALYs while reducing costs.
The cost-effective results showing that the genotype-based strategy is dominant were primarily driven by two differences in the first year. The first determining variable was the price for generic clopidogrel, which is lower (€0.05/day) than that for the patented ticagrelor and prasugrel (€2.18 and €1.65/day, respectively) [15,16,17]. The difference in costs between clopidogrel and the other P2Y12 inhibitors reflects the potential additional cost of performing a genetic test, which was estimated to be €150.00 for a point-of-care test. Since both ticagrelor and prasugrel are expected to have generic variants available in the next few years, which will likely cause a drop in prices, we conducted a scenario analysis in which the daily costs of ticagrelor and prasugrel were identical to those of clopidogrel (€0.05/day). Following this scenario analysis, the genotype-guided strategy remained cost saving, with QALYs gained similar to those in the base-case analysis. Therefore, it can be realistically assumed that extra costs associated with performing genetic testing will not change the results. The availability of generic ticagrelor and prasugrel will lower prices in the future, but it is uncertain to what extent. The scenario analysis is therefore on the conservative end of the spectrum.
The second important factor driving the results of the current analysis was the distribution of the patients at the onset of the Markov model. Based on the results from the POPular Genetics trial, patients in the genotype-guided arm were in a more favorable health state than patients in the standard treatment arm when they entered the Markov model, because the incidence of stroke and MI was lower in the genotype-guided cohort than in the standard treatment cohort. To account for the uncertainty that a genotype-guided strategy actually leads to numerically less stroke and less MI, as seen in the POPular Genetics trial, we conducted a scenario analysis in which there was no difference amongst the distribution of patients in the different health states when entering the Markov model between the two strategies. In this scenario analysis, the genotype-guided strategy remained cost saving, whereas only a small difference remained in QALYs gained. This was expected, since the difference in QALYs was then only caused by a difference in minor bleeding events between both groups, which have a relatively low impact on long-term health utilities. These results demonstrate that the cost savings and long-term benefits are based on the differences in the first year after genotype-guided treatment.
In the POPular Genetics trial, more than 95% of the included patients were Caucasian, with only a small proportion of Asian, Latin American, or African descent [10]. The prevalence of CYP2C19 loss-of-function alleles does not differ much between African, American, and European populations but is a lot higher in Asian populations [4]. A higher prevalence of loss-of-function alleles means more people will remain on ticagrelor or prasugrel, which will negatively affect the results of the cost-effectiveness analysis in these countries. In addition, it is uncertain how this affects outcomes of the trial. On the other hand, in countries with a similar prevalence of loss-of-function alleles, similar clinical outcomes as in our trial and similar results of a cost-effectiveness analysis could be expected. However, we should be aware that healthcare costs can differ significantly between countries.
4.1 Comparison with Other Studies
Several health economic analyses concerning a genotype-guided P2Y12 inhibitor strategy have been published [14, 26,27,28,29]. These analyses used extrapolated data from, for instance, the PLATO or TRITON TIMI (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel-Thrombolysis in Myocardial Infarction)-38 trial to build their decision tree, but they did not have data from a trial specifically investigating a genotype-guided strategy. Lala et al. [14], who based most of their model input parameters on TRITON TIMI 38, reported results similar to those presented within the current study. They found a genotype-guided strategy to be cost saving and to increase QALYs compared with both standard treatment with prasugrel and standard treatment with clopidogrel. Our results are also in accordance with the cost-effectiveness analysis by Wang et al. [26], which used data from the PLATO trial and found a genotype-guided strategy to be cost saving and to improve QALYs as compared with standard treatment with ticagrelor. In addition, they also concluded that, compared with standard treatment with clopidogrel, a genotype-guided strategy improved QALYs at an ICER of $US2560. A cost-effectiveness analysis by Limdi et al. [27] investigated whether universal ticagrelor treatment or genotype-guided de-escalation was cost effective in patients with acute coronary syndrome undergoing PCI as compared with universal clopidogrel treatment based on real-world data. Although both strategies increased QALYs compared with universal clopidogrel treatment, only genotype-guided de-escalation was cost effective at an ICER of $US42,365. Like our results, those from both Wang et al. [26] and Limdi et al. [27] were below the “high value” limit of $US50,000/QALY as set by the ACC/AHA guideline [25].
Unlike our results, studies by Sorich et al. [28] and Crespin et al. [29], both based on results from the PLATO trial, found that ticagrelor treatment was cost effective as compared with a genotype-guided strategy. This means higher costs with additional QALYs gained [28, 29]. The fact that ticagrelor compared with the genotype-guided strategy resulted in QALYs gained already explains the major difference between the results of Crespin et al. [29] and Sorich et al. [28] compared with our results. In addition, some important considerations with respect to the findings of Crespin et al. [29] and Sorich et al. [28] should be taken into account. Crespin et al. [29] noted that ticagrelor would no longer be cost effective if the hazard ratio (HR) for mortality between ticagrelor and clopidogrel were higher than 0.93, which was the case in the POPular Genetics trial (HR 1.00) [10]. In the study by Sorich et al. [28], the cost of ticagrelor was only three times the cost of clopidogrel, whereas the Dutch tariffs indicate a 43.6 times higher cost of ticagrelor compared with clopidogrel. Sorich et al. [28] reported that this small price difference between clopidogrel and ticagrelor was one reason why ticagrelor treatment was cost effective compared with a genotype-guided strategy in their study (ICER of ticagrelor vs. a genotype-guided strategy: Australian dollars [AUD] 22,821). Furthermore, researchers indicated that, if the HR between ticagrelor and clopidogrel exceeded 0.95, as it does in our study, the ICER would increase to over AUD50,000, making the cost effectiveness of ticagrelor compared with a genotype-guided strategy highly questionable.
While the previously mentioned studies used data from the PLATO and TRITON TIMI 38 trials to build their study models, the respective study groups themselves also wrote health economic analyses. The health economic analysis of the PLATO trial, which compared ticagrelor and clopidogrel, noted, like Crespin et al. [29], that most of the QALYs gained in the ticagrelor arm of their analysis were derived from the mortality benefit from ticagrelor as compared with clopidogrel [12]. The greatest benefit in the TRITON TIMI 38 health economic analysis was derived from a reduction in MI in the prasugrel arm as compared with the clopidogrel arm [30]. In the POPular Genetics trial, no numerical benefits in MI or mortality were seen in the standard treatment arm as compared with the genotype-guided arm [10]. Besides the much lower costs of clopidogrel treatment compared with the other P2Y12 inhibitors and some savings on bleeding events, this is one of the most important reasons for the lack of benefit for ticagrelor and prasugrel in our analysis.
4.2 Limitations
Our results should be interpreted in light of the following limitations. This cost-effectiveness analysis was based on data from patients with STEMI undergoing primary PCI. Therefore, whether these results also apply to patients with another form of acute coronary syndrome and patients not undergoing PCI is unknown. In addition, most of the patients in the POPular Genetics trial were treated with ticagrelor. Since the recently published ISAR-REACT (Intracoronary Stenting and Antithrombotic Regimen: Rapid Early Action for Coronary Treatment)-5 trial found that the use of prasugrel might be beneficial over the use of ticagrelor [31], both costs and event rates might be affected if more patients are treated with prasugrel instead of ticagrelor. This applies to both the standard treatment and genotype-guided groups, since one-third of patients in the genotyping group are still treated with ticagrelor or prasugrel. Concerning the health economic analysis, the analysis was based on a healthcare perspective instead of a societal perspective, which is sometimes preferred. However, using a societal perspective would mean further assumptions regarding costs would be necessary. Besides, the only difference in our model was present in the first year during the decision tree, therefore, adding the same costs to both arms (treatment and control) was not expected to add additional value to the model or to affect the result of the analysis.
5 Conclusion
In patients with STEMI undergoing primary PCI, a CYP2C19 genotype-guided strategy compared with standard treatment with ticagrelor or prasugrel resulted in QALYs gained and cost savings.
References
Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2016;68:1082–115.
Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–77.
Scott SA, Sangkuhl K, Shuldiner AR, et al. PharmGKB summary: very important pharmacogene information for cytochrome P450, family 2, subfamily C, polypeptide 19. Pharmacogenet Genomics. 2012;22:159–65.
Scott SA, Sangkuhl K, Stein CM, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin Pharmacol Ther. 2013;94:317–23.
Mega JL, Simon T, Collet JP, et al. Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA. 2010;304:1821–30.
Holmes DR, Dehmer GJ, Kaul S, Leifer D, O’Gara PT, Stein CM. ACCF/AHA clopidogrel clinical alert: approaches to the FDA “boxed warning”: a report of the American College of Cardiology foundation task force on clinical export consensus documents and the American Heart Association endorsed by the Society of Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2010;56:321–41.
Motovska Z, Hlinomaz O, Kala P, et al. 1-year outcomes of patients undergoing primary angioplasty for myocardial infarction treated with prasugrel versus ticagrelor. JACC. 2018;71:371–81.
Gimbel ME, Qaderdan K, Willemsen L, et al. Clopidogrel versus ticagrelor or prasugrel in patients aged 70 years or older with non-ST-elevation acute coronary syndrome (POPular AGE): the randomised, open-label, non-inferiority trial. Lancet. 2020;395:1374–81.
Zettler ME, Peterson ED, McCoy LA, et al. Switching of adenosine diphosphate receptor inhibitor after hospital discharge among myocardial infarction patients: insights from the treatment with adenosine diphosphate receptor inhibitors: Longitudinal assessment of treatment patterns and events after acute coronary syndrome (TRANSLATE-ACS) observational study. Am Heart J. 2017;183:62–8.
Claassens DMF, Vos GJA, Bergmeijer TO, et al. A genotype-guided strategy for oral P2Y12 inhibitors in primary PCI. N Engl J Med. 2019;381:1621–31.
Bergmeijer TO, Janssen PWA, Schipper JC, et al. CYP2C19 genotype-guided antiplatelet therapy in ST-segment elevation myocardial infarction patients-Rationale and design of the patient outcome after primary PCI (POPular) Genetics study. Am Heart J. 2014;168:16-22.e.1.
Nikolic E, Janzon M, Hauch O, Wallentin L, Henriksson M. Cost-effectiveness of treating acute coronary syndrome patients with ticagrelor for 12 months: results from the PLATO study. Eur Heart J. 2012;34:220–8.
Central Bureau for Statistics. Lifetables. https://opendata.cbs.nl/statline/#/CBS/nl/dataset/83482NED/table?ts=1603871419734. Accessed 15 Oct 2020.
Lala A, Berger JS, Sharma G, Hochman JS, Braithwaite RS, Ladapo JA. Genetic testing in patients with acute coronary syndrome undergoing percutaneous coronary intervention: a cost-effectiveness analysis. J Thromb Haemost. 2013;11:81–91.
Zorginstituut Nederland. GIPdatabank: Vergoeding per DDD 2015-2019 voor ATC-subgroep B01AC04 : Clopidogrel. https://www.gipdatabank.nl/databank?infotype=g&label=00-totaal&tabel_g_00-totaal=B_01-basis&geg=vg&spec=vg_ddd&item=B01AC04. Accessed 15 Oct 2020.
Zorginstituut Nederland. GIPdatabank: Vergoeding per DDD 2015-2019 voor ATC-subgroep B01AC24 : Ticagrelor. https://www.gipdatabank.nl/databank?infotype=g&label=00-totaal&tabel_g_00-totaal=B_01-basis&geg=vg&spec=vg_ddd&item=B01AC24. Accessed 15 Oct 2020.
Zorginstituut Nederland. GIPdatabank: Vergoeding per DDD 2015-2019 voor ATC-subgroep B01AC22 : Prasugrel. https://www.gipdatabank.nl/databank?infotype=g&label=00-totaal&tabel_g_00-totaal=B_01-basis&geg=vg&spec=vg_ddd&item=B01AC22. Accessed 15 Oct 2020.
Jacobs MS, De Jong LA, Postma MJ, Tieleman RG, Van Hulst M. Health economic evaluation of rivaroxaban in elective cardioversion of atrial fibrillation. Eur J Health Econ. 2018;19:957–65.
ten Cate-Hoek AJ, Toll DB, Buller HR, et al. Cost-effectiveness of ruling out deep venous thrombosis in primary care versus care as usual. J Thromb Haemost. 2009;7:2042–9.
Stevanovic J, Pompen M, Le HH, Rozenbaum MH, Tieleman RG, Postma MJ. Economic evaluation of apixaban for the prevention of stroke in non-valvular atrial fibrillation in the Netherlands. PLoS ONE. 2014;9:e103974.
De Jong LA, Groeneveld J, Stefanovic J, et al. Cost-effectiveness of apixaban compared to other anticoagulants in patients with atrial fibrillation in the real-world and trial settings. PLoS ONE. 2019;14(9):e0222658.
Van Eeden M, Van Heugten C, Van Mastrigt GAPG, Van Mierlo M, Visser-Meily JMA, Evers SMAA. Evers SMAA. The burden of stroke in the Netherlands: estimating quality of life and costs for 1 year poststroke. BMJ Open. 2015;5:e008220.
Ijzerman MJ, Al MJ, De Boer A, et al. Richtlijn voor het uitvoeren van economische evaluaties in de gezondheidszorg. Zorginstituut Ned. 2016; 1–38. https://www.zorginstituutnederland.nl/publicaties/publicatie/2016/02/29/richtlijn-voor-het-uitvoeren-van-economische-evaluaties-in-de-gezondheidszorg. Accessed 15 Oct 2020.
Ligtenberg G, Staal PC, Goettsch WG, Knies S. Kosteneffectiviteit in de zorg, op weg naar een genuanceerd en geaccepteerd gebruik van kosteneffectiviteitsgegevens in de zorg. College voor Zorgverzekeringen 2013; 1–41. https://www.zorginstituutnederland.nl/binaries/zinl/documenten/rapport/2013/09/30/kosteneffectiviteit-in-de-zorg/Kosteneffectiviteit+in+de+zorg.pdf. Accessed 15 Oct 2020.
Anderson JL, Heidenreich PA, Barnett PG, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2304–22.
Wang Y, Yan BP, Liew D, Lee VWY. Cost-effectiveness of cytochrome P450 2C19 *2 genotype-guided selection of clopidogrel or ticagrelor in Chinese patients with acute coronary syndrome. Pharmacogenom J. 2018;18:113–20.
Limdi NA, Cavallari LH, Lee CR, et al. Cost-effectiveness of CYP2C19-guided antiplatelet therapy in patients with acute coronary syndrome and percutaneous coronary intervention informed by real-world data. Pharmacogenom J. 2020;20:724–35.
Sorich MJ, Horowitz JD, Sorich W, Wiese MD, Pekarsky B, Karnon JD. Cost-effectiveness of using CYP2C19 genotype to guide selection of clopidogrel or ticagrelor in Australia. Pharmacogenomics. 2013;14:2013–21.
Crespin DJ, Federspiel JJ, Biddle AK, Jonas DE, Rossi JS. Ticagrelor versus genotype-driven antiplatelet therapy for secondary prevention after acute coronary syndrome: a cost-effectiveness analysis. Value Health. 2011;14:483–91.
Mahoney EM, Wang K, Arnold SV, et al. Cost-effectiveness of prasugrel versus clopidogrel in patients with acute coronary syndromes and planned percutaneous coronary intervention: results from the trial to assess improvement in therapeutic outcomes by optimizing platelet inhibition with prasugrel-thrombolysis in myocardial infarction TRITON-TIMI 38. Circulation. 2010;121:71–9.
Schüpke S, Neumann FJ, Menichelli M, et al. Ticagrelor or prasugrel in patients with acute coronary syndromes. N Engl J Med. 2019;381:1524–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by ZonMw, a Dutch government agency, as part of its efficiency research program (project 171102022). Spartan Bioscience (Nepean, Ottawa, ON, Canada) provided the Spartan RX system and the reagents used free of charge.
Conflicts of interest
Dr. Asselbergs has received grants from the University College London Hospitals National Institute for Health Research Biomedical Research Centre. Dr. van 't Hof has received institutional grants from Medtronic, AstraZeneca, and Sanofi and personal fees from AstraZeneca and Amgen. Dr. Barbato has received personal fees from Boston Scientific, Abbott Vascular, and GE. Dr. Ten Berg has received institutional grants from AstraZeneca and ZonMw and personal fees from AstraZeneca, Daiichi Sankyo, Eli Lilly, the Medicines Company, Accumetrics, Boehringer-Ingelheim, Bayer, BMS, Pfizer, and Ferrer. Dr. Postma has received institutional grants from AstraZeneca, GSK, Pfizer, and Amgen and personal fees from AstraZeneca, Daiichi Sankyo, Boehringer-Ingelheim, Bayer, BMS, Pfizer, GSK, and Roche. Daniel M.F. Claassens, Pim W.M. van Dorst, Gerrit J.A. Vos, Thomas O. Bergmeijer, Renicus S. Hermanides, Pim van der Harst, Carmine Morisco, Richard M. Tjon Joe Gin, Arend Mosterd, Jean-Paul R. Herrman, Willem J.M. Dewilde, Vera H.M. Deneer, and Cornelis Boersma have no conflicts of interest that are directly relevant to the content of this article.
Availability of data and material
Data will be made available upon reasonable request
Code availability
Analyses were performed using R version 3.6 or later and Excel.
Ethics approval
An institutional review board at each site approved the trial.
Consent to participate
All patients provided informed consent to participate in the trial.
Author contributions
Conceptualization: TOB, JMtB, VHMD. Methodology: DMFC, WMvD, CB. Formal analysis and investigation: DMFC, WMvD, TOB, GJAV. Writing—original draft preparation: DMFC, WMvD. Writing—review and editing: GJAV, TOB, RSH, AWJv’tH, PvdH, EB, CM, RMTJG, FWA, AM, JPRH, WJMD, MJP. Funding acquisition: VHMD. Resources: RSH, AWJv’tH, PvdH, EB, CM, RMTJG, FWA, AM, JPRH, WJMD. Supervision: VHMD, JMtB, CB, MJP.
Rights and permissions
About this article
Cite this article
Claassens, D.M.F., van Dorst, P.W.M., Vos, G.J.A. et al. Cost Effectiveness of a CYP2C19 Genotype-Guided Strategy in Patients with Acute Myocardial Infarction: Results from the POPular Genetics Trial. Am J Cardiovasc Drugs 22, 195–206 (2022). https://doi.org/10.1007/s40256-021-00496-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-021-00496-4