Abstract
Background
The overuse of antimicrobials favors the dissemination of antimicrobial resistance, as well as invasive fungal diseases and Clostridium difficile infections (CDI). In this study, we assessed the impact of a mixed educational and semi-restrictive antimicrobial stewardship (AMS) project in a large teaching hospital in Italy.
Methods
The AMS project was conducted from May 2014 to April 2016. It consisted of two initiatives in two consecutive periods: (1) educational activities; (2) semi-restrictive control of antimicrobial prescribing through a computerized software. The primary endpoint was consumption of antibacterials and antifungals. Secondary endpoints were incidence of CDI, methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections (BSI), carbapenem-resistant Klebsiella pneumoniae (CRKP) BSI, and Candida BSI.
Results
During the study period, a statistically significant reduction in consumption was observed for antibacterials (−1.45 defined daily doses (DDD)/1000 patient-days monthly, 95% confidence intervals [CI] −2.38 to −0.52, p 0.004), mainly driven by reductions in the use of fluoroquinolones, third/fourth generation cephalosporins, and carbapenems. No decrease in consumption of antifungals was observed (−0.04 DDD/1000 patient-days monthly, 95% CI −0.34 to +0.25, p 0.750). A statistically significant trend towards reduction was observed for incidence of CRKP BSI (incidence rate ratio 0.96, 95% CI 0.92–0.99, p 0.013). No statistically significant variations in trends were observed for CDI, MRSA BSI, and Candida BSI.
Conclusions
The mixed AMS project was effective in reducing the use of major antibacterials and the incidence of CRKP BSI. Further research is needed to assess the extent of long-term benefits of semi-restrictive approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Antimicrobials are undoubtedly one of the major successes of modern medicine [1]. However, due to the unceasing spread of antimicrobial resistance, the risk of losing their efficacy has become a looming threat [1, 2]. Among factors deemed as responsible for the current crisis are the overuse and misuse of antibacterials, which, besides antimicrobial resistance, also trigger other unintended consequences, such as invasive fungal diseases and C. difficile infections (CDI) [3,4,5,6,7,8,9,10,11,12].
Therefore, antimicrobial stewardship (AMS), initially intended as the sum of interventions to improve the appropriate use of antibacterials, has become a priority in the global strategy to prevent the further development and dissemination of resistance, as well as to reduce the incidence of fungal infections and CDI [13,14,15,16,17,18,19]. Subsequently, the judicious use of antifungals has also emerged as an important additional aim of AMS, mostly because of the high mortality of fungal diseases and the high cost of treatments [20, 21].
Although national and supranational interventions remain essential to reduce the overuse and misuse of antimicrobials in an effective way, AMS projects should also be tailored to the needs, resources, and microbiological epidemiology of every single hospital, with the aim of maximizing their cost-effectiveness locally. With this purpose, the impact of a mixed educational and semi-restrictive AMS project was assessed in a large teaching hospital in Italy.
Materials and methods
The AMS project was started in 2014 at Ospedale Policlinico San Martino, a 1200-bed adult acute care hospital in Genoa, Italy. The project was developed by infectious diseases (ID) specialists and pharmacists, in agreement with the hospital infection-control unit, and it consisted of two periods: (1) in the first 12 months (May 2014–April 2015) wards physicians participated in targeted educational activities (in the form of separate meetings dedicated to different medical and surgical specialists, each starting with lectures provided by ID specialists, pharmacists, pharmacologists, infection-control experts, and microbiologists, and followed by interactive discussion of appropriate indications, doses, duration, and route of administration of antimicrobials); (2) in the second 12 months (May 2015–April 2016), besides a few additional educational meetings, we adopted a semi-restrictive and computerized AMS approach using a software which allows individualized prescription and administration of drugs (Sofia®, SANTALUCIA PHARMA APPS©, Località Gragnanino, PC, Italy). Briefly, for each prescription of antimicrobials deemed to have a major impact on antibiotic resistance and/or routinely used in the treatment of resistant infections (i.e., vancomycin, teicoplanin, daptomycin, ceftaroline, ceftobiprole, meropenem, ertapenem, imipenem, linezolid, tigecycline, colistin, voriconazole, posaconazole, liposomal amphotericin B, micafungin, caspofungin, anidulafungin) a request for approval was automatically generated by the software, to be evaluated by an ID specialist. After prescription, the ID specialist was allowed a maximum of 48 h (72 h if the prescription was made during weekend days) for approval or rejection, always following discussion with the original prescriber in case of rejection. Pending the ID specialist’s decision, the prescribed drug could be administered to avoid omission of the initial doses. In the absence of approval or rejection by IDS within the recommended 48/72 h, the prescriber was anyway allowed to administer the drug to avoid the omission of doses, but a phone call was made from the hospital pharmacy to remind the ID specialist of the need for a decision. In addition to approval or rejection, the ID specialist had the chance to change the duration of treatment in days proposed by the prescriber, with a need for a new request for approval whenever the prescriber wanted to continue the administration beyond the end of the approved period.
The analysis was restricted to those wards where the computerized system was used for drug delivery during the entire study period (i.e., most of medical and surgical wards but not intensive care and emergency units, where it was not implemented at the time of the study).
Study endpoints
The primary endpoint of this study was consumption of antibacterials and antifungals, expressed as defined daily doses (DDD)/1000 patient-days. Secondary endpoints were: (1) incidence of C. difficile infections (CDI); (2) incidence of methicillin-resistant S. aureus (MRSA) bloodstream infections (BSI); (3) incidence of carbapenem-resistant K. pneumoniae (CRKP) BSI; (4) incidence of Candida BSI.
Definitions
Antibiotic and antifungal consumption was calculated as DDD per 1000 patient-days. Incidence of CDI, MRSA BSI, CRKP BSI, and Candida BSI were calculated as the number of events per 1000 patient-days. Only health-care associated CDI, MRSA BSI, CRKP BSI, and Candida BSI were considered for the analysis. CDI was defined as the presence of at least one unformed stool specimen positive for C. difficile toxin A and/or B [22]. Recurrences of CDI (i.e., novel events occurring within 56 days after the first positive stool sample) were excluded from the analyses [22]. A CDI episode was considered as healthcare-associated if occurring after at least 72 h from hospitalization, or within 28 days after discharge [22]. In line with the European Centre for Disease Control and prevention (ECDC) definition, health-care associated MRSA, CRKP, and Candida BSI were defined by a positive blood culture collected at least 48 h after hospital admission, or within 48 h from hospital admission in those patients who had been discharged in the preceding 2 days [23]. For patients with multiple episodes of BSI, a novel event was considered as independent if occurring at least 30 days after the last positive blood culture.
Data collection
Anonymized data on antibiotic and antifungal consumption were retrieved from the computerized database of the dedicated software. Anonymized data on CDI and BSI were extracted from the microbiological laboratory database.
Microbiology
Presence of C. difficile toxin A and/or B in stool specimens was diagnosed with the C. Diff Quick Chek complete® assay (Techlab, USA; Alere Medical Co. Ltd, USA). The Vitek 2 system (bioMérieux, Marcy l’Etoile, France) was used for the identification of MRSA, CRKP and Candida from blood cultures and for antimicrobial susceptibility testing. The interpretative breakpoints were based on the European Committee on Antimicrobial Susceptibility Testing (EUCAST) criteria (EUCAST break point tables for interpretation of MICs and zone diameters, version 6.0, 2016; http://www.eucast.org). Klebsiella pneumoniae isolates which tested resistant to at least one carbapenem were considered CRKP.
Statistical analysis
The trends in DDD/1000 patient-days of antimicrobials during the entire study period (May 2014–April 2016) were assessed through univariable linear regression models, whereas the trends in the incidence rate (IR, defined as the number of events/patient-days) of CDI and BSI over the same period were assessed through univariable Poisson or negative binomial regression, according to the absence or presence of overdispersion in count data, respectively. Time in months was the independent variable in all univariable models.
The impact of the computerized semi-restrictive program on the trends of consumption of antimicrobials (either restricted or unrestricted) was assessed by including the following variables in the pertinent multivariable linear regression model: (1) time in months; (2) phase (pre-implementation from May 2014 to April 2015 and post-implementation from May 2015 to April 2016); (3) the appropriate term for interaction (time × phase), to specifically assess the effect of the intervention in modifying the slope of the regression line (i.e., the monthly change in DDD/1000 patient-days). The analyses were performed using R Statistical Software version 3.3.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Overall, 931/1204 hospital beds were considered in this study (77%), representing those wards where the dedicated computerized system was used during the entire study period. The total consumption of antibacterials and antifungals in DDD during the study period is detailed in Fig. 1. As shown, the most used antibacterials were semisynthetic penicillins (148,321 DDD), followed by fluoroquinolones (53,203 DDD) and third generation cephalosporins (36,128 DDD), whereas fluconazole was the most used antifungal (9323 DDD), followed by echinocandins (4892 DDD).
Trends in antimicrobials consumption over the entire study period are detailed in Table 1, with trends for the most used classes being also displayed graphically in Fig. 2. Overall, a statistically significant reduction was observed for antibacterials (−1.45 DDD/1000 patient-days monthly, 95% confidence intervals [CI] −2.38 to −0.52, p 0.004). More in detail, statistically significant reductions were observed for fluoroquinolones (−0.84 DDD/1000 patient-days monthly, 95% CI −1.38 to −0.31, p = 0.003), third/fourth generation cephalosporins (−0.47 DDD/1000 patient-days monthly, 95% CI −0.85 to −0.09, p 0.018), carbapenems (−0.35 DDD/1000 patient-days monthly, 95% CI −0.69 to −0.02, p 0.041), and metronidazole (−0.24 DDD/1000 patient-days monthly, 95% CI −0.40 to −0.08, p 0.005). On the other hand, a statistically significant increase was observed for linezolid (+0.18 DDD/1000 patient-days monthly, 95% CI +0.05 to +0.31, p 0.009). Regarding antifungals, no statistically significant variations were observed, both overall and for fluconazole and echinocandins taken singularly (Table 1).
Subgroup analyses of antimicrobial consumption in the educational and semi-restrictive phases of the AMS project are shown in Table 2. Although some interesting patterns were observed (apparent inversion from increasing to decreasing consumption of restricted antibacterials, achievement of a plateau in the reduction of unrestricted antibacterials), the semi-restrictive phase did not significantly modify the trends established in the educational period (p for interaction 0.240, 0.081, 0.208, and 0.431 for restricted antibacterials, unrestricted antibacterials, restricted antifungals, and unrestricted antifungals, respectively), with the two phases contributing together to the overall effect.
During the semi-restrictive period, the ID specialist in most cases approved the prescribed drug and just change or confirm the length of treatment (5534/5607, 98.7%), while he/she rejected the prescription in only 73/5607 cases (1.3%). The ID specialist did not evaluate the request within the recommended 48/72 h in 343/5607 cases (6.1%).
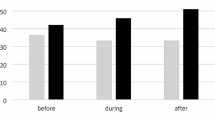
The IR of CDI (incidence rate ratio [IRR] 1.00, 95% CI 0.98–1.03, p 0.731) and MRSA BSI (IRR 0.99, 95% CI 0.97–1.02, p 0.624) remained stable over the entire study period. As shown in Fig. 3, a statistically significant reduction was observed for CRKP BSI (IRR 0.96, 95% CI 0.92–0.99, p 0.013), while, although not statistically significant, an increasing IR over time was observed for Candida BSI (IRR 1.02, 95% CI 0.99–1.05, p 0.156).
Trends in the incidence of Clostridium difficile infections (CDI), methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infections (BSI), carbapenem-resistant Klebsiella pneumoniae (CRKP) BSI, and Candida BSI during the study period. *Statistically significant trend towards reduced incidence (p < 0.05)
Discussion
After the introduction of a mixed two-step educational and semi-restrictive AMS project in our hospital, we observed an important reduction in the consumption of antibacterials and in the incidence of CRKP BSI.
AMS is crucial for reducing the dissemination of resistance and improving patient care, and dedicated documents have been developed for implementing AMS programs in acute-care hospitals, such as the guidelines by the Infectious Diseases Society of America (IDSA) [24]. In addition to educational activities, two main approaches are described in IDSA guidelines for improving prescriptions, each with pros and cons: (1) prospective audit with intervention and feedback; (2) formulary restriction and preauthorization. The former has been associated with improved antimicrobial use and has the advantage of providing education of prescribers on a patient-to-patient basis, while the latter can lead to immediate and significant reductions in antimicrobial use and cost but with less clear long-term educational effects [24]. While strongly supporting the first approach, we also thought it was urgent to apply a more aggressive approach to rapidly counteract the dissemination of CRKP, which, as widely known, is endemic in our country, and unfortunately our hospital is not an exception [25,26,27,28]. Thus, as the second step of our AMS project after 12 months of education, we adopted a hybrid semi-restrictive system, including both feedback and pre-authorization aspects. During the entire study period (educational plus semi-restrictive phases), we observed a significant reduction in the use of antibacterials, in particular of fluoroquinolones, third generation cephalosporins, and carbapenems, the use of which has been associated with increased incidence of CDI and/or CRKP BSI in previous studies [9, 10, 29, 30]. In this regard, we also observed a reduction in CRKP BSI, which is in line with a favourable effect of the decreasing use of antibacterials. Of course, this effect might also be explained by the dedicated infection-control measures we have adopted since 2012 (rapid identification and isolation of colonized/infected patients through a centralized and computerized laboratory-based alert system, patient-dedicated use of gowns and gloves). However, taking into account previous data from our hospital [26], it should be noted that the reduction in CRKP BSI was observed only after starting the educational phase of the AMS project. This conceivably reflects an important synergistic effect of AMS and infection-control efforts. The same might be true for CDI. Indeed, the steep increase in the incidence of CDI that was observed in our centre in previous years [6] appeared to cease during the study period. From this standpoint, the flattening of the line might be consistent with a favourable effect of the AMS project. Back to the consumption of antibacterials, the only increasing trend we observed was that of linezolid. This might reflect either overuse or, conversely, an increased appropriateness in treating MRSA or vancomycin-resistant Enterococci infections. In any case, although further investigation is needed to better explain this result, it should be noted that the use of linezolid was limited and did not influence the overall reduction.
While we observed a reduction in the use of antibacterials, the same was not true for antifungals. This apparent lack of effect of our AMS efforts might rely on the particular distribution of Candida BSI, which mainly clustered in two non-consecutive months in 2015 (August and November), and that were necessarily treated with antifungals. This suggests that important variables other than AMS might contribute in shaping the use of antimicrobials and the microbiological epidemiology of every single hospital, including the occurrence of outbreaks, the promptness of response in case of outbreaks, the clustering in time and space of patients with specific risk factors for infection, the type and extension of infection-control measures, the staff adherence to contention protocols, and the possible selection/diffusion of more/less virulent organisms, all factors that should always be considered when interpreting the results of AMS interventions.
In this study, we also tried to assess the specific impact of the semi-restrictive period, which, as mentioned above, was implemented after 12 months of education. In this regard, the semi-restrictive phase apparently contributed only additively to the overall effect. However, it is of note that the results of this secondary analysis should be considered as preliminary. Indeed, a short period of 12 months might not be enough to observe any definitive impact on trends. Further observation is also needed to clarify why the decrease in consumption of unrestricted antibacterials apparently slowed down in the second phase of the study. Indeed, this might reflect either the achievement of a plateau (overuse can be reduced, but ultimately many patients need antibiotics) or an unintended—but not necessarily unfavourable—effect of restriction (increase in the prescription of unrestricted agents to avoid the need for authorization).
This study also helped us to notice some limitations of our semi-restricted approach, that should be improved. For example, the fact that ID specialists just changed or confirmed the length of treatment in more than 98% of cases might give the impression that our educational efforts were successful, but this result should be considered cautiously, in view of an important information bias. Indeed, at the time of the study our system was unable to account for those cases in which the ID specialists contacted the prescribers directly and suggested an alternative prescription without formally rejecting the prescription through the dedicated software. These changes (ultimately performed by the original prescriber) were not detected but likely contributed to the overall decrease in the use of antibacterials. In addition, we were also unable to distinguish whether, in case of approval, ID specialists changed rather than confirm the proposed length of treatment. We are currently working together with pharmacists, prescribers, and informaticists on the traceability of these and other aspects (including financial costs and benefits, as well as patient-level data for calculating other important outcome measures of ASM interventions, such as days of therapy [24]), with the aim of improving our AMS efforts in the future.
The main limitation of this study is that we could not collect data on antimicrobial consumption before the start of the educational phase of the project. Indeed, the number of wards using the dedicated software increased with time, and extending the study period to the preceding years would have considerably reduced the number of wards to be included and, therefore, the representativeness of the sample. Nonetheless, it should be noted that the observed trend towards reduction in the IR of CRKP BSI, which was previously increasing [26], is overall suggestive of a true positive effect of our AMS efforts independently of previous consumption of antimicrobials. Another important limitation, as reported above, is that our secondary analysis of the impact of the computerized semi-restrictive approach is still preliminary, because of the limited 12-month study period. It would be of interest to finalize this analysis in the future, including also the assessment of the possible contribution of further improvements/changes in our program. Finally, it is worth reminding that our analysis was restricted to those wards where the computerized system was used at the time of the study. Therefore, our results cannot be extrapolated to peculiar settings such as intensive care units and the emergency department that were not included.
In conclusion, mixed AMS projects might be helpful for restricting the prescription of some antimicrobials without losing the long-term benefits of continuous education, which are essential to achieve and maintain the best plateau of consumption in the long run.
Change history
05 October 2017
A technical error led to incorrect rendering of the author group in this article. The correct authorship is as follows: Daniele Roberto Giacobbe1, Valerio Del Bono1, Malgorzata Mikulska1, Giulia Gustinetti1, Anna Marchese2, Federica Mina3, Alessio Signori4, Andrea Orsi5, Fulvio Rudello6, Cristiano Alicino5, Beatrice Bonalumi3, Alessandra Morando7, Giancarlo Icardi5, Sabrina Beltramini3, Claudio Viscoli1; On behalf of the San Martino Antimicrobial Stewardship Group
References
Marston HD, Dixon DM, Knisely JM, et al. Antimicrobial resistance. JAMA. 2016;316:1193–204.
Fauci AS, Marston ID. The perpetual challenge of antimicrobial resistance. JAMA. 2014;311:1853–4.
Clatworthy AE, Pierson E, Hung DT. Targeting virulence: a new paradigm for antimicrobial therapy. Nat Chem Biol. 2007;3:541–8.
Schmieder R, Edwards R. Insights into antibiotic resistance through metagenomic approaches. Future Microbiol. 2012;7:73–89.
Giacobbe DR, Del Bono V, Trecarichi EM, De Rosa FG, Giannella M, Bassetti M, et al. Risk factors for bloodstream infections due to colistin-resistant KPC-producing Klebsiella pneumoniae: results from a multicenter case-control-control study. Clin Microbiol Infect. 2015;21:1106.e1–8.
Alicino C, Giacobbe DR, Durando P, et al. Increasing incidence of Clostridium difficile infections: results from a 5-year retrospective study in a large teaching hospital in the Italian region with the oldest population. Epidemiol Infect. 2016;144:2517–26.
Asensio A, Di Bella S, Lo Vecchio A, et al. The impact of Clostridium difficile infection on resource use and costs in hospitals in Spain and Italy: a matched cohort study. Int J Infect Dis. 2015;36:31–8.
Falcone M, Tiseo G, Tascini C, et al. Assessment of risk factors for candidemia in non-neutropenic patients hospitalized in Internal Medicine wards: a multicenter study. Eur J Intern Med. 2017;. doi:10.1016/j.ejim.2017.03.005.
Šuljagić V, Miljković I, Starčević S, et al. Risk factors for Clostridium difficile infection in surgical patients hospitalized in a tertiary hospital in Belgrade, Serbia: a case–control study. Antimicrob Resist Infect Control. 2017;6:31.
Adams DJ, Elberly MD, Rajnik M, et al. Risk factors for community-associated Clostridium difficile in children. J Pediatr. 2017;. doi:10.1016/j.jpeds.2017.03.032.
Del Bono V, Giacobbe DR. Bloodstream infections in internal medicine. Virulence. 2016;7:353–65.
De Rosa FG, Corcione S, Raviolo S, et al. Candidemia, and infections by Clostridium difficile and carbapenemase-producing Enterobacteriaceae: new enteropethogenetic opportunistic syndromes? Infez Med. 2015;23:105–16.
Charani E, Cooke J, Holmes A. Antibiotic stewardship programmes–what’s missing? J Antimicrob Chemother. 2010;65:2275–7.
Hamilton KW, Fishman NO. Antimicrobial stewardship interventions: thinking inside and outside the box. Infect Dis Clin N Am. 2014;28:301–13.
White AC, Atmar RL, Wilson J, et al. Effects of requiring prior authorization for selected antimicrobials: expenditures, susceptibilities, and clinical outcomes. Clin Infect Dis. 1997;25:230–9.
Pear SM, Williamson TH, Bettin KM, et al. Decrease in nosocomial Clostridium difficile-associated diarrhea by restricting clindamycin use. Ann Intern Med. 1994;120:272–7.
Carling P, Fung T, Killion A, et al. Favorable impact of a multidisciplinary antibiotic management program conducted during 7 years. Infect Control Hosp Epidemiol. 2003;24:699–706.
Solomon DH, Van Houten L, Glynn RJ. Academic detailing to improve use of broad-spectrum antibiotics at an academic medical center. Arch Intern Med. 2001;161:1897–902.
Ben-Ami R, Olshtain-Pops K, Krieger M, Israeli Candidemia Study Group, et al. Antibiotic exposure as a risk factor for fluconazole-resistant Candida bloodstream infection. Antimicrob Agents Chemother. 2012;56:2518–23.
Ananda-Rajah MR, Slavin MA, Thursky KT. The case for antifungal stewardship. Curr Opin Infect Dis. 2012;25:107–15.
Denning DW, Perlin DS, Muldoon EG, et al. Delivering on antimicrobial resistance agenda not possible without improving fungal diagnostic capabilities. Emerg Infect Dis. 2017;23:177–83.
Centers for Disease Control and Prevention. National Health Safety Network multidrug-resistant organism and Clostridium difficile infection (MDRO/CDI) module (http://www.cdc.gov/nhsn/PDFs/pscManual/12pscMDRO_CDADcurrent.pdf). Accessed 20 April 2017.
European Centre for Disease Control and Prevention. Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals. Protocol version 4.3, 2012. http://ecdc.europa.eu/en/publications/publications/0512-ted-pps-hai-antimicrobial-use-protocol.pdf. Accessed 20 April 2017.
Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;15(62):e51–77.
Conte V, Monaco M, Giani T, et al. Molecular epidemiology of KPC-producing Klebsiella pneumoniae from invasive infections in Italy: increasing diversity with predominance of the ST512 clade II sublineage. J Antimicrob Chemother. 2016;71:3386–91.
Alicino C, Giacobbe DR, Orsi A, et al. Trends in the incidence of carbapenem-resistant Klebsiella pneumoniae bloodstream infections: a 8-year retrospective study in a large teaching hospital in northern Italy. BMC Infect Dis. 2015;15:415.
Giacobbe DR, Del Bono V, Marchese A, et al. Early carbapenem-resistant Klebsiella pneumoniae bacteraemia: should we expand the screening? Clin Microbiol Infect. 2014;20:O1157–8.
Cristina ML, Alicino C, Sartini M, et al. Epidemiology, management, and outcome of carbapenem-resistant Klebsiella pneumoniae bloodstream infections in hospitals within the same endemic metropolitan area. J Infect Public Health. 2017;. doi:10.1016/j.jiph.2017.06.003.
Okamoto K, Lin MY, Haverkate M, et al. Modifiable risk factors for the spread of Klebsiella pneumoniae carbapenemase-producing enterobacteriaceae among long-term acute-care hospital patients. Infect Control Hosp Epidemiol. 2017;. doi:10.1017/ice.2017.62.
Tumbarello M, Trecarichi EM, Tumietto F, et al. Predictive models for identification of hospitalized patients harboring KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2014;58:3514–20.
Acknowledgements
The authors wish thank Federico Tassinari (University of Genoa, DISSAL) for his help with data collection.
Participants in the San Martino Antimicrobial Stewardship Group: Antonio Ferrazin, Ferdinando Dodi, Norberto Morandi, Federica Toscanini, Marco Camera, Antonio Di Biagio, Giovanni Mazzarello, Anna Ida Alessandrini, Andrea De Maria, Emanuele Delfino, Laura Ambra Nicolini, Carolina Saffioti, Federica Magnè, Nemo Gandolfo.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Fulvio Rudello is an employer of SANTALUCIA PHARMA APPS©. The other authors declare no conflicts of interest relevant to this paper.
Additional information
The original version of this article was revised: A technical error led to incorrect rendering of the author group in this article. The correct authorship is as follows: Daniele Roberto Giacobbe1, Valerio Del Bono1, Malgorzata Mikulska1, Giulia Gustinetti1, Anna Marchese2, Federica Mina3, Alessio Signori4, Andrea Orsi5, Fulvio Rudello6, Cristiano Alicino5, Beatrice Bonalumi3, Alessandra Morando7, Giancarlo Icardi5, Sabrina Beltramini3, Claudio Viscoli1; on behalf of the San Martino Antimicrobial Stewardship Group
The collaborators are: Antonio Ferrazin, Ferdinando Dodi, Norberto Morandi, Federica Toscanini, Marco Camera, Antonio Di Biagio, Giovanni Mazzarello, Anna Ida Alessandrini, Andrea De Maria, Emanuele Delfino, Laura Ambra Nicolini, Carolina Saffioti, Federica Magnè, Nemo Gandolfo
A correction to this article is available online at https://doi.org/10.1007/s15010-017-1068-2.
Rights and permissions
About this article
Cite this article
Giacobbe, D.R., Del Bono, V., Mikulska, M. et al. Impact of a mixed educational and semi-restrictive antimicrobial stewardship project in a large teaching hospital in Northern Italy. Infection 45, 849–856 (2017). https://doi.org/10.1007/s15010-017-1063-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1063-7