Abstract
BACKGROUND:
As a contour-supporting material, the cartilage has a significant application value in plastic surgery. Since the development of hydrogel scaffolds with sufficient biomechanical strength and high biocompatibility, cell-laden hydrogels have been widely studied for application in cartilage bioengineering. This systematic review summarizes the latest research on engineered cartilage constructed using cell-laden hydrogel scaffolds in plastic surgery.
METHODS:
A systematic review was performed by searching the PubMed and Web of Science databases using selected keywords and Medical Subject Headings search terms.
RESULTS:
Forty-two studies were identified based on the search criteria. After full-text screening for inclusion and exclusion criteria, 18 studies were included. Data collected from each study included culturing form, seed cell types and sources, concentration of cells and gels, scaffold materials and bio-printing structures, and biomechanical properties of cartilage constructs. These cell-laden hydrogel scaffolds were reported to show some feasibility of cartilage engineering, including better cell proliferation, enhanced deposition of glycosaminoglycans and collagen type II in the extracellular matrix, and better biomechanical properties close to the natural state.
CONCLUSION:
Cell-laden hydrogels have been widely used in cartilage bioengineering research. Through 3-dimensional (3D) printing, the cell-laden hydrogel can form a bionic contour structure. Extracellular matrix expression was observed in vivo and in vitro, and the elastic modulus was reported to be similar to that of natural cartilage. The future direction of cartilage tissue engineering in plastic surgery involves the use of novel hydrogel materials and more advanced 3D printing technology combined with biochemistry and biomechanical stimulation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
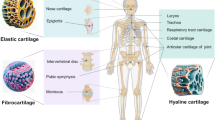
As a contour-supporting material, the cartilage has a significant application value in plastic surgery. Auricular and nasal reconstruction requires the auricular and costal cartilages to be cut and carved, resulting in the consumption of autologous materials, which is significantly greater than what is available [1]. Trauma of the donor site and loss of autologous tissue are inevitable [2]. Cartilage tissue engineering, which has been widely discussed and researched in recent times, provides a new method for producing contour-supporting materials for plastic surgery.
Owing to the poor self-healing and proliferation ability of the cartilage, cartilage regeneration has always been a challenging direction for research and clinical applications [3]. With the development of three-dimensional (3D) culture and 3D bio-printing, tissue engineering technologythat combines cells (somatic cells and stem cells) and biomaterials has shown potential for the preparation of cartilage scaffolds and the repair of cartilage defects [2].
The cell-laden hydrogel scaffold is an emerging area of bioengineering scaffolds. In recent years, with the progress of materials science and 3D printing technology, researchers have been able to obtain cell-laden scaffolds with sufficient biomechanical strength and high biocompatibility [4]. The bioengineered cartilage with cell-laden hydrogel has been studied in vitro and in animal experiments, in which there have been many attempts in the field of plastic surgery, including the regeneration of nasal cartilage, ear cartilage, and tracheal cartilage.
In this study, we aimed to systematically review the literature published in the field of plastic surgery in the past 10 years focusing on cartilage tissue engineering based on cell-laden hydrogel scaffolds, and attempted to clarify the following questions: What types of biomimetic scaffolds have been prepared? What hydrogel materials have been used, and what new materials have potential application? What cells have been loaded into hydrogels and have been proven to have good chondrogenesis? Are there any new advances in cartilage bioengineering that may have application in the field of plastic surgery?
2 Methods of systematic review
This was a systematic review of the literature in which cell-laden hydrogels were used for cartilage tissue engineering in the field of plastic surgery. The involved cells included chondrocytes, auricular cartilage progenitor cells, and mesenchymal stem cells in humans and animals, and the 3D bio-printed technique was used to create the tissue constructs or hydrogel models.
The PubMed and Web of Science databases were searched. The following terms were used (including synonyms and closely related words) as index terms or free-text words: “cartilage” or “chondrocyte”; “hydrogel”; “3D” or “printing” or “bio-printed” or “scaffold”; and “plastic surgery.” The articles were restricted to those written in English. The publication date was from January 2010 to June 2021. Studies were included if they investigated a hydrogel scaffold in which cells were loaded inside and reported its potential for cartilage tissue regeneration and reconstruction in plastic surgery application.
3 Results
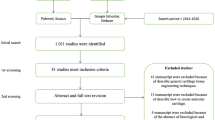
Using the search terms described above, 42 publications were identified. A flow diagram of the inclusion and exclusion process is shown in Fig. 1. After reading the full-length text of these publications, 18 studies were included in this review [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. Basic information on culture form, seed cell types, sources, and seeding density is presented in Table 1. And basic information on hydrogel and scaffold contents, experimental animal choices, and scaffold morphology is presented in Table 2.
Among the 18 studies, 11 used chondrocytes as the seeding cell [5,6,7,8,9,10,11,12,13,14,15], 1 used peri-chondrocytes (CPCs) [15], and 2 used adipose mesenchymal stem cells (ADSCs) for chondrogenic differentiation [15, 16]. The remaining six studies [17,18,19,20,21,22] focused on co-culturing using the previously mentioned seed cells to form tissue-engineered cartilage. With regard to the sources of seed cells, five researchers used human cells [5, 6, 16, 19, 20], four used goat/sheep cells [11,12,13, 17], three used bovine cells [7, 9, 18], three used porcine/swine cells [8, 10, 22], two used rabbit cells [14, 21], and one used horse cells [15]. The density of seed cells varied, but was mostly approximately 10–30×106 cells/ml.
Collagen was the most frequently applied hydrogel [5, 7,8,9,10, 17, 18, 22], followed by alginate [6, 11, 16, 19, 20], hyaluronic acid (HA) [10, 17, 22], gelatin methacrylate (GelMA) [12, 15], extracellular matrix [14, 16], and thermo-sensitive hydroxypropyl chitin (HPCH) [13]. Some used more than one type of hydrogel to combine the advantages and obtain better material properties. Three-dimensional bio-printing of grid cube constructs was commonly used to verify the chondrogenic properties of the cell-laden scaffold. There were also some studies that reported the 3D reconstruction of human facial image data and bio-printed the cell-laden scaffold in the shape of a human auricle or nasal implant, which further promotes the combination of cartilage engineering and clinical application [6, 7, 9,10,11, 14, 16]. In some studies [6, 7, 9], a pre-fabricated model was used to ensure the morphology and volume of the hydrogel and its scaffolds after solidity. Some studies used poly-ε-caprolactone (PCL) as a reinforcing material to form a skeleton with stronger biomechanical properties studies [8, 10,11,12, 16, 17, 21, 22].
Nude rats and mice were the most widely used experimental animals. As these studies are aimed at stimulating the ectopic chondrogenic environment of engineering constructs in the clinical application of plastic surgery, the dorsal subcutaneous embedding method was commonly chosen. In addition, in one study [21], in order to simulate the tracheal structure, authors chose to implant the construct under the pedicled muscle flap of rabbits.
The Young’s modulus of the scaffolds was tested to determine the biomechanical properties in eight of these studies, which are listed in Table 3. In these reports, the Young’s modulus varied greatly with the material of the scaffold. For hydrogel scaffolds without rigid support (four out of eight studies), the average value of the Young’s modulus was in the range of 100-380 kPa [7, 9, 15, 18]. For hydrogel scaffolds with PCL support, the Young’s modulus is in the range of 0.8-4 MPa [8, 12]. The constructs printed in the polylactide-co-glycolide (PLGA) scaffold filled with collagen had a Young’s modulus of 15-25 MPa [5]. Another study reported that the average Young’s modulus of PCL cell-laden hydrogel was 8-16 kPa [17]. It was obvious that the engineered constructs with different types of seed cells, that is, mesenchymal stem cells (MSCs), auricular cartilage progenitor cells (AuCPCs), and chondrocytes, had different Young’s moduli. However, there was no clear evidence to show which seed cells or which cell proportion of co-culture could result in the best biomechanical performance.
These cell-laden hydrogel scaffolds were reported to show some feasibility of cartilage engineering, including better cell proliferation, enhanced deposition of glycosaminoglycans and collagen type II in the extracellular matrix, and better biomechanical properties close to the natural state.
4 Discussion
4.1 Significant role of cartilage tissue engineering in plastic surgery
Cartilage has been widely applied as a contour-filling material in the fields of plastic surgery and cosmetic surgery. Nasal reconstruction and aesthetic surgery have high strength and shape requirements for augmentation materials. At present, the commonly used augmentation materials include conchal cartilage, costal cartilage, septal cartilage, and alloplastic implants (mainly silicone and expanded polytetrafluoroethylene) [23]. Because of the relative lack of blood supply and thin skin coverage of the external nose, prostheses implanted in the nasal cavity could produce more severe inflammatory reactions compared with those in areas with abundant blood supply [24]. The acquisition of autologous conchal and costal cartilage causes additional pain, surgical wounds, and risks of complications [2]. In addition, the cartilage needs to be cut and carved during the operation to meet the effect requirements to the greatest extent, thus increasing the patient’s surgical trauma and autologous tissue loss. In cases of nasal reconstruction and secondary repair of rhinoplasty, there is a further shortage of autologous cartilage materials.
Reconstruction of the auricle is frequently performed using the costal cartilage. During surgery, the costal cartilage is cut and fitted to the shape of the auricle. Because of the high demand for cartilage, children usually need to reach adolescence in order to undergo ear reconstruction surgery. Long-term external ear deformities often have a great impact on children’s mental health. In addition, the costal cartilage can retain a certain degree of compliance after carving, but it lacks the flexibility required by the external ear, and the contouring outcome is difficult to predict [25, 26]. At present, surgery not only involves the risk of severe hematoma and wound healing disorders, but also requires multiple surgeries to reduce the volume of the graft and to reshape the delicate structures of the helical and anti-helical folds [25].
3D printed polymers are also an option for nasal prostheses or external ear implants. However, these structures still have disadvantages in terms of flexibility and increasing the long-term risk of skin extrusion [27]. Hence, tissue-engineered cartilage, in which the addition of stem cells and bioactive molecules was performed to enhance the functionality of a biomaterial and to transform the generated construct into natural tissue after degradation of the biomaterial, has provided a new method for the repair of cartilage defects and the improvement of aesthetic contour.
4.2 Hydrogel options
At present, there are many types of hydrogel materials used as cell-laden scaffolds, such as collagen, sodium alginate, HA, and gelatin. These gels have good biocompatibility for chondrocytes and MSCs, but their mechanical strength is relatively weak. They usually need to be combined with rigid scaffolds or formed with prefabricated molds to form bio-constructs with concrete shapes [6, 7, 16, 17].
To further enhance their strength and make them more suitable for 3D printing, hydrogels gels have been highly modified. GelMA and methacrylated hyaluronic acid (HAMA) are typical crosslinked modified hydrogels that have been proven to be adequate for chondrocyte and MSC culturing. The combination of GelMA and HAMA results in the integration of the mechanical strength of HAMA and the great biocompatibility of GelMA to form a modified hybrid gel that further provides an ideal chemical and mechanical microenvironment for chondrocytes and chondrogenic differentiation of MSCs [28, 29].
Hybrid GelMA hydrogels combined with other components have also been reported to enhance the cartilage phenotype in scaffolds. Nano-patterned hybrid scaffolds made from GelMA, HA, and polyethylene glycol (PEG) dimethacrylate have been proven to enhance chondrogenesis in dental pulp stem cells [30]. The covalent bonding between modified PCL and GelMA was reported to improve the resistance to repeated axial and rotational forces at the interface. Human chondrocytes embedded within the hybrid constructs were able to form cartilage-specific matrices in vitro and in vivo [31]. Other combinations such as GelMA/silk fibroin [32], and GelMA/chondroitin sulfate [33] have also been reported to enhance the outcome of cartilage regeneration. However, an important challenge in designing scaffolds for cartilage is achieving mechanical properties that closely mimic native tissues, which requires continuous development of hydrogel materials [34].
4.3 Seed cell options
For hydrogel scaffolds, seed cells are loaded inside the gel, and the gel is internally solidified to form pores, allowing cells to proliferate, migrate, and differentiate. There are three types of seed cells in cartilage tissue engineering: chondrocytes, chondrocyte progenitor cells, and MSCs. The proliferation ability of human adult chondrocytes was the weakest among the three types of seed cells; cells in passage 2 were mostly chosen in the reviewed studies. At present, human nasal septal chondrocytes are often used as the source of cartilage seed cells because they are easy to obtain, and the isolated chondrocytes have a stronger proliferative ability [6, 19]. However, the number of chondrocytes in the human nasal septum is small, making it very difficult to prepare a bio-engineering scaffold of a certain size. Despite having relatively larger cell volumes, acquiring human costal cartilage and ear cartilage requires donor site (costal and retroauricular) incisions. However, because of the clear and stable phenotype of the cartilage, chondrocytes are still the most widely applied seed cells in the research of cell-laden scaffolds.
Chondrocyte progenitor cells have stronger proliferation ability and more accurate chondrogenic properties than MSCs [35]. However, the tissue source of cartilage progenitor cells is limited, and donor site incisions are inevitable. At present, the application of chondroprogenitor cells is limited, but it still has good research and application prospects.
MSCs, including amniotic mesenchymal stem cells (AMSCs) [36], bone marrow mesenchymal stem cells (BMSCs) [19,20,21], and ADSCs [17, 18, 22] have been extensively studied as seed cells in cartilage tissue engineering in recent years. They have been reported to have certain chondrogenic abilities in vitro and in vivo in hydrogel scaffolds.
Research on ADSCs in cartilage tissue engineering is not as extensive as that on BMSCs, but as the most easily available source of stem cells in plastic surgery, ADSC ectopic chondrogenesis can be more widely used. An in vitro study showed that human ADSCs derived from different anatomical sites (breast, abdomen, and hip) displayed good cell yield, stemness, mesenchymal phenotype, proliferative ability, and viability, regardless of the cell tissue harvesting site [37]. Studies have shown that ADSCs with specific subpopulations have better chondrogenic differentiation potential [38]. The expression of CD146, CD73, CD90, CD105, and CD106 markers is necessary for ADSC differentiation into cartilage [39]. In addition, the combination of PDGF and insulin [40], TGF-beta [41], GF-1 [42], and BMP [43] with hydrogel was reported to effectively promote cartilage differentiation in ADSCs.
As a novel 3D culture method, spheroids of different seed cells have been applied in cartilage tissue engineering. Chondrocyte spheroids with a diameter of approximately 200 μm were used as micro units to form the ensemble cartilage tissue in agarose. Compared with chondrocytes cultured traditionally, chondrocyte spheroids produced more abundant cartilage extracellular matrix and had a higher expression of hyaline cartilage-related genes, which was close to that of natural cartilage [44]. Other studies reported that human BMSC spheroids were adaptable for bio-printing, and could help maintain cell viability, 3D architecture, chondrogenic phenotype, and fusion capacity in the hydrogel scaffold [45, 46]. The spheroid-laden hydrogel may pave the way to the future of cartilage engineering in the field of plastic surgery.
4.4 Prospects for mechanical bionic scaffolds
The chondrogenesis of MSCs in biological scaffolds is not only related to the choice of seed cells, but also closely related to the biomechanical environment, including the applied forces and cell-generated forces [47]. In recent years, the “mechanobiology of MSCs” has become an important research topic. Studies have shown that in 3D culture, the mechanical properties of the hydrogel matrix affect the differentiation outcomes of MSCs. Adipogenic differentiation of MSCs tends to occur in environments with lower forces, whereas osteogenic differentiation tends to occur in environments with higher forces [48, 49]. Studies have also shown that applied forces influence differentiation outcomes. Compressive force promotes chondrogenic differentiation of stem cells, while tensile force promotes osteogenic differentiation of stem cells [50]. With regard to cell-generated forces, recent studies have implicated multiple mechanical properties of the extracellular matrix as key elements of the stem cell microenvironment. Substrate rigidity [51], nanometer-scale topography [52, 53], and substrate patterning [54] were reported to have an impact on MSC differentiation.
In terms of articular cartilage regeneration, Yu et al. [55] studied the chondrogenic effect of a bionic mechanical environment. They used a customized dynamic tension-compression loading system to stimulate MSCs seeded into a biomimetic scaffold, and finally induced zonal, layer-specific expression of type I and type II collagens with similar structure and function to those present in the native meniscus tissue. In plastic surgery, a hydrogel biomimetic scaffold with an adequate mechanical strength is constructed according to the stress condition of the cartilage scaffolds needed for patients undergoing nasal reconstruction and ear reconstruction. This may also be one of the development directions for bioengineering cartilage scaffolds.
The limitation of this review is that the included studies are limited to those related to plastic surgery. As a subdivision, the application of tissue engineering in plastic surgery must lag behind the most frontier progress, so we may not be able to present the latest technological breakthrough. In addition, because the experimental design, materials, cell species and result evaluation parameters of each study are different, it is difficult to review quantitatively. However, we hope that through this detailed and enumerated review, we can bring readers an overview of the existing research on cartilage tissue engineering in plastic surgery.
Based on the review of the literature, cell-laden hydrogels have been found to be widely used in cartilage bioengineering research. Through 3D printing, the cell-laden hydrogel can form a bionic contour structure, including the shape of human auricular and nasal implants. Better cell proliferation, enhanced deposition of glycosaminoglycans, and collagen type II in the extracellular matrix were observed in vivo and in vitro, and the elastic modulus was reported to be similar to that of natural cartilage. Thus, the future direction of cartilage tissue engineering in plastic surgery involves the use of novel hydrogel materials and more advanced 3D printing technology, combined with biochemical and biomechanical stimulation.
References
Wiggenhauser PS, Schantz JT, Rotter N. Cartilage engineering in reconstructive surgery: auricular, nasal and tracheal engineering from a surgical perspective. Regen Med. 2017;12:303–14.
Daniel RK. Rhinoplasty: dorsal grafts and the designer dorsum. Clinics Plast Surg. 2010;37:293–300.
Zhou F, Hong Y, Zhang X, Yang L, Li J, Jiang D, et al. Tough hydrogel with enhanced tissue integration and in situ forming capability for osteochondral defect repair. Appl Mater Today. 2018;13:32–44.
Yang J, Zhang YS, Yue K, Khademhosseini A. Cell-laden hydrogels for osteochondral and cartilage tissue engineering. Acta Biomater. 2017;57:1–25.
Tanaka Y, Yamaoka H, Nishizawa S, Nagata S, Ogasawara T, Asawa Y, et al. The optimization of porous polymeric scaffolds for chondrocyte/atelocollagen based tissue-engineered cartilage. Biomaterials. 2010;31:4506–16.
Bichara DA, Zhao X, Hwang NS, Bodugoz-Senturk H, Yaremchuk MJ, Randolph MA, et al. Porous poly(vinyl alcohol)-alginate gel hybrid construct for neocartilage formation using human nasoseptal cells. J Surg Res. 2010;163:331–6.
Reiffel AJ, Kafka C, Hernandez KA, Popa S, Perez JL, Zhou S, et al. High-fidelity tissue engineering of patient-specific auricles for reconstruction of pediatric microtia and other auricular deformities. PloS One. 2013;8:e56506.
Chen CH, Shyu VB, Chen JP, Lee MY. Selective laser sintered poly-epsilon-caprolactone scaffold hybridized with collagen hydrogel for cartilage tissue engineering. Biofabrication. 2014;6:015004.
Cohen BP, Hooper RC, Puetzer JL, Nordberg R, Asanbe O, Hernandez KA, et al. Long-term morphological and microarchitectural stability of tissue-engineered, patient-specific auricles in vivo. Tissue Eng Part A. 2016;22:461–8.
Zopf DA, Flanagan CL, Mitsak AG, Brennan JR, Hollister SJ. Pore architecture effects on chondrogenic potential of patient-specific 3-dimensionally printed porous tissue bioscaffolds for auricular tissue engineering. Int J Pediatr Otorhinolaryngol. 2018;114:170–4.
Visscher DO, Gleadall A, Buskermolen JK, Burla F, Segal J, Koenderink GH, et al. Design and fabrication of a hybrid alginate hydrogel/poly(epsilon-caprolactone) mold for auricular cartilage reconstruction. J Biomed Mater Res B Appl Biomater. 2019;107:1711–21.
Ruiz-Cantu L, Gleadall A, Faris C, Segal J, Shakesheff K, Yang J. Multi-material 3D bioprinting of porous constructs for cartilage regeneration. Mater Sci Eng C Mater Biol Appl. 2020;109:110578.
Xu Y, Xu Y, Bi B, Hou M, Yao L, Du Q, et al. A moldable thermosensitive hydroxypropyl chitin hydrogel for 3D cartilage regeneration in vitro and in vivo. Acta Biomater. 2020;108:87–96.
Visscher DO, Lee H, van Zuijlen PPM, Helder MN, Atala A, Yoo JJ, et al. A photo-crosslinkable cartilage-derived extracellular matrix bioink for auricular cartilage tissue engineering. Acta Biomater. 2021;121:193–203.
Otto IA, Levato R, Webb WR, Khan IM, Breugem CC, Malda J. Progenitor cells in auricular cartilage demonstrate cartilage-forming capacity in 3D hydrogel culture. Eur Cell Mater. 2018;35:132–50.
Yi HG, Choi YJ, Jung JW, et al. Three-dimensional printing of a patient-specific engineered nasal cartilage for augmentative rhinoplasty. J Tissue Eng. 2019;10:2041731418824797.
Visscher DO, Bos EJ, Peeters M, Kuzmin NV, Groot ML, Helder MN, et al. Cartilage tissue engineering: preventing tissue scaffold contraction using a 3D-printed polymeric cage. Tissue Eng Part C Methods. 2016;22:573–84.
Morrison KA, Cohen BP, Asanbe O, Dong X, Harper A, Bonassar LJ, et al. Optimizing cell sourcing for clinical translation of tissue engineered ears. Biofabrication. 2016;9:015004.
Möller T, Amoroso M, Hägg D, Brantsing C, Rotter N, Apelgren P, et al. In vivo chondrogenesis in 3D bioprinted human cell-laden hydrogel constructs. Plast Reconstr Surg Glob Open. 2017;5:e1227.
Apelgren P, Amoroso M, Lindahl A, et al. Chondrocytes and stem cells in 3D-bioprinted structures create human cartilage in vivo. PloS One. 2017;12:e0189428.
Chang CS, Yang CY, Hsiao HY, Chen L, Chu IM, Cheng MH, et al. Cultivation of auricular chondrocytes in poly(ethylene glycol)/poly(epsilon-caprolactone) hydrogel for tracheal cartilage tissue engineering in a rabbit model. Eur Cell Mater. 2018;35:350–64.
Morrison RJ, Nasser HB, Kashlan KN, Zopf DA, Milner DJ, Flanangan CL, et al. Co-culture of adipose-derived stem cells and chondrocytes on three-dimensionally printed bioscaffolds for craniofacial cartilage engineering. Laryngoscope. 2018;128:E251-7.
Li D, An Y, Yang X. An overview of asian rhinoplasty. Ann Plast Surg. 2016;77:S22-4.
Idone F. Diced cartilage grafts wrapped in rectus abdominis fascia for nasal dorsum augmentation. Plast Reconstr Surg. 2016;138:762e.
Storck K, Staudenmaier R, Buchberger M, Strenger T, Kreutzer K, von Bomhard A, et al. Total reconstruction of the auricle: our experiences on indications and recent techniques. Biomed Res Int. 2014;2014:373286.
Nagata S. A new method of total reconstruction of the auricle for microtia. Plast Reconstr Surg. 1993;92:187–201.
Liao J, Chen Y, Chen J, He B, Qian L, Xu J, et al. Auricle shaping using 3D printing and autologous diced cartilage. Laryngoscope. 2019;129:2467–74.
Eke G, Mangir N, Hasirci N, MacNeil S, Hasirci V. Development of a UV crosslinked biodegradable hydrogel containing adipose derived stem cells to promote vascularization for skin wounds and tissue engineering. Biomaterials. 2017;129:188–98.
Lam T, Dehne T, Krüger JP, Hondke S, Endres M, Thomas A, et al. Photopolymerizable gelatin and hyaluronic acid for stereolithographic 3D bioprinting of tissue-engineered cartilage. J Biomed Mater Res B Appl Biomater. 2019;107:2649–57.
Nemeth CL, Janebodin K, Yuan AE, Dennis JE, Reyes M, Kim DH. Enhanced chondrogenic differentiation of dental pulp stem cells using nanopatterned PEG-GelMA-HA hydrogels. Tissue Eng Part A. 2014;20:2817–29.
Boere KW, Visser J, Seyednejad H, Rahimian S, Gawlitta D, van Steenbergen MJ, et al. Covalent attachment of a three-dimensionally printed thermoplast to a gelatin hydrogel for mechanically enhanced cartilage constructs. Acta Biomater. 2014;10:2602–11.
Shi W, Sun M, Hu X, Ren B, Cheng J, Li C, et al. Structurally and functionally optimized silk-fibroin-gelatin scaffold using 3d printing to repair cartilage injury in vitro and in vivo. Adv Mater. 2017. https://doi.org/10.1002/adma.201701089.
Levett PA, Melchels FP, Schrobback K, Hutmacher DW, Malda J, Klein TJ. A biomimetic extracellular matrix for cartilage tissue engineering centered on photocurable gelatin, hyaluronic acid and chondroitin sulfate. Acta Biomater. 2014;10:214–23.
Yue K, Trujillo-de Santiago G, Alvarez MM, Tamayol A, Annabi N, Khademhosseini A. Synthesis, properties, and biomedical applications of gelatin methacryloyl (GelMA) hydrogels. Biomaterials. 2015;73:254–71.
Ma Q, Liao J, Cai X. Different sources of stem cells and their application in cartilage tissue engineering. Curr Stem Cell Res Ther. 2018;13:568–75.
You Q, Liu Z, Zhang J, Shen M, Li Y, Jin Y, et al. Human amniotic mesenchymal stem cell sheets encapsulating cartilage particles facilitate repair of rabbit osteochondral defects. Am J Sports Med. 2020;48:599–611.
Veronesi F, Maglio M, Tschon M, Aldini NN, Fini M. Adipose-derived mesenchymal stem cells for cartilage tissue engineering: state-of-the-art in in vivo studies. J Biomed Mater Res A. 2014;102:2448–66.
Bexkens R, Ogink PT, Doornberg JN, Kerkhoffs GMMJ, Eygendaal D, Oh LS, et al. Donor-site morbidity after osteochondral autologous transplantation for osteochondritis dissecans of the capitellum: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25:2237–46.
Hurley ET, Yasui Y, Gianakos AL, Seow D, Shimozono Y, Kerkhoffs GMMJ, et al. Limited evidence for adipose-derived stem cell therapy on the treatment of osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2018;26:3499–507.
Scioli MG, Bielli A, Gentile P, Cervelli V, Orlandi A. Combined treatment with platelet-rich plasma and insulin favours chondrogenic and osteogenic differentiation of human adipose-derived stem cells in three-dimensional collagen scaffolds. J Tissue Eng Regen Med. 2017;11:2398–410.
Yang Q, Teng BH, Wang LN, Li K, Xu C, Ma XL, et al. Silk fibroin/cartilage extracellular matrix scaffolds with sequential delivery of TGF-beta 3 for chondrogenic differentiation of adipose-derived stem cells. Int J Nanomedicine. 2017;12:6721–33.
Cho H, Kim J, Kim S, Jung YC, Wang Y, Kang BJ, et al. Dual delivery of stem cells and insulin-like growth factor-1 in coacervate-embedded composite hydrogels for enhanced cartilage regeneration in osteochondral defects. J Control Release. 2020;327:284–95.
Deng ZH, Li YS, Gao X, Lei GH, Huard J. Bone morphogenetic proteins for articular cartilage regeneration. Osteoarthritis Cartilage. 2018;26:1153–61.
Chen Y, Ma M, Teng Y, Cao H, Yang Y, Wang Y, et al. Efficient manufacturing of tissue engineered cartilage in vitro by a multiplexed 3D cultured method. J Mater Chem B. 2020;8:2082–95.
De Moor L, Fernandez S, Vercruysse C, Tytgat L, Asadian M, De Geyter N, et al. Hybrid bioprinting of chondrogenically induced human mesenchymal stem cell spheroids. Front Bioeng Biotechnol. 2020;8:484.
Vainieri ML, Lolli A, Kops N, D'Atri D, Eglin D, Yayon A, et al. Evaluation of biomimetic hyaluronic-based hydrogels with enhanced endogenous cell recruitment and cartilage matrix formation. Acta Biomater. 2020;101:293–303.
Hao J, Zhang Y, Jing D, Shen Y, Tang G, Huang S, et al. Mechanobiology of mesenchymal stem cells: perspective into mechanical induction of MSC fate. Acta Biomater. 2015;20:1–9.
Huebsch N, Arany PR, Mao AS, Shvartsman D, Ali OA, Bencherif SA, et al. Harnessing traction-mediated manipulation of the cell/matrix interface to control stem-cell fate. Nat Mater. 2010;9:518–26.
Khetan S, Guvendiren M, Legant WR, Cohen DM, Chen CS, Burdick JA. Degradation-mediated cellular traction directs stem cell fate in covalently crosslinked three-dimensional hydrogels. Nat Mater. 2013;12:458–65.
Sen B, Xie Z, Case N, Ma M, Rubin C, Rubin J. Mechanical strain inhibits adipogenesis in mesenchymal stem cells by stimulating a durable beta-catenin signal. Endocrinology. 2008;149:6065–75.
Lee J, Abdeen AA, Zhang D, Kilian KA. Directing stem cell fate on hydrogel substrates by controlling cell geometry, matrix mechanics and adhesion ligand composition. Biomaterials. 2013;34:8140–8.
Dalby MJ, Gadegaard N, Tare R, Andar A, Riehle MO, Herzyk P, et al. The control of human mesenchymal cell differentiation using nanoscale symmetry and disorder. Nat Mater. 2007;6:997–1003.
Liao S, Nguyen LT, Ngiam M, Wang C, Cheng Z, Chan CK, et al. Biomimetic nanocomposites to control osteogenic differentiation of human mesenchymal stem cells. Adv Healthc Mater. 2014;3:737–51.
Kilian KA, Bugarija B, Lahn BT, Mrksich M. Geometric cues for directing the differentiation of mesenchymal stem cells. Proc Nat Acad Sci U S A. 2010;107:4872–7.
Zhang ZZ, Chen YR, Wang SJ, Zhao F, Wang XG, Yang F, et al. Orchestrated biomechanical structural and biochemical stimuli for engineering anisotropic meniscus. Sci Transl Med. 2019;11:eaao0750.
Acknowledgment
This article was funded by China Postdoctoral Science Foundation with the number of 2020M670001ZX.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they don’t have any conflict of interest.
Ethical statement
There are no animal experiments carried out for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, G., Zhang, X., Bu, X. et al. The Application of Cartilage Tissue Engineering with Cell-Laden Hydrogel in Plastic Surgery: A Systematic Review. Tissue Eng Regen Med 19, 1–9 (2022). https://doi.org/10.1007/s13770-021-00394-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-021-00394-5