Abstract
Prior studies had reported monocyte to high-density lipoprotein cholesterol ratio (MHR) as a new inflammation marker and stroke-associated pneumonia (SAP) is common after stroke. We investigated the predictive value of MHR for SAP in patients with acute ischemic stroke (AIS). A total of 803 AIS patients within 72 h after stroke were enrolled from April 2012 to January 2016 in Zhangjiagang TCM Hospital affiliated to the Nanjing University of Chinese Medicine. MHR measurement within 24 h of hospital admission was divided into quartiles: Q1 (< 0.21), Q2 (0.21–0.30), Q3 (0.30–0.45), and Q4 (≥ 0.45). Monocyte count was also divided into categories. Clinical outcomes were post-stroke SAP and 3-month mortality. 121 patients (15.1%) experienced SAP during hospitalization, and 109 patients (13.6%) died from all causes within 3 months after AIS. Compared to the lowest quartile, having admission MHR level in the highest quartile was associated with SAP [adjusted odds ratio (aOR) 2.79, 95% confidence interval (CI) 1.44–5.42; P trend = 0.003]. Compared with the lowest category of monocyte, the highest category was associated with a 2.60-fold increase in the odds of SAP (aOR 2.60, 95% CI 1.28–5.30; P trend = 0.005). However, there was no significant association between MHR (P trend = 0.514) and monocyte count (P trend = 0.684) and all-cause mortality at 3 months. We demonstrated that both higher MHR and higher monocyte count at admission predicted SAP in patients with AIS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Stroke is a major cause of disability and mortality worldwide [1]. Pneumonia is one of the most common complications of stroke occurring in approximately 9% of all patients, and up to 28% in the intensive care patients [2]. Previous studies showed a strong association between stroke-associated pneumonia (SAP) with poor outcome and death [3,4,5]. Early risk assessment of SAP is crucial for identifying patients with the highest likelihood of developing SAP and providing them with optimal treatment.
Inflammatory response underlies entire pathophysiological process of ischemic stroke [6], involving the activation of vascular endothelium, breakage of the blood brain barrier, accumulation of oxidizing agent and inflammatory mediator, as well as infiltration of abundant leukocyte and platelets. The inflammatory process gradually develops in several hours, resulting in post-ischemia damages [7, 8]. In particular, the release of inflammatory cytokines and neurotoxins may further worsen neurological function and even cause complications, such as SAP. Recently, several clinical predictive models were developed for the early prediction of SAP, such as A2DS2 score [9], PANTHER-IS score [10], and AIS-APS [11]. However, these predictive models are based on traditional clinical risk factors, and may not be suitable for use in patients with atypical clinical manifestations. Therefore, a more objective and easily obtainable predictor is needed.
Monocyte to high-density lipoprotein (HDL) cholesterol ratio (MHR) has emerged as a novel inflammation marker that is closely linked to cardiovascular and cerebrovascular events. Kanbay et al. [12] reported that high MHR was related to cardiovascular events in patients with chronic renal disease. Canpolat et al. [13] also demonstrated that elevated MHR was an independent risk factor for atrial fibrillation relapse after radiofrequency ablation procedure. In addition, a previous study of 316 acute intracerebral hemorrhage (ICH) patients found that higher baseline MHR was associated with increased risk of disability or death at discharge and at 3 months after ICH [14]. Moreover, Bolayir et al. [15] reported that high MHR was an independent marker for the prediction of 30-day mortality in patients with ischemic stroke. However, the significance of MHR for prediction of SAP and long-term outcome after acute ischemic stroke (AIS) remains uncertain. Thus, we aimed to elucidate the relationship between monocyte count and MHR with SAP and 3-month mortality after AIS.
Materials and methods
Study design and population
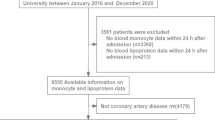
From April 2012 to January 2016, we prospectively identified AIS patients from the Zhangjiagang TCM Hospital Affiliated to Nanjing University of Chinese Medicine in China. Diagnosis of AIS was made according to World Health Organization-defined criteria based on patient history, clinical characteristics, and neuroimaging data (computed tomography or magnetic resonance imaging). A team of investigators, including neurologists, reviewed the eligibility of study participants. Additional exclusion criteria were as follows: (1) time from onset to admission over 72 h (n = 116); (2) diagnosis with fatal brain stem infarction(n = 5); (3) no serum monocyte count or HDL-C data (n = 13); and (4) loss of follow-up at 3 months (n = 14); 803 patients with available data were finally included in this study. (Flowchart of participants selection; Fig. 1).
Ethics statement
This study was approved by the Ethics Committee of the Zhangjiagang TCM Hospital affiliated to the Nanjing University of Chinese Medicine. Written consent was obtained from all study participants or their immediate family members.
Data collection
We collected baseline information, including patient demographics, vascular risk factors, stroke severity (National Institutes of Health Stroke Scale, NIHSS; Modified Rankin Scale score, mRS), medication use, imaging data, and diagnosis-related information. Vascular risk factors included history of stroke, history of hypertension, history of diabetes mellitus, history of atrial fibrillation, history of coronary heart disease, current or previous smoking status, and alcohol consumption.
Blood samples were collected within 24 h of hospital admission. White blood cell (WBC) and monocyte levels were measured by the XE-5000 (Mindray, China). Serum HDL-C and other biochemical parameters were analyzed using Olympus AU5400 automatic biochemical analyzer (First chemical CO, LTD, Japan) with commercial reagents. The MHR was calculated as the ratio of monocyte count to HDL-C level.
Outcomes assessment
In this study, main research outcomes were SAP and 3-month all-cause mortality. Diagnosis of SAP was adjudicated by doctors from neurology and radiology department. Diagnosis mainly referred to the 2015 diagnosis consensus on SAP [16]. Specifically, (1) at least one of the following criteria were met: (a) body temperature of > 38 °C for no reasons, (b) reduction or increase in WBC count to approximately < 4 × 109/Land > 11 × 109/L, respectively. (2) At least two of following criteria were met: (a) new occurrence of purulent sputum, or change in character of sputum over a 24 h period, or increased respiratory secretions, or increased suctioning requirements; (b) new onset or worsening cough, or dyspnea, or tachypnea (respiratory rate > 25/min); (c) rale or bronchial breathing sound can be heard by lung auscultation and (d) deterioration of gas exchange, for example, low oxygen saturation or increase in oxygen inhalation concentration. (3) Based on the combination of X-ray chest images or lung CT anomalies, new occurrence or progressive exudation, consolidation or cavity was found.
Deaths were reported by family members or work associates and/or obtained from death certificates and medical records.
Statistical analysis
Patients were divided into quartiles based on admission MHR (Q1 < 0.21, Q2 0.21–0.30, Q3 0.30–0.45, Q4 ≥ 0.45) and monocyte count (MC) (Q1: < 0.30, 109/L; Q2: 0.30–0.40, 109/L; Q3: 0.40–0.50, 109/L; Q4: ≥ 0.50, 109/L). Continuous variables were expressed as mean ± standard deviation (SD) or median [interquartile range (IQR)], and were compared using the analysis of variance or Wilcoxon rank-sum test. Categorical variables were expressed as frequency (%) and were compared using the Chi-square test.
Associations between quartiles of MHR, MC and the risk of SAP and all-cause mortality at 3 months were estimated using crude and multivariable logistic regression models. Odds ratios (ORs) and 95% confidence interval (CIs) were calculated for each group with the lowest quartiles of MHR and MC (Q1) as reference. We adjusted for potential confounders including age, sex, time from onset to admission, subtype of Oxfordshire Community Stroke Project (OCSP) classification, history of hypertension, history of diabetes mellitus, history of atrial fibrillation, history of stroke, current smoking, current drinking, heart rate, systolic blood pressure (SBP), fasting plasma glucose, and baseline NIHSS score (< 4 vs. ≥ 4). All P values were two tailed, with < 0.05 considered statistically significant. All analyses were conducted using the SPSS Version 17.0 statistical software.
Results
Baseline characteristics of study participants
A total of 803 AIS patients (431men and 372 women) were included in the main analysis. The median age was (69 ± 12.3), and the median NIHSS score was 4.0 (IQR 3.0–7.0). The baseline characteristics of patients by MHR quartiles are shown in Table 1. In comparison to those with lower MHR levels, participants with higher MHR levels were more likely to be male, tended to be smokers, and were more likely to have hypertension. Patients with higher MHR level also differed in metabolic profile [higher white blood cell (WBC) levels and MC levels but lower total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and lower HDL-C levels].
Predictive value of MHR and MC on the risk of SAP
A total of 121 patients (15.1%) presented with pneumonia during hospitalization. In the unadjusted logistic regression model, SAP was significantly higher among study participants with admission MHR in the highest quartile (≥ 0.45) compared with those in the lowest quartile (< 0.21) (OR 1.73, 95% CI 1.01–2.98, P trend = 0.026). After adjusting for age, sex, baseline NIHSS score, and other traditional risk factors, the OR (95% CI) for the highest quartile of MHR at admission was 2.79 (95% CI 1.44–5.42; P trend = 0.003) as compared with the lowest quartile for SAP (Table 2). In the unadjusted logistic regression model, SAP was also significantly higher among study participants with admission MC in the highest quartile (≥ 0.50) compared with those in the lowest quartile (< 0.30) (OR 2.77, 95% CI 1.49–5.13, P trend < 0.001). The relationship between increased MC and SAP was still significant after adjusting for potential confounders (OR 2.60, 95% CI 1.28–5.30, P trend = 0.005) (Table 2).
Association between MHR and MC with 3-month mortality
A total of 109 patients (13.6%) died from all-cause during 3 months follow-up. In the unadjusted logistic regression model, there was no significant association between higher MHR and mortality at 3 months (OR 0.96, 95% CI 0.56–1.64, for highest quartile compared with lowest quartile, P trend = 0.901). We did not observe a significant association between MHR and the 3-month mortality after adjusting for age, sex, baseline NIHSS score, and other traditional risk factors (P trend = 0.514). In the unadjusted logistic regression model, mortality was higher among study participants with admission MC in the highest quartile compared with those in the lowest quartile (OR 1.71, 95% CI 0.96–3.02, P trend = 0.037). However, the relationship between increased MC and 3-month mortality was not significant after adjusting for potential confounders (P trend = 0.684) (Table 3).
Discussion
In this study, we demonstrated that having higher admission MHR and MC were associated with SAP in patients with AIS. However, no significant relationship between MHR and MC with 3-month all-cause mortality was found.
Currently, many prediction models have been developed for the prediction of SAP based on clinical symptoms. First, a study from Germany [9] reported that the A2DS2 score including age, history of atrial fibrillation, dysphagia, male sex, and NIHSS score as risk factors could effectively predict post-stroke pneumonia, especially in high-risk patients. Another study from China [11] showed that the acute ischemic stroke-associated pneumonia score (AIS-APS, accounting for age, history of atrial fibrillation, history of congestive heart failure, history of chronic obstructive pulmonary disease, smoking, stroke history, dysphagia, admission NIHSS score and Glasgow Coma Scale score, stroke subtype, and blood glucose), could also effectively predict SAP. Subsequently, a British study using sizable data also reported that ISAN [17] score (including stroke history, gender, age, and NIHSS score as risk factors) was a simple tool for predicting SAP in patients with ischemic stroke or ICH. ISAN score was equal to A2DS2 score in prediction performance. Nevertheless, these studies mainly predicted SAP based on clinical symptoms in patients with ischemic stroke.
As a strong relationship exists between inflammatory reaction and SAP, some inflammatory markers were reported to predict SAP, such as C-reactive protein [18,19,20]. Recently, some new inflammatory markers had been evaluated in studies of general diseases, including neutrophil to lymphocyte ratio (NLR) and MHR. These inflammatory biomarker values could be obtained from basic laboratory tests and easily calculated. Several studies had indicated that both high NLR and MHR were associated with poor outcome after stroke. Nam et al. [21] reported that having high NLR level at admission was closely related with occurrence and severity of SAP. To the best of our knowledge, no study has investigated the prognostic role of MHR and MC in a large cohort of AIS patients with regard to SAP risk. In our study, we found MHR and MC were independent predictors of SAP.
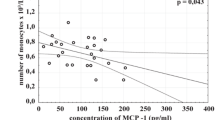
There are several possible explanations for the association between high MHR and MC with SAP. First, animal studies showed that increased monocyte turnover was associated with klebsiella pneumonia clearance and pulmonary tissue damage [22, 23]. Moreover, a growing body of studies suggested that monocytes can develop into terminally differentiated cells to perform versatile functions during infection. It has been reported that monocyte polarize to an M2b phenotype, contributing to the susceptibility of alcoholics to lung infection [24]. Another study [25] found that monocyte chemoattractant protein-1 has displayed good predictive power for community-acquired pneumonia. Furthermore, the MHR has been shown to be associated with many metabolic diseases, such as obstructive sleep apnea syndrome and diabetes, which are also known risk factors for SAP [26, 27].
A study of 466 AIS patients from Turkey showed that a high MHR was an independent predictor of 30-day mortality [15]. However, in this study, the relationship of MHR and MC with 3-month mortality was not significant. The conflicting finding may be partially due to differences in the confounders in the multivariable logistic regression model, the duration of mortality, the ethnicity, and sample size. The baseline NIHSS score and OCSP stroke classification were confounders in multivariable logistic regression in present study but not in Bolayir et al. study [15], which were the significant factors associated with mortality after AIS. In our study, we included 803 AIS patients and investigated the association between MHR and 3 months mortality, while Behrouz et al. study only enrolled 466 patients and reported 1-month mortality.
We recognize that this study has some limitations. First, our study is a single-center retrospective study. Although some possible confounders were accounted for in our multivariable analysis, residual confounding may still exist. Second, this study is based on a relatively small Chinese population and thus our findings may not be generalizable to other populations. Third, the mRS score at 3 months was not measured; therefore, we could not evaluate the relationship between MHR, MC, and major disability. Moreover, a proportion of patients were excluded due to missing data, which may lead to selection bias. Additionally, only patients admitted to hospital 72 h after stroke were selected, and thus the peak MC was not able to be evaluated accurately. Therefore, future prospective studies with larger population and longer period of follow-up are required to validate the current study findings.
Conclusions
High admission MHR and MC are both associated with SAP among patients with acute ischemic stroke, but not all-cause mortality at 3 months. This result may assist in early identification of high-risk patients to provide timely therapeutic intervention, thus reducing the rate of SAP.
References
Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG, Hamdan AD, Higashida RT, Hoh BL, Janis LS, Kase CS, Kleindorfer DO, Lee JM, Moseley ME, Peterson ED, Turan TN, Valderrama AL, Vinters HV (2013) An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44:2064–2089
Hannawi Y, Hannawi B, Rao CP, Suarez JI, Bershad EM (2013) Stroke-associated pneumonia: major advances and obstacles. Cerebrovasc Dis 35:430–443
Teh WH, Smith CJ, Barlas RS, Wood AD, Bettencourt-Silva JH, Clark AB, Metcalf AK, Bowles KM, Potter JF, Myint PK (2018) Impact of stroke-associated pneumonia on mortality, length of hospitalization, and functional outcome. Acta Neurol Scand 138:293–300
Yu YJ, Weng WC, Su FC, Peng TI, Chien YY, Wu CL, Lee KY, Wei YC, Lin SW, Zhu JX, Huang WY (2016) Association between pneumonia in acute stroke stage and 3-year mortality in patients with acute first-ever ischemic stroke. J Clin Neurosci 33:124–128
Vermeij FH, Scholte op Reimer WJ, de Man P, van Oostenbrugge RJ, Franke CL, de Jong G, de Kort PL, Dippel DW (2009) Stroke-associated infection is an independent risk factor for poor outcome after acute ischemic stroke: data from the Netherlands stroke survey. Cerebrovasc Dis 27:465–471
Chamorro A, Hallenbeck J (2006) The harms and benefits of inflammatory and immune responses in vascular disease. Stroke 37:291–293
Kim JY, Park J, Chang JY, Kim SH, Lee JE (2016) Inflammation after Ischemic stroke: the role of leukocytes and glial cells. Exp Neurobiol 25:241–251
Fu Y, Liu Q, Anrather J, Shi FD (2015) Immune interventions in stroke. Nat Rev Neurol 11:524–535
Hoffmann S, Malzahn U, Harms H, Koennecke HC, Berger K, Kalic M, Walter G, Meisel A, Heuschmann PU (2012) Development of a clinical score (A2DS2) to predict pneumonia in acute ischemic stroke. Stroke 43:2617–2623
Harms H, Grittner U, Droge H, Meisel A (2013) Predicting post-stroke pneumonia: the PANTHERIS score. Acta Neurol Scand 128:178–184
Ji R, Shen H, Pan Y, Wang P, Liu G, Wang Y, Li H, Wang Y (2013) Novel risk score to predict pneumonia after acute ischemic stroke. Stroke 44:1303–1309
Kanbay M, Solak Y, Unal HU, Kurt YG, Gok M, Cetinkaya H, Karaman M, Oguz Y, Eyileten T, Vural A, Covic A, Goldsmith D, Turak O, Yilmaz MI (2014) Monocyte count/HDL cholesterol ratio and cardiovascular events in patients with chronic kidney disease. Int Urol Nephrol 46:1619–1625
Canpolat U, Aytemir K, Yorgun H, Sahiner L, Kaya EB, Cay S, Topaloglu S, Aras D, Oto A (2015) The role of preprocedural monocyte-to-high-density lipoprotein ratio in prediction of atrial fibrillation recurrence after cryoballoon-based catheter ablation. Europace 17:1807–1815
You S, Zhong C, Zheng D, Xu J, Zhang X, Liu H, Zhang Y, Shi J, Huang Z, Cao Y, Liu CF (2017) Monocyte to HDL cholesterol ratio is associated with discharge and 3-month outcome in patients with acute intracerebral hemorrhage. J Neurol Sci 372:157–161
Bolayir A, Gokce SF, Cigdem B, Bolayir HA, Yildiz OK, Bolayir E, Topaktas SA (2018) Monocyte/high-density lipoprotein ratio predicts the mortality in ischemic stroke patients. Neurol Neurochir Pol 52:150–155
Smith CJ, Kishore AK, Vail A, Chamorro A, Garau J, Hopkins SJ, Di Napoli M, Kalra L, Langhorne P, Montaner J, Roffe C, Rudd AG, Tyrrell PJ, van de Beek D, Woodhead M, Meisel A (2015) Diagnosis of stroke-associated pneumonia: recommendations from the pneumonia in stroke consensus group. Stroke 46:2335–2340
Smith CJ, Bray BD, Hoffman A, Meisel A, Heuschmann PU, Wolfe CD, Tyrrell PJ, Rudd AG (2015) Can a novel clinical risk score improve pneumonia prediction in acute stroke care? A UK multicenter cohort study. J Am Heart Assoc 4:e001307
Warusevitane A, Karunatilake D, Sim J, Smith C, Roffe C (2016) Early diagnosis of pneumonia in severe stroke: clinical features and the diagnostic role of C-reactive protein. PLoS ONE 11:e0150269
De Raedt S, De Vos A, Van Binst AM, De Waele M, Coomans D, Buyl R, De Keyser J (2015) High natural killer cell number might identify stroke patients at risk of developing infections. Neurol Neuroimmunol Neuroinflamm 2(2):e71
Doll DN, Barr TL, Simpkins JW (2014) Cytokines: their role in stroke and potential use as biomarkers and therapeutic targets. Aging Dis 5(5):294–306
Nam KW, Kim TJ, Lee JS, Kwon HM, Lee YS, Ko SB, Yoon BW (2018) High neutrophil-to-lymphocyte ratio predicts stroke-associated pneumonia. Stroke 49:1886–1892
Xiong H, Keith JW, Samilo DW, Carter RA, Leiner IM, Pamer EG (2016) Innate Lymphocyte/Ly6C(hi) monocyte crosstalk promotes klebsiella pneumoniae clearance. Cell 165:679–689
Cai Y, Sugimoto C, Liu DX, Midkiff CC, Alvarez X, Lackner AA, Kim WK, Didier ES, Kuroda MJ (2015) Increased monocyte turnover is associated with interstitial macrophage accumulation and pulmonary tissue damage in SIV-infected rhesus macaques. J Leukoc Biol 97:1147–1153
Xiong H, Pamer EG (2015) Monocytes and infection: modulator, messenger and effector. Immunobiology 220:210–214
Yong KK, Chang JH, Chien MH, Tsao SM, Yu MC, Bai KJ, Tsao TC, Yang SF (2016) Plasma monocyte chemoattractant protein-1 level as a predictor of the severity of community-acquired pneumonia. Int J Mol Sci 17:179
Inonu Koseoglu H, Pazarli AC, Kanbay A, Demir O (2018) Monocyte count/hdl cholesterol ratio and cardiovascular disease in patients with obstructive sleep apnea syndrome: a multicenter study. Clin Appl Thromb Hemost 24:139–144
Vahit D, Mehmet KA, Samet Y, Huseyin E (2017) Assessment of monocyte to high density lipoprotein cholesterol ratio and lymphocyte-to-monocyte ratio in patients with metabolic syndrome. Biomark Med 11:535–540
Acknowledgements
We thank the study participants and their relatives and the clinical staff for their support and contribution to this study.
Funding
This work was supported in part by Grants from the National Natural Science Foundation of China (81901198), Basic research of Suzhou Medical and health care (SYS201724) and Natural Science Foundation for Higher Education of Jiangsu Province of China (19KJB320004).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the Ethics Committee of the Zhangjiagang TCM Hospital affiliated to the Nanjing University of Chinese Medicine.
Informed consent
Written consent was obtained from all study participants or their immediate family members.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, Y., Lu, J., Zheng, D. et al. Predictive value of monocyte to HDL cholesterol ratio for stroke-associated pneumonia in patients with acute ischemic stroke. Acta Neurol Belg 121, 1575–1581 (2021). https://doi.org/10.1007/s13760-020-01418-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-020-01418-y