Abstract
Trigeminal neuralgia (TN) recurring after surgery can be difficult to treat. Treatment algorithms have not been standardized or universally accepted. Here we investigated the effectiveness of percutaneous balloon compression (PBC) in the treatment of patients with TN recurrence after other surgical techniques and analyzed the role of some clinical and operative factors in determining the prognosis. The records of 22 patients (13 M and 9 F) suffering recurrent TN after one (2 gamma knife surgery, 5 percutaneous radiofrequency rhizotomy, 6 percutaneous retrogasserian glycerol rhizotomy, 3 microvascular decompression) or more (6 patients) procedures and submitted to PBC at our institution from January 2003 to February 2012 were reviewed. Seven patients had TN related to multiple sclerosis (MS). Mean follow-up was 51.81 ± 26.63 months. 81.81 % of patients reported an acute pain relief. No major complication was observed after PBC. Eight patients (36.36 %) experienced pain recurrence and underwent one (five patients) or more (three patients) PBC. At the last follow-up, we obtained an excellent outcome (BNI I–II) in 16 patients out of 22 (72.72 %) and a good outcome (BNI III) in the remaining six. No patients had an uncontrolled pain. The lack of history of MS (p = 0.0174), the pear-like shape of the balloon at the operation (p = 0.0234) and a compression time <5 min (p < 0.05) were associated to higher pain-free survival. Considering these results PBC could be considered a useful technique for patients whose pain recurs after other procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A general consensus exists on the utility of percutaneous balloon compression (PBC) to treat patients with drug-resistant trigeminal neuralgia (TN) both in general population [1] and in multiple sclerosis [2, 3]. Nonetheless, some authors suggested lower efficacy of PBC after other surgical procedures [4, 5]. As a matter of fact this topic has been focused only in two papers [6, 7] and considered only marginally by other authors [8–13]. We report on the effectiveness of PBC in patients with TN recurrence after other surgical procedures. We also analyze potential prognostic factors and discuss our results and the pertinent literature.
Methods
We retrospectively analyzed 22 patients (13 M and 9 F) suffering recurrent TN after one or more procedures and submitted to PBC at our institution from January 2003 to February 2012. The mean age was 60.95 ± 13.54 years with a mean follow-up of 51.81 ± 26.63 months. Seven patients had MS-related TN. TN duration before the PBC was 13.94 ± 9.45 years and the pain was atypical in three patients. Eleven cases had a pre-operative hypoesthesia. Six patients had undergone two or more procedures before PBC. Patient’s clinical data are summarized in Table 1. Patients reported their pain as the worst possible pain. The operation was performed under general anesthesia and fluoroscope image intensifier using a 14-gauge needle and a Fogarty balloon catheter 4-French filled with 0.75 ml of medium of contrast with a compression time ranging from 1 to 12 min (Table 1), as previously reported [14, 15]. As outcome indicators, we used the acute pain relief (APR: pain-free at hospital discharge) and pain-free survival (PFS). At follow-up, the outcome was evaluated using the Barrow Neurological Institute (BNI) pain scale [16].
Moreover, we investigated the role of sex, history of MS, TN type, number of affected trigeminal divisions, pre-operative deficit, number and type of previous operations, compression time (<5 min vs. ≥5 min), balloon shape at operation (pear-like vs elliptical) as potential prognostic factors. A comparison of categorical variables was performed by Chi-square statistic. Kaplan–Meier curves were plotted and differences in pain-free survival between groups of patients were compared using the log-rank test. p values <0.05 were considered as statistically significant.
Results
Eighteen out of twenty-two patients (81.81 %) reported an APR. No major complication was observed after the procedure. Four patients complained of mild worsening (#7, #12, #22) or onset (#15) of hypoesthesia (see Table 1). None of the considered potential prognostic factors was associated to a higher probability of APR.
Eight patients (36.36 %) experienced a recurrence of pain with a mean pain-free survival of 20.12 ± 17.87 months. All of them were further submitted to one (#2, #7, #14, #19, #21) or more (#4, #9, #10) PBC (see Table 2).
At latest follow-up (mean 51.81 ± 26.63 months), patients who did not recur after the first PBC (63.64 %) showed an excellent (BNI I–II) or good (BNI III) outcome in ten (#1, #3, #5, #6, #11, #12, #13, #15, #16, #20) and in four (#8, #17, #18, #22) cases, respectively.
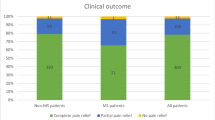
Overall we obtained an excellent outcome (BNI I–II) in 16 patients out of 22 (72.72 %) and a good outcome (BNI III) in the remaining ones. No patients had an uncontrolled pain (see Table 2).
Among possible prognostic factors, the lack of history of MS (p = 0.0174), the pear-like shape of the balloon at the operation (p = 0.0234) and a compression time <5 min (p < 0.05) were associated to higher pain-free survival (Fig. 1).
Kaplan–Meier curves of patients submitted to PBC and stratified by a history of MS, b balloon shape at operation and c compression time. The lack of history of MS (p = 0.0174), the pear-like shape of the balloon at the operation (p = 0.0234) and a compression time <5 min (p < 0.05) were associated to higher pain-free survival
Discussion
TN is a facial pain syndrome characterized by paroxysmal, shock like pain attacks located in the somatosensory distribution of the trigeminal nerve whose prevalence is 0.015 % [17] in the general population and 1 % [5] to 6.3 % in MS patients [18]. From its introduction by Mullan et al. [19, 20], PBC has been extensively used to treat TN patients due to low-cost, simplicity and the advantage of being the only percutaneous procedure performed with the patient under general anesthesia. While there is a general consensus about the usefulness of PBC either in general population [1] or in MS patients [2, 3], some authors suggested [4, 5] a lower efficacy in patients previously treated with other surgical procedures. However, the results of PBC in this subset of patients have previously been reported only marginally in the literature [8–13] and only two papers [6, 7] specifically focused on this topic.
In their work Kouzounias et al. [6] studied 47 patients (42 with previous operations) and reported the follow-up after the first PBC for each patient. They observed an 85 % initial success rate with 70 % of patients experiencing pain recurrence. Similarly Omeis et al. [7] reported an 83 % immediate pain relief after PBC in a series of 29 patients with 45.5 % of recurrence rate.
In our study, we observed an APR of 81.81 % with a recurrence rate of 36.36 %. Moreover, we found that repeating PBC was very useful in these patients because we obtained an excellent (BNI I–II)–good (BNI III) response after a single or multiple procedures in all patients (see Table 2).
In agreement with other reports [3, 6] the pear-like shape of the balloon at the operation was found to be a good prognostic factor. These data likely reflect an engagement of the balloon within the porus trigeminus producing a better compression of the retrogasserian root.
Even if we observed that the history of MS was associated with lower pain-free survival, we obtained a control of pain with repeating the procedure also in these patients [2, 3, 6].
Moreover, we found that a compression time <5 min was associated to better pain-free survival, confirming that a longer compression time did not affect the pain relief and only increase the complication rate [9, 14, 21].
Other techniques for the treatment of recurrent TN have been proposed. Recently Zhang et al. [22] reported that radiofrequency thermocoagulation rhizotomy was effective for recurrent TN after a failed microvascular decompression (MVD). Nonetheless MVD has been advised in patient with recurrent TN if other less invasive procedures have not relieved the facial pain [23, 24]. Most of published studies on recurrent TN after a failed previous procedure are focused on the role of gamma knife radiosurgery (GKS) [25–28]. However the reported data are difficult to compare due to differences in dose [29, 30] and target location [31, 32]. Thus, evaluating the potentially prognostic factors associated to GKS is difficult. Despite these limitations, these studies suggest that repeating GKS provides a similar rate of pain relief as the first procedure [27] and that initial failed treatment is not a factor affecting the pain control [26]. Moreover, the development of sensory loss seems to predict better long-term pain control [25, 27, 28]. These data could be explained by the mechanism of pain relief after GKS probably related to a diffuse damage of all axons of trigeminal nerve [33]. It has also been suggested that after GKS pain sensation could be not conveyed because of a raising of pain threshold rather than a selective destruction of pain transmission fibers, like percutaneous procedures [34].
PBC is well accepted by patients with mild side effects [7] and good results after one or more operations. In our opinion this makes PBC a useful technique for patients whose pain recurs after other surgical procedures [35].
References
Tatli M, Satici O, Kanpolat Y, Sindou M (2008) Various surgical modalities for trigeminal neuralgia: literature study of respective long-term outcomes. Acta Neurochir (Wien) 150:243–255
Montano N, Papacci F, Cioni B, Di Bonaventura R, Meglio M (2013) What is the best treatment of drug-resistant trigeminal neuralgia in patients affected by multiple sclerosis? A literature analysis of surgical procedures. Clin Neurol Neurosurg 115:567–572
Montano N, Papacci F, Cioni B, Di Bonaventura R, Meglio M (2012) Percutaneous balloon compression for the treatment of trigeminal neuralgia in patients with multiple sclerosis. Analysis of the potentially prognostic factors. Acta Neurochir (Wien) 154:779–783
Jellish WS, Benedict W, Owen K, Anderson D, Fluder E, Shea JF (2008) Perioperative and long-term operative outcomes after surgery for trigeminal neuralgia: microvascular decompression vs percutaneous balloon ablation. Head Face Med 2:4–11
Skirving DJ, Dan NG (2001) A 20-year review of percutaneous balloon compression of the trigeminal ganglion. J Neurosurg 94:913–917
Kouzounias K, Schechtmann G, Lind G, Winter J, Linderoth B (2010) Factors that influence outcome of percutaneous balloon compression in the treatment of trigeminal neuralgia. Neurosurgery 67:925–934
Omeis I, Smith D, Kim S, Murali R (2008) Percutaneous balloon compression for the treatment of recurrent trigeminal neuralgia: long-term outcome in 29 patients. Stereotact Funct Neurosurg 86:259–265
Bergenheim AT, Asplund P, Linderoth B (2013) Percutaneous retrogasserian balloon compression for trigeminal neuralgia: review of critical technical details and outcomes. World Neurosurg 79:359–368
Brown JA, Pilitsis JG (2005) Percutaneous balloon compression for the treatment of trigeminal neuralgia: results in 56 patients based on balloon compression pressure monitoring. Neurosurg Focus 18:E10
Campos WK, Linhares MN (2011) A prospective study of 39 patients with trigeminal neuralgia treated with percutaneous balloon compression. Arq Neuropsiquiatr 69:221–226
Chen JF, Tu PH, Lee ST (2011) Long-term follow-up of patients treated with percutaneous balloon compression for trigeminal neuralgia in Taiwan. World Neurosurg 76:586–591
Stomal-Słowińska M, Słowiński J, Lee TK, Uitti RJ, Deen HG, Reimer R, Cheshire WP Jr, Herzog-Bryan G, Wharen RE Jr (2011) Correlation of clinical findings and results of percutaneous balloon compression for patients with trigeminal neuralgia. Clin Neurol Neurosurg 113:14–21
Trojnik T, Ŝmigoc T (2012) Percutaneous trigeminal ganglion balloon compression rhizotomy: experience in 27 patients. Sci World J. doi:10.1100/2012/328936
Meglio M, Cioni B (1989) Percutaneous procedures for trigeminal neuralgia: microcompression versus radiofrequency thermocoagulation. Personal experience. Pain 38:9–16
Meglio M, Cioni B, Moles A, Visocchi M (1990) Microvascular decompression versus percutaneous procedures for typical trigeminal neuralgia: personal experience. Stereotact Funct Neurosurg 54–55:76–79
Ruge D, Brochner R, Davis L (1958) A study of the treatment of 637 patients with trigeminal neuralgia. J Neurosurg 15:528–536
Penman J (1968) Trigeminal neuralgia. In: Vinken PJ, Bruyn GW (eds) Handbook of clinical neurology, vol 5. North-Holland Publishing Company, Amsterdam, pp 296–322
Putzki N, Pfriem A, Limmroth V, Yaldizli O, Tettenborn B, Diener HC, Katsarava Z (2009) Prevalence of migraine, tension-type headache and trigeminal neuralgia in multiple sclerosis. Eur J Neurol 16:262–267
Mullan S, Duda EE, Patronas NJ (1980) Some examples of balloon technology in neurosurgery. J Neurosurg 52:321–329
Mullan S, Lichtor T (1983) Percutaneous microcompression of the trigeminal ganglion for trigeminal neuralgia. J Neurosurg 59:1007–1012
Park SS, Lee MK, Kim JW, Jung JY, Kim IS, Ghang CG (2008) Percutaneous balloon compression of trigeminal ganglion for the treatment of idiopathic trigeminal neuralgia: experience in 50 patients. J Korean Neurosurg Soc 43:186–189
Zhang LW, Liu YG, Wu CY, Xu SJ, Zhu SG (2011) Radiofrequency thermocoagulation rhizotomy for recurrent trigeminal neuralgia after microvascular decompression. Chin Med J (Engl) 124:3726–3730
Amador N, Pollock BE (2008) Repeat posterior fossa exploration for patients with persistent or recurrent idiopathic trigeminal neuralgia. J Neurosurg 108:916–920
Pollock BE, Stein KJ (2010) Surgical management of trigeminal neuralgia patients with recurrent or persistent pain despite three or more prior operations. World Neurosurg 73:523–528
Kano H, Kondziolka D, Yang HC, Zorro O, Lobato-Polo J, Flannery TJ, Flickinger JC, Lunsford LD (2010) Outcome predictors after gamma knife radiosurgery for recurrent trigeminal neuralgia. Neurosurgery 67:1637–1644
Huang CF, Chiou SY, Wu MF, Tu HT, Liu WS (2010) Gamma knife surgery for recurrent or residual trigeminal neuralgia after a failed initial procedure. J Neurosurg 113(Suppl):172–177
Park KJ, Kondziolka D, Berkowitz O, Kano H, Novotny J Jr, Niranjan A, Flickinger JC, Lunsford LD (2012) Repeat gamma knife radiosurgery for trigeminal neuralgia. Neurosurgery 70:295–305
Aubuchon AC, Chan MD, Lovato JF, Balamucki CJ, Ellis TL, Tatter SB, McMullen KP, Munley MT, Deguzman AF, Ekstrand KE, Bourland JD, Shaw EG (2011) Repeat gamma knife radiosurgery for trigeminal neuralgia. Int J Radiat Oncol Biol Phys 81:1059–1065
Hasegawa T, Kondziolka D, Spiro R, Flickinger JC, Lunsford LD (2002) Repeat radiosurgery for refractory trigeminal neuralgia. Neurosurgery 50:494–500
Shetter AG, Rogers CL, Ponce F, Fiedler JA, Smith K, Speiser BL (2002) Gamma knife radiosurgery for recurrent trigeminal neuralgia. J Neurosurg 97(5 Suppl):536–538
Gellner V, Kurschel S, Kreil W, Holl EM, Ofner-Kopeinig P, Unger F (2008) Recurrent trigeminal neuralgia: long term outcome of repeat gamma knife radiosurgery. J Neurol Neurosurg Psychiatry 79:1405–1407
Urgosik D, Liscak R, Novotny J Jr, Vymazal J, Vladyka V (2005) Treatment of essential trigeminal neuralgia with gamma knife surgery. J Neurosurg 102(Suppl):29–33
Regis J, Metellus P, Hayashi M, Roussel P, Donnet A, Bille-Turc F (2006) Prospective controlled trial of gamma knife surgery for essential trigeminal neuralgia. J Neurosurg 104:913–924
Park YS, Kim JP, Chang WS, Kim HY, Park YG, Chang JW (2011) Gamma knife radiosurgery for idiopathic trigeminal neuralgia as primary vs. secondary treatment option. Clin Neurol Neurosurg 113:447–452
Chen JF, Tu PH, Lee ST (2012) Repeated percutaneous balloon compression for recurrent trigeminal neuralgia: a long-term study. World Neurosurg 77:352–356
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Montano, N., Papacci, F., Cioni, B. et al. The role of percutaneous balloon compression in the treatment of trigeminal neuralgia recurring after other surgical procedures. Acta Neurol Belg 114, 59–64 (2014). https://doi.org/10.1007/s13760-013-0263-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-013-0263-x