Abstract
Polypoid endometriosis is a distinctive variant of endometriosis with histological features simulating those of endometrial polyps. Müllerianosis is characterized by the presence of lesions at any site containing admixtures of endosalpingiosis, endometriosis, and endocervicosis. Here, we report a rare case of polypoid endometriosis of the ovary with müllerianosis of the pelvic lymph nodes in a 44-year-old woman without a past history of pelvic surgery. Magnetic resonance imaging revealed an ovarian tumor containing papillary nodules up to 3.0 cm in diameter and left pelvic lymph node enlargement. Nodules in ovarian tumor showed heterogeneous high intensity on T2-weighted image and high intensity on diffusion-weighted image and were mildly enhanced by gadolinium contrast material. Enlarged lymph node was markedly enhanced by gadolinium. We considered polypoid endometriosis in the differential diagnosis according to the results of the magnetic resonance imaging, and polypoid endometriosis was included in intraoperative consultation, however, ovarian carcinoma with lymph node metastasis could not be denied. According to histological examination, the final diagnosis was determined as polypoid endometriosis with glandular hyperplasia of the left ovary and müllerianosis in the obturator lymph nodes. To the best of our knowledge, this is the first report of polypoid endometriosis and müllerianosis of the pelvic lymph node.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polypoid endometriosis was first described by Mostoufizadeh and Scully as a distinctive variant of endometriosis with histological features simulating those of endometrial polyps [1]. Endometriosis is a benign inflammatory disease defined as the presence of endometrial glands and stroma outside the uterine cavity. Polypoid endometriosis can be mistaken for neoplasia on clinical, intraoperative, and pathological examinations.
On the other hand, müllerianosis was first described by Young and Clement as lesions seen at any site containing admixtures of endosalpingiosis, endometriosis, and endocervicosis [2]. Müllerianosis composed of nonneoplastic müllerian glands is a benign tumor-like lesion. It is most commonly found in the urinary bladder [3], however, it may also occur at other sites, such as the ureter [4], mesosalpinx [5], inguinal lymph nodes [6], spinal code [7], and uterus [8].
Here, we report a rare case of a patient with polypoid endometriosis of the ovary with müllerianosis of the pelvic lymph nodes, mimicking an ovarian carcinoma with lymph node metastasis.
Case report
A 44-year-old woman, gravida 2 para 1, who presented with swelling in the lower abdomen, visited another hospital. Bilateral ovarian tumors were detected by transvaginal ultrasound and magnetic resonance imaging (MRI). She was referred to our hospital for further evaluation and management. She was diagnosed with adenomyosis at 40 years of age and had no history of pelvic surgery.
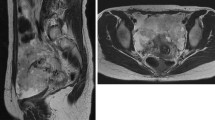
Biochemical analyses demonstrated an elevated serum cancer antigen (CA) 125 level of 261 U/ml and CA19-9 level of 78 U/ml. MRI demonstrated the presence of ovarian cystic tumors bilaterally. Cystic fluid showed high intensity on T1-weighted images (T1-WI) and heterogeneous low intensity on T2-weighted images (T2-WI). The right ovarian tumor was multilocular, and the left ovarian tumor contained papillary nodules, measuring 3.0 cm in the greatest diameter. These nodules showed heterogeneous high intensity on T2-WI and high intensity on diffusion-weighted imaging and were mildly enhanced by gadolinium contrast material. MRI also revealed a left pelvic enlarged lymph node nearby the left ovarian tumor, measuring 1.2 cm in short axis, with marked enhancement (Fig. 1a–d). Computed tomography (CT) revealed no distant metastasis. The preoperative diagnosis was ovarian carcinoma, including clear cell carcinoma, endometrioid carcinoma, and seromucinous borderline tumor with lymph node metastasis or polypoid endometriosis.
The imaging findings of pelvis obtained by magnetic resonance imaging. a On axial T1-weighted image, bilateral ovarian cystic tumors showing high intensity. The right ovarian tumor was multilocular (arrow). The left ovarian tumor contained low-signal-intense papillary nodules up to 3.0 cm in diameter (arrowhead). These nodules showed heterogeneous high intensity (arrow) on axial T2-weighted image (b) and high intensity (arrow) on diffusion-weighted image (c) and were enhanced (arrow) on axial gadolinium-enhanced and fat-suppressed T1-weighted image (d). Left pelvic enlarged lymph node with marked enhancement existed nearby the ovarian tumor (arrowhead) (d)
On laparotomy, the left ovarian tumor was observed to have progressed into the retroperitoneum and contained solid nodules (Fig. 2). As the left obturator lymph node was found to be enlarged, measuring 1.5 cm in the greatest diameter, which were suspected of metastasis, and the left ovarian tumor was considered most likely to be an endometrioid borderline tumor or polypoid endometriosis on intraoperative consultation, we performed bilateral salpingo-oophorectomy, hysterectomy, omentectomy, left pelvic lymphadenectomy and a right pelvic lymph node biopsy. Microscopic examination of the nodule from the left ovary demonstrated proliferation of endometrial-type glands similar to endometrial hyperplasia and the presence of endometrial stroma with fibrosis. Neither the glands nor stromal cells had cellular atypia (Fig. 3a, b). The enlarged left obturator lymph node consisted of an admixture of variably sized glands that resembled tubal-type and endometrial-type epithelium with endometrial stroma (Fig. 3c–e). Therefore, the final diagnosis was determined as polypoid endometriosis and glandular hyperplasia of the left ovary and müllerianosis in the obturator lymph nodes.
Microscopic findings of polypoid endometriosis in the left ovary (a, b) and müllerianosis in the obturator lymph node (c, d, e). a The nodule in the left ovarian tumor had multiple cysts (Hematoxylin and Eosin stain (H&E), ×20). b The cyst consisted of endometrial type glands similar to endometrial hyperplasia and endometrial stroma with fibrosis (H&E, ×100). c The enlarged left obturator lymph node consisted of variably sized glands that resembled tubal-type (arrow; d) and endometrial-type epithelium with surrounding endometrial stroma (arrowhead: e) (H&E, ×20; c, H&E, ×100; d, e)
Discussion
Polypoid endometriosis was first described by Mostoufizadeh and Scully as a distinctive variant of endometriosis with histological features simulating those of endometrial polyps [1]. Parker et al. reviewed 24 patients with polypoid endometriosis and reported several clinicopathological differences when compared with typical endometriosis [9]. They showed that polypoid endometriosis usually occurs in older women (60% of patients were aged >50 years) and posited an association between polypoid endometriosis and hormone therapy, including tamoxifen treatment. The present patient was a 44-year-old woman who had not previously received hormone treatment. Polypoid endometriosis may be mistaken for ovarian cancer on imaging, because of solid nodule. MRI findings that may differentiate polypoid endometriosis from endometriosis-related ovarian carcinoma include a round, solid nodule with a smooth shape and high signal intensity with a low-signal-intense marginal edge on T2-WI [10]. In the present patient, we did not see a low signal intense margin of the tumor, however, the nodules demonstrated heterogeneous high intensity on T2-WI, and we could included polypoid endometriosis in the differential diagnosis. Solid portion of epithelial borderline ovarian tumors also shows high intensity on T2-WI [11], the precise histological differential diagnosis between polypoid endometriosis and epithelial borderline tumor is difficult. Microscopically, regions of polypoid endometriosis were composed of an admixture of endometrial glands and stroma. The glandular epithelium demonstrated various architectural patterns and degrees of cytologic atypia. While hyperplastic, metaplastic, and atypical glandular epithelium can be observed in endometriosis of the usual type, these findings appear to be more common in polypoid endometriosis [9]. In some patients, malignant tumors arise from polypoid endometriosis; however, the risk of progression of polypoid endometriosis to neoplasia appears to be rarer than that of typical endometriosis [9, 12].
On the other hand, müllerianosis was first described by Young and Clement [2]. For the diagnosis of müllerianosis, the presence of an admixture of at least two types of müllerian epithelium is necessary. Müllerianosis is most commonly observed in the urinary bladder. Müllerianosis affecting the lymph nodes is very rare, with only one previous report involving inguinal lymph nodes. The pathogenesis of müllerianosis remains unclear. Implantation, metaplastic, and developmental theories have been proposed. The theory of implantation proposed by Young and Clement may explain cases associated with previous pelvic surgery, particularly cesarean section [2]. Another theory of metaplastic proposed by Donne posits the presence of multiple müllerian components that may result from the differentiation of müllerian epithelium [13]. The theory of metaplastic is supported by a case described by Koren et al. [14] that demonstrated morphological continuity between the glands of müllerianosis and that of glandular cystitis. The theory of development was proposed by Batt et al. who redefined müllerianosis as an organoid structure of embryonic origin; a choristoma composed of müllerian rests singly or in combination, incorporated within other normal organs during organogenesis [15]. According to their criteria, müllerianosis can be diagnosed with certainty when the following three conditions are met: (1) no evidence of pelvic endometriosis; (2) no direct communications with the endocervix, endometrium, or endosalpinx; and (3) no history of surgery on the reproductive organs. The present patient had no history of surgery, and her case was complicated by endometriosis. Taking this into account, the theory of implantation and development cannot be applied to the present patient. Furthermore, Sinkre et al. proposed that glandular elements with a müllerian phenotype in pelvic lymph nodes most likely represent a metaplastic change of peritoneal mesothelium [6]. Therefore, we believe that the findings in the present patient support the theory of metaplastic pathogenesis.
In summary, we report a rare case of a patient with polypoid endometriosis of the ovary with müllerianosis of the pelvic lymph nodes. Polypoid endometriosis was included in the preoperative MRI and intraoperative consultation. However, ovarian malignant tumor could not be excluded not only by MRI but also by intraoperative frozen section. To the best of our knowledge, this is the first report of polypoid endometriosis accompanied by müllerianosis.
References
Mostoufizadeh M, Scully RE (1980) Malignant tumors arising in endometriosis. Clin Obstet Gynecol 23:951–963
Young RH, Clement PB (1996) Mülleriannosis of the urinary bladder. Mod Pathol 9:731–737
Branca G, Barresi V (2014) Müllerianosis of the urinary bladder: a rare tumorlike lesion. Arch Pathol Lab Med 138:432–436
Li WM, Yang SF, Lin HC et al (2007) Müllerianosis of ureter: a rare cause of hydronephrosis. Urology 69:1208.e9–1208.e11
Lim S, Kim JY, Park K et al (2003) Müllerianosis of the mesosalpinx: a case report. Int J Gynecol Pathol 22:209–212
Sinkre P, Hoang MP, Albores-Saavedra J (2002) Müllerianosis of inguinal lymph nodes: report of a case. Int J Gynecol Pathol 21:60–64
Barresi V, Cerasoli S, Vitarelli E et al (2006) Spinal intradural müllerianosis: a case report. Histol Histopathol 21:1111–1114
Jayalakshmy PS, Velusamy S, Augustine J (2014) Multiloculated cystic mullerianosis of uterus: a case report. J Turk Ger Gynecol Assoc 15:197–200
Parker RL, Dadmanesh F, Young RH et al (2004) Polypoid endometriosis: a clinicopathologic analysis of 24 cases and a review of the literature. Am J Surg Pathol 28:285–297
Yamada Y, Miyamoto T, Horiuchi A et al (2014) Polypoid endometriosis of the ovary mimicking ovarian carcinoma dissemination: a case report and literature review. J Obstet Gynaecol Res 40:1426–1430
Kataoka M, Togashi K, Koyama T et al (2002) MR imaging of müllerian mucinous borderline tumors arising from endometriotic cyst. J Comput Assist Tomogr 26:532–537
Hansen K, Simon RA, Lawrence WD et al (2012) Unilateral pelvic mass presenting in postmenopausal patients: report of two unusual cases. Ann Diagn Pathol 16:298–301
Donne C, Vidal M, Buttin X et al (1998) Müllerianosis of the urinary bladder: clinical and immunohistochemical findings. Histopathology 33:290–292
Koren J, Mensikova J, Mukensnabl P et al (2006) Müllerianosis of the urinary bladder: report of a case with suggested metaplastic origin. Virchows Arch 449:268–271
Batt RE, Smith RA, Buck Louis GM et al (2007) Müllerianosis. Histol Histopathol 22:1161–1166
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Iida, Y., Tabata, J., Yorozu, T. et al. Polypoid endometriosis of the ovary and müllerianosis of pelvic lymph nodes mimicking an ovarian carcinoma with lymph node metastasis. Int Canc Conf J 6, 145–148 (2017). https://doi.org/10.1007/s13691-017-0295-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13691-017-0295-9