Abstract
Purpose of Review
This review examines the food addiction model and the role of food hedonic pathways in the pathogenesis and treatment of obesity.
Recent Findings
The hedonic pathway interacts with the obesogenic environment to override homeostatic mechanisms to cause increase in body weight. Weight gain sustained over time leads to “upward setting” of defended level of body-fat mass. There are neurobiological and phenotypic similarities and differences between hedonic pathways triggered by food compared with other addictive substances, and the entity of food addiction remains controversial. Treatment for obesity including pharmacotherapy and bariatric surgery impacts on neural pathways governing appetite and hedonic control of food intake. The food addiction model may also have significant impact on public health policy, regulation of certain foods, and weight stigma and bias.
Summary
Recent rapid progress in delineation of food hedonic pathways advances our understanding of obesity and facilitates development of effective treatment measures against the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a serious chronic relapsing disease that leads to numerous metabolic and mechanical complications including type 2 diabetes, hypertension, hyperlipidemia, cardiovascular disease, non-alcoholic fatty liver disease, obstructive sleep apnea, osteoarthritis, and certain cancers [1]. The considerable social, psychological, and economic burden that obesity places upon the individual and society is also well recognized.
The underlying causes of the obesity epidemic are complex, multifactorial, and have both genetic and environmental influences. On the one hand, twin studies have shown that BMI and adiposity have high heritability rates of 25–50% [2]. On the other hand, most genetic variants identified in genome-wide association studies explain only a small proportion of variance in interindividual BMI [3]. The modern urban environment, with its wide availability and increased intake of palatable, energy-dense food and reduced physical activity, is often cited as a major contributing factor in the obesity epidemic [4]. However, numerous other aspects of our environment also contribute, and assigning proportional blame is problematic [5].
Although food addiction was described more than 60 years ago [6], there has been a surge in interest in the concept of food addiction in recent years by the scientific community and healthcare professionals. The concept of food addiction has also gained traction amongst the lay public as it provides an explanatory narrative for those with difficulty adhering to caloric restriction required for weight loss [7]. In the food addiction model, certain foods, typically energy dense with high salt, sugar, or fat content, have addictive qualities which lead to overeating, weight gain, and obesity.
In this paper, we aim to review recent literature on the relevance and integration of homeostatic and hedonic systems in the pathogenesis of obesity. We examine the neurobiological and phenotypic similarities and differences between hedonic pathways triggered by food compared with other addictive substances. We explore the effect of pharmacotherapy and bariatric surgery on these neural pathways, and how they interact with gut hormonal changes. We also review the implications of food addiction model on broader public health measures and regulations of certain types of foods. We conclude by examining the way in which the concept of food addiction affects stigma and bias by both healthcare professionals and the lay public towards patients with obesity.
Homeostatic and Hedonic Systems in Obesity
Homeostatic Energy Balance Circuitry
The hypothalamus is the key brain area that controls energy intake and expenditure via two sets of antagonistic neurons: agouti-related peptide (AgRP) neurons to promote feeding and pro-opiomelanocortin (POMC) neurons to decrease feeding [8]. These neurons receive feedback and integrate signals from a complex network of peripheral neuropeptide hormones including leptin, ghrelin, cholecystokinin, peptide YY, insulin, pancreatic polypeptide, and glucagon-like peptide 1 (GLP-1) to regulate energy balance and body weight [4, 9]. The long-term precision of energy balance required to maintain weight stability has led to the hypothesis of “set point” of body weight regulation, with an active feedback mechanism linking adiposity to energy intake and expenditure [10]. This homeostatic feedback mechanism is evident in the physiological neuro-hormonal changes that occur following weight loss that drive food-seeking behavior to increase energy intake, whilst simultaneously reducing energy expenditure [9]. These physiological adaptations provide ideal conditions for weight regain and explain the limited efficacy of lifestyle interventions in effecting durable weight loss. However, the set-point model does not explain the increase in obesity prevalence over the recent decades, which coincided with significant change in environment and a shift in work and social practices favoring a more sedentary lifestyle.
Hedonic Controls of Appetite and Food Intake
In our modern environment, eating often occurs even in the absence of hunger. This “non-homeostatic” or “hedonic” eating refers to food intake that is not regulated by metabolic feedback and is related to cognitive, reward, and emotional factors [11]. Key components of this hedonic pathway are located in the cortico-limbic areas of the brain and include the nucleus accumbens and caudate nucleus (dopaminergic reward pathways which govern anticipation and motivation); amygdala and hippocampus (learning); anterior insula (sensory processing); and orbitofrontal cortex (reward value appraisal, executive control, and decision-making) [11]. Apart from influencing energy balance, the cortico-limbic circuitry plays many vital roles including memory, learning, and emotional regulation [12]. Weight-loss pharmacotherapy and bariatric surgery which affect the hedonic pathways therefore have potential for unintended neuropsychiatric adverse effects, which are explored later in this review.
Integration of Homeostatic and Hedonic Pathways
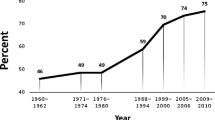
The homeostatic and hedonic pathways interact; peripheral hormones involved in energy homeostasis such as leptin, insulin, and ghrelin can modulate the activity of the mesolimbic dopamine system [13]. It has been hypothesized that hypothalamic AgRP and POMC neurons may not directly drive eating, but rather these signals are mediated by the brain reward circuitry in response to food and other cues in the environment [14]. The interaction between homeostatic and hedonic systems, shown in Fig. 1, could at least partially explain the relatively recent obesity epidemic, whereby the ubiquitous marketing of abundant, cheap, nutrient-poor, energy-dense foods overwhelms cognitive restraints and overrides homeostatic mechanisms, leading to weight gain. Subsequently, there is an upward drift of the set point, leading to higher maintained body weight [15]. The food industry expends tremendous effort to manipulate the salt, sugar, fat, and other additives in products to enhance their rewarding properties [16]. However, despite similar environmental conditions, some individuals are more susceptible than others to weight gain, and it has been suggested that the hedonic system may play an important role in influencing food intake and development of obesity [17].
Interaction between homeostatic and hedonic mechanisms in the regulation of body weight and development of obesity. Green boxes depict the homeostatic circuitry governing energy balance and body weight. The feedback mechanisms to defend body weight in response to weight loss is stronger than to weight gain, as indicated by the size of green arrows. The hedonic pathway interacts with the obesogenic environment to override homeostatic mechanisms to cause increase in body weight. Weight gain sustained over time leads to upward setting of defended level of body-fat mass
In appetite research, these hedonic processes have been explored using functional magnetic resonance imaging (fMRI) [18]. Greater activation of the hedonic pathways on fMRI in response to food images has been shown to influence satiety and food consumption [18, 19], predict short-term weight loss [20, 21] or weight gain [22], and was associated with successful maintenance of ≥ 13.6 kg (30 lb.) weight loss over 3 years or more [23]. On the other hand, cross-sectional studies involving individuals with obesity or binge-eating disorder have shown inconsistent findings on activation of the different areas of the reward circuitry in response to food-related stimuli [24], which complicates the role of hedonic systems in obesity. Most of these studies had small sample sizes, and there was significant heterogeneity in age, gender, and other baseline characteristics, which may explain the discordant results.
Food Addiction: Useful Concept or Damaging Distraction?
The characteristics of addiction can be divided into three stages: binge and intoxication, withdrawal and negative affect, and pre-occupation and anticipation (craving) [25]. There is loss of control and inability to reduce or stop the behavior despite negative physical, emotional, social, or economic consequences. Addiction, often attributed to poor lifestyle choices or character flaws, is increasingly recognized as a brain disease, and repeated drug use leads to progressive neuroadaptations in the brain [26]. Similar to obesity and many other chronic conditions, susceptibility also varies across individuals depending on various genetic, environmental, and social factors.
Addiction is not limited to substances alone. For example, gambling is considered a non-substance-related addictive disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), given that the behavior elicits symptoms similar to substance addictions such as craving, tolerance, and withdrawal [27]. Eating is intrinsically rewarding, and it is intuitive to consider that the ability of food to activate hedonic pathways may mean that there are addictive properties to food. Proponents of the food addiction model point to the neurobiological resemblances between hedonic responses to food and other substances, and similar phenotypic traits of cravings, withdrawal, and loss of control [28]. The increased activation of the reward circuitry in response to food cues and reduced activation of inhibitory regions in response to food intake seen with addictive-like eating behavior on fMRI studies also display neural patterns similar to substance dependence [29].
However, there has been controversy surrounding the concept of food addiction. Critics of the concept point out that much of the data on food addiction were based on animal models, and the regimented experimental conditions do not readily translate to humans [7]. There is also as yet no identified biochemical property of food that has been shown to be addictive, nor any clearly defined phenotype, genetics, or pathophysiology of food addiction [18]. Although it is clear that certain types of food induce changes in the mesolimbic system and activate the endogenous opioid system, that in itself does not imply that excessive consumption of these foods would lead to dependence. Another key difference between drugs and food is that sensitization of the wanting pathways in the brain occurs with drug use, but not with food [30]. It is this neural sensitization in susceptible individuals that is postulated to be the essence of addiction [31].
Yale Food Addiction Scale
In an effort to provide clarity to the definition of food addiction, Gearhardt and colleagues developed the Yale Food Addiction Scale (YFAS), modeled after the criteria for substance dependence in DSM-IV-TR [32•]. The YFAS tool has sparked interest and research into food addiction. Many cross-sectional studies have shown positive association between YFAS scores and BMI [33]. A systematic review estimated that prevalence of YFAS-diagnosed food addiction was almost fivefold higher in overweight or obese samples compared to the general population (33 vs 6.8%) [33]. Nevertheless, the relationship between food addiction and obesity is not straightforward. The majority of persons with obesity do not meet YFAS criteria for food addiction, whilst some with food addiction have normal BMI [34]. YFAS scores have been used in short-term studies to predict response to weight-loss intervention, with mixed results. One study showed that YFAS-diagnosed food addiction has no effect on weight loss or attrition after a weight-loss program [35], whilst in another study, lower YFAS scores after a 7-month cognitive behavioral therapy program for weight loss predicted weight-loss maintenance at 12 and 24 months [36].
Perhaps the condition that more closely resembles food addiction is binge-eating disorder (BED) (Table 1). There are many similarities between BED and substance addiction including behavioral impulsivity and compulsivity, heightened sensitivity to reward, increased neuroticism, and reduced conscientiousness [17, 38]. A recent systematic review estimated that up to 56.8% of those with BED and 83.6–100% of those with bulimia nervosa have YFAS scores consistent with food addiction [34]. Although the development of YFAS has spurred research on food addiction, critics argue that YFAS remains an extrapolation of the constellation of clinical symptoms seen in substance dependence, and further research to explore the underlying etiology and neurobiological underpinnings of food addiction is needed, rather than relying on a diagnosis-by-proxy [9, 17].
Genetic Studies
It has been argued that altered dopamine signaling in the brain could potentially lead to compensatory reward-seeking behavior which predisposes to substance dependence and overeating. Genetic studies have shown that polymorphisms in D2 dopamine receptors, such as Taq1A, are associated with reduced striatal D2 receptors and reduced reward sensitivity [39]. There are allelic associations between Taq1A A1 carriers and cocaine and opioid dependence as well as binge-eating disorder [34]. A meta-analysis has also shown an association between Taq1A polymorphism and alcohol dependence [40, 41]. However, a recent meta-analysis has shown that Taq1A A1 allele was not associated with difference in BMI [42]. Similarly, a large genome-wide association study (GWAS) involving > 300,000 individuals did not detect any relationship between Taq1A polymorphisms and BMI [3]. Another recent GWAS study in a food addiction cohort, using a modified YFAS in the Nurse’s Health Study population, has shown limited genetic similarities between food and drug addiction [43•]. Together, these genetic, functional neuroimaging and psychometric studies cast doubt on the entity of food addiction and its relevance in the pathogenesis of obesity.
Targeting Hedonic Pathways in Obesity Management
There has been arguments suggesting that treatment of obesity is guided by specific etiology, whether it is “metabolic” or “hedonic” obesity. This would imply tailoring treatments such as behavioral interventions, and possibly pharmacotherapy for “hedonic” obesity; whilst using pharmacotherapy and bariatric surgery for “metabolic” obesity. But is there a clear distinction?
In this section, we explore the effects of behavioral interventions, weight-loss pharmacotherapy, and bariatric surgery on food reward pathways.
Behavioral Interventions
Central to the addiction model are certain behavioral characteristics including increased impulsivity, compulsivity, and susceptibility to internal and external cues. It has been posited that behavioral interventions may be helpful in those with susceptibility to cue-based eating [44]. A randomized controlled trial (RCT) has shown that mindfulness training, when used in conjunction with diet and exercise, resulted in reduced reward-based eating, decreased consumption of sweets, and better short-term weight loss [45, 46]. Another pilot RCT showed that behavioral intervention over 6 months led to increased activation in the striatum for healthier food cues and decreased activation for unhealthy food cues on fMRI compared with controls [47]. Larger, longer-term studies are needed to confirm and quantify the effect of behavioral interventions on the hedonic pathway and weight loss.
Pharmacotherapy
With the exception of orlistat, all currently approved pharmacotherapies for weight loss in the USA work primarily via a variety of mechanisms to decrease appetite and food intake. Most of these agents affect neurotransmitters in the brain. Conversely, most antipsychotic medications lead to increased appetite and weight gain, due to their interactions with serotonergic and dopaminergic neurotransmitter systems [48]. Given our understanding of neurobiological responses to food, drugs that target the dopaminergic pathway could potentially alter hedonic responses to energy-dense foods. In 2014, the USFDA approved the combination of naltrexone/bupropion (Contrave) for long-term management of obesity [49]. Bupropion, a dopamine and norepinephrine reuptake inhibitor, appears to activate pro-opiomelanocortin (POMC) neurons, whereas naltrexone, an opioid antagonist, amplifies this effect by blocking autoinhibition of these neurons [50]. In a study involving fMRI, Contrave attenuated hypothalamic reactivity to food cues, but also enhanced activity in brain regions thought to be involved in hedonic control [51], which suggests that the drug may influence hedonic pathways directly. Indeed, Contrave has been marketed as a solution to reduce cravings for food [52], given that it is a combination of two drugs that are used to treat other addictive disorders (naltrexone for alcohol and opioid dependence, and bupropion for smoking cessation).
Liraglutide is a GLP-1 receptor agonist, originally developed as a diabetes drug, but more recently approved for use in weight management. GLP-1 is an incretin hormone released by L cells in the small intestine, with pleiotropic effects throughout the body. GLP-1 receptors are present in areas of the brain involving both homeostatic and hedonic appetite control [17]. A study showed that infusion of GLP-1 led to reduced activation in brain areas associated with reward-driven eating as seen on fMRI in response to visual stimuli [53]. This finding also corresponded to decreased food intake in a meal provided right after scanning [53]. In another RCT, fMRI showed reduced activation in the brain’s reward system in response to highly desirable food cues after treatment with liraglutide [54]. Hence, the anorectic effect of GLP-1 receptor agonist could be, at least in part, explained by its effect on the brain’s mesolimbic system and reward-seeking behavior.
Phentermine is a sympathomimetic amine that increases norepinephrine in the brain and causes reduced appetite and weight loss. Unlike amphetamine, phentermine does not increase brain dopamine levels, which likely explains its much lower addiction potential [55]. There is currently a lack of evidence on the effect of phentermine or other pharmacotherapies for obesity, including topiramate and lorcaserin, on the hedonic pathway.
Targeting the brain dopamine pathway with ecopipam, a dopamine antagonist originally developed for cocaine addiction, leads to weight loss [56]. Unfortunately, unintended neuropsychiatric adverse events including anxiety, depression, and suicidal ideation were observed [56]. Rimonabant, a cannabinoid-1 receptor blocker, targets the endocannabinoid system in the brain which is thought to link the homeostatic and hedonic systems of energy balance regulation [57]. Rimonabant was withdrawn from the European market following safety concerns of increased risk of suicide [58]. These off-target effects of suicidal ideation and depression have also been seen, albeit rarely, with some other weight-loss pharmacotherapies such as bupropion (increased risk especially in those under 25 years old) and topiramate.
Bariatric Surgery
Bariatric surgery has the ability to alter energy balance set point and circumvent the body’s compensatory physiological responses to weight loss. The impact of surgery on these homeostatic mechanisms is not yet fully understood but is thought to be due to changes in key hormones, especially gut hormones, which are related to energy balance and weight loss [59]. Additionally, significant changes in food choice, taste sensitivity, hedonic evaluation, motivation, and self-control have also been observed after bariatric surgery [60]. Remarkably, self-reported questionnaires reveal changes in food preference, with a shift away from highly palatable, energy-dense foods to healthier, less energy-dense foods after laparoscopic adjustable gastric banding (LAGB) and Roux-en-Y gastric bypass (RYGB) [60,61,62]. A multicenter study of the LAGB has reported improvement in Three-Factor Eating Questionnaire scores which suggest cognitive restraint, and reduced disinhibition and hunger over a 5-year period [63]. Notwithstanding the limitations of YFAS, the prevalence of YFAS-diagnosed food addiction decreased from 57.8% prior to bariatric surgery to 13.7% at 12 months after surgery, although presence of food addiction did not impact on weight loss [64].
Given the above, delineating the potential impact of bariatric surgery on the brain reward pathway via fMRI studies has also garnered significant interest. Patients who had LAGB appeared to have attenuated fasting activity in brain reward areas on fMRI in response to food cues following weight loss. In contrast controls with similar weight loss following behavioural interventions had increase fasting activity in these reward regions indicating a greater interest and attention to the food. The method of weight loss therefore generated different responses to food cues with the reduced food focus in the surgically treated group [65•]. Similar fMRI studies have also shown reduced activation of mesolimbic reward areas after RYGB [62]. However, not all bariatric procedures exert the same effects on brain activation. One study found that visual food cues trigger lower activation of brain reward areas in patients who had RYGB compared to LAGB [66•]. Correspondingly, there was comparatively lower palatability for energy-dense foods and healthier eating behaviors in the RYGB cohort [66•].
Reasons for the changes in brain reward system after different bariatric procedures are yet to be fully elucidated, but changes in gut hormones including GLP-1, peptide YY, and oxyntomodulin may play an important role [62]. As discussed earlier, GLP-1 modulates the mesolimbic system and is increased after RYGB, but unchanged after LAGB. GLP-1 signaling might also alter taste perception [11], appetite, and changes in food preferences. Post-ingestive unpleasant symptoms (dumping) after RYGB may contribute to conditioned aversion or avoidance of certain sugary or fatty foods [62, 67]. Ghrelin, a gut hormone that acts on the hypothalamus to stimulate appetite, also has important extra-hypothalamic neuronal effects on learning, memory, mood, reward, motivation, and neuroprotection [68]. Animal and human studies have shown that ghrelin activates the mesolimbic dopaminergic system to affect motivation and reward [68]. Ghrelin levels increase following LAGB, decrease following sleeve gastrectomy (SG), and can be variable following RYGB [59]. Recent preliminary data have also shown associations between alterations in gut microbiome with reduced hedonic eating after SG [69], though this would need to be explored further. The notion that surgical alteration of the gut can lead to such powerful changes in energy homeostasis and hedonic evaluation of food underscores the importance of the gut-brain axis as a target in developing future treatments for obesity.
However, the loss of hedonic response to food after RYGB appears to have adverse consequences in a small subset of patients, who may turn to alternative avenues including alcohol or other substance abuse. In this “addiction transfer” hypothesis that has been popularized recently, patients with underlying food addiction prior to surgery would simply trade their food addiction with another form of addiction after surgery. The evidence for this thus far is mixed. Several studies have shown increased alcohol and other drug misuse and dependency after bariatric surgery, particularly RYGB [70•, 71, 72]. In a Mayo Clinic cohort, 17% of post-bariatric surgery patients presenting for alcohol dependency treatment remarkably did not consume any alcohol prior to surgery [73]. Altered metabolism of alcohol after RYGB has been proposed as a possible mechanism [74], but sensitization of the brain reward systems to other addictive substances following loss of hedonic response to food is obviously a concern. In a retrospective analysis, there was also an association between higher pre-surgical YFAS scores and substance use disorder after RYGB [75]. On the other hand, the prospective Longitudinal Assessment of Bariatric Surgery-2 cohort study did not show an association between pre-operative binge-eating disorder (which may be closely linked to food addiction) with alcohol use disorder after surgery [70•]. The observations that off-target neuropsychiatric adverse effects involving risks of suicide and depression can occur after RYGB [76] as well as with certain pharmacotherapies raise the question of the importance of hedonic effects of food for mental well-being.
Changing the Obesogenic Environment: Public Health Measures and Policy
The current obesity epidemic cannot be solved by solely focusing on the treatment of individuals afflicted by the disease, when it is the modern obesogenic environment that has triggered the crisis. Hence, broader public health measures and policies that aim to modify behavior and the environment are paramount to combat obesity and prevent weight gain.
Tobacco and alcohol are two widely available substances that have potential to cause dependence and impaired health. Taxes on alcohol and tobacco have been seen as an attractive lever to both achieve public health goals and raise revenues for public spending in many countries. Advocates of the food addiction model argue that the addictive nature of energy-dense foods warrants regulations similar to that of tobacco and alcohol, and that restrictions on sale and advertising of these foods would be effective to reduce obesity rates. An online survey of the general public in the USA and Australia have shown interesting results; although the majority agreed that some types of foods are addictive, there was very little support for increasing taxes on these obesogenic foods [77]. In another recent US survey, belief in the food addiction model appeared to be significantly associated with greater support for obesity-related initiatives and policies [78].
Regulations and taxes on some of these foods (e.g., sugar-sweetened beverages, saturated fat) have been imposed in several countries such as Mexico, Finland, France, and Hungary. The evidence base for these “health taxes” in changing consumer behavior and producing positive health outcomes is still growing, and current studies suggest the effect to be price-sensitive, with price increases of ≥ 20% being more effective [79]. The appreciation of nicotine as an addictive substance was crucial in garnering public and political support for tobacco control and taxes [34], and similar work to delineate the food addiction model (particularly in children and adolescents) would be important to build the scientific basis and public support for these innovative taxes.
Impact on Weight-Related Stigma and Health Beliefs
Individuals with obesity are often negatively stereotyped as being lazy, unmotivated, and lacking in self-control and discipline [80]. In Western societies, weight-based discrimination and stigma is highly prevalent in various settings (including employment, healthcare, and education) with consequent adverse physical, emotional, social, and economic outcomes [80]. Much work is still needed to change the public narrative around obesity, in that it is a disease that is influenced by genetic, environmental, and many other factors beyond a person’s control, and not simply a matter of personal choice.
Given the above, how does the food addiction model influence stigma associated with obesity? Surveys have shown conflicting results on whether holding the view that obesity is a food addiction influences stigmatization, with some studies suggesting it reduces bias [81], whilst others do not [82]. A recent review suggests that people who believe that they have food addiction may lead to restrained eating in the short term, but that these restrictions could lead to cravings and subsequently more aberrant eating behaviors in the long term [83]. These findings merit further research on the impact of the food addiction message on weight bias and stigma, as well as on health-related behaviors in individuals with obesity.
Conclusions
Over recent years, there has been rapid progress in our understanding of food hedonic systems and changes in neural pathways in response to different types of foods. Insights from bariatric surgery highlight the importance of the gut-brain axis in energy homeostasis, and further research into mechanisms in which alterations in gut hormones affect the brain’s food reward systems would advance our understanding of the pathogenesis and treatment of obesity. However, the central nervous system is complex, and we have yet to fully elucidate how the pleasure of food affects our brain and behavior. Moving forward, we need to be wary of potential off-target neuropsychiatric adverse effects in the pursuit of novel therapeutic strategies for obesity. There remains much controversy surrounding the food addiction model. Further research into this area is warranted as validation of the model would have important implications for public health policy and may affect eating behaviors in individuals with obesity, as well as influence attitudes of society towards obesity.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bray GA, Kim KK, Wilding JPH, World Obesity F. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18(7):715–23.
O'Rahilly S, Farooqi IS. Human obesity as a heritable disorder of the central control of energy balance. Int J Obes. 2008;32(Suppl 7):S55–61.
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197–206.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376(3):254–66.
McAllister EJ, Dhurandhar NV, Keith SW, Aronne LJ, Barger J, Baskin M, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr. 2009;49(10):868–913.
Randolph TG. The descriptive features of food addiction; addictive eating and drinking. Q J Stud Alcohol. 1956;17(2):198–224.
Ziauddeen H, Fletcher PC. Is food addiction a valid and useful concept? Obes Rev. 2013;14(1):19–28.
Schwartz MW, Woods SC, Porte D Jr, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404(6778):661–71.
Sumithran P, Prendergast LA, Delbridge E, Purcell K, Shulkes A, Kriketos A, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365(17):1597–604.
Speakman JR, Levitsky DA, Allison DB, Bray MS, de Castro JM, Clegg DJ, et al. Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity. Dis Model Mech. 2011;4(6):733–45.
Berthoud HR. Metabolic and hedonic drives in the neural control of appetite: who is the boss? Curr Opin Neurobiol. 2011;21(6):888–96.
Bergstrom HC, Pinard CR. Corticolimbic circuits in learning, memory, and disease. J Neurosci Res. 2017;95(3):795–6.
Palmiter RD. Is dopamine a physiologically relevant mediator of feeding behavior? Trends Neurosci. 2007;30(8):375–81.
Seeley RJ, Berridge KC. The hunger games. Cell. 2015;160(5):805–6.
Yu YH, Vasselli JR, Zhang Y, Mechanick JI, Korner J, Peterli R. Metabolic vs. hedonic obesity: a conceptual distinction and its clinical implications. Obes Rev. 2015;16(3):234–47.
Gearhardt AN, Davis C, Kuschner R, Brownell KD. The addiction potential of hyperpalatable foods. Curr Drug Abuse Rev. 2011;4(3):140–5.
Cameron JD, Chaput JP, Sjodin AM, Goldfield GS. Brain on fire: incentive salience, hedonic hot spots, dopamine, obesity, and other hunger games. Annu Rev Nutr. 2017.
Finlayson G. Food addiction and obesity: unnecessary medicalization of hedonic overeating. Nat Rev Endocrinol. 2017.
Lawrence NS, Hinton EC, Parkinson JA, Lawrence AD. Nucleus accumbens response to food cues predicts subsequent snack consumption in women and increased body mass index in those with reduced self-control. NeuroImage. 2012;63(1):415–22.
Paolini BM, Laurienti PJ, Simpson SL, Burdette JH, Lyday RG, Rejeski WJ. Global integration of the hot-state brain network of appetite predicts short term weight loss in older adult. Front Aging Neurosci. 2015;7:70.
Murdaugh DL, Cox JE, Cook EW 3rd, Weller RE. fMRI reactivity to high-calorie food pictures predicts short- and long-term outcome in a weight-loss program. NeuroImage. 2012;59(3):2709–21.
Demos KE, Heatherton TF, Kelley WM. Individual differences in nucleus accumbens activity to food and sexual images predict weight gain and sexual behavior. J Neurosci. 2012;32(16):5549–52.
McCaffery JM, Haley AP, Sweet LH, Phelan S, Raynor HA, Del Parigi A, et al. Differential functional magnetic resonance imaging response to food pictures in successful weight-loss maintainers relative to normal-weight and obese controls. Am J Clin Nutr. 2009;90(4):928–34.
Ziauddeen H, Farooqi IS, Fletcher PC. Obesity and the brain: how convincing is the addiction model? Nat Rev Neurosci. 2012;13(4):279–86.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35(1):217–38.
Volkow ND, Koob GF, McLellan AT. Neurobiologic advances from the brain disease model of addiction. N Engl J Med. 2016;374(4):363–71.
Meule A, Gearhardt AN. Food addiction in the light of DSM-5. Nutrients. 2014;6(9):3653–71.
Lerma-Cabrera JM, Carvajal F, Lopez-Legarrea P. Food addiction as a new piece of the obesity framework. Nutr J. 2016;15:5.
Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68(8):808–16.
Westwater ML, Fletcher PC, Ziauddeen H. Sugar addiction: the state of the science. Eur J Nutr. 2016;55(Suppl 2):55–69.
Berridge KC, Robinson TE. Liking, wanting, and the incentive-sensitization theory of addiction. Am Psychol. 2016;71(8):670–9.
• Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009;52(2):430–6. This study proposes a novel questionnaire to diagnose food addiction based on substance addiction criteria and has spurred research into the area of food addiction.
Long CG, Blundell JE, Finlayson G. A systematic review of the application and correlates of YFAS-diagnosed ‘food addiction’ in humans: are eating-related ‘addictions’ a cause for concern or empty concepts? Obes Facts. 2015;8(6):386–401.
Carter A, Hendrikse J, Lee N, Yucel M, Verdejo-Garcia A, Andrews Z, et al. The neurobiology of “food addiction” and its implications for obesity treatment and policy. Annu Rev Nutr. 2016;36:105–28.
Lent MR, Eichen DM, Goldbacher E, Wadden TA, Foster GD. Relationship of food addiction to weight loss and attrition during obesity treatment. Obesity (Silver Spring). 2014;22(1):52–5.
Sawamoto R, Nozaki T, Nishihara T, Furukawa T, Hata T, Komaki G, et al. Predictors of successful long-term weight loss maintenance: a two-year follow-up. Biopsychosoc Med. 2017;11:14.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Davis C. A narrative review of binge eating and addictive behaviors: shared associations with seasonality and personality factors. Front Psychiatry. 2013;4:183.
Blum K, Braverman ER, Holder JM, Lubar JF, Monastra VJ, Miller D, et al. Reward deficiency syndrome: a biogenetic model for the diagnosis and treatment of impulsive, addictive, and compulsive behaviors. J Psychoactive Drugs. 2000;32(Suppl:i-iv):1–112.
Wang F, Simen A, Arias A, Lu QW, Zhang H. A large-scale meta-analysis of the association between the ANKK1/DRD2 Taq1A polymorphism and alcohol dependence. Hum Genet. 2013;132(3):347–58.
Smith L, Watson M, Gates S, Ball D, Foxcroft D. Meta-analysis of the association of the Taq1A polymorphism with the risk of alcohol dependency: a HuGE gene-disease association review. Am J Epidemiol. 2008;167(2):125–38.
Benton D, Young HA. A meta-analysis of the relationship between brain dopamine receptors and obesity: a matter of changes in behavior rather than food addiction? Int J Obes. 2016;40(Suppl 1):S12–21.
• Cornelis MC, Flint A, Field AE, Kraft P, Han J, Rimm EB, et al. A genome-wide investigation of food addiction. Obesity (Silver Spring). 2016;24(6):1336–41. This study involved genome-wide investigation of YFAS-diagnosed food addiction cohort and found limited similarities between food addiction and drug addiction.
Forman EM, Butryn ML. A new look at the science of weight control: how acceptance and commitment strategies can address the challenge of self-regulation. Appetite. 2015;84:171–80.
Mason AE, Epel ES, Aschbacher K, Lustig RH, Acree M, Kristeller J, et al. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: data from the SHINE randomized controlled trial. Appetite. 2016;100:86–93.
Mason AE, Epel ES, Kristeller J, Moran PJ, Dallman M, Lustig RH, et al. Effects of a mindfulness-based intervention on mindful eating, sweets consumption, and fasting glucose levels in obese adults: data from the SHINE randomized controlled trial. J Behav Med. 2016;39(2):201–13.
Deckersbach T, Das SK, Urban LE, Salinardi T, Batra P, Rodman AM, et al. Pilot randomized trial demonstrating reversal of obesity-related abnormalities in reward system responsivity to food cues with a behavioral intervention. Nutr Diabetes. 2014;4:e129.
Bak M, Fransen A, Janssen J, van Os J, Drukker M. Almost all antipsychotics result in weight gain: a meta-analysis. PLoS One. 2014;9(4):e94112.
Apovian CM, Aronne LJ, Bessesen DH, McDonnell ME, Murad MH, Pagotto U, et al. Pharmacological management of obesity: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(2):342–62.
Vetter ML, Faulconbridge LF, Webb VL, Wadden TA. Behavioral and pharmacologic therapies for obesity. Nat Rev Endocrinol. 2010;6(10):578–88.
Wang GJ, Tomasi D, Volkow ND, Wang R, Telang F, Caparelli EC, et al. Effect of combined naltrexone and bupropion therapy on the brain’s reactivity to food cues. Int J Obes. 2014;38(5):682–8.
Contrave Product Information Website. [Available from: https://contrave.com/.]
De Silva A, Salem V, Long CJ, Makwana A, Newbould RD, Rabiner EA, et al. The gut hormones PYY 3-36 and GLP-1 7-36 amide reduce food intake and modulate brain activity in appetite centers in humans. Cell Metab. 2011;14(5):700–6.
Farr OM, Sofopoulos M, Tsoukas MA, Dincer F, Thakkar B, Sahin-Efe A, et al. GLP-1 receptors exist in the parietal cortex, hypothalamus and medulla of human brains and the GLP-1 analogue liraglutide alters brain activity related to highly desirable food cues in individuals with diabetes: a crossover, randomised, placebo-controlled trial. Diabetologia. 2016;59(5):954–65.
Bray GA. Medical treatment of obesity: the past, the present and the future. Best Pract Res Clin Gastroenterol. 2014;28(4):665–84.
Astrup A, Greenway FL, Ling W, Pedicone L, Lachowicz J, Strader CD, et al. Randomized controlled trials of the D1/D5 antagonist ecopipam for weight loss in obese subjects. Obesity (Silver Spring). 2007;15(7):1717–31.
Di Marzo V, Ligresti A, Cristino L. The endocannabinoid system as a link between homoeostatic and hedonic pathways involved in energy balance regulation. Int J Obes. 2009;33(Suppl 2):S18–24.
Topol EJ, Bousser MG, Fox KA, Creager MA, Despres JP, Easton JD, et al. Rimonabant for prevention of cardiovascular events (CRESCENDO): a randomised, multicentre, placebo-controlled trial. Lancet. 2010;376(9740):517–23.
Dixon JB, Lambert EA, Lambert GW. Neuroendocrine adaptations to bariatric surgery. Mol Cell Endocrinol. 2015;418(Pt 2):143–52.
Munzberg H, Laque A, Yu S, Rezai-Zadeh K, Berthoud HR. Appetite and body weight regulation after bariatric surgery. Obes Rev. 2015;16(Suppl 1):77–90.
Ullrich J, Ernst B, Wilms B, Thurnheer M, Hallschmid M, Schultes B. The hedonic drive to consume palatable foods appears to be lower in gastric band carriers than in severely obese patients who have not undergone a bariatric surgery. Obes Surg. 2013;23(4):474–9.
Behary P, Miras AD. Food preferences and underlying mechanisms after bariatric surgery. Proc Nutr Soc. 2015;74(4):419–25.
Dixon JB, Eaton LL, Vincent V, Michaelson R. LAP-BAND for BMI 30-40: 5-year health outcomes from the multicenter pivotal study. Int J Obes. 2016;40(2):291–8.
Sevincer GM, Konuk N, Bozkurt S, Coskun H. Food addiction and the outcome of bariatric surgery at 1-year: prospective observational study. Psychiatry Res. 2016;244:159–64.
• Bruce AS, Bruce JM, Ness AR, Lepping RJ, Malley S, Hancock L, et al. A comparison of functional brain changes associated with surgical versus behavioral weight loss. Obesity (Silver Spring). 2014;22(2):337–43.
• Scholtz S, Miras AD, Chhina N, Prechtl CG, Sleeth ML, Daud NM, et al. Obese patients after gastric bypass surgery have lower brain-hedonic responses to food than after gastric banding. Gut. 2014;63(6):891–902. This study compares the brain hedonic responses to different bariatric procedures using fMRI.
Scholtz S, Goldstone AP, le Roux CW. Changes in reward after gastric bypass: the advantages and disadvantages. Curr Atheroscler Rep. 2015;17(10):61.
Andrews ZB. The extra-hypothalamic actions of ghrelin on neuronal function. Trends Neurosci. 2011;34(1):31–40.
Sanmiguel CP, Jacobs J, Gupta A, Ju T, Stains J, Coveleskie K, et al. Surgically induced changes in gut microbiome and hedonic eating as related to weight loss: preliminary findings in obese women undergoing bariatric surgery. Psychosom Med. 2017.
• King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307(23):2516–2525. This study examined the prevalence and factors associated with alcohol use disorders in the prospective Longitudinal Assessment of Bariatric Surgery-2 cohort.
Conason A, Teixeira J, Hsu CH, Puma L, Knafo D, Geliebter A. Substance use following bariatric weight loss surgery. JAMA Surg. 2013;148(2):145–50.
Ostlund MP, Backman O, Marsk R, Stockeld D, Lagergren J, Rasmussen F, et al. Increased admission for alcohol dependence after gastric bypass surgery compared with restrictive bariatric surgery. JAMA Surg. 2013;148(4):374–7.
Cuellar-Barboza AB, Frye MA, Grothe K, Prieto ML, Schneekloth TD, Loukianova LL, et al. Change in consumption patterns for treatment-seeking patients with alcohol use disorder post-bariatric surgery. J Psychosom Res. 2015;78(3):199–204.
Woodard GA, Downey J, Hernandez-Boussard T, Morton JM. Impaired alcohol metabolism after gastric bypass surgery: a case-crossover trial. J Am Coll Surg. 2011;212(2):209–14.
Reslan S, Saules KK, Greenwald MK, Schuh LM. Substance misuse following Roux-en-Y gastric bypass surgery. Subst Use Misuse. 2014;49(4):405–17.
Dixon JB. Self-harm and suicide after bariatric surgery: time for action. Lancet Diabetes Endocrinol. 2016;4(3):199–200.
Lee NM, Lucke J, Hall WD, Meurk C, Boyle FM, Carter A. Public views on food addiction and obesity: implications for policy and treatment. PLoS One. 2013;8(9):e74836.
Schulte EM, Tuttle HM, Gearhardt AN. Belief in food addiction and obesity-related policy support. PLoS One. 2016;11(1):e0147557.
Wright A, Smith KE, Hellowell M. Policy lessons from health taxes: a systematic review of empirical studies. BMC Public Health. 2017;17(1):583.
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941–64.
Latner JD, Puhl RM, Murakami JM, O'Brien KS. Food addiction as a causal model of obesity. Effects on stigma, blame, and perceived psychopathology. Appetite. 2014;77:77–82.
Lee NM, Hall WD, Lucke J, Forlini C, Carter A. Food addiction and its impact on weight-based stigma and the treatment of obese individuals in the U.S. and Australia. Nutrients. 2014;6(11):5312–26.
Ruddock HK, Hardman CA. Food addiction beliefs amongst the lay public: what are the consequences for eating behaviour? Curr Addict Rep. 2017;4(2):110–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Phong Ching Lee declares that he has no conflict of interest.
John B. Dixon has a Senior Research Fellowship with the National Health and Medical Research Council (Australia); has received compensation from Apollo Endosurgery, Bariatric Advantage, and Covidien for service as a consultant; has received compensation from iNova Pharmaceuticals for service as a consultant and guest speaker; has received compensation from Nestlé for serving as a guest speaker as well as on a scientific advisory board(s); has received compensation from Novartis for serving as a guest speaker as well as on a scientific advisory board(s); has received compensation from Novo Nordisk for service on scientific advisory boards; and has received compensation from mdBriefCase for providing assistance in the development of educational materials.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Rights and permissions
About this article
Cite this article
Lee, P.C., Dixon, J.B. Food for Thought: Reward Mechanisms and Hedonic Overeating in Obesity. Curr Obes Rep 6, 353–361 (2017). https://doi.org/10.1007/s13679-017-0280-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-017-0280-9