Abstract
Purpose of Review
Despite the emergence of various new wound care products, millions of people continue to suffer from complications associated with acute and chronic wounds. Nanomaterials offer a variety of strategies to accelerate wound closure and promote appropriate progression through the stages of healing, which will be detailed in this review.
Recent Findings
The small size of nanomaterials enhances penetration and permeation of tissues and lends a large surface area-to-volume ratio, ideal for topical drug delivery. Furthermore, nanofibers may be utilized to create nanoscaffold wound dressings that simulate the topographic appearance of endogenous extracellular matrix, thereby stimulating wound reepithelialization and collagen production.
Summary
Together, nanomaterials offer many approaches to reduce the morbidity associated with acute and chronic wounds, as demonstrated by a substantial body of pre-clinical data. Future investigations should aim to address the paucity of human clinical trial data, essential for translating wound-healing benefits from bench to bedside.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Wound care is an enormous industry with the global wound care market estimated to exceed $22 billion USD annually by 2020 [1]. Recent advancements have yielded a variety of new types of dressings—films, foams, alginates, hydrocolloids, and hydrogels—in addition to inventive topical therapies with active ingredients including beta blockers, growth factors, silver, and honey [2–4]. Although there has been a recent explosion of new products on the market, wound-healing success rates have improved at a far slower pace. Millions of people continue to suffer from complications and consequences associated with acute and chronic wounds, which pose a significant burden to the healthcare system and cause patient and caregiver stress, economic loss, and decreased quality of life.
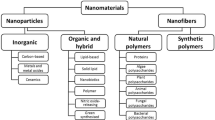
Nanomaterials, defined as materials that measure on the nanoscale (1–100 nm) or that contain nanoscale structures internally or on their surfaces, represent one of the most promising strategies for improving the treatment of acute and chronic wounds [5]. Nanomaterials enable the exploitation of unique characteristics of matter at the nanoscale, which typically exhibits chemical, electronic, and optical properties different from those of the bulk material [6]. The small size of nanomaterials enhances their penetration and permeation of tissues, and their surface characteristics can be manipulated to facilitate selective accumulation within specific target tissues or cell types [7–9]. Their size also lends an extremely large surface area-to-volume ratio, thereby increasing the interaction of therapeutic agents with their biological targets, improving treatment efficacy and decreasing the required dose.
While nanomaterials share many advantageous properties, their compositions are widely varied. Some have structures comprised of one or more substances that provide both physical architecture and therapeutic activity (e.g., copper nanoparticles, silver-chitosan nanoparticles). By contrast, other nanomaterials are engineered to deliver therapeutic agents (e.g., growth factors, oligonucleotides) that otherwise may not be bioavailable in vivo secondary to poor solubility, short half-life, or leakage from the site of the wound. Such nanomaterials can encapsulate or incorporate therapeutic substances into their structures to be released in vivo in a sustained manner, and a release rate may be controlled by altering nanomaterial composition and physical characteristics. Sustained release allows continuous interface between a therapeutic agent and its biological target without the rapid saturation and washout of a bolus dose, thereby allowing the delivery of potent drugs while minimizing side effects, as the maximum amount of drug is never in contact with the skin at one time [6, 10].
In addition to these categories of nanomaterials, nanoscale fibers may be utilized to fabricate nanoscaffold wound dressings, which have increased porosity, and their physical composition can be modulated to provide optimal absorbency and gas permeability for maintaining moist, oxygenated wounds [11]. The structure of nanoscaffold wound dressings can simulate the topographic appearance of endogenous extracellular matrix (ECM), facilitating attachment and spreading of fibroblasts and keratinocytes, thereby enhancing collagen synthesis and reepithelialization [12, 13]. Furthermore, nanoscaffold wound dressings have an exceedingly large surface area-to-volume ratio, thus maximizing their interaction with the wound bed and enabling improved drug delivery when drugs are incorporated into the dressing.
Physical nanomaterials, drug-releasing nanomaterials, and nanoscaffold wound dressings represent promising therapeutic platforms for improving wound care. Given the social, emotional, and economic burdens presently posed by protracted healing and delayed closure, wound care products that accelerate the healing process and improve closure success rates are sorely needed. Here, we present a brief overview of the wound-healing process followed by a review of innovative nanomaterials that may fill this unmet therapeutic need.
Wound Healing
Wound healing is a dynamic process defined by three simultaneous, overlapping phases. Following fibrin clot formation, wound healing begins with an inflammatory phase marked by the recruitment of neutrophils and macrophages. These cells release pro-inflammatory cytokines and clear pathogens and debris via phagocytosis and release of reactive oxygen species and matrix metalloproteinases [14, 15]. Next, collagen deposition and angiogenesis occur during the proliferative phase to form granulation tissue, characterized by high vascularity and immature type III collagen. During this phase, reepithelialization and contraction of myofibroblasts occur [16, 17]. Finally, the remodeling phase includes the replacement of type III collagen by type I collagen, leading to the formation of a less vascularized scar with improved mechanical strength [18].
Under ideal healing conditions, acute wounds progress linearly through these phases. By contrast, chronic wounds are characterized by arrest, typically in the inflammatory phase, with wound physiology that represents a pathologic cycle. Unlike normal wounds that are typically rich in essential growth factors and pro-healing cytokines, chronic wounds feature an excess of pro-inflammatory cytokines and factors [19]. Chronic wounds may exhibit decreased angiogenesis, increased hyperkeratotic tissue, accumulation of devitalized tissue, malodorous exudates, and biofilm formation. These wounds tend to arise in patients with inadequate tissue perfusion, suppressed immune systems, and/or chronic inflammatory states as seen in diabetes mellitus, sickle cell disease, cancer, peripheral arterial and venous stasis diseases, obesity, smoking, and malnutrition. In such patients, therapies that accelerate wound physiology through the phases of healing are essential to ensure that the inflammatory phase is sufficiently limited and avoid development of a chronic wound [14].
Physical Nanomaterials
Silver
Metal nanomaterials have demonstrated significant wound-healing benefits alone, as conjugates, in wound dressings and in conjunction with activating light sources. They are well known for aiding the clearance of microbes, which may otherwise prolong the inflammatory phase of healing. Of all metal nanomaterials, silver nanoparticles (Ag-np) are perhaps the most frequently utilized; they have been incorporated into burn ointments, wound dressings, and medical devices to effectively prevent infection [20]. Ag-np are known for their potent, broad spectrum antimicrobial activity, effectively killing gram-positive and gram-negative bacteria as well as fungi [21], viruses [22], and protozoa [23]. Ag-np can counteract bacterial virulence factors by inhibiting biofilm formation [24, 25], neutralizing bacterial toxins [25] and interfering with quorum sensing [26]. Furthermore, they demonstrate synergy with conventional antimicrobial drugs, enabling killing of microbes that would otherwise be unaffected or resistant [27].
Ag-np are oxidized in vivo leading to silver ion release under acidic conditions. It is the silver ions, not Ag-np themselves, that are credited for providing antimicrobial activity by compromising microbial membranes, damaging DNA, inhibiting ATP production, and generating reactive oxygen species (ROS) [28]. The antimicrobial activity of Ag-np is particularly intriguing as it inhibits microbes via multiple, non-specific mechanisms. Unlike conventional antibiotics with a single biological target, multi-mechanistic nanomaterials such as Ag-np may circumvent antimicrobial resistance as multiple, simultaneous mutations would need to occur in the same organism for resistance to occur. Ag-np have also been shown to evade non-specific resistance mechanisms such as drug efflux [29] and biofilm formation [24].
Ag-np’s antimicrobial properties support the critical elimination of microbes that may otherwise prevent efficient progression through the phases of healing. Further, Ag-np may modulate local and systemic inflammatory processes to support the healing process independently of their antimicrobial activity. A study of Ag-np impact on human keratinocytes and dermal fibroblasts indicated that they attenuate the production of pro-inflammatory cytokines and factors [30], while another study of Ag-np dressings applied to burn wounds in mice demonstrated a reduction in wound neutrophils and IL-6 associated with increased IL-10, TGF-β, VEGF, and IFN-γ in Ag-np treated wounds. Additionally, pro-inflammatory acute-phase proteins in the serum of Ag-np treated mice showed an accelerated return to baseline [31]. These findings may support a larger role for Ag-np in wound healing, in addition to microbial clearance.
A common technique for utilizing Ag-np involves their incorporation into dressings. For example, dressings made of biocompatible bacterial cellulose have been impregnated with Ag-np, demonstrating activity against Escherichia coli, Staphylococcus aureus, and Pseudomonas aeruginosa and facilitating attachment and growth of keratinocytes while maintaining an ideal moist, absorbent barrier [13]. In another study, Ag-np were incorporated into a mussel-inspired nanofiber poly(dopamine methacrylamide-co-methyl methacrylate) (MADO) wound dressing, which effectively inhibited E. coli, S. aureus, and P. aeruginosa (Fig. 1) [32]. This dressing displayed 13 % initial silver ion release on the first day of application, corresponding to a dose that is toxic to bacteria but not mammalian cells. This burst was followed by a slower, sustained release for at least 7 days under physiological conditions. When applied to partial-thickness wounds in rats, those treated with MADO-Ag-np dressings demonstrated 92 % healing over 15 days compared to 65 and 51 % in wounds receiving plain MADO and simple gauze dressings, respectively [32]. Although the ECM-like properties of the nanofiber MADO dressing exhibited a positive effect compared to simple gauze dressing, Ag-np had an even more significant impact on the acceleration of wound healing.
Ag-np were incorporated into poly(dopamine methacrylamide-co-methyl methacrylate) (MADO) nanofiber wound dressing. Field emission scanning electron microscopy was used to image electrospun MADO nanofibers alone (a), as well as following Ag-np incorporation (b). On high-resolution transmission electron microscopy, the incorporated Ag-np were compared following 24-h (c) versus 12-h (d) incubation of MADO nanofibers with silver nitrate. The average Ag-np diameter was shown to increase as a function of incubation time. Reprinted with permission from [32]
Thus far, multiple studies have concluded that Ag-np’s biological effects are due to silver ion release and that Ag-np themselves provide negligible direct activity [28, 33–35]. To challenge this concept, Zhou et al. synthesized silver-silver chloride nanoparticles complexed with reduced graphene oxide (Ag/AgCl/rGO nanomaterial), which demonstrated negligible release of silver ions under physiological conditions [36•]. Although Ag/AgCl/rGO nanomaterial did not release silver ions, it generated a large amount of oxidative radicals, exhibiting potent bactericidal activity against gram-positive and gram-negative bacteria. When functionalized with poly(diallyldimethylammonium chloride) (PDDA), Ag/AgCl/rGO nanomaterial demonstrated high adsorptive capacity and enhanced bactericidal activity. Furthermore, Ag/AgCl/rGO nanomaterial augmented wound healing when applied to partial-thickness burn wounds in mice. Earlier reepithelialization, increased deposition of organized collagen, and faster rates of wound closure were observed [36•].
Gold
Gold nanomaterials comprise another group of physical nanomaterials that can be utilized to improve wound healing. Unlike silver, gold nanomaterials alone do not offer antimicrobial activity [29]. Rather, they can be conjugated with existing antimicrobial drugs, thereby increasing their potency and broadening their spectrum of activity to effectively kill organisms that would otherwise be resistant or unaffected. For instance, vancomycin-conjugated gold nanoparticles (Au-Vanc-np) increased vancomycin’s activity against vancomycin-resistant enterococci (VRE) 50-fold, and Au-Vanc-np exhibited significant activity against E. coli, a gram-negative bacterium that is usually unaffected by vancomycin [37]. In addition to antimicrobial drugs, gold nanomaterials may be conjugated with pathogen-specific antibodies for photothermal therapy [38, 39] or photosensitizing molecules for photodynamic therapy (PDT) [40] to achieve microbial clearance from wounds. For example, gold nanoparticle-conjugated photosensitizers used for PDT have demonstrated superior fungal depletion from Candida albicans-infected wounds in mice [41].
In addition to improving wound healing by enhancing antimicrobial therapies, gold nanomaterials exhibit healing properties when administered to wounds as a topical monotherapy. In a study of full-thickness excision wounds in rats, gold nanoparticles (Au-np) enhanced the healing process, as characterized by increased reepithelialization, alignment of granulation tissue, and deposition of collagen fibers compared to untreated controls [42]. These differences were especially pronounced in earlier wound stages, thereby reducing the overall duration of healing. When compared to topical Ag-np monotherapy, Au-np demonstrated greater radical scavenging activity in vitro, in addition to greater wound-healing improvements in rats [42].
Wound-healing properties of Au-np may be further enhanced in combination with polymers or stem cells [42–44]. Polymer nanocomposites such as chitosan-Au-np increase the antioxidant activity of Au-np severalfold and offer improved biocompatibility. Further, polycationic chitosan may be doubly utilized as a mediator of Au-np synthesis. In surgical wounds in rats, chitosan-Au-np significantly enhanced hemostasis and reepithelialization with improved overall healing compared to chitosan alone or standard Tegaderm dressings. Furthermore, chitosan-Au-np were shown to increase proliferation of human fibroblasts in vitro [43]. Another study combined Au-np with cryopreserved human fibroblasts (CrHFC-Au-np), which were then applied to third-degree burn wounds in rats. CrHFC-Au-np-treated wounds demonstrated faster tissue recovery, less infiltration of inflammatory cells, and greater deposition of type I and III collagen compared to untreated controls or CrHFC alone [44].
Finally, gold nanoshells represent a newer class of gold nanomaterials characterized by thin metal shells that surround a dielectric core. One study utilized gold nanoshells with a silica core, designed to absorb near infrared (NIR) light for NIR laser tissue welding [45]. While laser tissue welding offers advantages over suture wound closure such as speed, reduced tissue trauma, immediate watertight anastomoses, and accelerated healing, the decreased wound strength produced by tissue welding has thus far limited its use. Gold nanoshells have demonstrated strong absorptive properties and large absorption cross-sections without photobleaching, which may enable laser tissue welding that is more focused, as well as more powerful. In the aforementioned study, gold nanoshells were used for NIR tissue welding in vivo following creation of full-thickness incisions in rat skin [45]. Wound samples revealed tensile strengths equaling that of uncut tissue, and histological investigations showed a robust wound-healing response, demonstrating yet another method by which gold nanomaterials may be utilized to improve wound healing and accelerate closure.
Nanomaterials for Therapeutic Delivery
Protein Delivery
A large class of nanomaterials with significant possibilities for wound healing are those that have been engineered to deliver therapeutic agents. Although many agents stand to benefit from nanomaterial delivery, those with short half-lives or poor in vivo solubility have the most to gain, as these limitations may otherwise prohibit their use. For example, human antimicrobial peptide LL37 is known to improve wound healing, although it must be administered at very high doses with frequent dosing schedules given rapid in vivo degradation [46]. LL37 offers several benefits due to its broad spectrum antimicrobial activity, enhancement of angiogenesis, epithelial cell migration and proliferation, and modulation of immune response; however, in vivo administration without the use of nanomaterials has proven to be impractical [46, 47•]. Progress was made when one group encapsulated LL37 in poly(lactic-co-glycolic acid) (PLGA) nanoparticles, producing significant wound-healing improvements at lower doses of LL37; however, these nanoparticles required intradermal injection for optimal effect [48]. More recently, LL37 was encapsulated in nanostructured lipid carriers (NLCs), a type of lipid nanoparticle with enhanced loading capacity capable of creating an ultrafine film for controlled occlusion, which is advantageous for topical therapeutic delivery [47•]. LL37 retained its properties following NLC encapsulation without toxicity against human fibroblasts and significantly improved wound-healing outcomes when applied topically to full-thickness diabetic mouse wounds compared to untreated controls or free LL37. Specifically, NLC-LL37 accelerated closure and resolution of inflammatory processes and improved reepithelialization following only three topical administrations over a 96-h period at a low dose [47•].
In addition to antimicrobial peptides, nanomaterials may be used to enable the delivery of growth factors, another category of endogenous molecules with otherwise limited delivery options due to in vivo degradation. Especially in chronic wounds where there is excessive inflammation and proteolytic activity, pro-healing proteins and growth factors are degraded even more rapidly, potentiating the cycle of aberrant healing. A major mediator of wound healing, stromal cell-derived factor 1 (SDF1), acts via recruitment of endothelial progenitor cells to contribute to revascularization and support the reepithelialization process [49, 50]. As with LL37, frequent topical application of SDF1 at high doses has demonstrated therapeutic healing effects; however, this is expensive and impractical [51]. Yeboah et al. combined SDF1 with elastin-like peptide to generate a nanoparticulate fusion protein (SDF1-ELP), which exhibited greater in vivo activity compared to free SDF1. When administered topically to full-thickness diabetic mouse wounds, SDF1-ELP led to 95 % closure by day 21 and full wound closure by day 28. By contrast, only 80 % closure by day 21 was seen with free SDF1, ELP alone, or vehicle controls, which required 42 days to achieve complete healing [50]. These results in refractory diabetic wounds warrant further exploration of SDF1-ELP for other chronic wound states.
Oligonucleotide Delivery
Therapeutic oligonucleotides have potential benefits for wound healing. They can affect a myriad of therapeutic targets via small interfering RNA (siRNA)-mediated gene knockdown, and antisense inhibitors can be used to target pathologic oligonucleotides. However, as with growth factors and antimicrobial peptides, oligonucleotides suffer from increased degradation in vivo, particularly in the setting of chronic wounds. To overcome this limitation, one group delivered an oligonucleotide antisense inhibitor using lipid nanoparticles to specifically target a pathologic microRNA (miRNA) that inhibits endogenous messenger RNA (mRNA) in the setting of ischemic wounds. Peripheral vasculopathies cause wound ischemia, which can lead to increased local levels of hypoxia-induced miRNAs (hypoxamiR). The specific hypoxamiR targeted in this study, miR-210, has drawn interest as a target of therapeutic inhibition due to its suppression of mitochondrial metabolism and inhibition of cellular proliferation necessary for proper healing. Lipid nanoparticles loaded with antisense miR-210 inhibitor were injected intradermally in bipedicle flap wounds created in mice prone to diabetes and atherosclerosis. After only one treatment, the nanoparticles led to significantly reduced miR-210 levels in ischemic wound edge tissue, which demonstrated rescued keratinocyte proliferation and increased ATP production, as well as improved wound closure [52•].
By investigating the physiology of chronic wound processes, scientists have been able to develop improved therapies capable of targeting specific wound pathology, as demonstrated by a nanoparticulate antisense miR-210 inhibitor. In another example, the study of notoriously difficult diabetic foot ulcers has led to the observation of increased macrophage infiltrates, which cause TNF-α overproduction, thereby instigating fibroblast apoptosis, collagen dismantling, and decreased angiogenesis [53]. Given this knowledge, one group designed lipidoid nanoparticles loaded with siRNA targeting TNF-α-encoding mRNA via RNA interference pathways. These nanoparticles were assessed in a macrophage/fibroblast co-culture designed to mimic the wound environment, where they were found to silence TNF-α mRNA and protein expression at doses that did not cause non-specific gene silencing or cell death. Since TNF-α induces fibroblast production of monocyte chemoattractant protein-1 (MCP-1), the group also demonstrated MCP-1 downregulation in vitro, which could inhibit the recruitment of additional macrophages in wounds [53].
In addition to silencing TNF-α, siRNA-loaded nanoparticles have been employed to knock down a microtubule-severing enzyme and regulator of cell migration called fidgetin-like 2 (FL2). Charafeddine et al. demonstrated that in vitro siRNA-mediated FL2 knockdown can more than double the rate of migration in a variety of cell types, including human keratinocytes, osteosarcoma cells, and mouse fibroblasts in a standard scratch assay [54•]. Next, FL2-targeting siRNA was loaded into nanoparticles and applied topically in murine full-thickness excisional and burn wounds. With either a single treatment on day 0 or two total treatments on days 0 and 2, the nanoparticles significantly accelerated wound closure in both wound models (Fig. 2). Furthermore, the addition of a second treatment on day 2 accelerated closure even more than the single treatment group, indicating that cells did not become refractory to siRNA, and healing could still be further enhanced. After only 7 days post-wounding in the excision model, the nanoparticles were shown to yield a completely reepithelialized epidermis with basket weaving stratum corneum, a less inflammatory dermis infiltrated with parallel fibroblasts, well-organized collagen, and a normal subcutis indicative of healthy scar formation. By contrast, untreated wounds revealed a very thin epidermal layer with mounds of serum crust and an inflammatory, disorganized dermis without evidence of subcutis, as a characteristic of a wound that is still early in the proliferative phase of healing [54•].
Fidgetin-like 2-targeting siRNA-loaded nanoparticles (FL2 NPsi) were applied topically in murine full-thickness excisional wounds, either one dose (day 0) or two doses (days 0 and 2) post-wounding. Representative images (a) show closure of untreated wounds (upper panel) versus wounds treated with two doses of FL2 NPsi. Scale bar = 4 mm. Plots comparing relative wound area of untreated wounds, non-FL2 targeting nanoparticle (control NPsi) treated wounds, and FL2 NPsi treated wounds (b) showed that FL2 NPsi treatment lead to significantly accelerated closure compared to controls. Furthermore, wound closure could be further accelerated with two doses versus one dose of FL2 NPsi. Quantitative PCR (c) of FL2 mRNA performed on days 2 and 8 showed a significant reduction in mRNA in FL2 NPsi treated but not control NPsi treated wounds. *P < 0.05; **P < 0.005; ***P < 0.0005. Error bars denote SEM. Reprinted with permission from [54]
Finally, Zheng et al. utilized spherical nucleic acids (SNAs) that consist of an Au-np core surrounded by dense layers of covalently-attached, highly oriented siRNA (Fig. 3) [55]. In addition to providing protection from nucleases, SNAs offer rapid cellular entry via receptor-mediated endocytosis, as well as protection from off-target effects or other cellular toxicities [56•]. Preliminary studies with keratinocytes in vitro demonstrated that SNAs were more than 100-fold more potent and suppressed their genetic target longer than siRNA that was delivered with commercial lipid agents [55]. Given these benefits, the same group investigated the use of SNAs to target ganglioside-monosialic acid 3 (GM3), a sialylated glycosphingolipid related to insulin resistance and poor healing. Levels of GM3 and GM3 synthase (GM3S) are significantly elevated in diabetic skin samples, and studies have shown that GM3S knockout improves insulin resistance in adipose tissue and muscle, as well as skin. This effectively reverses wound-healing impairments associated with diabetes as evidenced by increased cell migration and proliferation and levels of pro-healing factors [56•]. Following creation of SNAs with siRNA targeting GM3S (GM3S-SNAs), the nanomaterials were delivered topically in mouse and human skin, without the need for epidermal disruption, where they effectively knocked down GM3S. In diabetic mouse wounds, GM3S-SNAs significantly accelerated wound healing compared to vehicle, Au-np alone, or siRNA alone. SNA-treated wounds were completely healed 12 days post-wounding while control wounds were less than 50 % healed at this time point. At day 12, SNA-treated wounds demonstrated fourfold greater area of granulation tissue and twofold greater vascularity on CD31 staining, in addition to significantly greater insulin-like growth factor-1 receptor (IGF1R) and epidermal growth factor receptor (EGFR) activation in wound edge tissue [56•].
Spherical nucleic acids (SNAs) (a) consist of 13 nm gold cores surrounded by dense layers of covalently-attached, highly oriented thiolated siRNA duplexes that target ganglioside-monosialic acid 3 synthase (GM3S). Dynamic light scattering (b) revealed an average hydrodynamic diameter of 32 nm. Quantification studies (c) showed that approximately 40 siRNA duplexes are anchored to each gold nanoparticle, and this remains stable over at least 75 days. Reprinted with permission from [56]
Nanoscaffold Wound Dressings
Bacterial Nanocellulose
While nanoparticle therapies have presented many promising advances for wound healing, nanofibers have also been utilized to enhance wound dressings, an essential component of the wound care armamentarium. Ideal dressings accelerate healing by lowering microbial burden, providing a moist, oxygenated environment, and facilitating cellular attachment and reepithalialization. To create such dressings, bacterial nanocellulose (BNC) has drawn considerable interest given its hydrogel properties, biocompatibility, and ultra-high surface area and nanofibrillar structure, distinct from that of plant cellulose or anything that can currently be achieved synthetically [57]. BNC resembles natural collagen in nanostructure and morphology and its innate properties enhance the healing of wounds [58]. Due to its multiple advantageous properties, BNC has been utilized in dressings, skin substitutes, and implanted medical devices such as artificial menisci and vascular grafts [57].
To harness BNC for wound healing, it is necessary to improve its tensile strength, which is inadequate particularly when BNC is in a highly swollen state. Although a variety of strengthing modifications have been employed, many alter BNC’s natural structure and/or chemical composition, thereby altering its wound-healing properties, as well. To circumvent this issue, Zhang et al. recently manufactured a BNC-chitosan (BNC-CS) hydrogel dressing reinforced with a fabric skeleton that provided enhanced mechanical properties without significantly altering BNC’s native features [57]. The addition of chitosan, a biocompatible, antimicrobial, and anti-inflammatory polysaccharide derived from chitin, a component of crustacean exoskeletons, was achieved using dynamic cultures in a rotating bioreactor so that chitosan’s antimicrobial properties would not stunt the production of BNC [57]. Analysis of the fabric-reinforced BNC-CS hydrogel dressing on field emission scanning electron microscopy demonstrated conservation of BNC nanofibrillar networks and covering of CS on BNC. Infrared spectrophotometry revealed improved water absorption capacity following addition of CS, and tensile strength testing showed excellent mechanical properties and tensile fracture strength. BNC-CS fabric-reinforced hydrogel dressings effectively inhibited E. coli and S. aureus in vitro, thus presenting this dressing as an attractive new therapeutic for wound care.
Instead of adding chitosan for antimicrobial activity, another group engineered BNC wound dressing with incorporated polyhexamethylene biguanide (PHMB), an antimicrobial agent, as well as sericin, a compound that accelerates wound healing. Various loading sequences and concentrations were studied to yield optimal antimicrobial activity and improved collagen production [59]. In vitro, the dressing was non-toxic to mouse fibroblasts and promoted cell migration. When applied to full-thickness wounds in rats, wounds treated with the novel BNC dressing demonstrated significantly reduced wound sizes and greater collagen deposition, and when implanted in rats subcutaneously, a reduced inflammatory response was observed compared to conventional dressing. Finally, a clinical trial patch test involving dressing application to normal skin of healthy volunteers indicated that BNC dressing with PHMB and sericin is non-irritating and may warrant further investigation in clinical wound studies [59].
Silk Fibroin
Silk fibroin has also emerged as a key biomaterial for tissue engineering and wound healing due to its superior mechanical properties, biocompatibility, and ability to promote hemostatsis, as well as adhesion and proliferation of keratinocytes and fibroblasts [60]. In one study, Ju et al. fabricated a silk fibroin nanomatrix via electrospinning. When applied in a rat burn wound model, the silk fibroin nanomatrix demonstrated decreased wound size and increased reepithelialization, with enhanced collagen organization in the dermis compared to simple gauze controls. Compared to controls, the silk fibroin nanomatrix reduced wound levels of pro-inflammatory cytokine IL-1α after 7 days post-wounding. Furthermore, TGF-β1, a mediator of cell proliferation and differentiation, peaked after 21 days in the nanomatrix group versus peaking after 7 days in the gauze controls, thus presenting silk fibroin nanomatrix wound dressings as a potential treatment for burn wounds [60].
In addition to an acute burn wound environment, silk fibroin nanomatrix has been assessed in diabetic rats prone to chronic wounds. Specifically, silk fibroin (SF) was combined with poly(lactide-co-glycolic acid) (PLGA), a biocompatible polymer used for a variety of biomedical and pharmaceutical applications, to create PLGA-SF hybrid nanofiber scaffold dressings. In diabetic rats, PGLA-SF nanofiber dressings decreased wound size after 15 days compared to traditional dressings, and in vitro assessment showed enhanced fibroblast attachment and proliferation, essential for encouraging formation of new ECM and granulation tissue [12].
Conclusions
The data presented here illustrate the vast potential of nanoscaffold wound dressings, physical nanomaterials, and nanomaterials engineered for therapeutic delivery to accelerate healing and reduce the morbidity associated with acute and chronic wounds. In spite of this evidence, it would be imprudent to overlook the fact that nanomaterials for wound healing comprise a relatively new and emerging field, and more in depth studies are needed to determine any potential toxic effects associated with these therapies. Thus far, many investigations have uncovered limited toxicity without significant evidence of nanomaterial absorption systemically; however, standardized methods for assessing the safety of nanomaterials have yet to be established. Given the extensive pre-clinical data regarding nanomaterials for wound healing, there is a paucity of human clinical trial data, and the lack of standardized safety assessments may contribute to this disparity. As the application of nanomaterials for wound healing continues to advance, investigators should pursue standardized methodology for assessing local and systemic effects of nanomaterials. If investigations continue to provide reassuring safety data, clinical studies should be undertaken with urgency to stem patient suffering and economic losses currently caused by acute and chronic wounds.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Tricco AC, Cogo E, Isaranuwatchai W, et al. A systematic review of cost-effectiveness analyses of complex wound interventions reveals optimal treatments for specific wound types. BMC Med. 2015;13(1):1.
Braun LR, Lamel SA, Richmond NA, Kirsner RS. Topical timolol for recalcitrant wounds. JAMA Dermatol. 2013;149(12):1400–2.
Fang RC, Galiano RD. A review of becaplermin gel in the treatment of diabetic neuropathic foot ulcers. Biologics. 2008;2(1):1.
Pereira RF, Bartolo PJ. Traditional therapies for skin wound healing. Adv Wound Care. 2014.
National nanotechnology initiative: Frequently asked questions. Http://www.Nano.Gov/nanotech-101/nanotechnology-facts. Accessed on may 23, 2016.
Kim BY, Rutka JT, Chan WC. Nanomedicine. N Engl J Med. 2010;363(25):2434–43.
Alvarez-Román R, Naik A, Kalia Y, Guy RH, Fessi H. Skin penetration and distribution of polymeric nanoparticles. J Control Release. 2004;99(1):53–62.
Zhou W, Wang Y, Jian J, Song S. Self-aggregated nanoparticles based on amphiphilic poly(lactic acid)-grafted-chitosan copolymer for ocular delivery of amphotericin b. Int J Nanomedicine. 2013;8:3715.
Janát-Amsbury M, Ray A, Peterson C, Ghandehari H. Geometry and surface characteristics of gold nanoparticles influence their biodistribution and uptake by macrophages. Eur J Pharm Biopharm. 2011;77(3):417–23.
Krausz AE, Adler BL, Cabral V, et al. Curcumin-encapsulated nanoparticles as innovative antimicrobial and wound healing agent. Nanomedicine. 2015;11(1):195–206.
Cheirmadurai K, Thanikaivelan P, Murali R. Highly biocompatible collagen–delonix regia seed polysaccharide hybrid scaffolds for antimicrobial wound dressing. Carbohydr Polym. 2016;137:584–93.
Shahverdi S, Hajimiri M, Esfandiari MA, et al. Fabrication and structure analysis of poly (lactide-co-glycolic acid)/silk fibroin hybrid scaffold for wound dressing applications. Int J Pharm. 2014;473(1):345–55.
Wu J, Zheng Y, Song W, et al. In situ synthesis of silver-nanoparticles/bacterial cellulose composites for slow-released antimicrobial wound dressing. Carbohydr Polym. 2014;102:762–71.
Chiara G, Letizia F, Luca L, et al. Nanoparticle therapies for wounds and ulcer healing. Nanomedicine in drug delivery: CRC Press; 2013:143–86.
Stojadinovic A, Carlson JW, Schultz GS, Davis TA, Elster EA. Topical advances in wound care. Gynecol Oncol. 2008;111(2):S70–80.
Nijhawan RI, Smith LA, Mariwalla K. Mohs surgeons’ use of topical emollients in postoperative wound care. Dermatol Surg. 2013;39(8):1260–3.
Morales-Burgos A, Loosemore MP, Goldberg LH. Postoperative wound care after dermatologic procedures: a comparison of 2 commonly used petrolatum-based ointments. J Drugs Dermatol. 2013;12(2):163–4.
Gardin C, Ferroni L, Lancerotto L, et al. Nanoparticle therapies for wounds and ulcer healing. Nanomedicine Drug Deliv. 2013:143.
Bucalo B, Eaglstein WH, Falanga V. Inhibition of cell proliferation by chronic wound fluid. Wound Repair Regen. 1993;1(3):181–6.
Lee JS, Murphy WL. Functionalizing calcium phosphate biomaterials with antibacterial silver particles. Adv Mater. 2013;25(8):1173–9.
Kim K-J, Sung WS, Moon S-K, Choi J-S, Kim JG, Lee DG. Antifungal effect of silver nanoparticles on dermatophytes. J Microbiol Biotechnol. 2008;18(8):1482–4.
Gaikwad S, Ingle A, Gade A, et al. Antiviral activity of mycosynthesized silver nanoparticles against herpes simplex virus and human parainfluenza virus type 3. Int J Nanomedicine. 2013;8:4303.
Cameron P, Gaiser BK, Bhandari B, Bartley PM, Katzer F, Bridle H. Silver nanoparticles decrease the viability of Cryptosporidium parvum oocysts. Appl Environ Microbiol. 2015: AEM. 02806–02815.
Roe D, Karandikar B, Bonn-Savage N, Gibbins B, Roullet J-B. Antimicrobial surface functionalization of plastic catheters by silver nanoparticles. J Antimicrob Chemother. 2008;61(4):869–76.
Lambadi PR, Sharma TK, Kumar P, et al. Facile biofunctionalization of silver nanoparticles for enhanced antibacterial properties, endotoxin removal, and biofilm control. Int J Nanomedicine. 2015;10:2155.
Singh BR, Singh BN, Singh A, Khan W, Naqvi AH, Singh HB. Mycofabricated biosilver nanoparticles interrupt pseudomonas aeruginosa quorum sensing systems. Sci Rep. 2015; 5.
Shahverdi AR, Fakhimi A, Shahverdi HR, Minaian S. Synthesis and effect of silver nanoparticles on the antibacterial activity of different antibiotics against Staphylococcus aureus and Escherichia coli. Nanomedicine. 2007;3(2):168–71.
Xiu Z-m, Zhang Q-b, Puppala HL, Colvin VL, Alvarez PJ. Negligible particle-specific antibacterial activity of silver nanoparticles. Nano Lett. 2012;12(8):4271–5.
Brown AN, Smith K, Samuels TA, Lu J, Obare SO, Scott ME. Nanoparticles functionalized with ampicillin destroy multiple-antibiotic-resistant isolates of pseudomonas aeruginosa and Enterobacter aerogenes and methicillin-resistant Staphylococcus aureus. Appl Environ Microbiol. 2012;78(8):2768–74.
Franková J, Pivodová V, Vágnerová H, Juráňová J, Ulrichová J. Effects of silver nanoparticles on primary cell cultures of fibroblasts and keratinocytes in a wound-healing model. J Appl Biomater Funct Mater. 2016; 14(2).
Tian J, Wong KK, Ho CM, et al. Topical delivery of silver nanoparticles promotes wound healing. ChemMedChem. 2007;2(1):129–36.
GhavamiNejad A, Rajan Unnithan A, Ramachandra Kurup Sasikala A, et al. Mussel-inspired electrospun nanofibers functionalized with size-controlled silver nanoparticles for wound dressing application. ACS Appl Mater Interfaces. 2015;7(22):12176–83.
Lee D, Cohen RE, Rubner MF. Antibacterial properties of ag nanoparticle loaded multilayers and formation of magnetically directed antibacterial microparticles. Langmuir. 2005;21(21):9651–9.
Liu J, Sonshine DA, Shervani S, Hurt RH. Controlled release of biologically active silver from nanosilver surfaces. ACS Nano. 2010;4(11):6903–13.
Morones JR, Elechiguerra JL, Camacho A, et al. The bactericidal effect of silver nanoparticles. Nanotechnology. 2005;16(10):2346.
Zhou Y, Chen R, He T, et al. Biomedical potential of ultrafine ag/agcl nanoparticles coated on graphene with special reference to antimicrobial performances and burn wound healing. ACS Appl Mater Interfaces. 2016. This study presents silver-silver chloride nanoparticles that exhibit antimicrobial activity and enhance wound healing in mouse models independently of silver ion release.
Gu H, Ho P, Tong E, Wang L, Xu B. Presenting vancomycin on nanoparticles to enhance antimicrobial activities. Nano Lett. 2003;3(9):1261–3.
Zharov VP, Mercer KE, Galitovskaya EN, Smeltzer MS. Photothermal nanotherapeutics and nanodiagnostics for selective killing of bacteria targeted with gold nanoparticles. Biophys J. 2006;90(2):619–27.
Norman RS, Stone JW, Gole A, Murphy CJ, Sabo-Attwood TL. Targeted photothermal lysis of the pathogenic bacteria, pseudomonas aeruginosa, with gold nanorods. Nano Lett. 2008;8(1):302–6.
Gil-Tomás J, Tubby S, Parkin IP, et al. Lethal photosensitisation of Staphylococcus aureus using a toluidine blue o–tiopronin–gold nanoparticle conjugate. J Mater Chem. 2007;17(35):3739–46.
Sherwani MA, Tufail S, Khan AA, Owais M. Gold nanoparticle-photosensitizer conjugate based photodynamic inactivation of biofilm producing cells: potential for treatment of C. albicans infection in balb/c mice. PLoS One. 2015;10(7).
Naraginti S, Kumari PL, Das RK, Sivakumar A, Patil SH, Andhalkar VV. Amelioration of excision wounds by topical application of green synthesized, formulated silver and gold nanoparticles in albino wistar rats. Mater Sci Eng C. 2016;62:293–300.
Hsu S-h, Chang Y-B, Tsai C-L, Fu K-Y, Wang S-H, Tseng H-J. Characterization and biocompatibility of chitosan nanocomposites. Colloids Surf B: Biointerfaces. 2011;85(2):198–206.
Volkova N, Yukhta M, Pavlovich O, Goltsev A. Application of cryopreserved fibroblast culture with au nanoparticles to treat burns. Nanoscale Res Lett. 2016;11(1):–6.
Gobin AM, O'Neal DP, Watkins DM, Halas NJ, Drezek RA, West JL. Near infrared laser-tissue welding using nanoshells as an exogenous absorber. Lasers Surg Med. 2005;37(2):123–9.
Ramos R, Silva JP, Rodrigues AC, et al. Wound healing activity of the human antimicrobial peptide ll37. Peptides. 2011;32(7):1469–76.
Garcia-Orue I, Gainza G, Girbau C, et al. Ll37 loaded nanostructured lipid carriers (nlc): a new strategy for the topical treatment of chronic wounds. Eur J Pharm Biopharm. 2016. This group successfully delivered LL37 antimicrobial peptide as a topical wound healing therapy via nanostructured lipid carrier (NLC) encapsulation, which demonstrated wound healing benefits in full-thickness diabetic mouse wounds.
Chereddy KK, Her C-H, Comune M, et al. Plga nanoparticles loaded with host defense peptide ll37 promote wound healing. J Control Release. 2014;194:138–47.
Xu X, Zhu F, Zhang M, et al. Stromal cell-derived factor-1 enhances wound healing through recruiting bone marrow-derived mesenchymal stem cells to the wound area and promoting neovascularization. Cells Tissues Organs. 2012;197(2):103–13.
Yeboah A, Cohen RI, Faulknor R, Schloss R, Yarmush ML, Berthiaume F. The development and characterization of sdf1α-elastin-like-peptide nanoparticles for wound healing. J Control Release. 2016;232:238–47.
Sarkar A, Tatlidede S, Scherer SS, Orgill DP, Berthiaume F. Combination of stromal cell-derived factor-1 and collagen–glycosaminoglycan scaffold delays contraction and accelerates reepithelialization of dermal wounds in wild-type mice. Wound Repair Regen. 2011;19(1):71–9.
Ghatak S, Li J, Chan YC, et al. Antihypoxamir functionalized gramicidin lipid nanoparticles rescue against ischemic memory improving cutaneous wound healing. Nanomed: Nanotechnol, Biol Med. 2016. Lipid nanoparticles were utilized to deliver an antisense inhibitor of hypoxia-induced microRNA that inhibits endogenous mRNA in the setting of ischemic wounds and leads to imparied healing. In mice prone to diabetes and atherosclerosis, a single injection of these nanoparticles significantly improved wound healing.
Kasiewicz LN, Whitehead KA. Silencing tnfα with lipidoid nanoparticles downregulates both tnfα and mcp-1 in an in vitro co-culture model of diabetic foot ulcers. Acta Biomater. 2016;32:120–8.
Charafeddine RA, Makdisi J, Schairer D, et al. Fidgetin-like 2: a microtubule-based regulator of wound healing. J Investig Dermatol. 2015;135(9):2309–18 This group has identified fidgetin-like 2 (FL2), a microtubule-severing enzyme, as a new knockdown target to promote wound healing. In vitro FL2 knockdown demonstrated enhanced cell migration, and nanoparticles delivering FL2-targeting siRNA significantly improved wound healing in vivo in murine full-thickness excision and burn wounds.
Zheng D, Giljohann DA, Chen DL, et al. Topical delivery of sirna-based spherical nucleic acid nanoparticle conjugates for gene regulation. Proc Natl Acad Sci. 2012;109(30):11975–80.
Randeria PS, Seeger MA, Wang X-Q, et al. Sirna-based spherical nucleic acids reverse impaired wound healing in diabetic mice by ganglioside gm3 synthase knockdown. Proc Natl Acad Sci. 2015;112(18):5573–8 Spherical nucleic acids (SNAs) consisting of an Au-np core surrounded by dense layers of covalently-attached, highly oriented siRNA were used to knock down ganglioside-monosialic acid 3 synthase (GM3S), an enzyme related to insulin resistance. Wound healing was accelerated following topical SNA delivery in mouse and human skin, accompanied by increased pro-healing growth factors in wound edge tissue.
Zhang P, Chen L, Zhang Q, Hong FF. Using in situ dynamic cultures to rapidly biofabricate fabric-reinforced composites of chitosan/bacterial nanocellulose for antibacterial wound dressings. Front Microbiol. 2016;7.
Czaja W, Krystynowicz A, Bielecki S, Brown RM. Microbial cellulose—the natural power to heal wounds. Biomaterials. 2006;27(2):145–51.
Napavichayanun S, Yamdech R, Aramwit P. The safety and efficacy of bacterial nanocellulose wound dressing incorporating sericin and polyhexamethylene biguanide: in vitro, in vivo and clinical studies. Arch Dermatol Res. 2016;308(2):123–32.
Ju HW, Lee OJ, Lee JM, et al. Wound healing effect of electrospun silk fibroin nanomatrix in burn-model. Int J Biol Macromol. 2016;85:29–39.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Tarl Prow and Breanne Mordorski declare they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Wound Care and Healing
Rights and permissions
About this article
Cite this article
Mordorski, B., Prow, T. Nanomaterials for Wound Healing. Curr Derm Rep 5, 278–286 (2016). https://doi.org/10.1007/s13671-016-0159-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-016-0159-0