Abstract
Glucagon is a crucial hormone involved in the maintenance of glucose homeostasis. Large efforts to define the role of glucagon receptor (GCGR) have been continuously made in recent years, but it is still incomplete about its function and mechanism. We performed this study to verify its potential impacts on papillary thyroid carcinoma (PTC) progression. Correlation between GCGR expression and PTC was elaborated using The Cancer Genome Atlas (TCGA) database. The Kaplan–Meier method was used to analyze the connection between GCGR expression and prognosis of PTC patients. GCGR expression was measured by quantitative real-time polymerase chain reaction (qRT-PCR) and western blot analysis; simultaneously, cell viability was elucidated using cell proliferation and colony formation assays following siRNAs strategy. Transwell analyses were conducted to measure the invasion and migration of PTC cells. Flow cytometry analysis was conducted to examine apoptotic ability. The cAMP ELISA kit was employed to measure the cAMP level in PTC cells. Our data determined that the expression level of GCGR was increased in PTC tissues and cells in contrast to normal tissues and Nthy-ori 3-1, respectively. Up-regulated GCGR expression was linked with the lower survival rate in patients with PTC. Functional analysis in vitro suggested that GCGR knockdown attenuated PTC cell proliferation, colony formation, invasion, and migration whilst intensified apoptosis. Down-regulated GCGR was able to increase cAMP level. Furthermore, reduction of GCGR could result in the inactivation of epithelial–mesenchymal transition (EMT) and P38/ERK pathways. In conclusion, the findings of this study disclosed that GCGR promoted PTC cell behaviors by mediating the EMT and P38/ERK pathways, serving as a potential diagnostic and prognostic biomarker as well as therapeutic target for PTC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid carcinoma (TC), posing continuous occurrence and high mortality, is the most common endocrine-system-related malignancy [1]. It is classified into four pathological types: papillary thyroid carcinoma (PTC), follicular thyroid carcinoma (FTC), medullary thyroid carcinoma (MTC), and differentiated thyroid carcinoma (DTC) [2, 3]. Among these pathological types, PTC is responsible for more than 85% of all malignant TC with slow tumor growth and better prognosis [3]. Despite advances in clinical therapies in PTC offer a desirable 5-year survival rate [4], high recurrence rates and morbidity are still reminding us of the importance of exploring the molecular mechanisms of PTC and related treatments [5].
It is well established that the occurrence of TC is relevant to hormones, heredity, and other environmental parameters, and thus, the investigation of underlying hormones and their receptors gain more attentions currently [6]. Glucagon is a hormone secreted by pancreatic islet α-cells and consists of a 29 amino acid linear polypeptide. Its physiological functions are exerted via the activation of glucagon receptor (GCGR) [7]. As we all known, GCGR is a G-protein-coupled receptor (GPCR) regulating blood glucose levels and mainly expressed in pancreas, liver, and kidneys [8]. By coupling to guanine nucleotide-binding proteins (G proteins), many biological functions are modulated by GPCRs [9]. Recent studies further validated the correlation between aberrant expression of GPCRs and cancer progression. Down-regulation of leucine-rich repeat-containing G-protein coupled receptor 6 (Lgr6) held the capability to suppress the cell proliferation and invasion in human colorectal cancer [10]. The study of Ye et al. disclosed that GPRC6A was involved in the pathogenesis of prostate cancer [11]. Increased occurrence of skin cancer was induced by the polymorphisms of melanocortin-1 receptor [12]. Up-regulated GPR30 was associated with tumor recurrence and promoted breast cancer cell adhesion, migration, and invasion [13, 14]. Glucagon-like peptide-1 receptor (GLP-1R) was highly expressed in endometrial cancer and evidently related with better prognosis [15]. However, a limited amount of studies has been conducted to explore the role of GCGR in PTC when compared with the other GPCRs in this context.
In our study, we disclosed that GCGR expression was highly regulated in PTC and connected with poor prognosis of PTC patients. In addition, the findings of in vitro functional analysis indicated that GCGR deficiency inhibited proliferation, colony formation, invasion, and migration while stimulated apoptosis. The cAMP level of PTC cells was negatively related with GCGR expression. These observations were proved to be associated with the EMT and P38/ERK pathways. Therefore, deciphering the role of GCGR in PTC might shed new insight on our understanding of potential mechanism driving PTC progression and improve PTC treatment.
Materials and methods
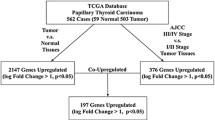
Gene expression analysis in tumor tissues
The gene expression profile derived from TCGA database was composed of 58 normal specimens and 510 human tumor cases, which was used to show the GCGR expression level in PTC tissues. We enrolled 415 patients with complete clinical data to analyze the correlation between GCGR expression and clinical characteristics by Chi square test. The overall survival (OS) curves were plotted using Kaplan–Meier method with log-rank test. Cox regression analysis was applied to explore whether GCGR is an independent predictor of prognosis for PTC.
Cell culture
The human normal thyroid gland cell line Nthy-ori 3-1 and human PTC cell lines including SW579, TT, FTC-133 were purchased from Cell Biology of the Chinese Academy of Sciences (Shanghai, China). Cells were cultured in Roswell Park Memorial Institute (RPMI) 1640 medium with fetal bovine serum (10% FBS; Gibco, Grand Island, NY, USA), penicillin (100 U/mL; Gibco), and streptomycin (0.1 mg/mL; Gibco). The cell culture condition was held at 37 °C and 5% CO2.
Cell transfection
To decrease the expression level of GCGR, siRNA technology was conducted with two siRNAs, si-GCGR#1 and si-GCGR#2, accompanying with siRNA control (si-con). The targets of siRNAs for GCGR are exhibited as follows: si-GCGR#1, 5′-GCACCACACAGACTACAAGTT-3′; si-GCGR#2, 5′-CGCGAATCTGTTTGCGTCCTT-3′; si-con, and 5′-CGAACUCACUGGUCUGACC-3′. The transfection was performed by the means of Lipofectamine2000 in the further experiments.
qRT-PCR
The qRT-PCR was run according to the following steps. At first, TRIzol solution (Invitrogen, Carlsbad, CA, USA) was utilized to separate the whole RNA from transfected cells. Second, TranScript First-Strand cDNA Synthesis SuperMix (Transgen Biotech, Beijing, China) was employed to transcribe cDNA, and finally, qRT-PCR was determined by TransScript® II Green One-Step qRT-PCR SuperMix (Transgen Biotech) on the 7900HT real-time PCR system. To analyze the relative expression level, GAPDH was considered as the internal control relying on 2−∆∆Ct method. Specific primers are shown subsequently: GCGR: F, 5′-CGCTGACCCTCATCCCTCCTG-3′, R: 5′-TAGAGGACAGCCACCAGCAG-3′; Tubulin: F: 5′-CTCAAGAGGCTGACGCAGAA-3′, R: 5′-AGGAGATGCTGGTGTGGTTG-3′. Each sample was examined in three times.
Western blot analysis
After 48 h transfection, cells were placed into 6-well plate, homogenized with RIPA lyses containing protease inhibitor, and then assessed the protein concentrations using BCA method. Following denatured proteins at 95 °C for 5 min, the equal amount protein was separated with SDS-PAGE and transferred onto polyvinylidene difluoride membrane (PVDF; Millipore Corp., Bedford, MA, USA) membrane. Then, the PVDF membranes were incubated with 5% skim milk for 1 h at 25 °C. Then, the membranes were incubated with primary antibodies and secondary antibody in succession. Protein signals were probed with enhanced chemiluminescence, revealed on films, and scanned by QUANTITY ONE software.
Cell counting kit 8 assay
SW579 and FTC-133 cells were inoculated in 96-well plate at a density of 1000 cells per well in a humidified atmosphere containing 5% CO2 at 37 °C. After 0 h, 24 h, 48 h, and 72 h, 10 μL CCK8 regents was added into per well, then maintained cells for additional 1.5 h, and examined the optical density (OD) values under the microplate reader with a wavelength of 450 nm.
Colony formation assay
A total of cells (400 cells/dish) were seeded in 60 mm dish at a carbon dioxide incubator that set at 37 °C with 5% for 1 or 2 weeks. The colonies were fixed using paraformaldehyde (4%) and dyed by crystal violet (0.1%), respectively.
Transwell analysis
Cell invasion and migration assays were performed utilizing transwell chamber. For invasion detection, the inserts of 24-well plates were pre-coated with 100 μL Matrigel-diluted 1:6 with serum-free medium. The 24 h-transfected cells (1 × 105) were suspended into cell suspension and added to the upper chamber, while the lower chamber was filled with 500 μL serum-free medium. After incubation 24 h, remaining cells were wiped out with the help of cotton swabs; meanwhile, invasive cells were fixed and stained by paraformaldehyde (4%) for 30 min and crystal violet (0.1%) for 20 min. Differently, the inoculated density of migration detection was 5000 cells per well and there was no Matrigel coated on the inserts.
Flow cytometry analysis
Briefly, cells were inoculated into 6-well plates and treated with si-con or si-GCGR#2. After transfection for 48 h, cells were washed with PBS and resuspended by binding buffer. Then, cells were stained with 5 μL Annexin V FITC for 10 min in the dark and incubated with 5 μL PI reagent for 5 min. Finally, cell apoptosis was assessed by a flow cytometry (BD Biosciences, Franklin Lakes, NJ, USA) and analyzed using FlowJo software (BD Biosciences).
Detection of cAMP level
To measure the intracellular cAMP level, cells were first preincubated in serum-free medium for 30 min. Then, cells were lysed and the intracellular cAMP level was evaluated using cAMP ELISA kit (Cell Signaling Technology, Danvers, MA, USA) according to the manufacturer’s protocols.
Statistically analysis
Student’s t test and one-way analysis of variance with Dunnett’s (compare all groups versus control group) or Tukey’s (compare all pairs of groups) post hoc tests were implemented to describe the differences between groups. SPSS 22.0 software and GraphPad Prism 5.0 software were employed to analyze results and all data were exhibited as the mean ± standard deviation (SD). Statistical significance was depicted as P < 0.05.
Results
GCGR was highly expressed in PTC tissues and correlated with prognostic outcome and pathological characteristics
Clinical profiles obtained from TCGA database demonstrated that GCGR expression was significantly high-regulated in PTC tissues compared with the normal tissues throughout qRT-PCR analysis (Fig. 1a, P < 0.01). Then, on the basis of median value of GCGR expression, the data were classified into high expression group (> median value) and low expression group (< median value). As can be seen in Fig. 1b, the OS rate was remarkably higher in low expression group (n = 207) than that in high expression group (n = 208) (P = 0.027), indicating that GCGR might stimulate PTC progression. GCGR expression presented a positive correlation with the tumor (P = 0.002) and death (P = 0.020) in Table 1. Moreover, the Cox regression analysis demonstrated that GCGR might act as an independent predictor for PTC diagnosis (Table 2, P < 0.05).
GCGR was up-regulated in PTC cell lines and depleted using siRNA strategy
Considering the expression level of GCGR in PTC tissues, the GCGR expression was examined in PTC cell lines and found that GCGR mRNA expression level was significantly increased in PTC cell lines (SW579, TT, FTC-133) compared to Nthy-ori 3-1 cell line (Fig. 2a, P < 0.01). In consistent with the GCGR mRNA expression level in PTC cell lines, the protein expression level of GCGR in PTC was higher than that in Nthy-ori 3-1 cell line by western blot analyses (Fig. 2b, c, P < 0.01).
The expression level of GCGR in PTC cell lines and silence efficiency by siRNA method. a GCGR was highly expressed in three PTC cell lines compared with Nthy-ori 3-1 cell line, **P < 0.01. b Different protein expression levels of GCGR in three PTC cell lines and normal thyroid gland cell line Nthy-ori 3-1. c The quantification of gray value, **P < 0.01. c After si-GCGR#1 and si-GCGR#2 transfection, the expression of GCGR was markedly decreased in comparison to si-con group, **P < 0.01. d Western blotting analysis of silence efficiency. e The fold change of protein bands, **P < 0.01. Each experiment was performed in three times independently
To down-regulate GCGR expression, si-GCGR#1 and si-GCGR#2 were used to treat SW579 cells. According to the qRT-PCR analysis, we observed that GCGR was suppressed successfully when compared with si-con group (Fig. 2d, P < 0.01). In consistent with that, western blot test indicated a similar tendency at the aspect of GCGR protein expression level (Fig. 2e, f, P < 0.01). More importantly, Fig. 2d, e shows that the interference of si-GCGR#2 provided higher silence efficiency than si-GCGR#1. Therefore, the next knockdown experiments were completed by si-GCGR#2.
Knockdown of GCGR had an inhibitory effect on proliferation, colony formation, invasion, and migration, whilst had a promoting impact on apoptosis and cAMP level.
To ulteriorly assess the potential contribution of GCGR to PTC cell behaviors, CCK8, colony formation, transwell assays, and flow cytometry assay were conducted in SW579 and FTC-133 cells. Based on the CCK8 assay, cell proliferation of SW579 cells transfected with si-GCGR#2 was blocked in contrast to the si-con group, especially at 72 h (Fig. 3a, P < 0.01). Consistently, colony formation assay also verified that GCGR knockdown induced the attenuation of clone number in SW579 cells (Fig. 3c, P < 0.01). Transwell assay demonstrated that GCGR reduction had a negative impact on the invasion and migration of SW579 cells (Fig. 3e, P < 0.01). Meanwhile, the similarly suppressive effect of GCGR deficiency on proliferative, clonogenic, invasive, and migratory capabilities was also exhibited in FTC-133 cells (Fig. 3b, d, f, P < 0.01).
Knockdown of GCGR inhibited the proliferation, colony formation, invasion, and migration. Cell proliferative ability was examined after GCGR knockdown in a SW579 and b FTC-133, **P < 0.01. Colony formation assay was performed and clone number was calculated using c SW579 and d FTC-133, respectively, **P < 0.01. Transwell assays showed the difference of invasive and migratory capabilities in e SW579 and f FTC-133, and then, corresponding cell number was counted, **P < 0.01. All the experiments were conducted in triplicates
In addition, flow cytometry analyses were performed in SW579 and FTC-133 cells and uncovered that knockdown of GCGR with the application of si-GCGR#2 markedly elevated the rate of apoptosis of SW579 (Fig. 4a, b, P < 0.01) and FTC-133 cells (Fig. 4c, d, P < 0.01).
Apoptotic capability and cAMP level of PTC cells were promoted after GCGR knockdown. a, b Apoptotic potential was measured by flow cytometry analysis in SW579 cells. The percentage of apoptosis cells was quantified, **P < 0.01. c, d Apoptosis of FTC-133 cells was determined by flow cytometry, **P < 0.01. e Intracellular cAMP level in PTC cells before and after treated with si-GCGR#2, **P < 0.01. Each experiment was repeated in three times
Previous evidence has indicated that cAMP level is negatively correlated with proliferative ability of cancer cells [16, 17]. To examine the functionality of GCGR expressed in PTC cells, we measured the intracellular cAMP level in PTC cells transfected before and after GCGR knockdown. Results showed that cAMP level was higher in si-GCGR#2 group than in blank control group (Fig. 4e, P < 0.01), indicating that cAMP level was negatively correlated to GCGR expression in PTC cells.
Taken together, these findings suggested that knockdown of GCGR had an inhibitory effect on proliferation, colony formation, invasion, and migration, whilst had a promoting impact on apoptosis.
Reduction of GCGR impaired the activation of EMT and P38/ERK pathways
To explore the potential mechanism of how GCGR affects the cell behaviors of PTC cells, we detected the EMT and P38/ERK pathway-related gene expression using western blotting. It has been reported that EMT is an important process related with tumor invasion and migration [18]. Extensive studies have suggested that GCGR could contribute to tumorigenesis by regulating the activation of P38/ERK pathway [19, 20]. Therefore, western blotting method was performed to elevate the management of EMT and P38/ERK pathways after GCGR depletion in SW579 cells. Results of western blotting revealed that GCGR knockdown significantly improved the expression of E-cadherin and down-regulated the expression of N-cadherin, Vimentin, and Snail in SW579 cells (Fig. 5a, b, P < 0.01). In addition, results in Fig. 5c identified that the expression levels of P38 and ERK were unchanged in SW579 cells transfected with si-GCGR#2. However, the si-GCGR#2-transfected SW579 cells suggested that the phosphorylation of P38 and ERK was decreased compared with the si-con-treated SW579 cells (Fig. 5c). The quantitative results were the same as the protein bands (Fig. 5d, P < 0.01). Overall, our data illustrated that reduction of GCGR affected the activation of EMT and P38/ERK pathways, which correlated with the change of proliferation, colony formation, invasion, migration, and apoptosis revealed in PTC cells.
Knockdown of GCGR had a significant effect on EMT and P38/ERK pathways in SW579 cells. a E-cadherin expression was promoted, while N-cadherin, Vimentin, and Snail were inhibited in si-GCGR#2 group relative to si-con group. b The quantification of a, **P < 0.01. c The phosphorylation of P38 and ERK was attenuated in si-GCGR#2 group when compared with si-con group, **P < 0.01. d The fold change of protein bands, **P < 0.01
Discussion
PTC is the most frequent subtype of TC with complicated environmental and molecular factors [6]. To date, increased evidence of clinical analyses of PTC has made a greatly progress in diagnosis and prognosis in PTC [21]. Although some targets have been examined in PTC progression preliminarily, the perfect treatment of PTC is still unknown. Therefore, we accessed to TCGA data set to collect and analyze the profile of PTC clinical samples, and found that GCGR was highly regulated in PTC tissues. The overall survival rates showed that up-regulation of GCGR was positively correlated with the worse prognosis of PTC patients. To further identify the correlation between GCGR and PTC, we then utilized the qRT-PCR analysis and western blotting to assess the relative expression level of GCGR in PTC cell lines; the result was consistent with those of the data in clinical specimens when compared with Nthy-ori 3-1 cells. Thus, we speculated that GCGR might be a potential biomarker for PTC development.
Much of the current literature on GCGR pays particular attention to its function in the regulation of blood glucose. For example, Okamoto et al. uncovered the inhibition of GCGR which can lead to a normalized blood glucose in severe insulin-resistant mice [22]. Abnormal expression of angiopoietin-like 4 (Angptl4) was related with α-cell proliferation in endocrine pancreas via inhibiting GCGR activation [23]. Importantly, the mutations of GCGR were closely linked with the occurrence of glucagon cell adenomatosis by means of glucagon cell hyperplasia [24]. A new therapy of type 2 diabetes was proposed by Graham et al., which is based on the regulatory effects of dual GCGR [25]. The antibody for glucagon receptor can hinder type 1 diabetes through disordering the diabetogenic pathway [26]. Notably, Luo et al. highlighted that thyroid cancer risk can be increased by the occurrence of type 2 diabetes [27]. Moreover, thyroid dysfunction and abnormal thyroid stimulating hormone concentration, the reasons linked with higher prevalence of thyroid cancer, have been observed in patients with type 2 diabetes [28, 29]. In addition to the blood glucose-related diseases, a few and growing body emphasize on the effects of GCGR in additional malignancies. Energy metabolism, participating in diverse biological processes, is mediated by GCGR signaling through hepatic farnesoid X receptor and fibroblast growth factor 21 [30]. Using the mice model with myocardial infraction, the outcomes of mice are controlled by cardiomyocyte GCGR signaling and cardiac function can be improved by targeting the GCGR [31, 32]. It is the essential step for the murine hepatocyte survival [33]. Considering the above-mentioned data, we performed experiments in vitro to verify our hypothesis. The findings revealed that GCGR knockdown played an inhibitory role on the proliferation, colony formation, invasion, and migration, and facilitated to apoptosis in SW579 and FTC-133 cells in comparison with the si-con group. In addition, it has been previously reported that high-regulated cAMP level can impair the proliferation in cancers [34]. Thus, we measured the cAMP level of PTC cells before and after GCGR deficiency to determine the functionality of GCGR expression. The findings revealed that knockdown of GCGR increased the cAMP level in PTC cells.
Given the impacts of GCGR knockdown on the cell invasion and migration in PTC cells, we measured the EMT-related genes expression by western blot analysis. As described in previous reports, cell invasion and migration are pivotal aspects of tumorigenesis and EMT is required for cell invasion and migration of tumor cells as an important transformation process driving the invasive phenotype of tumors [35, 36]. Studies suggested that many important oncogenes and cancer suppressors implicated in cancer progression could mediate the EMT process [37]. The activation of EMT process has been verified correlated with various signaling pathways, including P38/ERK pathway [38]. Up to date, there are three MAPKs including P38, extracellular signal-regulated kinases (ERKs) and c-jun NH2-terminal kinases (JNK) [39]. There is a large volume of published studies describing the role of P38/ERK pathway in multiple tumors, such as non-small cell lung cancer, cervical cancer, breast cancer, prostate cancer, hepatocellular carcinoma, and so on [40,41,42,43]. Moreover, the progression of PTC has been demonstrated that has a significantly connection with the activation of MAPK pathway, especially P38/ERK pathway [44,45,46]. In our study, we analyzed the effect of GCGR knockdown on the expression level of EMT-related genes and phosphorylation of P38/ERK. After knockdown the expression of GCGR, E-cadherin was increased, and N-cadherin, Vimentin, and Snail were decreased. The phosphorylation of P38/ERK was declined compared to the si-con group. These observations hinted that GCGR possibly regulated cell malignant aggressiveness through the EMT and P38/ERK pathways.
In conclusion, the results of our investigation elaborated that GCGR was highly regulated in PTC tissues and cells. The high regulation of GCGR was remarkably associated with poor outcome of PTC patients, indicating a shorter survival period. Furthermore, functional analysis in vitro suggested that reduction of GCGR impaired cell proliferation, colony formation, invasion, and migration via mediating the EMT and P38/ERK pathways in PTC. Meanwhile, down-regulated GCGR expression elevated the cAMP level in PTC cells. Collectively, GCGR might become a favorable therapeutic target for PTC development.
References
Cabanillas ME, McFadden DG, Durante C. Thyroid cancer. Lancet (London, England). 2016;388(10061):2783–95. https://doi.org/10.1016/s0140-6736(16)30172-6.
Gezer E, Selek A, Tarkun I, Canturk Z, Cetinarslan B. Papillary thyroid carcinoma presenting as a primary renal tumor with multiple pulmonary and bone metastases: a case report. J Med Case Rep. 2019;13(1):95. https://doi.org/10.1186/s13256-019-2025-8.
Zhu J, Zhang Q, Jin XY, Cai JB, Chen X, Shi WB, et al. MiR-506 suppresses papillary thyroid carcinoma cell proliferation and metastasis via targeting IL17RD. Eur Rev Med Pharmacol Sci. 2019;23(7):2856–62. https://doi.org/10.26355/eurrev_201904_17563.
Du L, Wang Y, Sun X, Li H, Geng X, Ge M, et al. Thyroid cancer: trends in incidence, mortality and clinical-pathological patterns in Zhejiang Province, Southeast China. BMC Cancer. 2018;18(1):291. https://doi.org/10.1186/s12885-018-4081-7.
Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940–1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg. 2002;26(8):879–85. https://doi.org/10.1007/s00268-002-6612-1.
Wei ZL, Gao AB, Wang Q, Lou XE, Zhao J, Lu QJ. MicroRNA-221 promotes papillary thyroid carcinoma cell migration and invasion via targeting RECK and regulating epithelial-mesenchymal transition. Oncotargets Ther. 2019;12:2323–33. https://doi.org/10.2147/OTT.S190364.
Mayo KE, Miller LJ, Bataille D, Dalle S, Goke B, Thorens B, et al. International Union of Pharmacology. XXXV. The glucagon receptor family. Pharmacol Rev. 2003;55(1):167–94. https://doi.org/10.1124/pr.55.1.6.
Bansal P, Wang Q. Insulin as a physiological modulator of glucagon secretion. Am J Physiol Endocrinol Metab. 2008;295(4):E751–61. https://doi.org/10.1152/ajpendo.90295.2008.
Kobilka BK. G protein coupled receptor structure and activation. Biochem Biophys Acta. 2007;1768(4):794–807. https://doi.org/10.1016/j.bbamem.2006.10.021.
Wang F, Dai CQ, Zhang LR, Bing C, Qin J, Liu YF. Downregulation of Lgr6 inhibits proliferation and invasion and increases apoptosis in human colorectal cancer. Int J Mol Med. 2018;42(1):625–32. https://doi.org/10.3892/ijmm.2018.3633.
Ye R, Pi M, Cox JV, Nishimoto SK, Quarles LD. CRISPR/Cas9 targeting of GPRC6A suppresses prostate cancer tumorigenesis in a human xenograft model. J Exp Clin Cancer Res CR. 2017;36(1):90. https://doi.org/10.1186/s13046-017-0561-x.
Demenais F, Mohamdi H, Chaudru V, Goldstein AM, Newton Bishop JA, Bishop DT, et al. Association of MC1R variants and host phenotypes with melanoma risk in CDKN2A mutation carriers: a GenoMEL study. J Natl Cancer Inst. 2010;102(20):1568–83. https://doi.org/10.1093/jnci/djq363.
Shang D, Li Z, Zhu Z, Chen H, Zhao L, Wang X, et al. Baicalein suppresses 17-beta-estradiol-induced migration, adhesion and invasion of breast cancer cells via the G protein-coupled receptor 30 signaling pathway. Oncol Rep. 2015;33(4):2077–85. https://doi.org/10.3892/or.2015.3786.
Wei W, Chen ZJ, Zhang KS, Yang XL, Wu YM, Chen XH, et al. The activation of G protein-coupled receptor 30 (GPR30) inhibits proliferation of estrogen receptor-negative breast cancer cells in vitro and in vivo. Cell Death Dis. 2014;5:e1428. https://doi.org/10.1038/cddis.2014.398.
Kanda R, Hiraike H, Wada-Hiraike O, Ichinose T, Nagasaka K, Sasajima Y, et al. Expression of the glucagon-like peptide-1 receptor and its role in regulating autophagy in endometrial cancer. BMC Cancer. 2018;18(1):657. https://doi.org/10.1186/s12885-018-4570-8.
Wang W, Li Y, Zhu JY, Fang D, Ding HF, Dong Z, et al. Triple negative breast cancer development can be selectively suppressed by sustaining an elevated level of cellular cyclic AMP through simultaneously blocking its efflux and decomposition. Oncotarget. 2016;7(52):87232–45. https://doi.org/10.18632/oncotarget.13601.
Zhang DD, Li Y, Xu Y, Kim J, Huang S. Phosphodiesterase 7B/microRNA-200c relationship regulates triple-negative breast cancer cell growth. Oncogene. 2019;38(7):1106–20. https://doi.org/10.1038/s41388-018-0499-2.
Yuan JH, Yang F, Wang F, Ma JZ, Guo YJ, Tao QF, et al. A long noncoding RNA activated by TGF-beta promotes the invasion-metastasis cascade in hepatocellular carcinoma. Cancer Cell. 2014;25(5):666–81. https://doi.org/10.1016/j.ccr.2014.03.010.
Du Z, Wang Q, Ma G, Jiao J, Jiang D, Zheng X, et al. Inhibition of Nrf2 promotes the antitumor effect of Pinelliae rhizome in papillary thyroid cancer. J Cell Physiol. 2019;234(8):13867–77. https://doi.org/10.1002/jcp.28069.
Wang N, Li Y, Wei J, Pu J, Liu R, Yang Q, et al. TBX1 functions as a tumor suppressor in thyroid cancer through inhibiting the activities of the PI3K/AKT and MAPK/ERK pathways. Thyroid. 2019;29(3):378–94. https://doi.org/10.1089/thy.2018.0312.
Ferrari SM, Antonelli A, Guidi P, Bernardeschi M, Scarcelli V, Fallahi P, et al. Genotoxicity evaluation of the soybean isoflavone genistein in human papillary thyroid cancer cells. Study of its potential use in thyroid cancer therapy. Nut Cancer. 2019. https://doi.org/10.1080/01635581.2019.1604004.
Okamoto H, Cavino K, Na E, Krumm E, Kim SY, Cheng X, et al. Glucagon receptor inhibition normalizes blood glucose in severe insulin-resistant mice. Proc Natl Acad Sci USA. 2017;114(10):2753–8. https://doi.org/10.1073/pnas.1621069114.
Ben-Zvi D, Barrandon O, Hadley S, Blum B, Peterson QP, Melton DA. Angptl4 links alpha-cell proliferation following glucagon receptor inhibition with adipose tissue triglyceride metabolism. Proc Natl Acad Sci USA. 2015;112(50):15498–503. https://doi.org/10.1073/pnas.1513872112.
Sipos B, Sperveslage J, Anlauf M, Hoffmeister M, Henopp T, Buch S, et al. Glucagon cell hyperplasia and neoplasia with and without glucagon receptor mutations. J Clin Endocrinol Metab. 2015;100(5):E783–8. https://doi.org/10.1210/jc.2014-4405.
Graham GV, Conlon JM, Abdel-Wahab YH, Flatt PR. Glucagon-related peptides from phylogenetically ancient fish reveal new approaches to the development of dual GCGR and GLP1R agonists for type 2 diabetes therapy. Peptides. 2018;110:19–29. https://doi.org/10.1016/j.peptides.2018.10.013.
Wang MY, Yan H, Shi Z, Evans MR, Yu X, Lee Y, et al. Glucagon receptor antibody completely suppresses type 1 diabetes phenotype without insulin by disrupting a novel diabetogenic pathway. Proc Natl Acad Sci USA. 2015;112(8):2503–8. https://doi.org/10.1073/pnas.1424934112.
Luo J, Phillips L, Liu S, Wactawski-Wende J, Margolis KL. Diabetes, diabetes treatment, and risk of thyroid cancer. J Clin Endocrinol Metab. 2016;101(3):1243–8. https://doi.org/10.1210/jc.2015-3901.
Perros P, McCrimmon RJ, Shaw G, Frier BM. Frequency of thyroid dysfunction in diabetic patients: value of annual screening. Diab Med J Br Diab Assoc. 1995;12(7):622–7.
Celani MF, Bonati ME, Stucci N. Prevalence of abnormal thyrotropin concentrations measured by a sensitive assay in patients with type 2 diabetes mellitus. Diabetes research (Edinburgh, Scotland). 1994;27(1):15–25.
Kim T, Nason S, Holleman C, Pepin M, Wilson L, Berryhill TF, et al. Glucagon receptor signaling regulates energy metabolism via hepatic farnesoid X receptor and fibroblast growth factor. Diabetes. 2018;67(9):1773–82. https://doi.org/10.2337/db17-1502.
Ali S, Ussher JR, Baggio LL, Kabir MG, Charron MJ, Ilkayeva O, et al. Cardiomyocyte glucagon receptor signaling modulates outcomes in mice with experimental myocardial infarction. Mol Metab. 2015;4(2):132–43. https://doi.org/10.1016/j.molmet.2014.11.005.
Karwi QG, Zhang L, Wagg CS, Wang W, Ghandi M, Thai D, et al. Targeting the glucagon receptor improves cardiac function and enhances insulin sensitivity following a myocardial infarction. Cardiovasc Diabetol. 2019;18(1):1. https://doi.org/10.1186/s12933-019-0806-4.
Sinclair EM, Yusta B, Streutker C, Baggio LL, Koehler J, Charron MJ, et al. Glucagon receptor signaling is essential for control of murine hepatocyte survival. Gastroenterology. 2008;135(6):2096–106. https://doi.org/10.1053/j.gastro.2008.07.075.
Naviglio S, Di Gesto D, Illiano F, Chiosi E, Giordano A, Illiano G, et al. Leptin potentiates antiproliferative action of cAMP elevation via protein kinase A down-regulation in breast cancer cells. J Cell Physiol. 2010;225(3):801–9. https://doi.org/10.1002/jcp.22288.
Ye X, Brabletz T, Kang Y, Longmore GD, Nieto MA, Stanger BZ, et al. Upholding a role for EMT in breast cancer metastasis. Nature. 2017;547(7661):e1–3. https://doi.org/10.1038/nature22816.
Luo X, Qiu Y, Jiang Y, Chen F, Jiang L, Zhou Y, et al. Long non-coding RNA implicated in the invasion and metastasis of head and neck cancer: possible function and mechanisms. Mol Cancer. 2018;17(1):14. https://doi.org/10.1186/s12943-018-0763-7.
Zhang Y, Weinberg RA. Epithelial-to-mesenchymal transition in cancer: complexity and opportunities. Front Med. 2018;12(4):361–73. https://doi.org/10.1007/s11684-018-0656-6.
Cho JH, Hong WG, Jung YJ, Lee J, Lee E, Hwang SG, et al. Gamma-Ionizing radiation-induced activation of the EGFR-p38/ERK-STAT3/CREB-1-EMT pathway promotes the migration/invasion of non-small cell lung cancer cells and is inhibited by podophyllotoxin acetate. Tumour Biol J Int Soc Oncodev Biol Med. 2016;37(6):7315–25. https://doi.org/10.1007/s13277-015-4548-y.
Lei YY, Wang WJ, Mei JH, Wang CL. Mitogen-activated protein kinase signal transduction in solid tumors. Asian Pac J Cancer Prev APJCP. 2014;15(20):8539–48.
Zhang G, He J, Ye X, Zhu J, Hu X, Shen M, et al. beta-Thujaplicin induces autophagic cell death, apoptosis, and cell cycle arrest through ROS-mediated Akt and p38/ERK MAPK signaling in human hepatocellular carcinoma. Cell Death Dis. 2019;10(4):255. https://doi.org/10.1038/s41419-019-1492-6.
Wang Y, Yu L, Wang T. MicroRNA-374b inhibits the tumor growth and promotes apoptosis in non-small cell lung cancer tissue through the p38/ERK signaling pathway by targeting JAM-2. J Thorac Dis. 2018;10(9):5489–98. https://doi.org/10.21037/jtd.2018.09.93.
Li GC, Cao XY, Li YN, Qiu YY, Li YN, Liu XJ, et al. MicroRNA-374b inhibits cervical cancer cell proliferation and induces apoptosis through the p38/ERK signaling pathway by binding to JAM-2. J Cell Physiol. 2018;233(9):7379–90. https://doi.org/10.1002/jcp.26574.
Tang G, Du R, Tang Z, Kuang Y. MiRNALet-7a mediates prostate cancer PC-3 cell invasion, migration by inducing epithelial-mesenchymal transition through CCR43/MAPK pathway. J Cell Biochem. 2018;119(4):3725–31. https://doi.org/10.1002/jcb.26595.
Song B, Li R, Zuo Z, Tan J, Liu L, Ding D, et al. LncRNA ENST00000539653 acts as an oncogenic factor via MAPK signalling in papillary thyroid cancer. BMC Cancer. 2019;19(1):297. https://doi.org/10.1186/s12885-019-5533-4.
Liu F, Yin R, Chen X, Chen W, Qian Y, Zhao Y, et al. Over-expression of miR-206 decreases the Euthyrox-resistance by targeting MAP4K3 in papillary thyroid carcinoma. Biomed Pharmacother. 2019;114:108605. https://doi.org/10.1016/j.biopha.2019.108605.
Fuziwara CS, Saito KC, Leoni SG, Waitzberg AFL, Kimura ET. The highly expressed FAM83F protein in papillary thyroid cancer exerts a pro-oncogenic role in thyroid follicular cells. Front Endocrinol. 2019;10:134. https://doi.org/10.3389/fendo.2019.00134.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jiang, HC., Chen, XR., Sun, HF. et al. Tumor promoting effects of glucagon receptor: a promising biomarker of papillary thyroid carcinoma via regulating EMT and P38/ERK pathways. Human Cell 33, 175–184 (2020). https://doi.org/10.1007/s13577-019-00284-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-019-00284-y