Abstract
Natalizumab is effective against multiple sclerosis (MS), but is associated with progressive multifocal leukoencephalopathy (PML), fatal disease caused by the JCV polyomavirus. The SF2/ASF (splicing factor2/alternative splicing factor) inhibits JCV in glial cells. We wondered about SF2/ASF modulation in the blood of natalizumab-treated patients and if this could influence JCV reactivation. Therefore, we performed a longitudinal study of MS patients under natalizumab, in comparison to patients under fingolimod and to healthy blood donors. Blood samples were collected at time intervals. The expression of SF2/ASF and the presence and expression of JCV in PBMC were analyzed. A bell-shaped regulation of SF2/ASF was observed in patients treated with natalizumab, increased in the first year of therapy, and reduced in the second one, while slightly changed, if any, in patients under fingolimod. Notably, SF2/ASF was up-regulated, during the first year, only in JCV DNA-positive patients, or with high anti-JCV antibody response; the expression of the JCV T-Ag protein in circulating B cells was inversely related to SF2/ASF protein expression. The SF2/ASF reduction, parallel to JCV activation, during the second year of therapy with natalizumab, but not with fingolimod, may help explain the increased risk of PML after the second year of treatment with natalizumab, but not with fingolimod. We propose that SF2/ASF has a protective role against JCV reactivation in MS patients. This study suggests new markers of disease behavior and, possibly, help in re-evaluations of therapy protocols.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Natalizumab is a therapeutic monoclonal antibody for the treatment of relapsing–remitting multiple sclerosis (MS) and of Crohn’s disease (CD; Craddock and Markovic-Plese 2015; Kornek 2015; Baroncini et al. 2016). It inhibits the α4integrin-mediated adhesion of leukocytes to their counter-receptor(s) and the transmigration across the endothelia of activated leukocytes into MS brain parenchima, hence its effects in preventing disease progression (Kappos et al. 2013; Vitaliti et al. 2015). Unfortunately, natalizumab use is associated with the development of progressive multifocal leukoencephalopathy (PML), fatal demyelinating disease due to the lytic infection of brain oligodendrocytes by the JC polyomavirus (JCV, Padgett and Walker 1973; De Gascun and Carr 2013; Wollebo et al. 2015). This virus is ubiquitous, and 10–25 % of healthy individuals have asymptomatic virus release in the urines. JCV can persist latently in a variety of cell types, including CD34+ hematopoietic precursor cells and B cells (Monaco et al. 1996; Chalkias et al. 2014). The development of PML requires a context of immunosuppression and JCV rearrangements in the genomic non-coding control region (NCCR), leading to new binding sites for cellular transcription factors and enhanced viral gene expression (Pietropaolo et al. 2015). The neurotropic JCV forms, or PML types, have NCCR deletions, duplications, and rearrangements, with respect to the normal archetype strain. They have been detected also in immunocompetent individuals, in peripheral blood leukocytes, bone marrow, and also in normal brain (Chalkias et al. 2014; White and Khalili 2011; Houff et al. 1988). Bone marrow CD34+ hematopoietic stem cells harbor JCV; their differentiation in CD19+/CD10+ pre-B and mature CD19+ B cells increases virus load (Frohman et al. 2014; Major 2011). In natalizumab-treated patients, pre-B and mature B cells are mobilized from bone marrow to periphery, possibly carrying JCV, which could spread to blood and brain (Chalkias et al. 2014; Chapagain and Nerurkar 2010). JCV-infected monocytes were also found (Chalkias et al. 2014). As of June 2016,Footnote 1 more than 600 cases of natalizumab-associated PML (Dubey et al. 2016) have been reported (including 3 CD cases, Van Assche et al. 2005), with an overall incidence of 3.78/1000 patients (Kornek 2015). Currently, three major risk factors have been identified (Bloomgren et al. 2012): (i) presence of anti-JCV antibodies, (ii) previous immunosuppressant therapy, (iii) natalizumab treatment duration >24 months. In patients with all three risk factors, the chance of developing PML was estimated to be 1 in 44 (Berger and Fox 2016), or 1 in 83 (De Gascun and Carr 2013). To reduce the risk of developing PML under natalizumab therapy, the daily clinical practice evaluates the presence of anti-JCV antibodies to decide for therapy discontinuation (Kornek 2015; White et al. 2016). However, several laboratories indicate that the serologic status it is not ever representative of a prior exposure to JCV and vice versa (Koralnik 2014; Major et al. 2013; Gagne Brosseau et al. 2016), and both viremia and cell-mediated immune response to JCV were detected in seronegative individuals (Viscidi et al. 2011; Perkins et al. 2012).
Natalizumab alters transcriptional expression profiles of blood cells in MS patients, and the majority of altered genes are related to immune response, signal transduction, adhesion and metabolism relevant for T and B lymphocytes (Lindberg et al. 2008). The natalizumab-related regulation of NF-1X and Spi-B transcription factors in blood cells may increase the chance of JCV infection of the CNS (Marshall et al. 2014; Meira et al. 2016).
Since JCV is ubiquitous and PML occurs rarely, multiple barriers must exist to disease development. Several transcription factors were identified, based on their ability to regulate JCV replication (Wollebo et al. 2016). None of them was restricted to glial cells, and their overexpression in non-glial cells failed to induce JCV expression in vitro, suggesting that a combination of ubiquitous negative and inducible positive regulators of viral transcription regulates viral gene expression in glial and non-glial cells (Uleri et al. 2011; Sariyer and Khalili 2011).
The SF2/ASF (splicing factor 2/alternative splicing factor) is an ubiquitous member of the arginine/serine splicing factor family, regulator of alternative splicing, involved in nonsense-mediated mRNA decay, protein translation, and mRNA export (Sinha et al. 2010; Manley and Tacke 1996; Shimoni-Sebag et al. 2013; Zhao et al. 2015).
Recent studies, including ours, found that the SF2/ASF inhibits JCV replication in glial cells, through binding to JCV DNA, within the viral promoter. This blocks the expression of JCV large T antigen (T-Ag), multifunctional protein that directs initiation of viral DNA replication, and the transcriptional switch from early to late gene expression (Uleri et al. 2011; Sariyer and Khalili 2011; Uleri et al. 2013). Conversely, T-Ag promotes JCV expression by suppressing SF2/ASF transcription in glial cells, revealing a molecular interplay between SF2/ASF and T-Ag in JCV control. This suggests a novel mechanism of JCV reactivation in patients at risk of PML (Craigie et al. 2015). Of note, SF2/ASF immune-reactivity was found lower than in normal brain in a post-mortem PML brain (Sariyer and Khalili 2011). SF2/ASF is present in oligodendrocyte nuclear inclusion bodies, which are the pathological hallmark of PML and the sites of JCV replication, and is antagonized by the pur-alpha cellular protein, which is a potent inducer of JCV replication in glial cells (Sariyer et al. 2016a).
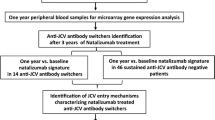
We wondered about a SF2/ASF modulation in the blood of MS patients during natalizumab therapy and if this regulation could influence JCV reactivation in blood. Therefore, we performed a longitudinal study of MS patients under natalizumab, in comparison to patients under fingolimod and to healthy blood donors.
Materials and methods
Study participants
Forty-one MS patients with clinically defined RRMS, consecutively referred to the Centre for MS Diagnosis and Treatment, Department of Clinical and Experimental Medicine, University Hospital of Sassari, Italy were enrolled. Twenty-five patients were under natalizumab treatment and received the standard 300 mg dose every 4 weeks. The remaining 16 patients were under fingolimod therapy, given as next choice after discontinuation of previous therapies, and received daily the standard dose of 0.5 mg orally. After discontinuation of natalizumab, the patients had 3 months of washout, before the treatment with fingolimod. Before initiation of therapies (T0) and after 3 (T3), 6 (T6), 12 (T12), 18 (T18), and 24 (T24) months, peripheral venous blood was collected as well as the clinical data, including expanded disability status scale (EDSS), anti-JCV seropositivity, new MR lesions, side effects, years of disease, previous treatments, etc. The study was approved by the Sassari ASL 1 Ethics Committee, and all participating subjects gave informed consent. In Table 1, the demographic and anamnestic data of the MS patients under study, as well as those of 22 healthy control blood donors (HD) are reported, presenting themselves voluntarily to the Immunohematology and Transfusion Unit, Asl1 Sassari. All patients remained stable during therapy and adverse effects were not reported.
Blood samples
The PBMC were isolated by Ficoll-Hypaque density gradient centrifugation from 20 ml of heparinized blood of enrolled subjects. The cells were divided in three aliquots to be used for: (i) mRNA extraction and evaluation of the SF2/ASF transcripts, (ii) DNA extraction, (iii) flow cytometry. The latter aliquot was suspended in bovine fetal serum, 10 % of dimethyl-sulfoxide and stored alive in liquid nitrogen.
JCV-related methods
The DNA extraction was carried out by the QIAamp DNA Blood Mini Kit (QIAGEN, Hilden, Germany). Real time PCR : In order to detect and to quantify the presence of JCV DNA, 100 ng of each DNA sample was amplified with primers and probe specific for T-Ag sequences (forward primer: 5′-GAGTGTTGGGATCCTGTGTTTT-3′; reverse primer 5′-AGAAGTGGGAT GAAGACCTGTTT-3′; probe 5′-FAM TCATCACTGGCAAA CATTTCTTCATGGC-BHQ-3′(Wittmann et al. 2015). For each sample, the Ct (cycle threshold) values of JCV-T-Ag were compared to the Ct of the glyceraldehyde-3-phosphate dehydrogenase (GAPDH) housekeeping gene (Serra et al. 2008). The data were expressed according to the 2−ΔCt method (Mameli et al. 2013), applying the following formula:
where GI is the gene of interest, and ΔCt = [Ct GI - Ct GAPDH]. Nested PCR: The presence of JCV genomes was investigated by amplifying the NCCR by nested-PCR, with primers as in (Boldorini et al. 1998). Sequencing : PCR amplification products were cloned using TA cloning kit for sequencing (Life Technologies, Eugene, OR), as in (Elsner and Dorries 1998). Ligation products were used to transform competent cells. DNA was extracted from colonies by a miniprep kit (Qiagen, Hilden, Germany). From each sample, ten colonies were sequenced. Anti-JCV antibody index : The anti-JCV antibody serological status and the anti-JCV antibody index were determined by the ELISA (STRATIFY JCV™ DxSelect™) assay (Unilabs-Copenaghen, Denmark), according to the manufacturer’s instructions. An antibody index >0.40 denotes anti-JCV antibody positivity, and an index <0.20 denotes anti-JCV antibody negativity. The 0.9 value is the cutoff between low and high anti-JCV antibody values (Plavina et al. 2014).
SF2/ASF-related methods: mRNA extraction and retro-transcription
The mRNAs were extracted from 50,000 cells, using the Dynabeads® mRNA kit (Dynal Biotech, Oslo, Norway); for each sample, 1 μg was retro-transcribed with the M-MLV retro-transcription kit (Life Technology, Carlsbad, CA, USA). Real-time RT-PCR: The selective amplification of the SF2/ASF mRNA, after retro-transcription into cDNA, was obtained by a real-time PCR (forward primer: 5′- GACATCGACCTCAAGAATCGC-3′; reverse primer: 5′-GACCATACACCGCGTCTTCC-3′; TaqMan probe: 5′-TCCTGTGTGTCTGCACCAGAGGCT-3′). The TaqMan SF2/ASF probe was designed by the Beacon Designer software (PREMIER Biosoft International, Corina Way Palo Alto, CA, USA). To verify the proper mRNA extraction and retro-transcription outcomes, a positive cell sample was submitted in parallel to the extraction and reverse transcription procedures, and the cDNA was amplified in duplicate. An additional positive DNA sample was amplified in duplicate, as a control for the amplification reaction. Parallel RNA samples were also exposed to PCR amplification without the RT step, to detect contaminant DNA. For each sample, the Ct values of SF2/ASF were compared to the Ct of the GAPDH housekeeping gene. The data were expressed according to the 2−ΔCt method (Mameli et al. 2013).
Cells and transfection
The human Namalwa B cell line was cultured in RPMI supplemented with 2 mM l-glutamine, 1.5 g/L sodium bicarbonate, 4.5 g/L glucose, 10 mM HEPES, 1 mM sodium pyruvate, 10 % fetal bovine serum, and antibiotics. Cells were maintained at 37 °C in a humidified atmosphere with 5 % CO2. To be used as a JCV-T-Ag-positive control, Namalwa cells were transiently transfected with an expression plasmid (pcDNA3.1zeo + JCV-Early, kindly provided by K. Khalili, Philadelphia, PA), carrying the JCV early DNA sequence, under the control of the CMV-promoter, or transfected with the empty plasmid (negative control). Transfection was performed with Lipofectamine 3000 (Life Technologies, Carlsbad-CA). Aliquots of 106 cells were transfected with 3 μg of the above plasmids, according to the manufacturer’s instructions. Since Namalwa cells grow in suspension to improve the efficiency of transfection, the incubation with the transfection mixture was carried out in a rotating vessel. After 4 h at 37 °C, cells were washed and cultured for 48 h, then stopped for flow cytometry analysis.
Flow cytometry
The detection of the proteins of interest was performed as described (Mameli et al. 2013). Antibodies: anti-SF2/ASF rabbit polyclonal antibody (Abcam, Cambridge, UK) and secondary FITC-conjugated goat anti-rabbit IgG (Sigma-Aldrich, S. Louis, MO); preimmune rabbit serum (isotype control, Santa Cruz Biotechnology Inc). Anti-T-Ag mAb (Calbiochem, CA, USA) and secondary APC-conjugated goat anti-mouse antibody (Life Technology, Eugene, OR); APC-conjugated IgG1k mouse antibody, as isotype control; PE-conjugated mouse anti-CD19 mAb and PE-IgG1 isotype (BD Biosciences, S. Jose, CA). Stained cells were analyzed in a Flow Cytometer (Accuri, BD), using the C6 Accuri software. The area of positivity was determined using isotype-matched antibodies. A total of 50,000 events for each sample were acquired.
Statistical analyses
Descriptive analyses included the computation of means, standard deviations (SD), and t test or ANOVA, as appropriate, for independent samples for continuous variables. Linear regression tests (Pearson’s test–Spearman’s test) were performed to quantify the strength of the relationship between SF2/ASF and the X variable (JCV seronegativity, JCV DNA positivity, gender, age, disease years, previously therapy). Statistics were performed using SOFA Statistics version 1.4.6 (Paton-Simpson & Associates Ltd., Auckland, New Zealand). Possible misstated outliers were checked and excluded from the survey. To reduce spurious association outcomes, the SF2/ASF RNA data were adjusted for confounders, to have the same range of values and to reach a more robust linear relationship (Kowalski 1972). All SF2/ASF mRNA values were normalized to zero mean and unit variance, according to the following formula:
because of the adjustment, all values are between the −1/+1 interval. Therefore, some of the data of Fig. 4 appear as negative values (Kowalski 1972).
Results
SF2/ASF transcription is up-regulated in the first year of natalizumab therapy
Blood samples from MS patients under natalizumab and under fingolimod were collected at time intervals, during 1 year of therapy, and compared to samples from healthy blood donors (HD). The PBMC were isolated, and their SF2/ASF transcripts were quantified by real-time RT-PCR analysis, as described in Methods. The data of the first year of therapy are reported in Fig. 1 and indicate that the mean levels of SF2/ASF mRNAs were significantly increased in MS patients during the therapy with natalizumab (Fig. 1a). The increase was apparent particularly after 3 and 6 months of therapy and remained elevated in the second semester of therapy, with a strong statistical significance (Time 0, T0, versus T6: p = 0.001; T0 versus T12: p = 0.005, by independent Student’s t test). In the fingolimod cohort, instead, the mean levels of SF2/ASF mRNAs remained unchanged during the year of therapy (Fig. 1b). On the whole, MS patients under fingolimod exhibit lower SF2/ASF levels compared to those under natalizumab. A direct comparison of the data of the two cohorts and its statistical significance at each time point are reported in Fig. 1d. The levels of SF2/ASF expression of HD were intermediate between those of T0 samples of the natalizumab and of the fingolimod cohorts (Fig. 1c).
Levels of SF2/ASF transcripts in PBMC of MS patients treated for 12 months with natalizumab or fingolimod and of healthy donors. a Natalizumab-treated patients (n = 25); the increase over T0 levels is statistically significant, based on two-tailed Student’s t test. b Fingolimod-treated patients ( n = 14). c Healthy donors (HD, n = 22). d Step-wise comparison of SF2/ASF mRNA levels in PBMC of MS patients treated with natalizumab or fingolimod. The statistical significance at each time point between the two MS cohorts was determined by using ANOVA analysis. The data are expressed according to the 2−ΔCt method (Mameli et al. 2013), and reported as box plots. The statistical significance (p) was calculated by the two-tailed Student’s t test
We noticed that the increase of SF2/ASF expression in PBMC of the Natalizumab cohort during time was paralleled by an increased spreading of the individual values (Fig. 1a). To give insights on this finding, the data were stratified by different variables, as gender, age, previous years of MS disease, progression index, and pre-therapy treatments. No statistically significant differences were observed with respect to gender, age, previous MS years, and progression index (data not shown).
In patients pre-treated with interferonβ, the levels of SF2/ASF transcripts correlate inversely with MS years
One of the three recognized PML risk factors for natalizumab-treated patients is the pre-treatment with immunosuppressive drugs (De Gascun and Carr 2013). Therefore, we stratified the values of SF2/ASF transcripts of the T0 samples of all patients, with respect to the previous therapies. A strong statistical significance was found only in those patients that have been treated previously with interferonβ (IFNβ), in which SF2/ASF levels were inversely related to the previous years of MS duration (Fig. 2, Pearson’s R correlation test, R = −0.82, p = 0.007).
Inverse correlation among levels of SF2/ASF transcripts and MS years in patients pre-treated with interferon-β before the first infusion of natalizumab. The T0 SF2/ASF mRNA levels of patients that had received IFNβ were plotted against the previous years of MS duration (n = 9). The statistical significance, calculated by the two-tailed Student’s t test (p) and the Pearson’s correlation test (R), was R = −0.82, p = 0.007. The data are expressed according to the 2−ΔCt method (Mameli et al. 2013)
The increase of SF2/ASF in natalizumab-treated patients is related to the presence of JCV DNA and of anti-JCV antibody
As known, the ascertained scientific evidence related to the risk of Natalizumab-associated PML lies in JCV viremia, presence of JCV antibodies and anti-JCV cell-mediated immunity (Bloomgren et al. 2012). Therefore, DNA was extracted from PBMC of all the MS patients, and exposed to both NCCR-specific nested PCR, and T-Ag-specific real-time PCR.
By nested PCR, the NCCR of JCV was selectively identified in DNA extracts from PBMC of 70 % of the Natalizumab-treated patients,Footnote 2 and three of them became DNA-positive during the therapy. The NCCR amplicons from all the JCV-positive patients were of the expected size. As reported on Fig. 3, the sequencing of NCCR amplicons from T0 and T12 samples of two representative Natalizumab-treated MS patients revealed a PML-associated, Mad-1 NCCR structure, which presents two SF2/ASF-binding sequences, instead of the one of the archetype structure (Uleri et al. 2011), without differences between T0 and T12 samples.
Structure of the NCCR regions amplified from PBMCs of two representative natalizumab-treated MS patients at T0 and T12 of therapy, in comparison to the archetype and Mad-1 JCV strains. The asterisks indicate point mutations. Ori: origin of DNA replication; segment length is given in bp. The arrow indicates the initiation codon for the agnogene. The filled circle indicates the binding site for the SF2/ASF protein. NCBI accession numbers: PML-type JCV NCCR: AF044714; archetype JCV NCCR: AB008765.1. The sequences from the patients matched the PML-type structure
By real-time PCR, all the DNA samples positive for the NCCR, were found positive also for the T-Ag domain. The JCV DNA copies showed an increase after 3 months of therapy, followed by a significant decrease at 12 months (p = 0.001), as reported in Fig. 4, panel d.
SF2/ASF transcription levels of PBMC from natalizumab-treated patients according to JCV DNA and anti-JCV antibody status along 12 months of therapy. a SF2/ASF mean values of JCV DNA+ patients (black rectangle, black line, n = 13–16 patients per time point) compared to JCV DNA patients (grey diamond, gray line, n = 7–10 patients per time point). Plots of the SF2/ASF values of each of the patients of panel (a) are reported in (b) for the JCV DNA patients, and in (c) for the JCV DNA+ patients: a linear correlation is observed only in the JCV DNA+ patients. d Quantification of JCV DNA copies by real-time PCR for the T-Ag gene, in PBMC samples that were found positive by nested PCR for the NCCR region (see the text for details). e, f SF2/ASF transcription values of JCV-antibody-positive samples, stratified according to the JCV antibody index (Ab index <0.9 n = 4 and Ab index >0.9, n = 8). The statistical significance was calculated by the two tailed Student’s t test (p) and the Pearson’s correlation test (R). The data are expressed according to the 2−ΔCt method (Mameli et al. 2013)
Then, the amounts of SF2/ASF mRNAs present in PBMC of MS patients under natalizumab were evaluated by real-time RT PCR and stratified with respect to the presence/absence of JCV DNA sequences. As reported in Fig. 4a–c, the mean values of the two groups were similar in the first trimester of therapy; a different trend of SF2/ASF expression in JCV DNA-negative and JCV DNA-positive individuals started after 6 months and continued in the second semester of therapy. In fact, in JCV DNA-positive individuals, the mean SF2/ASF levels steadily increased up to the 12th month, while in JCV DNA-negative ones the mean SF2/ASF increase started to ease off at the 6th month, and declined thereafter. The SF2/ASF mRNA values have been adjusted for confounders (Kowalski 1972), as explained in Methods; because of the adjustment, some of the data of Fig. 4a–c appear as negative values. The SF2/ASF values of individual samples are reported in Fig. 4b, c (JCV DNA-negative and JCV DNA-positive individuals, respectively). Correlation analyses were performed (χ2 Pearson’s R correlation test), and a statistically significant correlation was observed only in samples from JCV DNA-positive patients (R = 0.62 and p = 0.005; Fig. 4c).
Since the anti-JCV antibody blood levels have been proposed as another predictor of PML-risk (Plavina et al. 2014), natalizumab-treated patients were stratified also according to the anti-JCV antibody index (Figs. 4e–3F). The anti-JCV-positive patients with an anti-JCV antibody index ≤0.9 (Fig. 4d) showed a reduction of SF2/ASF transcripts at T6 and T12, while patients with an anti-JCV antibody index >0.9 showed a constant increase in the transcription of SF2/ASF up to 12 months (p < 0.05).
For 23 of the 25 patients, both JCV DNA and anti-JCV antibody evaluations were available throughout the first 12 months of therapy.Footnote 3 Only two of them were doubly negative (8.7 %), seven were doubly positive (30.4 %), five were Ab-positive/DNA-negative (13.2 %), and eight were Ab-negative/DNA-positive (34.8 %).
In the second year of natalizumab therapy, SF2/ASF expression is downregulated preferentially in CD19+ B cells
During the course of the study, 17 patients completed the second year of therapy (ten subjects under natalizumab and seven under fingolimod); their behavior in the 2 years of therapy was studied and compared to HD. The SF2/ASF mRNA levels were analyzed by real-time RT-PCR. As reported in Fig. 5, the data indicate that in the second year of natalizumab treatment, the levels of SF2/ASF mRNA decrease down to those in the range of T0. The SF2/ASF mRNA levels of fingolimod-treated patients showed a modest increase.
Levels of SF2/ASF transcripts in PBMC from natalizumab-treated and fingolimod-treated MS patients along 2 years of therapy. Ten patients of the natalizumab cohort (filled circle) and seven patients of the fingolimod cohort (filled triangle) were analyzed by real-time RT-PCR. A bell-shaped SF2/ASF regulation is observed only in natalizumab-treated patients. The data are expressed according to the 2−ΔCt method (Mameli et al. 2013). The statistical significance was calculated by the two-tailed Student’s t test (p)
Several studies reported the presence of JCV DNA in bone marrow CD34+ lymphocyte precursors (Chalkias et al. 2014; Monaco and Major 2015; Frohman et al. 2014; Tan et al. 2009) and in B cells and monocytes from MS patients under Natalizumab therapy (Chalkias et al. 2014). Therefore, to test the hypothesis that SF2/ASF is involved in the control of JCV, by intracellular flow cytometry, we measured SF2/ASF protein levels during time, in total PBMCs and in the B cell subpopulation. Seven patients of each cohort, for which alive PBMC were available throughout the 24 months of treatment, were analyzed, in parallel with seven HD (Fig. 6).
CD19+ B cells and SF2/ASF protein expression in PBMC from HD and MS patients treated with natalizumab or fingolimod for 2 years. Flow cytometry was performed simultaneously on PBMC stored alive (n = 7 for each group) (see Methods for details); 50,000 events for each sample were acquired. a, d, g Percentage of CD19+ B cells in overall PBMC. b, e, h Percentage of SF2/ASF+/CD19+ cells in overall PBMC. c, f, i Percentage of SF2/ASF+ cells in overall PBMC. The statistical significance of the observed differences was calculated by the two-tailed Student’s t test (p)
The percentage of CD19+ B cells of natalizumab patients was slightly higher than that of controls since study entry (12.8 vs 8.6 %) and increased during time (Fig. 6a, d). The natalizumab-treated patients that completed the second year of therapy (Fig. 6d) had a 50 % increase at 12 months of therapy (p < 0.01 versus T0) and a 170 % increase at the end of the second year of therapy (T12: 15.8 % and T24: 21.8 %, p < 0.05 versus T12, p < 0.01 versus T0), in line with published data, including ours (Arru et al. 2014; Koudriavtseva et al. 2014).
At T0 and T12, the percent values of SF2/ASF positivity of B cells from natalizumab-treated patients were higher than those of controls, with a sharp decline of SF2/ASF positivity of B cells at the end of the second year of therapy (controls: 60.8 %; T0: 67.2 %; T12: 78.5 %; T24: 49.5 %, Fig. 6b, e). The above differences in the expression of the SF2/ASF protein were barely detectable in overall PBMC, since the B cell subpopulation is a minority of PBMC, and the SF2/ASF differences in whole PBMC during time were not statistically significant (Fig. 6F). During the follow-up of the patients, the SF2/ASF-positive B cells were approximately 1/5 of overall SF2/ASF-positive PBMC (18.9, 19.0, and 19.8 % at T0, T12, and T24, respectively), with a relative enrichment of SF2/ASF-negative B cells (7.0, 10.3, and 24.2 % of SF2/ASF-negative PBMC at T0, T12, and T24, respectively).
The Fingolimod cohort did not show statistically significant differences during the follow-up (Fig. 6g–i). The patients had reduced levels of circulating B cells during the follow-up (32 % at T24 with respect to T0 values, Fig. 6g). The SF2/ASF positivity of B cells was increased of ~20 %, although the differences did not reach the statistical significance (66.9, 80.2, and 79.3 % at T0, T12, and T24, respectively, Fig. 6h). The SF2/ASF-positive B cells were 8.7, 7.1, and 6.3 % of overall SF2/ASF-positive PBMC at T0, T12 and T24, respectively, with a relative depletion of SF2/ASF-negative B cells (T24 values: 53 % of the T0 values of overall SF2/ASF-negative PBMC).
As expected, also the intensity of anti-SF2/ASF staining fluorescence was decreased in patients treated with natalizumab for 24 months. At T24, the SF2/ASF fluorescence intensity in CD19+ B cells of the natalizumab-treated patients was 3–4-fold lower than that of the same cells at T12, while the SF2/ASF fluorescence intensity in CD19+ B cells of the fingolimod-treated patients; instead, it did not vary significantly (not shown).
Natalizumab therapy increases JCV T-Ag expression mostly in B cells, in which SF2/ASF is downregulated
The capability of JCV to replicate in B cells is a debated issue: production or presence of intact JCV virions in CD34+ cells and B cells has been reported (Atwood et al. 1992; Monaco et al. 1996; Tan et al. 2009; Wei et al. 2000), while other studies reported negative results (Saure et al. 2011; Warnke et al. 2011). Thus, by intracellular flow cytometry, cell samples were analyzed simultaneously for T-Ag and SF2/ASF proteins. Of the seven patients tested, four were positive for T-Ag, both in total PBMC and in B cells, with an increasing trend during the 24 months of therapy. In Fig. 7, the mean values of percent positivity to SF2/ASF and T-Ag stainings, and a dot-plot of a single individual are reported.
Opposite trends of SF2/ASF and T-Ag protein expression in CD19+ B cells from natalizumab-treated patients. a Fold increase of expression of SF2/ASF and T-Ag proteins over the pre-therapy T0 values by flow cytometry of five samples. In whole PBMCs and in the CD19+ B subpopulation. b Dot plots of SF2/ASF and T-Ag protein expression in total PBMCs and CD19+ B subpopulation, in a representative natalizumab-treated patient. c T-Ag protein expression in Namalwa cells, either transfected with the empty plasmid (upper panel, negative control) or transfected with pcDNA3.1Zeo + JCV-Early (lower panel). Light gray: staining with the isotype control antibody; dark gray: staining with the anti-T-Ag antibody. Data are expressed as numbers of events (y-axis) and intensity of fluorescence (x-axis). 50,000 events for each sample were acquired
The differences between the data of T12 and T24 were more apparent in the B cell subpopulation than on whole PBMC (Fig. 7a). At T24, the mean percentage of SF2/ASF-positive B cells was reduced by ~3-fold, with respect to that of T12, even though this could not be appreciated in whole PBMC, where only a 14 % reduction was detected (Fig. 7a, left). In the same cells, a sharp increase of T-Ag expression occurred (~2.5-fold increase in T-Ag+ PBMC, and 5.6-fold in CD19+/T-Ag+ B cells, respectively, from T12 to T24 of therapy (Fig. 7a, right). Moreover, the relative percentage of B cells expressing T-Ag was 1 Log higher than those measured in PBMC (not shown). A dot-plot of cells from a single patient is reported in Fig. 7b. As shown, in PBMC, the percentage of T-Ag-positive B cells was 0.6 % at T12 and 2.5 % at T24. Parallel PBMC samples were processed for DNA extraction and evaluation by nested PCR of DNA sequences specific for JCV-NCCR. The PCR data confirmed the flow cytometry data (not shown). As a positive control for the specificity of the anti-T-Ag antibody, the Namalwa cell line, which is negative for JCV expression, has been transiently transfected with an expression plasmid with/without the JCV-T-Ag sequence. After 48 h, the presence of the T-Ag protein was evaluated, by intracellular flow cytometry, and detected only in cells transfected with the T-Ag-plasmid, as reported in Fig. 7c.
Discussion
Natalizumab is the most effective therapy for MS available over the last 10 years (Craddock and Markovic-Plese 2015; Kornek 2015), but is associated with increased risk of PML, fatal demyelinating disease caused by JCV, estimated to be up to 1:44 (Berger and Fox 2016), or 1:83 (De Gascun and Carr 2013).
Since JCV is ubiquitous, multiple barriers must exist against PML development. We hypothesized that one could be the SF2/ASF regulator of alternative splicing (Manley and Tacke 1996), since it inhibits JCV replication in glial cells, through binding to JCV promoter, and blocking the expression of JCV T-Ag (Uleri et al. 2011; Sariyer and Khalili 2011; Uleri et al. 2013, Craigie et al. 2015).
We wondered about a JCV containment by SF2/ASF in MS patients, that might be altered during Natalizumab therapy, and if SF2/ASF regulation could influence JCV reactivation in the blood. Therefore, we performed a longitudinal study of MS patients under natalizumab, in comparison to patients under Fingolimod and to healthy donors.
This study documents the novel finding of the regulation of SF2/ASF in MS patients under therapy with natalizumab, but not with Fingolimod. The SF2/ASF mRNA levels changed during the natalizumab therapy (Figs. 1 and 5), with a bell-shaped pattern: a sharp rise in the first 6 months (up to levels around three times those of HD, Fig. 1), stability for subsequent 12 months, and a decline thereafter, to levels twice those of HD. In fingolimod-treated patients, instead, the SF2/ASF levels were always in the range of those of HD.
Since SF2/ASF plays a key role in JCV control, its decrease in the second year of natalizumab therapy (Fig. 5) could account for the increased risk of PML associated with a treatment duration longer than 24 months, that is one of the three major risk factors for natalizumab-associated PML: Natalizumab treatment duration >24 months, previous immunosuppressant therapy, presence of anti-JCV antibodies (Bloomgren et al. 2012; Plavina et al. 2014). As for previous use of immunosuppressants (De Gascun and Carr 2013), only one of the patients received an immunosuppressant drug. However, in patients pre-treated with IFNβ, the levels of SF2/ASF transcripts correlated inversely with the years of disease (p = 0.007, Fig. 2), while no correlations were found with other prior therapies. Though IFNβ is not considered an immunosuppressant, de facto it is immunosuppressive, when given for prolonged time intervals, and/or at high doses, as those reached in the site of injection, since IFNβ does not spread out (Capobianchi et al. 2015).
The most relevant link between Natalizumab therapy and PML is JCV, the etiological agent of PML. When SF2/ASF mRNA values of the first year of natalizumab treatment were stratified according to the presence of JCV DNA, in JCV DNA-positive patients, the mean SF2/ASF levels steadily increased up to T12, while in JCV DNA-negative patients the mean SF2/ASF increase started to ease off at T6, and declined thereafter (Fig. 4a–c). Alongside to SF2/ASF increase, in JCV DNA-positive patients, there was a concomitant decrease of circulating JCV DNA copies, which at T12 were below detection limits in 77 % of the patients. These findings suggest that the increased expression of SF2/ASF in blood cells is related to the reactivation of JCV during natalizumab treatment, with a protective role against virus replication. This possibility is reinforced by the finding that SF2/ASF expression increased in a statistical significant manner only in patients with high anti-JCV antibody index (Fig. 4e, f). When both JCV DNA and anti-JCV antibody evaluations were available, 34.8 % of the patients were Ab-negative/DNA-positive, thus confirming previous studies, which reported both viremia and cell-mediated immune response to JCV in seronegative individuals (Viscidi et al. 2011; Perkins et al. 2012).
Altogether, the data provide a strong evidence of specific links between SF2/ASF expression and presence of JCV and of anti-JCV response, during natalizumab treatment. In the patients, JCV and JCV-specific response could trigger indirect mechanisms of SF2/ASF regulation (Sariyer et al. 2016b), or, alternatively, increased degradation of the SF2/ASF protein, that, by feedback mechanism, might activate the transcription of its own gene.
To define the actual effects of natalizumab therapy on the SF2/ASF protein, flow cytometry was performed on PBMC from natalizumab- and fingolimod-treated MS patients, throughout the 2 years of therapy and on HD. We focused on CD19+ B cells, since JCV is detected mainly in CD34+, pre-B and mature B cells (Frohman et al. 2014; Chalkias et al. 2014). Moreover, natalizumab promotes mobilization of hematopoietic stem cells and CD19+ cells from the bone marrow (Frohman et al. 2014). Overall data, as reported in Fig. 6, indicate that, with respect to pre-therapy values and healthy controls, natalizumab-treated MS patients had higher numbers of circulating B cells, which were almost doubled at T24, in line with published data, including ours (Arru et al. 2014; Koudriavtseva et al. 2014).
The SF2/ASF-positive B cells were approximately 1/5 of overall SF2/ASF-positive PBMC during all the follow-up. Conversely, a relative >3-fold enrichment of SF2/ASF-negative B cells was observed at T24, with respect to the SF2/ASF-negative PBMC (T0: 7.0 %, T24: 24.2 %). Therefore, if natalizumab-treated MS patients have circulating JCV, the virus has more chances to find SF2/ASF-negative target cells, and to escape the SF2/ASF control, in keeping with the increased risk of natalizumab-associated PML, after 2 years of therapy (Kornek 2015; Bloomgren et al. 2012; Warnke et al. 2011; Faulkner 2015).
The PBMC samples from the fingolimod cohort did not show statistically significant differences during the follow-up (Fig. 6g–i). The patients had reduced levels of circulating B cells, likely due to the effect of the drug in preventing the egress from lymphoid tissues (Chun and Hartung 2010), in keeping with previous reports (Claes et al. 2014; Chiarini et al. 2015). The SF2/ASF positivity of B cells was found ~20 % increased, with an additional relative depletion of SF2/ASF-negative B cells. These new findings imply that circulating JCV would have more chances of finding SF2/ASF-positive target cells, and to be inhibited by SF2/ASF, in keeping with the nearly absence of PML risk associated with Fingolimod treatment (Monaco and Major 2015; Faulkner 2015; Van Schependom et al. 2015).
The capability of JCV to replicate in B cells is debated (Monaco and Major 2015; Atwood et al. 1992; Wei et al. 2000; Warnke et al. 2011; Van Schependom et al. 2015; Chapagain and Nerurkar 2010; Houff and Berger 2010). It is generally accepted that B cells, either supporting JCV replication, or hosting JCV, carry the virus into the brain, like “Trojan horses”, and that local B cell death results in JCV release, infection of oligodendrocytes and demyelination (Houff and Berger 2010). Therefore, PBMC samples of natalizumab-treated MS patients were analyzed simultaneously by flow cytometry for T-Ag and SF2/ASF proteins (Fig. 7). Of the seven patients tested, four produced the T-Ag protein (a finding never reported previously), both in total PBMCs and in CD19+ B cells, with a sharp increase of T-Ag expression from T12 to T24 (5.6-fold in B cells). In addition, the relative percentage of T-Ag-positive cells was 1 Log higher in the B cell subset than in whole PBMC. The above flow cytometry data were confirmed by PCR evaluation of DNA sequences specific for JCV-NCCR. Concomitant to the T-Ag increase at T24 in natalizumab-treated patients, a mean ~3-fold reduction of SF2/ASF-positive cells was observed, indicating again the negative correlation between SF2/ASF and JCV expression. Even though the presence of T-Ag does not mean necessarily viral replication, the reduction of SF2/ASF might explain the JCV reactivation at the blood level. Conversely, JCV was shown to reduce SF2/ASF expression, through binding to the SF2/ASF promoter (Craigie et al. 2015). The detection of the T-Ag protein in B cells is a finding not reported previously; it confirms that B cells are the most important JCV reservoir in blood cells (Wollebo et al. 2015) and gives further support to the active role of circulating B cells for JCV transport to the brain.
This study presents some novel findings: (a) the evaluation of the JCV inhibitor SF2/ASF in MS patients under therapy with natalizumab or with fingolimod, in a 2-year follow up; (b) the bell-shaped regulation of SF2/ASF levels in MS patients under therapy with natalizumab, increased in the first year of therapy, and reduced in the second one, while slightly changed, if any, by fingolimod; (c) SF2/ASF up-regulation, during the first year, only in natalizumab-treated patients that are JCV DNA-positive, or have high anti-JCV antibody response; (d) inverse correlation between SF2/ASF mRNA levels and the years of disease, in patients previously treated with IFNβ; (e) differential SF2/ASF protein expression by B cells from patients treated with natalizumab or fingolimod, with enrichment, only in natalizumab-treated patients, of the SF2/ASF-negative B cell subset, likely more susceptible to JCV than the SF2/ASF-positive ones; (f) expression of the T-Ag protein of JCV in circulating B cells, inversely related to SF2/ASF protein expression.
We propose that SF2/ASF has a protective role against JCV reactivation in MS patients. The SF2/ASF reduction during the second year of therapy with natalizumab, but not with fingolimod, may help explaining the increased risk of PML after the second year of treatment with natalizumab.
Notes
685 cases (682 MS, 3 CD), as of September 7, 2016 (http://chefarztfrau.de/?page_id=716, accessed October 19, 2016). At the time of writing, three PML cases were reported in Natalizumab-naïve Fingolimod-treated patients, with doubts for diagnosis and/or treatments (Faulkner 2015).
For two patients the JCV DNA could not be evaluated, for scarcity of the samples.
The other two patients were anti-JCV antibody-negative, but the JCV DNA could not be evaluated.
References
Arru G, Leoni S, Pugliatti M, Mei A, Serra C, Delogu LG, Manetti R, Dolei A, Sotgiu S, Mameli G (2014) Natalizumab inhibits the expression of human endogenous retroviruses of the W family in multiple sclerosis patients: a longitudinal cohort study. Mult Scler 20:174–182
Atwood WJ, Amemiya K, Traub R, Harms J, Major EO (1992) Interaction of the human polyomavirus, JCV, with human B-lymphocytes. Virology 190:716–723
Baroncini D, Ghezzi A, Annovazzi PO, Colombo B, Martinelli V, Minonzio G, Moiola L, Rodegher M, Zaffaroni M, Comi G (2016) Natalizumab versus fingolimod in patients with relapsing-remitting multiple sclerosis non-responding to first-line injectable therapies. Mult Scler 22:1315–1326
Berger JR, Fox RJ (2016) Reassessing the risk of natalizumab-associated PML. J Neurovirol 22:533–535
Bloomgren G, Richman S, Hotermans C, Subramanyan M, Goelz S, Natarajan A, Lee S, Plavina T, Scanlon JV, Sandrock A, Bozic C (2012) Risk of Natalizumab-associated progressive multifocal leukoencephalopathy. N Engl J Med 366:1870–1880
Boldorini R, Caldarelli-Stefano R, Monga G, Zocchi M, Mediati M, Tosoni A, Ferrante P (1998) PCR detection of JC virus DNA in the brain tissue of a 9-year-old child with pleomorphic xanthoastrocytoma. J Neurovirol 4:242–245
Capobianchi MR, Uleri E, Caglioti C, Dolei A (2015) Type I IFN family members: similarity, differences and interaction. Cytokine Growth Factor Rev 26:103–111
Chalkias S, Dang X, Bord E, Stein MC, Kinkel RP, Sloane JA, Donnelly M, Ionete C, Houtchens MK, Buckle GJ, Batson S, Koralnik IJ (2014) JC virus reactivation during prolonged Natalizumab monotherapy for multiple sclerosis. Ann Neurol 75:925–934
Chapagain ML, Nerurkar VR (2010) Human polyomavirus JC (JCV) infection of human B lymphocytes: a possible mechanism for JCV transmigration across the blood-brain barrier. J Infect Dis 202:184–191
Chiarini M, Sottini A, Bertoli D, Serana F, Caimi L, Rasia S, Capra R, Imberti L (2015) Newly produced T and B lymphocytes and T-cell receptor repertoire diversity are reduced in peripheral blood of fingolimod-treated multiple sclerosis patients. Mult Scler 21:726–734
Chun J, Hartung HP (2010) Mechanism of action of oral fingolimod in multiple sclerosis. Clin Neuropharmacol 33:91–101
Claes N, Dhaeze T, Fraussen J, Broux B, Van Wijmeersch B, Stinissen P, Hupperts R, Hellings N, Somers V (2014) Compositional changes of B and T cell subtypes during fingolimod treatment in multiple sclerosis patients: a 12-month follow-up study. PLoS One 9:e111115
Craddock J, Markovic-Plese S (2015) Immunomodulatory therapies for relapsing-remitting multiple sclerosis: monoclonal antibodies, currently approved and in testing. Expert Rev Clin Pharmacol 8:283–296
Craigie M, Regan P, Otalora YL, Sariyer IK (2015) Molecular interplay between T-antigen and splicing factor, arginine/serine-rich 1 (SRSF1) controls JC virus gene expression in glial cells. Virol J 12:196
De Gascun CF, Carr MJ (2013) Human polyomavirus reactivation: disease pathogenesis and treatment approaches. Clin Dev Immunol 2013:373579
Dubey D, Cano CA, Stüve O (2016) Update on monitoring and adverse effects of approved second-generation disease-modifying therapies in relapsing forms of multiple sclerosis. Curr Opin Neurol 29:278–285
Elsner C, Dörries K (1998) Human polyomavirus JC control region variants in persistently infected CNS and kidney tissue. J Gen Virol 79:789–799
Faulkner M (2015) Risk of progressive multifocal leukoencephalopathy in patients with multiple sclerosis. Expert Opin Drug Saf 14:1737–1748
Frohman EM, Mc M, Remington G, Ryschkewitsch C, Jensen PN, Johnson K, Perkins M, Liebner J, Greenberg B, Monson N, Frohman TC, Douek D, Major EO (2014) JC virus in CD34+ and Cd19+ cells in patients with multiple sclerosis treated with Natalizumab. JAMA Neurol 71:596–602
Gagne Brosseau MS, Stobbe G, Wundes A (2016) Natalizumab-related PML 2 weeks after negative anti-JCV antibody assay. Neurology 86:484–486
Houff SA, Berger J (2010) The curious incident of the dog in the nighttime: does the absence of virus replication in Epstein-Barr virus-transformed B cells point to an important feature of JC virus biology? J Infect Dis 202:181–183
Houff SA, Major EO, Katz DA, Kufta CV, Sever JL, Pittaluga S, Roberts JR, Gitt J, Saini N, Lux W (1988) Involvement of JC virus-infected mononuclear cells from the bone marrow and spleen in the pathogenesis of progressive multifocal leukoencephalopathy. N Engl J Med 318:301–305
Kappos L, O’Connor PW, Polman CH, Vermersch P, Wiendl H, Pace A, Zhang A, Hotermans C (2013) Clinical effects of Natalizumab on multiple sclerosis appear early in treatment course. J Neurol 260:1388–1395
Koralnik IJ (2014) Finger pointing to JC virus: a tale of two indexes. Ann Neurol 76:789–791
Kornek B (2015) An update on the use of Natalizumab in the treatment of multiple sclerosis: appropriate patient selection and special considerations. Patient Prefer Adherence 9:675–684
Koudriavtseva T, Sbardella E, Trento E, Bordignon V, D’Agosto G, Cordiali-Fei P (2014) Long-term follow-up of peripheral lymphocyte subsets in a cohort of multiple sclerosis patients treated with Natalizumab. Clin Exp Immunol 176:320–326
Kowalski CJ (1972) On the effects of non-normality on the distribution of the sample product-moment correlation coefficient. J R Stat Soc Ser C Appl Stat 1–12
Lindberg RLP, Achtnichts L, Hoffman F, Kuhle J, Kappos L (2008) Natalizumab alters transcriptional expression profiles of blood cell subpopulations of multiple sclerosis patients. J Neuroimmunol 194:153–164
Major EO, Frohman E, Douek D (2013) More on JC viremia in Natalizumab-treated patients with multiple sclerosis. N Engl J Med 369:1280
Major EO (2011) History and current concepts in the pathogenesis of PML. Clev Clin J Med 78(2):S3–S7
Mameli G, Madeddu G, Mei A, Uleri E, Poddighe L, Delogu LG, Maida I, Babudieri S, Serra C, Manetti R, Mura MS, Dolei A (2013) Activation of MSRV-type endogenous retroviruses during infectious mononucleosis and Epstein-Barr virus latency: the missing link with multiple sclerosis? PLoS One 8:e78474
Manley JL, Tacke R (1996) SR proteins and splicing control. Genes Dev 10:1569–1579
Marshall LJ, Ferenczy MW, Daley EL, Jensen PN, Ryschkewitsch CF, Major EO (2014) Lymphocyte gene expression and JC virus noncoding control region sequences are linked with the risk of progressive multifocal leukoencephalopathy. J Virol 88:5177–5183
Meira M, Sievers C, Hoffmann F, Haghikia A, Rasenack M, Décard BF, Kuhle J, Derfuss T, Kappos L, Lindberg RL (2016) Natalizumab-induced POU2AF1/Spi-B upregulation: a possible route for PML development. Neurol Neuroimmunol Neuroinflamm 3:e223
Monaco MC, Atwood WJ, Gravell M, Major EO (1996) JCV infection of hematopoietic progenitor cells, primary B lymphocytes and tonsillar stromal cells: implication for viral latency. J Virol 70:7004–7012
Monaco MC, Major EO (2015) Immune system involvement in the pathogenesis of JC virus induced PML: what is learned from studies of patients with underlying diseases and therapies as risk factors. Front Immunol 6:159
Padgett BL, Walker DL (1973) Prevalence of antibodies in human sera against JC virus, an isolate from a case of progressive multifocal leukoencephalopathy. J Infect Dis 127:467–470
Perkins MR, Ryschkewitsch C, Liebner JC, Monaco MC, Himelfarb D, Ireland S, Roque A, Edward HL, Jensen PN, Remington G, Abraham T, Abraham J, Greenberg B, Kaufman C, LaGanke C, Monson NL, Xu X, Frohman E, Major EO, Douek DC (2012) Changes in JC virus-specific T cell responses during Natalizumab treatment and in Natalizumab-associated progressive multifocal leukoencephalopathy. PLoS Pathog 8:e1003014
Pietropaolo V, Bellizzi A, Anzivino E, Iannetta M, Zingaropoli MA, Rodio DM, Morreale M, Pontecorvo S, Francia A, Vullo V, Palamara AT, Ciardi MR (2015) Human polyomavirus JC replication and non-coding control region analysis in multiple sclerosis patients under Natalizumab treatment. J Neurovirol 21:653–665
Plavina T, Subramanyam M, Bloomgren G, Richman S, Pace A, Lee S, Schlain B, Campagnolo D, Belachew S, Ticho B (2014) Anti-JC virus antibody levels in serum or plasma further define risk of natalizumab-associated progressive multifocal leukoencephalopathy. Ann Neurol 76:802–812
Sariyer IK, Khalili K (2011) Regulation of human neurotropic JC virus replication by alternative splicing factor SF2/ASF in glial cells. PLoS One 6:e14630
Sariyer IK, Sariyer R, Otte J, Gordon J (2016a) Pur-alpha induces JCV gene expression and viral replication by suppressing SRSF1 in glial cells. PLoS One 11:e0156819
Sariyer R, De Simone FI, Gordon J, Sariyer IK (2016b). Immune suppression of JC virus gene expression is mediated by SRSF1. J Neurovirol 22:597–606
Saure C, Warnke C, Zohren F, Schroeder T, Bruns I, Cadeddu RP, Weigelt C, Fischer U, Kobbe G, Hartung HP, Adams O, Kieseier BC, Haas R (2011) Natalizumab and impedance of the homing of CD34+ hematopoietic progenitors. Arch Neurol 68:1428–1431
Serra C, Biolchini A, Mei A, Kotenko S, Dolei A (2008) Type III and I interferons increase HIV uptake and replication in human cells that overexpress CD4, CCR5, and CXCR4. AIDS Res Hum Retrovir 24:173–180
Shimoni-Sebag A, Lebenthal-Loinger I, Zender L, Karni R (2013) RRM1 domain of the splicing oncoprotein SRSF1 is required for MEK1-MAPK-ERK activation and cellular transformation. Carcinogenesis 34:2498–2504
Sinha R, Allemand E, Zhang Z, Karni R, Myers MP, Krainer AR (2010) Arginine methylation controls the subcellular localization and functions of the oncoprotein splicing factor SF2/ASF. Mol Cell Biol 30:2762–2774
Tan CS, Dezube BJ, Bhargava P, Autissier P, Wuthrich C, Miller J, Koralnik IJ (2009) Detection of JC virus DNA and proteins in the bone marrow of HIV-positive and HIV-negative patients: implications for viral latency and neurotropic transformation. J Infect Dis 199:881–888
Uleri E, Beltrami S, Gordon J, Dolei A, Sariyer IK (2011) Extinction of tumor antigen expression by SF2/ASF in JCV-transformed cells. Genes Cancer 2:728–736
Uleri E, Regan P, Dolei A, Sariyer IK (2013) SF2/ASF binding region within JC virus NCCR limits early gene transcription in glial cells. Virol J 10:147
Van Assche G, Van Ranst M, Sciot R, Dubois B, Vermeire S, Noman M, Verbeeck J, Geboes K, Robberecht W, Rutgeerts P (2005) Progressive multifocal leukoencephalopathy after natalizumab therapy for Crohn’s disease. N Engl J Med 353:362–368
Van Schependom J, Gielen J, Laton J, Nagels G (2015) Assessing PML risk under immunotherapy: if all you have is a hammer, everything looks like a nail. Mult Scler 22:389–392
Viscidi RP, Khanna N, Tan CS, Li X, Jacobson L, Clifford DB, Nath A, Margolick JB, Shah KV, Hirsch HH, Koralnik IJ (2011) JC virus antibody and viremia as predictors of progressive multifocal leukoencephalopathy in human immunodeficiency virus-1-infected individuals. Clin Infect Dis 53:711–715
Vitaliti G, Matin N, Tabatabaie O, Di Traglia M, Pavone P, Lubrano R, Falsaperla R (2015) Natalizumab in multiple sclerosis: discontinuation, progressive multifocal leukoencephalopathy and possible use in children. Expert Rev Neurother 15:1321–1341
Warnke C, Smolianov V, Dehmel T, Andrée M, Hengel H, Zohren F, Arendt G, Wiendl H, Haas R, Hartung HP, Adams O, Kieseier BC (2011) CD34+ progenitor cells mobilized by natalizumab are not a relevant reservoir for JC virus. Mult Scler 17:151–156
Wei G, Liu CK, Atwood WJ (2000) JC virus binds to primary human glial cells, tonsillar stromal cells, and B-lymphocytes, but not to T lymphocytes. J Neurovirol 6:127–136
White MK, Khalili K (2011) Pathogenesis of progressive multifocal leukoencephalopathy-revisited. J Infect Dis 203:578–586
White MK, Sariyer IK, Gordon J, Delbue S, Pietropaolo V, Berger JR, Khalili K (2016) Diagnostic assays for polyomavirus JC and progressive multifocal leukoencephalopathy. Rev Med Virol 26:102–114
Wittmann T, Horowitz N, Benyamini N, Henig I, Zuckerman T, Rowe JM, Kra-Oz Z, Szwarcwort Cohen M, Oren I, Avivi I (2015) JC polyomavirus reactivation is common following allogeneic stem cell transplantation and its preemptive detection may prevent lethal complications. Bone Marrow Transplant 50:984–991
Wollebo HS, Cotto B, Adiga R, Langford D, White MK (2016) Expression of signaling molecules in progressive multifocal leukoencephalopathy. Curr HIV Res 14:47–53
Wollebo HS, White MK, Gordon J, Berger JR, Khalili K (2015) Persistence and pathogenesis of the neurotropic polyomavirus JC. Ann Neurol 77:560–570
Zhao Y, Zhu T, Zhang X, Wang Q, Zhang J, Ji W, Ma Y (2015) Splicing factor 2/alternative splicing factor contributes to extracellular signal-regulated kinase activation in hepatocellular carcinoma cells. Mol Med Rep 12:3890–3894
Acknowledgments
The authors wish to thank all patients and volunteers whose participation enabled this study, and E. Gomes, Immunohematology & Transfusion Unit, Asl1 Sassari, for providing samples of healthy volunteers. The study was supported in part by grants from CARITRO 2013 and grant CRP-59781, RAS LR-2012. EU was supported by a research fellowship of CARITRO 2013. Author contributions: EU and AD conceived and designed the study. EU, CP, MC, GI performed the experiments. SL and GA provided blood samples and related medical records of MS patients. AD, EU, GI analyzed the data. EU and GI performed the statistical analysis. AD, CS, GPS, SL and GA contributed reagents/materials/analysis tools. AD and EU wrote the manuscript. Potential conflicts of interest: nothing to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uleri, E., Ibba, G., Piu, C. et al. JC polyomavirus expression and bell-shaped regulation of its SF2/ASF suppressor during the follow-up of multiple sclerosis patients treated with natalizumab. J. Neurovirol. 23, 226–238 (2017). https://doi.org/10.1007/s13365-016-0492-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-016-0492-x