Abstract
The glycated albumin (GA) to HbA1c ratio (GA/HbA1c ratio) has been proposed as a marker of postprandial glucose excursion. The aim of this study was to explore the correlation between the GA/HbA1c ratio and beta cell function. Three hundred sixteen subjects with type 2 diabetes who had been admitted to our hospital were examined. Blood samples were obtained after fasting and 2 h after breakfast. Beta cell function was assessed by the serum C-peptide immunoreactivity (CPR) to plasma glucose ratio. Similarly, the correlation between the GA/HbA1c ratio and beta cell function was also estimated in 61 subjects with type 1 diabetes. As a result, the GA/HbA1c ratio was significantly correlated with the postprandial plasma glucose (r = 0.274, p < 0.001) and postprandial increment of plasma glucose (r = 0.269, p < 0.001), but not fasting plasma glucose level (r = 0.081, p = 0.15). Among HbA1c, GA and GA/HbA1c ratio, the GA/HbA1c ratio showed the highest correlation with beta cell function in subjects with type 2 diabetes (r = −0.455, p < 0.001). A robust association between beta cell function and the GA/HbA1c ratio was shown by multiple regression analysis adjusting for confounders. Similar correlations were also observed in subjects with type 1 diabetes. In conclusion, we confirmed a negative association between beta cell function and the GA/HbA1c ratio, a marker of postprandial glucose excursion, in this study using a relatively large sample size. These results indicate that beta cell dysfunction is associated with larger glucose excursions in subjects with both type 1 and type 2 diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes is characterized by beta cell dysfunction and insulin resistance, resulting in chronic hyperglycemia [1]. Chronic hyperglycemia leads to development of diabetic microvascular complications such as retinopathy, nephropathy and neuropathy. In addition, subjects with type 2 diabetes are at risk of development of cardiovascular disease.
Glycated hemoglobin (HbA1c) reflects the mean blood glucose level over 1–2 months and is widely used as a marker of glycemic control [2]. A higher HbA1c has been shown to be associated with diabetic microvascular complications and cardiovascular disease, and lowering the HbA1c level by intensive treatment has been shown to reduce these complications in subjects with both type 1 and type 2 diabetes [3, 4]. However, recent studies aiming at further reduction of HbA1c failed to show any benefit on overall mortality [5–7], raising the possibility that HbA1c may not be the only marker of glycemic control.
Glucose variability, especially postprandial glucose excursion, has also been shown to correlate with oxidative stress [8], atherosclerosis [9] and cardiovascular death [10–12]. In type 1 diabetes, loss of beta cell function has been reported to correlate with greater blood glucose variability [13–15]. In contrast, although recent studies have led to the emergence of the concept that beta cell dysfunction is a central pathophysiological feature of type 2 diabetes [1, 16], the impact of beta cell dysfunction on blood glucose variability in type 2 diabetes remains to be established.
Glycated albumin (GA) is another glycemic index that reflects the mean blood glucose level over a shorter period than does HbA1c [17]. Recently, glycated albumin (GA) or the GA/HbA1c ratio has been proposed as a marker of postprandial glucose excursion [18, 19]. Since postprandial hyperglycemia has been shown to correlate with cardiovascular death [10–12], it is important to explore the factors affecting postprandial glucose excursions. Although a recent study showed a correlation between beta cell function and GA/HbA1c in subjects with type 2 diabetes [20], no report has confirmed this result using a larger sample size. Therefore, in this study, using our cohort with a large sample size and detailed measurements of beta cell function, we investigated the correlation between the GA/HbA1c ratio and beta cell function in subjects with type 1 and type 2 diabetes.
Methods
Subjects
In our retrospective study, we included 316 patients with type 2 diabetes who had been admitted to our hospital between 2000 and 2007 [207 men and 109 women, age 64 ± 13 years (mean ± SD), duration of diabetes 12 ± 10 years, BMI 24.6 ± 4.1 kg/m2; Table 1]. Before admission, 156 subjects (49%) were treated with sulfonylureas, 8 (3%) with glinides, 36 (11%) with biguanides, 38 (12%) with thiazolidinedione, 88 (28%) with α-glucosidase inhibitors and 49 (16%) with insulin. Ninety-six subjects (30%) were receiving no medication. Most patients had been admitted to the hospital because of poor glycemic control, and received basal-bolus insulin therapy using regular and NPH insulin during admission. We excluded subjects in whom GA was not available. We also excluded subjects with renal failure defined as serum creatinine level ≥2 mg/dl [corresponding to glomerular filtration rate (GFR) ≤~30 ml/min/1.73 m2] and subjects with liver cirrhosis. Beta cell function may be transiently impaired by marked hyperglycemia, so-called glucose toxicity. It has been reported that the beta cell response to glucose is blunted above a plasma glucose level of 180 mg/dl [21]. Therefore, subjects with fasting plasma glucose (FPG) levels ≥200 mg/dl on the day of CPR measurement (~15% of our whole cohort) were also excluded. In addition, we also examined 61 subjects with type 1 diabetes who had been admitted to our hospital between 2000 and 2009 (22 men and 39 women, age 51 ± 18 years, duration of diabetes 11 ± 9 years, BMI 22.1 ± 4.1 kg/m2; Table 1). The diagnosis of type 1 and type 2 diabetes was made according to the diagnostic criteria of the Japan Diabetes Society (JDS) [22]. Especially type 1 diabetes was diagnosed with the presence of clinical manifestations such as polyuria, polydipsia, weight loss and ketosis if (1) the patient was positive for at least one of the islet-related autoantibodies [glutamate decarboxylase (GAD) antibody, islet cell antibody, insulinoma-associated antigen-2 (IA-2) antibody and/or insulin autoantibody (IAA)] and/or (2) the patient was in an insulin-dependent state and required insulin therapy within 6 months of the onset of diabetes. Other types of diabetes such as diabetes related to pancreatic disease, mitochondrial diabetes, maturity-onset diabetes of the young (MODY) and drug-induced diabetes were carefully excluded from the diagnosis of type 1 or type 2 diabetes. This study was conducted according to the principles expressed in the Declaration of Helsinki and was approved by the ethics review committee of Keio University School of Medicine, Tokyo, Japan.
Measurements
All measurements were conducted during admission and assayed by the Department of Laboratory Medicine, Keio University School of Medicine. Plasma glucose and serum CPR levels were measured after overnight fasting and 2 h after breakfast during admission, usually within a few days after admission under basal-bolus insulin therapy. All patients received the ideal dietary caloric intake calculated from their ideal body weight [i.e. height (m)2 × 22 × 25 kcal/kg] when blood samples were obtained. Plasma glucose was measured by glucose oxidase method, and CPR was measured by enzyme immunoassay (ST AIA-PACK C-Peptide, TOSOH, Tokyo, Japan). CV of the within-run and between-day precision of CPR was 2.39 and 2.97%, respectively. ΔPG was calculated as: postprandial plasma glucose (PPG, mg/dl) — fasting plasma glucose (FPG, mg/dl). Fasting and postprandial CPR indices were calculated as previously reported [23, 24], i.e., fasting or postprandial serum CPR (ng/ml)/fasting or postprandial plasma glucose (mg/dl) × 100, respectively. Homeostasis model assessment (HOMA2) was also calculated from fasting plasma glucose and CPR values (HOMA2 calculator, http://www.dtu.ox.ac.uk/homacalculator/index.php). In addition, 24 h urinary CPR was also measured within a few days after admission. HbA1c and GA were measured at the time of admission. HbA1c was measured by HPLC and expressed as international standard value, i.e., HbA1c (JDS) + 0.4%, as defined by JDS [22]. GA was measured by enzymatic method. The coefficients of variance (CV) of within-run and between-day precision were 0.4–1.0% and 0.5–0.9% for HbA1c, and 0.9–1.2% and 0.6–0.7% for GA, respectively.
Statistical analysis
Descriptive statistics were calculated for the baseline characteristics. Homogeneity of distributions between the two groups was examined with Mann-Whitney’s U test or Fisher’s exact test. The association between two variables was estimated with Pearson’s correlation coefficient. The difference in two slopes of the CPR index against GA/HbA1c between the type 1 and type 2 diabetes groups was examined with an ANOVA model that contained an interaction term between the CPR index and diabetes type. Multiple regression analysis adjusting for confounders was performed to evaluate the robustness of results. These analyses were performed with the Statistical Package for the Social Sciences (version 17.0; SPSS, Chicago, IL). All data were expressed as mean ± SD, and values of p < 0.05 were considered statistically significant.
Results
Correlation between plasma glucose levels and GA/HbA1c ratio
Correlations among HbA1c, GA, GA/HbA1c and other glycemic indices are shown in Figs. 1 and 2. There were significant positive correlations between GA and HbA1c (r = 0.684, p < 0.001, Fig. 1a) and GA/HbA1c (r = 0.716, p < 0.001, Fig. 1c), but not HbA1c and GA/HbA1c (r = 0.001, p = 0.98, Fig. 1b). GA/HbA1c was significantly positively correlated with postprandial glucose level (r = 0.274, p < 0.001, Fig. 2h) and ΔPG (r = 0.269, p < 0.001, Fig. 2i), but not FPG (r = 0.081, p = 0.15, Fig. 2g). GA also showed stronger correlations with PPG (r = 0.318, p < 0.001, Fig. 2e) and ΔPG (r = 0.284, p < 0.001, Fig. 2f) than with FPG (r = 0.151, p = 0.007, Fig. 2d), while HbA1c showed comparable correlations with PPG (r = 0.170, p = 0.002, Fig. 2b), ΔPG (r = 0.119, p = 0.04, Fig. 2c) and FPG (r = 0.146, p = 0.009, Fig. 2a).
Negative correlation between beta cell function and GA/HbA1c ratio
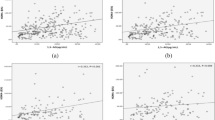
Next we assessed the correlation between beta cell function and GA/HbA1c (Fig. 3). There were significant negative correlations between indices of beta cell function and GA/HbA1c. Both fasting and postprandial CPR indices were more strongly correlated with GA (r = −0.365, p < 0.001 and r = −0.421, p < 0.001, Fig. 3b, e) than with HbA1c (r = −0.109, p = 0.05 and r = −0.134, p = 0.02, Fig. 3a, d), and most strongly correlated with GA/HbA1c (r = −0.410, p < 0.001 and r = −0.455, p < 0.001, Fig. 3c, f). There was also a modest but significant negative correlation between urinary CPR and GA (r = −0.127, p = 0.03) and GA/HbA1c (r = −0.228, p < 0.001), but not HbA1c (r = 0.057, p = 0.31). Significant negative correlations between GA/HbA1c and the postprandial CPR index were consistently observed irrespective of the treatment before admission (r = −0.378, p < 0.001; r = −0.579, p < 0.001; r = −0.428, p = 0.002 for diet only, oral hypoglycemic agents and insulin treatment, respectively). The correlation between GA/HbA1c and postprandial CPR index remained significant after adjustment for sex, age, duration of diabetes, family history of diabetes, BMI, FPG, PPG, creatinine and medication for diabetes (sulfonylureas, biguanides, thiazolidinediones, glinides, α-glucosidase inhibitors and insulin) (β = −0.351, p < 0.001, Table 2). In this analysis, BMI, age and PPG were also significantly associated with GA/HbA1c (Table 2).
Correlations of HbA1c (a), GA (b) and GA/HbA1c ratio (c) with fasting CPR index in subjects with type 2 diabetes. The GA/HbA1c ratio showed the strongest correlation with fasting CPR index compared to HbA1c and GA in subjects with type 2 diabetes. Similar results were observed for postprandial CPR index (d–f)
Beta cell function (HOMA-β%) was also assessed by HOMA2. HOMA-β% was strongly correlated with fasting and postprandial CPR indices (r = 0.858, p < 0.001 and r = 0.639, p < 0.001, respectively). The correlation between HOMA-β% and GA/HbA1c was the strongest (r = −0.379, p < 0.001) compared to those between HOMA-β% and GA (r = −0.316, p < 0.001) and HbA1c (r = −0.155, p = 0.006). Insulin resistance (HOMA-IR) was modestly correlated with GA/HbA1c (r = −0.316, p < 0.001) and GA (r = −0.251, p < 0.001), but not with HbA1c (r = −0.034, p = 0.55).
Comparable relationship between beta cell function and GA/HbA1c ratio in type 1 diabetes
Finally we examined whether the relationship between beta cell function and GA/HbA1c in subjects with type 2 diabetes is comparable to that in subjects with type 1 diabetes. The characteristics of subjects with type 1 diabetes in comparison with subjects with type 2 diabetes are shown in Table 1. Mean HbA1c was comparable, but GA was higher in subjects with type 1 diabetes than in those with type 2 diabetes, resulting in a higher GA/HbA1c ratio in subjects with type 1 diabetes than in those with type 2 diabetes (3.42 ± 0.59 vs. 2.97 ± 0.56, p < 0.001). There were significant negative correlations between beta cell function and HbA1c, GA and GA/HbA1c, with the strongest association between GA/HbA1c and beta cell function in subjects with type 1 diabetes, which was consistent with the findings in those with type 2 diabetes (Fig. 4). Moreover, the relationships between beta cell function and GA/HbA1c were comparable between subjects with type 1 and type 2 diabetes (Fig. 4c, f). It is of note that higher CPR levels were mainly seen in the subjects classified as having slowly progressive type 1 diabetes (SPIDDM). Comparable slopes of the CPR index against GA/HbA1c between subjects with type 1 and type 2 diabetes were confirmed (p = 0.88 and p = 0.90; for interaction between fasting or postprandial CPR index and diabetes type, respectively).
Correlations of HbA1c (a), GA (b) and GA/HbA1c ratio (c) with fasting CPR index in subjects with type 1 diabetes (white circles and solid line) overlaid on subjects with type 2 diabetes (gray circles and dotted line). Similarly to in subjects with type 2 diabetes, the GA/HbA1c ratio showed the strongest correlation with the fasting CPR index compared to HbA1c and GA in subjects with type 1 diabetes. Note that the relationships were comparable in subjects with type 1 and type 2 diabetes. Similar results were observed for postprandial CPR index (d–f)
As an exploratory analysis, multiple regression analysis for GA/HbA1c in the subjects with type 1 diabetes was performed. The model included sex, age, duration of diabetes, BMI, FPG, PPG, creatinine and postprandial CPR index as independent variables. The analysis revealed that the postprandial CPR index (r = −0.396, p < 0.001) as well as BMI (r = −0.225, p < 0.001), age (r = 0.213, p < 0.001), PPG (r = 0.127, p = 0.01) and duration of diabetes (r = −0.114, p = 0.02) was independently correlated with GA/HbA1c.
Discussion
Here, we report that (1) the GA/HbA1c ratio was significantly positively correlated with postprandial glucose excursion but not FPG, (2) there was a significant negative correlation between GA/HbA1c ratio and beta cell function in subjects with type 2 diabetes, and (3) the relationship between the GA/HbA1c ratio in subjects with type 2 diabetes was comparable to that in subjects with type 1 diabetes.
GA and the GA/HbA1c ratio have been reported to be markers of postprandial glucose excursion [18, 19]. We confirmed those previous findings in our study population with a larger sample size. On the other hand, HbA1c has been reported to have a stronger association with the preprandial glucose level than with the postprandial glucose level in subjects with both type 1 and type 2 diabetes in the A1C-Derived Average Glucose (ADAG) study [25]. We also found that HbA1c showed comparable associations with FPG and postprandial glucose levels in our population, which was different from GA and the GA/HbA1c ratio. Thus, based on our results, we can safely conclude that the GA/HbA1c ratio reflects postprandial glucose excursion and is a potential marker of postprandial glucose excursion. The mean HbA1c of the subjects in our study (9.8 ± 1.8%) was much higher than that in previous studies (7–8%) [18, 19]. It has also been reported that the relative contribution of postprandial glucose excursion versus fasting glucose decreases with higher HbA1c [26]. Nonetheless, we showed a significant positive association between postprandial glucose and GA/HbA1c, indicating that the GA/HbA1c ratio reflects postprandial glucose excursion even if the overall glycemic control is poor. On the contrary, since the contribution of postprandial glucose excursion to overall hyperglycemia increases in cases with lower HbA1c (≤~7%), the GA/HbA1c ratio may be affected in such cases.
The mechanism by which the GA/HbA1c ratio reflects glucose excursion remains unknown. Albumin has been reported to be more susceptible to glycation than hemoglobin [27]. A shortened life span of erythrocytes in subjects with diabetes and poor glycemic control has also been reported [28]. Other conditions that affect the turnover of erythrocytes or albumin, such as anemia, proteinuria and liver cirrhosis, could also affect the GA/HbA1c ratio. However, patients with renal failure or liver cirrhosis were excluded from this study.
Our study showed that GA itself also reflects glucose excursion. However, the GA level reflects not only glucose excursion, but also hyperglycemia per se. Indeed, GA was significantly correlated with not only postprandial glucose excursion, but also FPG and HbA1c. In contrast, GA/HbA1c was not significantly correlated with either FPG or HbA1c. These results indicate that GA/HbA1c reflects only glucose excursion independently of hyperglycemia per se. Since normally the GA/HbA1c ratio is approximately 3, we conclude that GA/HbA1c rather than GA itself is a useful marker of glucose excursion in clinical settings.
Recently, Koga et al. [20] reported a significant negative correlation between the GA/HbA1c ratio and beta cell function in subjects with type 2 diabetes. Our study confirmed their finding using a larger sample size and precise evaluation of beta cell function by fasting and postprandial CPR indices and urinary CPR measurement. Furthermore, the correlation between beta cell function and GA/HbA1c remained significant after adjustment for other confounders including age, BMI, FPG, postprandial glucose and previous medication. In this analysis, BMI, age and postprandial glucose level were also selected as independent variables. A negative correlation between BMI and GA has been reported [29, 30]. Obesity and aging may also affect the turnover of either erythrocytes or albumin, or both. The significant negative correlation between HOMA-IR and GA/HbA1c in this study may also reflect the effect of obesity on GA/HbA1c. Although medications such as α-glucosidase inhibitors, glinides and rapid-acting insulin analogs affect postprandial glucose excursion, those medications were not selected in our analysis. It would be of interest to examine whether medications that correct postprandial glucose excursion decrease the GA/HbA1c ratio.
Finally, consistent with previous studies [18, 20], our study showed that the GA/HbA1c ratio was higher in subjects with type 1 diabetes than in those with type 2 diabetes, suggesting greater glucose variability in subjects with type 1 diabetes. Furthermore, a comparable relationship between GA/HbA1c and beta cell function in subjects with type 1 and type 2 diabetes was demonstrated in this study. These findings indicate the fundamental importance of beta cell dysfunction in postprandial glucose excursion in both types of diabetes.
Our study limitations are as follows: (1) fasting and postprandial blood samples were obtained during admission, which may not fully reflect postprandial glucose excursion in daily life. In this study, most patients were receiving basal-bolus insulin therapy because of hyperglycemia at the time when postprandial glucose excursion was assessed. Since insulin therapy reduces glucose excursion as well as FPG, we might have underestimated the correlation between GA/HbA1c and postprandial glucose excursion. It is of note, however, that this does not affect our qualitative conclusion. (2) Since we did not examine hemoglobin level or thyroid function in our study population, we cannot completely exclude the possibility of the presence of mild iron deficiency anemia or thyroid dysfunction, which have been reported to affect GA and HbA1c in non-diabetic subjects [31, 32]. (3) Because of the retrospective design of this study, other confounding factors may exist. Prospective studies will be needed to confirm our findings.
In conclusion, we report a significant negative correlation between beta cell function and GA/HbA1c ratio in subjects with both type 1 and type 2 diabetes. Postprandial glucose excursion has been shown to associate with cardiovascular death [11]. Whether a higher GA/HbA1c level is a risk for diabetic complications in patients with diabetes is of interest. Our results indicate that preservation or recovery of beta cell function would be important to control postprandial glucose excursion, independently of HbA1c level, in patients with both type 1 and type 2 diabetes.
Abbreviations
- GA:
-
Glycated albumin
- CPR:
-
C-peptide immunoreactivity
- JDS:
-
Japan Diabetes Society
- GAD:
-
Glutamate decarboxylase
- IA-2:
-
Insulinoma-associated antigen-2
- IAA:
-
Insulin autoantibody
- FPG:
-
Fasting plasma glucose
- GFR:
-
Glomerular filtration rate
- SPIDDM:
-
Slowly progressive type 1 diabetes
References
Rhodes CJ. Type 2 diabetes-a matter of beta-cell life and death? Science. 2005;307:380–4.
Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31:1473–8.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–53.
Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360:129–39.
Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
Monnier L, Mas E, Ginet C, et al. Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA. 2006;295:1681–7.
Esposito K, Ciotola M, Carleo D, et al. Post-meal glucose peaks at home associate with carotid intima-media thickness in type 2 diabetes. J Clin Endocrinol Metab. 2008;93:1345–50.
Tominaga M, Eguchi H, Manaka H, Igarashi K, Kato T, Sekikawa A. Impaired glucose tolerance is a risk factor for cardiovascular disease, but not impaired fasting glucose. The Funagata Diabetes Study. Diabetes Care. 1999;22:920–4.
The DECODE Study Group on behalf of the European Diabetes Epidemiology Group. Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Arch Intern Med. 2001;161:397–405.
Nakagami T. Hyperglycaemia and mortality from all causes and from cardiovascular disease in five populations of Asian origin. Diabetologia. 2004;47:385–94.
Fukuda M, Tanaka A, Tahara Y, et al. Correlation between minimal secretory capacity of pancreatic beta-cells and stability of diabetic control. Diabetes. 1988;37:81–8.
Nakanishi K, Kobayashi T, Inoko H, Tsuji K, Murase T, Kosaka K. Residual beta-cell function and HLA-A24 in IDDM. Markers of glycemic control and subsequent development of diabetic retinopathy. Diabetes. 1995;44:1334–9.
Sassa M, Yamada Y, Hosokawa M, et al. Glycemic instability in type 1 diabetic patients: possible role of ketosis or ketoacidosis at onset of diabetes. Diabetes Res Clin Pract. 2008;81:190–5.
Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52:102–10.
Selvin E, Francis LM, Ballantyne CM, et al. Nontraditional markers of glycemia: associations with microvascular conditions. Diabetes Care. 2011.
Yoshiuchi K, Matsuhisa M, Katakami N, et al. Glycated albumin is a better indicator for glucose excursion than glycated hemoglobin in type 1 and type 2 diabetes. Endocr J. 2008;55:503–7.
Imai T, Oikawa Y, Shimada A. Improved monitoring of the hyperglycemic state in type 1 diabetes patients by use of the glycoalbumin/HbA1c ratio. Rev Diabet Stud. 2007;4:44–8.
Koga M, Murai J, Saito H, Kasayama S. Glycated albumin and glycated hemoglobin are influenced differently by endogenous insulin secretion in patients with type 2 diabetes. Diabetes Care. 2010;33:270–2.
Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–95.
The Commitee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Invest. 2010;1:212–28.
Saisho Y, Kou K, Tanaka K, et al. Postprandial serum C-peptide to plasma glucose ratio as a predictor of subsequent insulin treatment in patients with type 2 diabetes. Endocr J. 2011;58:315–22.
Goto A, Takaichi M, Kishimoto M, et al. Body mass index, fasting plasma glucose levels, and C-peptide levels as predictors of the future insulin use in Japanese type 2 diabetic patients. Endocr J. 2010;57:237–44.
Borg R, Kuenen JC, Carstensen B, et al. Associations between features of glucose exposure and A1C: the A1C-Derived Average Glucose (ADAG) study. Diabetes. 2010;59:1585–90.
Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care. 2003;26:881–5.
Tahara Y, Shima K. Kinetics of HbA1c, glycated albumin, and fructosamine and analysis of their weight functions against preceding plasma glucose level. Diabetes Care. 1995;18:440–7.
Virtue MA, Furne JK, Nuttall FQ, Levitt MD. Relationship between GHb concentration and erythrocyte survival determined from breath carbon monoxide concentration. Diabetes Care. 2004;27:931–5.
Koga M, Matsumoto S, Saito H, Kasayama S. Body mass index negatively influences glycated albumin, but not glycated hemoglobin, in diabetic patients. Endocr J. 2006;53:387–91.
Koga M, Otsuki M, Matsumoto S, Saito H, Mukai M, Kasayama S. Negative association of obesity and its related chronic inflammation with serum glycated albumin but not glycated hemoglobin levels. Clin Chim Acta. 2007;378:48–52.
Koga M, Murai J, Saito H, Matsumoto S, Kasayama S. Effects of thyroid hormone on serum glycated albumin levels: study on non-diabetic subjects. Diabetes Res Clin Pract. 2009;84:163–7.
Kim MK, Kwon HS, Baek KH, et al. Effects of thyroid hormone on A1C and glycated albumin levels in nondiabetic subjects with overt hypothyroidism. Diabetes Care. 2010;33:2546–8.
Acknowledgments
The authors thank Dr. Wendy Gray for editing the manuscript.
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Saisho, Y., Tanaka, K., Abe, T. et al. Glycated albumin to glycated hemoglobin ratio reflects postprandial glucose excursion and relates to beta cell function in both type 1 and type 2 diabetes. Diabetol Int 2, 146–153 (2011). https://doi.org/10.1007/s13340-011-0035-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-011-0035-x