Abstract
MicroRNAs (miRNAs) have been proven to be important oncogenes and tumor suppressors in wide range of cancers, including renal cell carcinoma (RCC). In our study, we evaluated miRNA-429 as potential diagnostic/prognostic biomarker in 172 clear cell RCC patients and as a potential regulator of epithelial-mesenchymal transition (EMT) in vitro. We demonstrated that miR-429 is down-regulated in tumor tissue samples (P < 0.0001) and is significantly associated with cancer metastasis (P < 0.0001), shorter disease-free (P = 0.0105), and overall survival (P = 0.0020). In addition, ectopic expression of miR-429 in 786-0 RCC cells followed by TGF-β treatment led to increase in the levels of E-cadherin expression (P < 0.0001) and suppression of cellular migration (P < 0.0001) in comparison to TGF-β-treated controls. Taken together, our findings suggest that miR-429 may serve as promising diagnostic and prognostic biomarker in RCC patients. We further suggest that miR-429 has a capacity to inhibit loss of E-cadherin in RCC cells undergoing EMT and consequently attenuate their motility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) comprises of various cancer subtypes characterized by different genetic drivers, histological patterns, and clinical outcome resulting in different responses to the therapy [1]. The most common subtype of RCC is clear cell renal cell carcinoma (ccRCC) accounting for approximately 70 % of cases [2]. Due to the lack of sensitive diagnostic markers, high percentage of RCC patients is still diagnosed with metastatic disease [3]. Five years overall survival is reached by 55 % of patients, whereas in metastatic RCC, this percentage decreases rapidly to 10 %. In recent years, short non-coding RNA molecules called microRNAs (miRNAs) have emerged as critical modulators of broad spectrum of cellular biological processes through post-transcriptional regulation of mRNA expression levels mainly by binding to 3′ end of the untranslated mRNA region [4–6]. MiRNAs were also proven to be involved in the epithelial-mesenchymal transition (EMT), the process primarily responsible for metastatic development [7–9]. Members of the miR-200 family (miR-200a, miR-200b, miR-200c, miR-141, miR-429) and miR-205 are among the first described miRNAs participating in the EMT process [10]. Inactivation of these tumor suppressor molecules is considered to be the EMT’s initial step. Loss of miR-200 family members causes up-regulation of expression levels of EMT inducers, ZEB1 and ZEB2, which further regulate expression of EMT-associated genes, such as E-cadherin through double negative feedback loop [11, 12]. Under physiological conditions, E-cadherin plays an important role in adherent junctions between epithelial cells and suppresses tumor cell invasion and metastasis. One of the most prominent features of the EMT process is loss of E-cadherin [13, 14]. Tumor cells lose contact with each other and undergo multiple molecular changes, which can lead to tumor progression and finally development of metastatic disease. In the present study, we sought to determine the expression profiles of miR-429 in ccRCC tumor tissue, adjacent renal parenchyma, and metastases; its association with ccRCC clinico-pathological features; and also the role of miR-429 in tumor cell migration and EMT in renal cell carcinoma lines in vitro.
Methods
Patient samples
One hundred eighty-seven patients diagnosed with ccRCC and surgically treated at the Masaryk Memorial Cancer Institute in Brno (Department of Urologic Oncology) and University Hospital Brno (Department of Urology), Czech Republic, were included in this study. In addition to primary tumor tissue, 45 samples which correspond to non-malignant kidney cortex were obtained during surgery from the same kidney as corresponding tumor tissue and 12 tissue samples were taken from ccRCC metastasis. All samples were frozen immediately after surgical resection in liquid nitrogen and further stored at −80 °C until RNA extraction. Patients did not receive any neo-adjuvant treatment before surgery. All ccRCC patients were of Czech origin and clinically and histologically verified as clear cell type carcinoma. Clinical stages were determined according to the 2011 Union for International Cancer Control TNM classification. All patients included in the study signed informed consent forms and the study was approved by the local Ethical Board at the Masaryk Memorial Cancer Institute and University Hospital Brno. Patient clinical characteristics are summarized in Table 1.
RNA isolation, reverse transcription, and real-time PCR
Total RNA was isolated from frozen tumor tissue samples, adjacent renal parenchyma, and metastases using mirVanaTM miRNA isolation kit (Ambion, TX, USA) and from cell line samples using TRIzol (Life Technologies, CA, USA). The RNA concentrations and purity were measured spectrophotometrically at 260/280 nm using NanoDrop 1000 Spectrophotometer (Thermo Fisher Scientific, DE, USA). Total RNA was reverse-transcribed using TaqMan MicroRNA Reverse Transcription Kit (Applied Biosystems) and High-Capacity Reverse Transcription Kit (Applied Biosystems). The qPCR was performed using TaqMan Universal Master Mix II, no UNG (Applied Biosystems) and TaqMan Gene Expression MasterMix (Applied Biosystems) and QuantStudio 12 K Flex Real-Time PCR System according to manufacturer’s recommendations. The quantification cycle (Cq) data were calculated using the default threshold settings set up at level 0.2. All miRNA and gene expression values were calculated according to the following formula: 2-dCt, and normalized to RNU48 for miRNA analysis and to PPIA for E-cadherin expression analysis. All samples were run in duplicates.
Cell culture and in vitro studies
Renal cell carcinoma cell lines ACHN and 786-0 were obtained from ATCC (CA, USA) and maintained in recommended media supplemented with 10 % fetal bovine serum, 2 mM glutamax, 100 U/ml penicillin G, and 0.1 μg/ml streptomycin. For transfection experiments, Lipofectamine® RNAiMAX reagent (Invitrogen, CA, USA) and 33.3 nM pre-miR-429/negative control #1 (Ambion) were used according to manufacturer’s protocol. To induce EMT, cells were treated with 10 ng/ml of recombinant human transforming growth factor-β (TGF-β) (Applied Biosystems). To study the role of miR-429 in EMT process in vitro, RCC cell lines were plated in 24-well plates 24 h prior to transfection. EMT was induced by TGF-β 1 day after transfection in ACHN (25 × 104 cells/well) and 786-0 (20 × 104 cells/well) cells. To study expression profiles, cells were harvested with Qiazol (Qiagen, Germany) for total RNA isolation 4 days after treatment and levels of miR-429 and E-cadherin were evaluated by RT-qPCR. Values are presented as means of three independent experiments. For scratch assay experiments, cells were transfected with pre-miR-429/negative control #1 (MOCK) and treated with 10 ng/ml of TGF-β 1 day after seeding. Using TS scratch software, differences in cell-free area was evaluated 24 h (ACHN) and 12 h (786-0) after scratch was made.
Data analysis
Differences between subgroups were tested by non-parametric Mann–Whitney U test. Differences between in vitro experiments were evaluated by t test. ROC analysis was performed to identify the optimal miR-429 cutoff value enabling discrimination of patients accordingly to their DFS and OS. Survival analyses were calculated by Kaplan–Meier method using log-rank test. P values less than 0.05 were considered to be statistically significant.
Results
We determined expression levels of miR-429 in 172 tissue samples of ccRCC primary tumors, 45 renal parenchyma tissues, and 12 metastases. We observed significantly lower levels of miR-429 in tumor tissue and metastasis compared to renal parenchyma (P < 0.0001) (Fig. 1a, b). Lower expression of miR-429 was identified also in metastases when compared to primary tumor tissue (P = 0.0391). MiR-429 expression levels negatively correlated with TNM stage (stage I + II versus stage III + IV; P < 0.0001) (Fig. 1b) and Fuhrman grade (grade 1 + 2, grade 3 + 4; P < 0.0001) in ccRCC. Further, we evaluated the association of miR-429 expression and disease-free survival (DFS) and overall survival (OS) in ccRCC patients. Patients with higher expression levels of miR-429 showed significantly longer DFS after radical nephrectomy than patients with lower expression levels of miR-429 (P = 0.0105) (Fig. 1c). Survival analysis also showed that lower levels of miR-429 are associated with shorter OS of ccRCC patients (P = 0.0020) (Fig. 1d).
Analysis of miR-429 expression in tumor and renal parenchyma tissue samples. MiR-429 a Normalized expression levels of miR-429 in paired tumor tissue and renal parenchyma samples. b Comparison of miR-429 expression in renal parenchyma, tumor tissue of the whole cohort, tumor tissue of patients with localized disease (stage I + II), metastatic disease (stage III + IV) and metastasis. Association of miR-429 expression levels with disease-free survival (c) and overall survival (d)
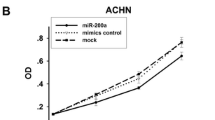
To determine the role of miR-429 in EMT in vitro, E-cadherin expression together with cell migratory capacity was studied in ACHN and 786-0 RCC cell lines by the use of TGF-β treatment to induce EMT and transfection of pre-miR-429 to increase the levels of miR-429. Expression levels of E-cadherin were measured 4 days after transfection and/or treatment. We observed a decrease in E-cadherin levels after TGF-β treatment, which was more prominent in 786-0 cell line (Fig. 2a, b). There was no effect of TGF-β on RCC cells transfected with pre-miR-429 prior to TGF-β treatment indicating capacity of miR-429 to inhibit E-cadherin loss induced by EMT. There was no effect of TGF-β treatment on E-cadherin expression levels in ACHN cells. We observed significant increase of E-cadherin levels in control ACHN cells after transfection with pre-miR-429 (P < 0.01); however, this effect was lost after TGF-β treatment (Fig. 2a). Further, migratory capacity of RCC cells was assessed by scratch wound assay. One day after transfection and treatment, the scratch wound assay was performed and after 12 h (786-0) and 24 h (ACHN), relative migration was evaluated. 786-0 cell line showed significantly increased relative cell migration after treatment with TGF-β in comparison to control cells (P = 0.0011). This potentiation of cell migration induced by TGF-β treatment in 786-0 was not observed in cells transfected with pre-miR-429 prior to treatment (P < 0.0001) (Fig. 2d, f). In ACHN cell line, we did not show any differences in relative cell migration regardless of transfection and/or treatment (Fig. 2c, e). These results indicate the ability of miR-429 to inhibit effects of TGF-β on cell migration in the 786-0 cell line.
MiR-429 involvement in the regulation of E-cadherin and cell motility. Effects of ectopic expression of miR-429 on the levels of E-cadherin in TGF-β treated ACHN (a) and 786–0 (b) RCC cell lines. Scratch migration assay for ACHN (c, e) and 786-O (d, f) was conducted 12 h/24 h after transfection with pre-miR-429. Images of RCC cells are presented as migration under three different conditions: negative control (MOCK), TGF-β treatment, pre-miR-429 + TGF-β treatment (magnification ×40). Data are presented as the mean of three experiments and the bars present the standard deviation (SD) of the mean. ** P < 0.01, **** P < 0.0001
Discussion
Approximately 40 % of all RCC patients with localized disease develops relapse of the disease after radical surgical removal of the tumor. This high rate of recurrence for clinically localized disease after nephrectomy underscores the importance of post-surgical surveillance [15, 16]. In recent years, miRNAs have been described as important regulators of EMT playing roles in metastatic development of RCC, which can also serve as potential biomarkers or therapeutic targets in RCC [17].
In our study, we observed significant decrease in miR-429 expression levels in primary tumors and metastasis of ccRCC patients. In addition, down-regulation of miR-429 was associated with shorter DFS and OS. Our results are in accordance with the number of studies describing down-regulation of miR-429 in tumor tissue of renal cell carcinoma [18] and wide range of other cancers: colorectal carcinoma [19], hepatocellular carcinoma [20], cervical carcinoma [21], nasopharyngeal carcinoma [22], and in non-small lung carcinoma (NSCLC) [23]. Lower serum levels of miR-429 were also associated with poor overall survival of NSCLC patients suggesting its prognostic value in NSCLC [23]. In another study, elevation of miR-429 serum levels in NSCLC patients compared to controls was reported [24].
Recently, miR-429 was described as a potential regulator of E-cadherin restoration during EMT in bladder cancer [25]; however, its effects in EMT in ccRCC are not fully understood. Based on our results, we suggest that miR-429 has a capacity to inhibit loss of E-cadherin expression induced by TGF-β treatment in RCC cells followed by decreased cell migration capacity. Using scratch wound assay, an ability of miR-429 to reverse effects of TGF-β on cell migration in 786-0 cell line derived from non-metastatic RCC was proved.
ACHN is a metastatic RCC cell line, which already underwent EMT, therefore TGF-β treatment had no effect on their phenotype and also transient over-expression of miR-429 in these cells followed with TGF-β treatment does not result in any changes of their migration capacity. Effects of miR-429 and other members of miR-200 family on regulation of E-cadherin expression level during TGF-β-induced EMT were studied in several studies with various results in regard to the cell line used [26, 27]. For instance, down-regulation of E-cadherin was previously reported in ACHN cells after TGF-β treatment, but no changes were observed in cell migration [28]. Contrary to these results, Caki-2 cell line does not prove any E-cadherin expression before/after TGF-β treatment, but TGF-β treatment was followed by significantly higher motility of cells compared to controls. In addition, these changes were followed by significant cell shape alternation after TGF-β treatment [28]. In agreement with our observations, elevated invasiveness and metastatic ability of human 786-0 renal carcinoma cell line after TGF-β treatment were previously studied by Huang et al. [29]. It was suggested that TGF-β induces the expression of Fascin1 and thus improves metastatic potential in 786-0. These observations were reported also in the gastric cancer cells MKN45 [30].
In conclusion, we found out that miR-429 is significantly down-regulated in tumor and metastatic tissue of ccRCC patients compared to adjacent renal parenchyma. In addition, decreased levels of miR-429 were linked to shorter DFS and OS. In vitro experiments showed ability of miR-429 to suppress the cell motility through inhibition of E-cadherin loss induced by TGF-β treatment in non-metastatic 786-0 carcinoma cell line. Our data suggest that miR-429 acts as a tumor suppressor with role in metastatic development, especially through modulation of E-cadherin expression.
References
The Cancer Genome Atlas Research Network. Comprehensive molecular characterization of papillary renal-cell carcinoma. N Engl J Med. 2016;374:135–45.
Ma X, Gao Y, Fan Y, Ni D, Zhang Y, Chen W, et al. Overexpression of E2F1 promotes tumor malignancy and correlates with TNM stages in clear cell renal cell carcinoma. PLoS One. 2013;8:1–12.
KY X, Wu S. Update on the treatment of metastatic clear cell and non-clear cell renal cell carcinoma. Biomark Res. 2015;3:1–5.
Ohtsuka M, Ling H, Doki Y, Mori M, Calin G. MicroRNA processing and human cancer. J Clin Med. 2015;4:1651–67.
Orom UA, Nielsen FC, Lund AH. MicroRNA-10a binds the 5’UTR of ribosomal protein mRNAs and enhances their translation. Mol Cell. 2008;30:460–71.
Xu J, Yao Q, Hou Y, Xu M, Liu S, Yang L, et al. MiR-223/Ect2/p21 signaling regulates osteosarcoma cell cycle progression and proliferation. Biomed Pharmacother = Biomédecine Pharmacothérapie. 2013;67:381–6.
Huang N, Wu Z, Lin L, Zhou M, Wang L, Ma H, et al. MiR-338-3p inhibits epithelial-mesenchymal transition in gastric cancer cells by targeting ZEB2 and MACC1/Met/Akt signaling. Oncotarget. 2015;6:15222–34.
Liu YC, Zhang M, Qian J, Bao M, Meng X, Zhang S, et al. miR-134 functions as a tumor suppressor in cell proliferation and epithelial-to-mesenchymal transition by targeting KRAS in renal cell carcinoma cells. DNA Cell Biol. 2015;34:429–36.
Korpal M, Lee ES, Hu G, Kang Y. The miR-200 family inhibits epithelial-mesenchymal transition and cancer cell migration by direct targeting of E-cadherin transcriptional repressors ZEB1 and ZEB2. J Biol Chem. 2008;283:14910–4.
Zhang Y, Yang P, Wang XF. Microenvironmental regulation of cancer metastasis by miRNAs. Trends Cell Biol. 2014;24:153–60.
Sundararajan BS, Gengenbacher N, Stemmler MP, Kleemann JA, Brabletz T. The ZEB1/miR-200c feedback loop regulates invasion via actin interacting proteins MYLK and TKS5. Oncotarget. 2015;6:27083–96.
Bracken CP, Gregory PA, Kolesnikoff N, Bert AG, Wang J, Shannon MF, Goodall GJ. A double-negative feedback loop between ZEB1-SIP1 and the microRNA-200 family regulates epithelial-mesenchymal transition. Cancer Res. 2008;68:7846–54.
Ceppi P, Mudduluru P, Kumarswamy R, Rapa I, Scagliotti GV, Papotti M, Allgayer H. Loss of miR-200c expression induces an aggressive, invasive, and chemoresistant phenotype in non-small cell lung cancer. Mol Cancer Res. 2010;8:1207–16.
Xiong H, Hong J, Du W, Lin Y, Ren L, Wang Y, et al. Roles of STAT3 and ZEB1 proteins in E-cadherin down-regulation and human colorectal cancer epithelial-mesenchymal transition. J Biol Chem. 2012;287:5819–32.
Paul C. Renal cell carcinoma. Cancer Biomark. 2011;1–6:461–73.
Stewart-Merrill SB, Thompson RH, Boorjian SA, Psutka SP, Lohse CM, Cheville JC, et al. Oncologic surveillance after surgical resection for renal cell carcinoma: a novel risk-based approach. J Clin Oncol. 2015;33:4151–7.
Chan SH, Wang LH. Regulation of cancer metastasis by microRNAs. J Biomed Sci. 2015;22:9.
Yoshino H, Enokida H, Itesako T, Tatarano S, Kinoshita T, Fuse M, et al. Epithelial-mesenchymal transition-related microRNA-200s regulate molecular targets and pathways in renal cell carcinoma. J Hum Genet. 2013;4:1–9.
Sun Y, Shen S, Liu X, Tang H, Wang Z, Yu Z, et al. MiR-429 inhibits cells growth and invasion and regulates EMT-related marker genes by targeting Onecut2 in colorectal carcinoma. Mol Cell Biochem. 2014;390:19–30.
Tang J, Li L, Huang W, Sui C, Yang Y, Lin X, et al. MiR-429 increases the metastatic capability of HCC via regulating classic Wnt pathway rather than epithelial-mesenchymal transition. Cancer Lett. 2015;364:33–43.
Wang Y, Dong X, Hu B, Wang XJ, Wang Q, Wang WL, et al. The effects of Micro-429 on inhibition of cervical cancer cells through targeting ZEB1 and CRKL. Biomed Pharmacother. 2016;80:311–21.
Wang F, Jiang C, Sun Q, Yan F, Wang L, Fu Z, et al. Downregulation of miR-429 and inhibition of cell migration and invasion in nasopharyngeal carcinoma. Mol Med Rep. 2016;13:3236–42.
Zhu Q, He J, Chen D, Zhang B, Xu L, Ma H, et al. Expression of miR-29c, miR-93, and miR-429 as potential biomarkers for detection of early stage non-small lung cancer. PLoS One. 2014;9:2.
Halvorsen AR, Bjaanæs M, LeBlanc M, Holm AM, Bolstad N, Rubio L, et al. A unique set of 6 circulating microRNAs for early detection of non-small cell lung cancer. Oncotarget. 2016.
Wu CL, Ho JY, Chou SC, Yu DS. MiR-429 reverses epithelial-mesenchymal transition by restoring E-cadherin expression in bladder cancer. Oncotarget. 2014.
Chen Y, Xiao Y, Ge W, Zhou K, Wen J, Yan W, et al. miR-200b inhibits TGF-β1-induced epithelial-mesenchymal transition and promotes growth of intestinal epithelial cells. Cell Death Dis. 2013;4:e541.
Wu CL, Ho JY, Chou SC, Yu DS. MiR-429 reverses epithelial-mesenchymal transition by restoring E-cadherin expression in bladder cancer. Oncotarget. 2016.
Jingushi K, Ueda Y, Kitae K, Hase H, Egawa H, Ohshio I, et al. miR-629 targets TRIM33 to promote TGFβ/Smad signaling and metastatic phenotypes in ccRCC. Mo Cancer Res. 2014;13:565–74.
Huang W, Cen S, Kang X, Wang W, Wang Y, Chen X. TGF-β1-induced Fascin1 promotes cell invasion and metastasis of human 786-0 renal carcinoma cells. Acta Histochem. 2016;118:144–51.
Fu H, Hu Z, Wen J, Wang K, Liu Y. TGF-β promotes invasion and metastasis of gastric cancer cells by increasing fascin1 expression via ERK and JNK signal pathways. Acta Biochim Biophys Sin Shanghai. 2009;41:648–56.
Acknowledgment
This study was supported by grant no. 15-34678A of the Czech Ministry of Health, by the Ministry of Education, Youth and Sports of the Czech Republic under the project CEITEC 2020 (LQ1601), the Project RVO (MOU, 00209805), and The Ministry of Education, Youth and Sports for the Project BBMRI CZ (LM2010004).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All patients included in the study signed informed consent forms and the study was approved by the local Ethical Board at the Masaryk Memorial Cancer Institute and University Hospital Brno.
Conflicts of interest
None.
Additional information
Tana Machackova and Hana Mlcochova contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Machackova, T., Mlcochova, H., Stanik, M. et al. MiR-429 is linked to metastasis and poor prognosis in renal cell carcinoma by affecting epithelial-mesenchymal transition. Tumor Biol. 37, 14653–14658 (2016). https://doi.org/10.1007/s13277-016-5310-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-016-5310-9