Abstract
MicroRNA (miR)-92 expression is often aberrant in human cancers. However, its expression in gastric carcinoma and its relation to clinicopathological features and prognosis are unclear.
Tissue microarrays were constructed from 180 patients with gastric cancer (GC), who were undergoing radical resection. MiR-92a expression was detected using miRNA-locked nucleic acid in situ hybridization, and its correlation with clinicopathological features and overall survival was analyzed. MiR-92a expression was decreased in 13.9 % (25/180) of GC, increased in 81.1 % (146/180), and unchanged in 5.0 % (9/180), compared with paracancerous normal tissue (P < 0.001). Univariate analysis showed that high miR-92a expression, tumor stage, tumor status, node status, and tumor size were significant negative prognostic predictors for overall survival in patients with GC (P < 0.001, P < 0.001, P = 0.008, P < 0.001, and P = 0.001, respectively). High miR-92a expression still remained a significant predictor of shorter survival in stage II (n = 56, P = 0.001) and stage III (n = 92, P = 0.009) GC. Multivariate regression analysis demonstrated that tumor status (hazard ratio [HR], 3.10; 95 % confidence interval [CI], 1.51–6.37; P = 0.002), stage (HR, 3.54; 95 % CI, 1.65–7.63; P = 0.000), lymph node metastasis (HR, 2.83; 95 % CI, 1.88–4.28; P = 0.000), high expression of miR-92a (HR, 2.94; 95 % CI, 2.01–4.31; P = 0.000), and tumor size (HR, 2.34; 95 % CI, 1.45–3.79; P = 0.002) predicted shorter OS.
High expression of miR-92a compared with adjacent normal tissues was associated with shorter OS. MiR-92a may thus be useful for evaluating prognosis and may provide a novel treatment target in patients with GC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is currently the fourth most common cancer and the second highest cause of cancer-related mortality worldwide [1]. Gastric carcinogenesis is a multistep and multifactorial process, and identification of the subtypes of GC will provide a roadmap for patient stratification and development of targeted therapies [2, 3]. Studies have shown that different molecular or protein expression profiles in GC may have different prognoses [4]. Four molecular subtypes of GC (tumors positive for Epstein–Barr virus with extreme DNA hypermethylation etc., microsatellite unstable tumors, genomically stable tumors, tumors with chromosomal instability) were recently linked to distinct patterns of molecular alterations, disease progression, and prognosis using gene expression data analysis [2, 3]. However, the precise mechanisms underlying gastric carcinogenesis remain still unclear and biomarker identification of GC prognosis are urgently needed.
MicroRNAs (miRNAs) are small noncoding RNAs regulating gene expression post-transcriptionally by annealing to complementary sequences in the 3′-untranslated region of their target messenger RNA (mRNA). Each miRNA has the potential to target multiple genes and to be involved in different kinds of biological functions like development, proliferation, metabolism, apoptosis, and cell motility [5–7]. More and more evidence suggests that miRNA dysregulation plays an important role in carcinogenesis through targeting oncogene or tumor suppressor gene expression [8, 9]. Various miRNA expression profiles in tissue or serum/plasma of GC point to the potential of miRNAs to be used as diagnostic or prognostic biomarkers [10, 11]. Potential miRNA biomarkers in GC tissue, gastric juice, or plasma have been reported [12–16]. However, it remains unclear whether miRNA signatures are the most reliable for the early detection of GC or for predicting the prognosis of advanced GC [17].
Reportedly, MiR-92a is markedly increased in hepatocellular cancer (HCC) tissues, and its higher expression correlates with significant p21 downregulation. Furthermore, the association has been related to poor survival of these patients [18]. It was reported that the miR-17-92 cluster, miR-19b, miR-20a, and miR-92a, might play a significant role in the development of GC stem cells and that miR-92a expression in 97 patients with GC using real-time PCR has the potential to be used as a predictive prognostic marker [19].
Patients and methods
Patients and tissue samples
Paraffin-embedded tissue samples were collected retrospectively from archival material stored in the Biobank Center at the National Engineering Center for Biochip at Shanghai (Shanghai Outdo Biotech Co. Ltd., Shanghai, China). Tumor tissue and corresponding adjacent normal tissue were collected from 180 patients with histologically diagnosed GC between 2006 and 2008.
The following clinicopathological data were obtained from GC patients, such as age, sex, tumor size, location and invasion, lymph node metastases, grade of differentiation, and tumor stage. Staging of GC was assessed according to the American Joint Committee on Cancer criteria. Written informed consent was obtained from all patients, and the Ethics Committee of the National Engineering Center approved the protocol for Biochip at Shanghai.
Survival time was calculated from the date of surgery to the time of death (or to the date of final follow-up). The last follow-up point was in September 2014, and 17 patients were out of touch in September 2014, but all of them had been lived for 5 years in the previous follow-up. The median follow-up time was 7.1 years (range 6.6–8.1 years). Among the 180 patients, 115 of them died during the follow-up period.
Tissue microarray construction
Tissue microarrays (TMAs) were constructed using appropriate tissue cores from formalin-fixed, paraffin-embedded samples as described previously [20]. Briefly, appropriate tumor areas and corresponding non-tumor gastric samples were selected by pathologists, and a single core (diameter 0.6 mm) was taken from each tissue. TMA blocks were constructed using an automated tissue arrayer (Beecher Instruments, Sun Prairie, WI, USA). Array blocks were cut into 5-μm sections, and sections were stained with hematoxylin and eosin to verify the presence of tumor cells. In all cases, tissue cores obtained from normal adjacent tissue served as internal controls.
miRNA-Locked Nucleic Acid (LNA) in situ hybridization
MiRNA-LNA in situ hybridization was performed using antisense oligonucleotide probes for miR-92a (Exiqon Inc., Woburn, MA, USA) with a Scramble-miR serving as a negative control. In order to inactivate the endogenous alkaline phosphatase activity in tissues, hydrochloric acid treatment was employed before hybridization. Sections were deparaffinized, hydrated, and deproteinized, followed by prehybridization in hybridization buffer for 2 h in a humidified chamber at 55 °C. Hybridization was performed by applying 20 nM of probe in hybridization buffer to the array slides covered with Nescofilm (Bando Chemical Co., Kobe, Japan) overnight at 55 °C in a humidified chamber. Hybridized probes were detected by incubation with anti-digoxigenin–alkaline phosphatase conjugate at 37 °C for 30 min, followed by nitro blue tetrazolium/5-bromo-4-chloro-3-indolyl-phosphate to develop a blue color. Finally, cells were counterstained with nuclear fast red for 3–5 min and mounted on slides. Sections with ≤5 % labeled cells were scored as 0, sections with 5–30 % labeled cells were scored as 1, with 31–70 % labeled cells as 2, and with ≥71 % labeled cells as 3. The staining intensity was scored similarly, with 0 indicating negative staining, 1 weakly positive, 2 moderately positive, and 3 strongly positive. Scores for the percentage of positive tumor cells and staining intensity were summed to generate an immunoreactive score for each specimen. A final score of 0–1 indicated negative expression (−), 2–3 indicated weak expression (+), 4–5 indicated moderate expression (++), and 6 indicated strong expression (+++). Each sample was examined separately and scored by two pathologists [21]. In our study, a high level of miR-92a in GC meant that the final score of miR-92a in GC was higher than that of normal paracancerous tissue. A low level of miR-92a in GC meant that the final score of miR-92a in GC was lower than that of normal paracancerous tissue. An unchanged level of miR-92a in GC meant that the final score of miR-92a in GC was equal to that of normal paracancerous tissue.
Statistical analysis
Associations between clinicopathological parameters and miR-92a expression were evaluated using χ 2 tests. When sample numbers in some categorical cells were less than 5, Fisher’s exact test was employed. Overall survival was calculated and survival curves were plotted using the Kaplan–Meier method; differences between groups were compared using log-rank tests. Significant variables in univariate models were further analyzed using multivariate Cox proportional hazards regression models to identify the independent prognostic values. All analyses were performed using the SPSS software package (SPSS Inc., Chicago, IL, USA, version 17.0). All tests were two-sided and P values <0.05 were considered statistically significant.
Results
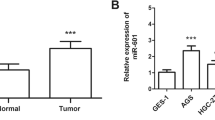
Aberrant expression of miR-92a in GC and paracancerous tissue
It showed that miR-92a was mainly located in the cytoplasm of cells of GC and normal paracancerous tissue in situ hybridization (Fig. 1). MiR-92a expression was decreased in 13.9 % (25/180) of GC, increased in 81.1 % (146/180), and unchanged in 5.0 % (9/180), compared with paracancerous normal tissue (P < 0.001).
MiR-92a levels were stained using in situ hybridization. a MiR-92a staining using in situ hybridization in GC. b MiR-92a staining in adjacent normal tissue; increased miR-92a expression in GC compared with neighboring normal tissue. c MiR-92a staining using in situ hybridization in GC. d MiR-92a staining in adjacent normal tissue; decreased miR-92a expression in GC compared with adjacent normal tissue
Relationships between miR-92a expression and clinicopathological features in GC
There was a tendency towards a difference in local invasion (χ 2 = 3.704, P = 0.054), and TNM stage (χ 2 = 1.477, P = 0.024) between patients with low/unchanged and high expression levels of miR-92a was significant, but no significant correlations between miR-92a expression levels and other clinicopathological variables, including age (χ 2 = 3.704, P = 0.054), gender (P = 0.087), tumor site (P = 0.879), tumor size (P = 0.576), nodal status (χ 2 = 2.783, P = 0.095), or distant metastasis (P = 1.0) (Tables 1 and 2), were found.
Survival analysis
Median overall survival (OS) in the study cohort was 41 months, and the longest was 98 months. Kaplan–Meier analysis showed that high expression of miR-92a, stage of disease, tumor status, node status, tumor size, and distant metastasis were related to significantly shorter OS in patients with GC (P < 0.001, P < 0.001, P = 0.008, P < 0.001, P = 0.001, and P = 0.005, respectively). Other clinicopathological characteristics, including age, sex, and location, were not (P = 0.005, Table 3).
Higher expression of miR-92a (n = 146) remained a significant predictor of shorter mean OS compared with lower/unchanged group (n = 34) (71.9 vs. 91.2 months, P < 0.001) (Fig. 2). After stratification, according to AJCC stage, higher expression of miR-92a remained a significant predictor of poor OS in stage II (30.6 vs. 64.9 months, P < 0.001, n = 56) and stage III GC (29.7 vs. 58.9 months, P < 0.001, n = 92) (Fig. 2).
Survival curves in patients with GC according to miR-92a levels. a Overall survival curves in 180 patients with GC according to miR-92a levels (P < 0.001). b Survival curves of patients with stage II GC according to miR-92a levels (P = 0.001). c Survival curves of patients with stage III GC according to miR-92a levels (P = 0.009)
Univariate Cox regression analysis identified the following predictors of poor prognosis: tumor status (hazard ratio [HR], 3.10; 95 % confidence interval [CI], 1.51–6.37; P = 0.002), stage (HR, 3.54; 95 % CI, 1.65–7.637; P < 0.001), lymph node metastasis (HR, 2.83; 95 % CI, 1.88–4.28; P < 0.001), high miR-92a expression (HR, 2.94; 95 % CI, 2.01–4.31; P < 0.001), and tumor size (HR, 2.34; 95 % CI, 1.45–3.79; P = 0.002). Gender, age, and tumor site were not predictors of poor prognosis (Table 4).
Multivariate Cox regression analysis identified the following predictors of poor prognosis: tumor stage (HR, 2.11; 95 % CI, 1.22–3.66; P = 0.008), miR-92a (HR, 3.34; 95 % CI, 1.67–6.70; P = 0.001), age (HR, 1.65; 95 % CI, 1.09–2.50; P = 0.019), and tumor site (HR, 1.68; 95 % CI, 1.01–2.80; P = 0.044). Gender, tumor status, lymph node metastasis, tumor site, and tumor size were not predictors of poor prognosis (Table 4).
Discussion
miRNAs are aberrant expressions in multiple tumors and play an important role in tumorigenesis and development and may be used as novel biomarkers for the diagnosis and treatment of cancer [11, 22]. To date, a potent cyclin-dependent kinase inhibitor p21 [18], the host gene jing-interacting regulatory protein 1 (jigr1) [23], PTEN [24–26], WD repeat domain-containing 7 (FBXW7) [27], Bim [28], DUSP10 [29], RECK [30], ITGA [31], and CDH1 [32] have been reported as potential targets for miR-92a.
MiR-92a may act as an oncogenic miRNA to promote tumor cell growth, development, and migration [33], such as hepatocellular carcinoma (HCC) [18, 34], cervical cancer [27], colorectal cancer (CRC) [25, 26, 35], pancreatic cancer [29], lung cancer [30], ovarian cancer [31], and esophageal squamous cell carcinoma [32]. Plasma miR-92a/miR-92a-3p was found to be overexpressed in HCC and may be used for early detection of HCC [36, 37]. Urine miR-92a was significantly upregulated in patients with ovarian and endometrial cancers compared with samples from control subjects, and may be used in the diagnosis of ovarian and endometrial cancers [38]. Serum miR-92a was part of an miRNA signature that could be used as a noninvasive biomarker for the diagnosis of colorectal cancer [39] and breast cancer [40]. MiR-92a has been shown to have diagnostic and prognostic value in CRC patients [41–43]. Moreover, detection of miR-92a and miR-21 in stool samples might be potential screening biomarkers for colorectal cancer and polyps [44].
In our previous work, we showed that plasma miR-92a was part of a five-miRNA signature that could be used as a noninvasive biomarker for early diagnosis of GC [11]. MR-92a can be used as a predictive prognostic marker in 97 patients with GC [19]. Nonetheless, some reported that miR-92a inhibited peritoneal dissemination of ovarian cancer cells by targeting integrin α5 expression, which implies that miR-92a has the tumor suppressor gene function [31]. Downregulation of miR-92a is associated with aggressive features in breast cancer patients and promotes tumor macrophage infiltration [45]. However, the mechanistic role of miR-92a as either an oncogene or tumor suppressor in GC remains largely undetermined. In addition, the expression and prognostic value of miR-92a in patients with GC is not well elucidated.
We compared miR-92a expression levels in GC and paracancerous tissues using miRNA-LNA in situ hybridization and found that miR-92a expression was significantly increased in GC tissues overall. However, its expression level was decreased in 13.9 % of samples and unchanged in 5.0 %, suggesting that miR-92a expression may have different prognostic implications in different individuals.
To the best of our knowledge, this study is the first to systematically explore the role of miR-92a in the clinicopathological features and prognosis of GC before surgery. In our previous work, we screened and found an increased circulating miR-92a expression in the early stages of GC [11]. Wu and colleagues found that miR-19b/20a/92a regulates the proliferation of GC stem cells and miR-92a could be used as a prognostic maker in 97 GC patients [19]. However, 2 years of follow-up may be not long enough to evaluate the prognostic value of miR-92a in GC. Moreover, what constituted high expression of miR-92a in normal paracancerous tissues was lacking. Our study included 180 patients with GC and median OS in the study cohort was 41 months, while the longest was 98 months. Moreover, samples were also from different multicenter hospitals.
In this study, GC patients with higher miR-92a expression showed worse prognoses than those with lower or unchanged expression. Moreover, using multivariate Cox regression analysis of potential prognostic factors for GC survival, we identified a significant relationship between high-level expression of miR-92 and poor prognosis (P = 0.001), while in univariate Cox regression analysis, miR-92 expression and poor prognosis were also significant (P < 0.001). As expected, the results for miR-92 expression in plasma and GC tissues were consistent. In our previous study, we showed that increased plasma miR-92a might provide a novel biomarker for early diagnosis of GC [11]. Therefore, increased circulating miR-92a in the plasma may originate primarily from gastric tumor cells. In this study, we found that miR-92a was often overexpressed in normal paracancerous gastric tissues. Thus, detection of miR-92a in the circulation or tissues may provide new information to help in the early diagnosis and prognostic evaluation of GC. Although the molecular function of miR-92a in GC is largely unknown, miR-92a may have an oncogenic function in GC [19]. But in various types of solid cancers or leukemias, miR-92a may play an oncogenic or tumor-suppressor role, depending on the tumor tissue type.
This study included patients with early GC who underwent surgical resection and patients with advanced GC who were supposed to have adjuvant chemotherapy. Although intervention after surgical resection seemed to be various for each patient and the effectiveness was also different, high expression of miR-92a compared with adjacent normal tissues was associated with a poor prognosis. But many clinical and biological factors may influence OS including miR-92a. For example, the group with a high expression of miR-92a has the tendency of advancing more in the clinical stage of GC even though this result was not statistically significant (Table 2). In tumor biology, factors other than miR-92a in advanced GC (for instance, p53 polymorphism or HER2 expression and so on) could be relevant to the efficacy of chemotherapy and affect the OS [46, 47]. These factors may be regarded as bias which may affect the significance of miR-92a in GC prognosis. So molecular function of miR-92a and more clinical GC samples should be further carried out to validate our finding.
The results of this study indicate that patients with gastric adenocarcinomas that have high expression levels of miR-92a compared with adjacent normal tissues have a relatively poor prognosis, while low/unchanged miR-92a expression is associated with a better prognosis. Although further studies are needed to confirm this work, these results suggest that miR-92a may represent a valuable prognostic indicator, as well as a potential target for the treatment of GC.
MiR-92a expression was found to be heterogeneous in GC tissues and corresponding normal gastric mucosa. Overall, miR-92a expression was found to be upregulated in GC. High expression levels of miR-92a in tumor compared with neighboring normal tissues were associated with a poor OS. MiR-92a may thus be useful for evaluating prognosis and may provide a novel target for the treatment of patients with GC.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Network. CGAR. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513:202–9.
Wadhwa R, Song S, Lee JS, Yao Y, Wei Q, Ajani JA. Gastric cancer—molecular and clinical dimensions. Nat Rev Clin Oncol. 2013;10:643–55.
Chen H, Ren C, Han C, Wang D, Chen Y, Fu D. Expression and prognostic value of miR-486-5p in patients with gastric adenocarcinoma. PLoS One. 2015;10, e0119384.
Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005;120:15–20.
Alvarez-Garcia I, Miska EA. MicroRNA functions in animal development and human disease. Development. 2005;132:4653–62.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–97.
Zhang B, Pan X, Cobb GP, Anderson TA. microRNAs as oncogenes and tumor suppressors. Dev Biol. 2007;302:1–12.
Song S, Ajani JA. The role of microRNAs in cancers of the upper gastrointestinal tract. Nat Rev Gastroenterol Hepatol. 2013;10:109–18.
Ueda T, Volinia S, Okumura H, Shimizu M, Taccioli C, Rossi S, et al. Relation between microRNA expression and progression and prognosis of gastric cancer: a microRNA expression analysis. Lancet Oncol. 2010;11:136–46.
Zhu C, Ren C, Han J, Ding Y, Du J, Dai N, et al. A five-microRNA panel in plasma was identified as potential biomarker for early detection of gastric cancer. Br J Cancer. 2014;110:2291–9.
Zhang X, Cui L, Ye G, Zheng T, Song H, Xia T, et al. Gastric juice microRNA-421 is a new biomarker for screening gastric cancer. Tumour Biol. 2012;33:2349–55.
Yu X, Luo L, Wu Y, Yu X, Liu Y, Yu X, et al. Gastric juice miR-129 as a potential biomarker for screening gastric cancer. Med Oncol. 2013;30:365.
Cui L, Zhang X, Ye G, Zheng T, Song H, Deng H, et al. Gastric juice microRNAs as potential biomarkers for the screening of gastric cancer. Cancer. 2013;119:1618–26.
Kogo R, Mimori K, Tanaka F, Komune S, Mori M. Clinical significance of miR-146a in gastric cancer cases. Clin Cancer Res. 2011;17:4277–84.
Rotkrua P, Shimada S, Mogushi K, Akiyama Y, Tanaka H, Yuasa Y. Circulating microRNAs as biomarkers for early detection of diffuse-type gastric cancer using a mouse model. Br J Cancer. 2013;108:932–40.
Ishimoto T, Baba H, Izumi D, Sugihara H, Kurashige J, Iwatsuki M, et al. Current perspectives towards the identification of key players in gastric cancer microRNA dysregulation. Int J Cancer 2015.
Su X, Wang H, Ge W, Yang M, Hou J, Chen T, et al. An in vivo method to identify microRNA targets not predicted by computation algorithms: p21 targeting by miR-92a in cancer. Cancer Res. 2015;75:2875–85.
Wu Q, Yang Z, Wang F, Hu S, Yang L, Shi Y, et al. MiR-19b/20a/92a regulates the self-renewal and proliferation of gastric cancer stem cells. J Cell Sci. 2013;126:4220–9.
He C, Jiang H, Geng S, Sheng H, Shen X, Zhang X, et al. Expression and prognostic value of c-Myc and Fas (CD95/APO1) in patients with pancreatic cancer. Int J Clin Exp Pathol. 2014;7:742–50.
Zhang CZ, Zhang JX, Zhang AL, Shi ZD, Han L, Jia ZF, et al. MiR-221 and miR-222 target PUMA to induce cell survival in glioblastoma. Mol Cancer. 2010;9:229.
Carthew RW, Sontheimer EJ. Origins and mechanisms of miRNAs and siRNAs. Cell. 2009;136:642–55.
Yuva-Aydemir Y, Xu XL, Aydemir O, Gascon E, Sayin S, Zhou W, et al. Downregulation of the host gene jigr1 by miR-92 is essential for neuroblast self-renewal in Drosophila. PLoS Genet. 2015;11, e1005264.
Zou H, Ding Y, Wang K, Xiong E, Peng W, Du F, et al. MicroRNA-29A/PTEN pathway modulates neurite outgrowth in PC12 cells. Neuroscience. 2015;291:289–300.
Ke TW, Wei PL, Yeh KT, Chen WT, Cheng YW. MiR-92a promotes cell metastasis of colorectal cancer through PTEN-mediated PI3K/AKT pathway. Ann Surg Oncol 2015.
Zhang G, Zhou H, Xiao H, Liu Z, Tian H, Zhou T. MicroRNA-92a functions as an oncogene in colorectal cancer by targeting PTEN. Dig Dis Sci. 2014;59:98–107.
Zhou C, Shen L, Mao L, Wang B, Li Y, Yu H. miR-92a is upregulated in cervical cancer and promotes cell proliferation and invasion by targeting FBXW7. Biochem Biophys Res Commun. 2015;458:63–9.
Lv XB, Zhang X, Deng L, Jiang L, Meng W, Lu Z, et al. MiR-92a mediates AZD6244 induced apoptosis and G1-phase arrest of lymphoma cells by targeting Bim. Cell Biol Int. 2014;38:435–43.
He G, Zhang L, Li Q, Yang L. miR-92a/DUSP10/JNK signalling axis promotes human pancreatic cancer cells proliferation. Biomed Pharmacother. 2014;68:25–30.
Lin HY, Chiang CH, Hung WC. STAT3 upregulates miR-92a to inhibit RECK expression and to promote invasiveness of lung cancer cells. Br J Cancer. 2013;109:731–8.
Ohyagi-Hara C, Sawada K, Kamiura S, Tomita Y, Isobe A, Hashimoto K, et al. miR-92a inhibits peritoneal dissemination of ovarian cancer cells by inhibiting integrin alpha5 expression. Am J Pathol. 2013;182:1876–89.
Chen ZL, Zhao XH, Wang JW, Li BZ, Wang Z, Sun J, et al. microRNA-92a promotes lymph node metastasis of human esophageal squamous cell carcinoma via E-cadherin. J Biol Chem. 2011;286:10725–34.
Li M, Guan X, Sun Y, Mi J, Shu X, Liu F, et al. miR-92a family and their target genes in tumorigenesis and metastasis. Exp Cell Res. 2014;323:1–6.
Shigoka M, Tsuchida A, Matsudo T, Nagakawa Y, Saito H, Suzuki Y, et al. Deregulation of miR-92a expression is implicated in hepatocellular carcinoma development. Pathol Int. 2010;60:351–7.
Yamada N, Nakagawa Y, Tsujimura N, Kumazaki M, Noguchi S, Mori T, et al. Role of intracellular and extracellular microRNA-92a in colorectal cancer. Transl Oncol. 2013;6:482–92.
Wen Y, Han J, Chen J, Dong J, Xia Y, Liu J, et al. Plasma miRNAs as early biomarkers for detecting hepatocellular carcinoma. Int J Cancer. 2015;137:1679–90.
Li LM, Hu ZB, Zhou ZX, Chen X, Liu FY, Zhang JF, et al. Serum microRNA profiles serve as novel biomarkers for HBV infection and diagnosis of HBV-positive hepatocarcinoma. Cancer Res. 2010;70:9798–807.
Zavesky L, Jandakova E, Turyna R, Langmeierova L, Weinberger V, Zaveska Drabkova L, et al. Evaluation of cell-free urine microRNAs expression for the use in diagnosis of ovarian and endometrial cancers. A pilot study. Pathol Oncol Res 2015.
Wang J, Huang SK, Zhao M, Yang M, Zhong JL, Gu YY, et al. Identification of a circulating microRNA signature for colorectal cancer detection. PLoS One. 2014;9, e87451.
Chan M, Liaw CS, Ji SM, Tan HH, Wong CY, Thike AA, et al. Identification of circulating microRNA signatures for breast cancer detection. Clin Cancer Res. 2013;19:4477–87.
Liu GH, Zhou ZG, Chen R, Wang MJ, Zhou B, Li Y, et al. Serum miR-21 and miR-92a as biomarkers in the diagnosis and prognosis of colorectal cancer. Tumour Biol. 2013;34:2175–81.
Faltejskova P, Bocanek O, Sachlova M, Svoboda M, Kiss I, Vyzula R, et al. Circulating miR-17-3p, miR-29a, miR-92a and miR-135b in serum: evidence against their usage as biomarkers in colorectal cancer. Cancer Biomark. 2012;12:199–204.
Huang Z, Huang D, Ni S, Peng Z, Sheng W, Du X. Plasma microRNAs are promising novel biomarkers for early detection of colorectal cancer. Int J Cancer. 2010;127:118–26.
Wu CW, Ng SS, Dong YJ, Ng SC, Leung WW, Lee CW, et al. Detection of miR-92a and miR-21 in stool samples as potential screening biomarkers for colorectal cancer and polyps. Gut. 2012;61:739–45.
Nilsson S, Moller C, Jirstrom K, Lee A, Busch S, Lamb R, et al. Downregulation of miR-92a is associated with aggressive breast cancer features and increased tumour macrophage infiltration. PLoS One. 2012;7, e36051.
Ozen A, Kocak Z, Sipahi T, Oz-Puyan F, Cakina S, Saynak M, et al. The prognostic significance of p21 and Her-2 gene expression and mutation/polymorphism in patients with gastric adenocarcinoma. Med Oncol. 2013;30:357.
Yang C, Ma X, Liu D, Wang Y, Tang R, Zhu Y, et al. Promoter polymorphisms of miR-34b/c are associated with risk of gastric cancer in a Chinese population. Tumour Biol. 2014;35:12545–54.
Acknowledgment
This study was supported by the National Nature Science Foundation of China (81573220), Jiangsu provincial Six Talent Peaks (WSN107), the Foundation of China Postdoctoral Studies (M2013541699), the Foundation of Jiangsu Province Postdoctoral Studies (1302149C), and the Foundation for Yong Scholar in Yangzhou (YZ2014046).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Ren, C., Wang, W., Han, C. et al. Expression and prognostic value of miR-92a in patients with gastric cancer. Tumor Biol. 37, 9483–9491 (2016). https://doi.org/10.1007/s13277-016-4865-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-016-4865-9