Abstract
Biochemical markers play a significant role in the diagnosis of lung cancer. Recent studies have demonstrated a link involving S100 Calcium Binding Proteins (S100A2, S100A6) and non-small cell lung cancer (NSCLC), but the expediency of their serum levels in NSCLC has not been established. In this study, we evaluate the potential of serum S100A2 and S100A6 levels as diagnostic markers for NSCLC. Enzyme-linked immunosorbent assay (ELISA) was performed to detect the levels of S100A2 and S100A6 in 141 NSCLC patients and 150 healthy subjects. Serum levels of the two proteins in patients with NSCLC were higher compared to healthy controls (P = 0.0002 for S100A2 and P < 0.0001 for S100A6). Moreover, the levels of S100A2 and S100A6 were higher in the sera of stage I/II NSCLC patients compared to healthy controls with P = 0.01 and <0.0001, respectively. Receiver operating characteristic (ROC) analysis showed that S100A2 could distinguish NSCLC patients from healthy controls (AUC = 0.646), and S100A6 could also identify NSCLC (AUC = 0.668). Meanwhile, these two proteins showed notable capabilities for distinguishing stage I/II NSCLC from healthy controls (AUC = 0.708 for S100A2 and AUC = 0.702 for S100A6). Our results indicate that serum levels of S100A2 and S100A6 are significantly elevated in early stage NSCLC and may have the potential for NSCLC biomarker. Further studies with large sample population would help validate our findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer at its early stage is mostly asymptomatic and radiologically occult. Screening using sputum cytology and low-dose computed tomography has been used with partial success [1]. Histological confirmation after biopsy serves as the mainstay of lung cancer diagnosis, but majority of patients are not willing to undergo biopsy unless presented with evidence of a high probability of having lung cancer [2, 3]. Non-small cell lung cancer (NSCLC) accounts for 85 % of all lung cancer cases and has a poor outcome, which is primarily due to advanced stage at diagnosis [4, 5]. Even in the USA, although nearly 174,000 cases of NSCLC are diagnosed every year, only 20 % of them undergo surgical resection [6, 7]. Serum biomarker levels are popular investigations in clinical practice, but inadequate sensitivity and/or specificity [8, 9] makes it essential to look for novel biochemical marker.
The S100 protein family is a multifunctional group comprising 25 known human members with common EF-hand calcium-binding motifs [10, 11]. There are reports suggesting their involvement in inflammatory responses [12] and cellular processes like cell-cycle progression, differentiation, cell invasion, and epithelial-mesenchymal transition (EMT) [13, 14]. Several members of S100 proteins were found to have atypical expression in a variety of tumors, including lung cancer [15–18]. S100A2 is an important member of S100 protein family and thought to be a putative tumor suppressor, as early studies showed decreased expression in some cancers [19, 20]. There is research confirming S100A2 over expression in early stage NSCLC, thereby suggesting a link with increased metastasis and dismal prognosis [14, 21, 22]. S100A6, also known as calcyclin, is another member of the S100 family. Increased cytoplasmic S100A6 expression was observed in NSCLC, hepatocellular carcinoma, and acute leukemia [23]. S100A6 has been demonstrated in association with a variety of biological processes, including cell-cycle, intracellular calcium homeostasis and signaling, apoptosis, cytoskeleton rearrangement, and ubiquitinated proteolytic degradation [24, 25]. Therefore, the analysis of serum S100A2/A6 (S100A2 and S100A6) expression may provide us with an important idea in the development of diagnostic biomarkers for lung cancer. In the present study, S100A2/A6 expression levels in the sera of patients with newly diagnosed primary lung cancer and healthy subjects were first examined by enzyme-linked immunosorbent assay (ELISA) and their clinical diagnostic values were assessed.
Materials and methods
Study participants
We recruited 150 newly diagnosed and histologically confirmed cases of primary lung cancer admitted at the department of respiratory and critical care medicine, the first affiliated hospital of Xi’an Jiaotong University. None of them had any other malignancy or undergone chemotherapy and/or radiotherapy. Controls were recruited from healthy unrelated individuals who came to our medical center for routine yearly health check-up. Age and gender matched control subjects were free from malignancy and did not have any family history of tumor.
Our study was approved by the Human Research Committee for Research Involving Human subjects at the first affiliated hospital of Xi’an Jiaotong University. All the participants were informed about the purpose of the study and experimental procedures. We obtained written consent from each participant and used a standardized questionnaire to collect demographic and personal data. Serum sample from each subject was immediately separated from the clotted whole blood by centrifugation at 1500×g for 10 min at 4 °C. After centrifugation, the samples were divided into 100 μL aliquots in cryotubes, stored at −80 °C and then analyzed for S100A2 and S100A6 using ELISA kits (USCN Life Sciences Inc., Hubei, China).
Quantification of serum S100A2/A6 using ELISA
ELISA kits for human S100A2 with catalog number SEC009Hu and ELISA kits for human S100A6 with catalog number SEB769Hu were used. Experimental procedures were performed according to the instruction manual. Serum dilutions for S100A2 and S100A6 were 1:1 and 1:10, respectively. To determine the concentration of S100A2/A6, the absorbance at 450 nm of the plates was read using ELISA reader. A standard curve was constructed by plotting absorbance values versus S100A2 or S100A6 concentrations of calibrators.
For S100A2, the sensitivity is 0.124 ng/mL; assay range is 0.312–20 ng/mL.
For S100A6, the sensitivity is 32 pg/mL; assay range is 78–5000 pg/mL.
Statistical analysis
Statistical analyses were performed using Microsoft Excel and the SPSS 22.0 statistical package. The two groups with normally distributed variables (according to an independent group’s t test) were compared with the others using the Mann–Whitney U test. We used analysis of covariance significance of the mean to evaluate the age variables between the two groups. Chi-square test was used to compare the gender variables in the cases with that in controls. Three group comparisons of normally distributed variables and one-way ANOVA for pair-wise comparisons were performed, and others were evaluated with Kruskal-Wallis one-way or Mann–Whitney U test. Two-tailed P < 0.05 was considered significant. Receiver operating characteristic (ROC) curves was constructed by plotting sensitivity versus 1-specificity for every possible cut-off score and area under the ROC curve (AUC) was calculated. The linear relation between S100A2/A6 and levels of present markers for lung cancer was assessed using Pearson product-moment correlation coefficient.
Results
Population characteristics
We recruited a total of 141 NSCLC patients and 150 healthy controls for this study. Table 1 lists the demographic, pathologic, and clinical details of the study population. The mean age of patients (61.1 years) was not significantly different from the controls (60.6 years) (P > 0.05). Male gender accounted for 78.7 % of the patients and 76 % of the control group, respectively, and the difference was not significant (P > 0.05).
Individual expression
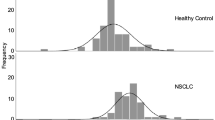
The mean serum S100A2 level in the patients with NSCLC was 15.02 ± 0.79 ng/ml, while the mean level of serum S100A2 in the control group was 11.18 ± 0.64 ng/ml (Table 2). The S100A2 serum levels were significantly higher in NSCLC patients than in healthy controls (P = 0.0002). The mean serum S100A6 level was 12760 ± 651.8 pg/ml in NSCLC patients versus 8434 ± 408.2 pg/ml in controls (P < 0.0001). Tumor staging was based on the International Union against Cancer (UICC) staging system (Table 1). Among the NSCLC patients, 16 (11.3 %) were at stage I, 14 (9.9 %) at stage II, 41 (29.1 %) at stage III, and 65 (46.1 %) at stage IV. As showed in Fig. 1, the serum S100A2 levels were significantly increased in NSCLC patients at both stage I/II (P = 0.01) and stage III/IV (P < 0.001) compared with the control group. Meanwhile, statistically significant differences in S100A6 levels were observed between stage I/II NSCLC patients and controls (P < 0.0001) and between stage III/IV NSCLC and controls (P < 0.0001).
ROC analysis
ROC curve analysis was performed to evaluate the value of S100A2/A6 as potential biomarkers for NSCLC (Fig. 2). The serum levels of S100A2 had an AUC of 0.646 with a specificity of 82 % at a sensitivity of 49.3 % for distinguishing NSCLC from healthy controls (the cut-off of was 13.81 ng/ml). The serum levels of S100A6 resulted in an AUC of 0.668 with a specificity of 64 % at a sensitivity of 61.7 % (the cut-off of was 10152 pg/ml). In differentiating early stage NSCLC from healthy controls, the serum level of S100A2 had an AUC of 0.708 with a specificity of 71.8 % at a sensitivity of 75 % for detecting early stage NSCLC (the cut-off was 12.42 ng/ml), while the serum levels of S100A6 had an AUC of 0.702 with a specificity 99.6 % and a sensitivity 42.9 %, respectively, and the cut-off was 16829 pg/ml.
Correlation of S100A2/A6 with clinical parameters
Table 3 provides the serum S100A2/A6 levels of patients with NSCLC according to the clinicopathologic variables, and the correlation between marker levels and clinical features. S100A2/A6 serum levels did not show significant correlation to age, gender, smoking status, histology, stage, differentiation, and tumor diameter. Linear regression analysis was performed to ensure the correlation of serum S100A2/A6 levels with the present lung cancer biomarkers including carcinoembryonic antigen (CEA), neuron-specific enolase (NSE), and cytokeratin 19 (CYFRA21-1). Serum S100A6 levels positively correlated with CEA levels, Pearson correlation coefficient was 0.212 (P = 0.014) (Fig. 3). S100A6 levels did not correlate with NSE and CYFRA21-1, and S100A2 levels did not correlate with any of the three markers for lung cancer (data not shown).
Discussion
In this study, we focused on the diagnostic and early detection value of the two members of S100 protein family, S100A2 and S100A6, in NSCLC. Our results firstly validate the association between the serum levels of S100A2/A6 and NSCLC and support the hypothesis that the expression of both these proteins is higher in the serum of NSCLC patients.
The S100 protein family comprises 25 known members, each coded by a separate gene and 22 of these genes are clustered at chromosome locus 1q21 [26]. Upon calcium binding, most S100 proteins undergo a conformational change, which allows the protein to interact with various protein targets, thereby exerting a broad range of intracellular and extracellular functions [10]. S100A2 and S100A6, members of the S100 protein family, have been reported to be associated with many types of cancers including lung cancer. A recent study by Naz et al. suggested that S100A2 increased invasion of A549 lung cancer cells by inducing EMT, loose colony morphology in soft agar and enhanced Akt phosphorylation, and modulated TGF-β/Smad-3 mediated transcriptional activity of target genes involved in tumor promotion [14]. Diederichs et al. found S100A2 to be over expressed in early stage NSCLC tissue that metastasized during the course of the disease [22]. A study by Bulk et al. also demonstrated that high mRNA expression levels of S100A2 were associated with poor survival in surgically resected NSCLC patients [21]. In this study, we found S100A2 was increased in the sera of patients with NSCLC and could be used as a promising marker to differentiate NSCLC from healthy subjects. Moreover, the serum levels of S100A2 were increased in patients with early stage NSCLC, which is consistent with the results of previous research in tissues.
S100A6 was initially identified to be up-regulated in acute leukemia and has been related with prognosis and risk of metastasis in several tumor types [27–29]. It has been reported that S100A6 induced EMT and promoted cell migration and invasion in a β-catenin-dependent mannerin pancreatic cancer [30]. S100A6 was demonstrated to interact with p53 and enhance p53 transcriptional activity, consequently facilitating the apoptotic action of p53 [31]. By performing tissue microarrays containing 103 stage I surgically resected NSCLC cases and 14 normal lung parenchyma specimens, Petriset al. found S100A6 was positively expressed in 25 % of early NSCLC cases while S100A6 expression was negative in all components of normal lung tissue [24]. Consistent with these findings, we verified the increased levels of S100A6 in the sera of early NSCLC patients in this study. Our results indicate that S100A6 could be a potential serum biomarker to detect NSCLC. S100A6 could distinguish early stage NSCLC from healthy controls (AUC = 0.702), the marker may be able to assist clinicians in detecting lung cancer at its early stage. Moreover, the present study firstly found that serum S100A6 levels positively correlated with CEA levels, which suggested that the combination of S100A6 and CEA could improve the diagnostic efficiency of lung cancer. Since the positive correlation is very weak and there are very few studies on the relationship of S100A6 and CEA, the exact role it plays and the specific mechanism involved could be better elucidated by further study.
Cumulatively, our results suggest that the levels of S100A2 and S100A6 were increased in the sera of NSCLC patients. Our data also indicate that S100A2/6 is up-regulated during the early phase carcinogenesis of NSCLC, and the levels of serum S100A2/6 may be useful for early detection and screening of NSCLC. The relatively low sensitivities (specificity 82 %, sensitivity 49.3 % for S100A2, and specificity 99.6 % and sensitivity of 42.9 % for S100A6) in our study diminish their clinical significance. Combining S100A2 and S100A6 with commonly used tumor markers in the diagnosis of NSCLC can also increase the sensitivities, which should be evaluated in future study. Experiments using larger patient cohorts could determine whether these two S100 proteins are truly reliable markers and help elucidate the precise biological roles of S100A2 and S100A6 in the development of lung cancer.
References
Yu H, Han Z, Wang Y, Xin H. The clonal evolution and therapeutic approaches of lung cancer. Cell Biochem Biophys. 2014;70:63–71.
Travis WD. Classification of lung cancer. Semin Roentgenol. 2011;46:178–86.
Travis WD, Rekhtman N. Pathological diagnosis and classification of lung cancer in small biopsies and cytology: strategic management of tissue for molecular testing. Semin Respir Crit Care Med. 2011;32:22–31.
Nicholson AG, Gonzalez D, Shah P, Pynegar MJ, Deshmukh M, Rice A, et al. Refining the diagnosis and egfr status of non-small cell lung carcinoma in biopsy and cytologic material, using a panel of mucin staining, ttf-1, cytokeratin 5/6, and p63, and egfr mutation analysis. J Thorac Oncol. 2010;5:436–41.
Travis WD, Brambilla E, Riely GJ. New pathologic classification of lung cancer: relevance for clinical practice and clinical trials. J Clin Oncol. 2013;31:992–1001.
Claiborne PM, Fowler CS, Vaporciyan AA. Follow-up of patients with resected thoracic malignancies. Thorac Surg Clin. 2012;22:123–31.
Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, et al. Cancer statistics, 2004. CA Cancer J Clin. 2004;54:8–29.
Li X, Lu J, Ren H, Chen T, Gao L, Di L, et al. Combining multiple serum biomarkers in tumor diagnosis: a clinical assessment. Mol Clin Oncol. 2013;1:153–60.
Smith RA, Cokkinides V, Brooks D, Saslow D, Shah M, Brawley OW. Cancer screening in the United States, 2011: a review of current american cancer society guidelines and issues in cancer screening. CA cancer J Clin. 2011;61:8–30.
Chen HY, Xu CS, Jin QE, Liu ZH. S100 protein family in human cancer. Am J Cancer Res. 2014;4:89–115.
Stradal TB, Troxler H, Heizmann CW, Gimona M. Mapping the zinc ligands of s100a2 by site-directed mutagenesis. J Biol Chem. 2000;275:13219–27.
Nacken W, Roth J, Sorg C, Kerkhoff C. S100a9/s100a8: Myeloid representatives of the s100 protein family as prominent players in innate immunity. Microsc Res Tech. 2003;60:569–80.
Donato R. Intracellular and extracellular roles of s100 proteins. Microsc Res Tech. 2003;60:540–51.
Naz S, Bashir M, Ranganathan P, Bodapati P, Santosh V, Kondaiah P. Protumorigenic actions of s100a2 involve regulation of pi3/akt signaling and functional interaction with smad3. Carcinogenesis. 2014;35:14–23.
Bartling B, Rehbein G, Schmitt WD, Hofmann HS, Silber RE, Simm A. S100a2-s100p expression profile and diagnosis of non-small cell lung carcinoma: impairment by advanced tumour stages and neoadjuvant chemotherapy. Eur J Cancer. 2007;43:1935–43.
Emberley ED, Murphy LC, Watson PH. S100 proteins and their influence on pro-survival pathways in cancer. Biochem Cell Biol. 2004;82:508–15.
Mishra SK, Siddique HR, Saleem M. S100a4 calcium-binding protein is key player in tumor progression and metastasis: Preclinical and clinical evidence. Cancer Metastasis Rev. 2012;31:163–72.
Salama I, Malone PS, Mihaimeed F, Jones JL. A review of the s100 proteins in cancer. Eur J Surg Oncol. 2008;34:357–64.
Wicki R, Franz C, Scholl FA, Heizmann CW, Schafer BW. Repression of the candidate tumor suppressor gene s100a2 in breast cancer is mediated by site specific hypermethylation. Cell Calcium. 1997;22:243–54.
Wolf S, Haase-Kohn C, Pietzsch J. S100a2 in cancerogenesis: a friend or a foe? Amino Acids. 2011;41:849–61.
Bulk E, Sargin B, Krug U, Hascher A, Jun Y, Knop M, et al. S100a2 induces metastasis in non-small cell lung cancer. Clin Cancer Res. 2009;15:22–9.
Diederichs S, Bulk E, Steffen B, Ji P, Tickenbrock L, Lang K, et al. S100 family members and trypsinogens are predictors of distant metastasis and survival in early-stage non-small cell lung cancer. Cancer Res. 2004;64:5564–9.
Ishii A, Suzuki M, Satomi K, Kobayashi H, Sakashita S, Kano J, et al. Increased cytoplasmic s100a6 expression is associated with pulmonary adenocarcinoma progression. Pathol Int. 2009;59:623–30.
De Petris L, Orre LM, Kanter L, Pernemalm M, Koyi H, Lewensohn R, et al. Tumor expression of s100a6 correlates with survival of patients with stage i non-small-cell lung cancer. Lung Cancer. 2009;63:410–7.
Melle C, Ernst G, Schimmel B, Bleul A, von Eggeling F. Colon-derived liver metastasis, colorectal carcinoma, and hepatocellular carcinoma can be discriminated by the ca(2+)-binding proteins s100a6 and s100a11. PLoS One. 2008;3:e3767.
Mischke D, Korge BP, Marenholz I, Volz A, Ziegler A. Genes encoding structural proteins of epidermal cornification and s100 calcium-binding proteins form a gene complex (“epidermal differentiation complex”) on human chromosome 1q21. J Investig Dermatol. 1996;106:989–92.
Luu HH, Zhou L, Haydon RC, Deyrup AT, Montag AG, Huo D, et al. Increased expression of s100a6 is associated with decreased metastasis and inhibition of cell migration and anchorage independent growth in human osteosarcoma. Cancer Lett. 2005;229:135–48.
McKiernan E, McDermott EW, Evoy D, Crown J, Duffy MJ. The role of s100 genes in breast cancer progression. Tumor Biol. 2011;32:441–50.
Nonaka D, Chiriboga L, Rubin BP. Differential expression of s100 protein subtypes in malignant melanoma, and benign and malignant peripheral nerve sheath tumors. J Cutan Pathol. 2008;35:1014–9.
Ohuchida K, Mizumoto K, Ishikawa N, Fujii K, Konomi H, Nagai E, et al. The role of s100a6 in pancreatic cancer development and its clinical implication as a diagnostic marker and therapeutic target. Clin Cancer Res. 2005;11:7785–93.
Slomnicki LP, Nawrot B, Legniak W. S100a6 binds p53 and affects its activity. Int J Biochem Cell Biol. 2009;41:784–90.
Acknowledgments
This study was supported by National Natural Science Foundation of China (No. 81302029), Natural Science Foundation of Shaanxi Province of China (No. 2014JQ4149), Fundamental Research Funds for the Central Universities in Xi’an Jiaotong University (No. xjj2015086), and China Postdoctoral Science Foundation (No. 2015 M570841).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding authors
Additional information
Ting Wang and Yiqian Liang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, T., Liang, Y., Thakur, A. et al. Diagnostic significance of S100A2 and S100A6 levels in sera of patients with non-small cell lung cancer. Tumor Biol. 37, 2299–2304 (2016). https://doi.org/10.1007/s13277-015-4057-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4057-z