Abstract
The elevation of alkaline phosphatase (ALP) and lactate dehydrogenase (LDH) has been demonstrated to predict worse prognosis in various malignancies; however, their prognostic value in esophageal squamous cell carcinoma has not been well studied. We conducted a retrospective study of 906 patients with esophageal squamous cell carcinoma to explore their prognostic value for overall survival. The optimal cutoff points for ALP and LDH were determined. We analyzed the association between the levels of ALP and LDH and clinicopathological characteristics. Their prognostic value for overall survival was explored by univariate and multivariate analysis. We also proposed the ALP and LDH classification and examined its prognostic value in the general population and subgroups. The optimal cutoff points of ALP and LDH to predict overall survival were 90.7 and 361.5 U/L respectively. Higher levels of ALP and LDH were both associated with more advanced TNM stage (P = 0.003 and 0.002, respectively) and more distant metastasis (P = 0.001 and P < 0.001, respectively). Both ALP (≤90.7/>90.7 U/L) and LDH (≤361.5/>361.5 U/L) were independent prognostic factors for overall survival in esophageal squamous cell carcinoma (P = 0.004 and P < 0.001 by multivariate analysis). The ALP and LDH classification categorized patients into three subgroups with distinct prognosis (P < 0.001 by multivariate analysis) and identified a small group of patients who had extremely poor overall survival with a median of 4.2 months. In conclusion, ALP and LDH were both independent prognostic factors for overall survival. A combination of the two indexes might contribute to further identification of survival differences in esophageal squamous cell carcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer (EC) is one of the most common malignancies across the world. China is an endemic area with a high incidence of EC, which ranked the fourth most frequent newly diagnosed case of cancer and the fourth leading cause of death from cancer in 2008 [1]. There are two main histopathological types, esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC), and the latter is the dominant type in China [2]. The tumor-node-metastasis (TNM) classification system has been widely used for prediction of prognosis [3]. However, even at the same TNM stage, patients may present survival differences. Thus, more accurate evaluation of prognosis is needed in clinical practice.
Some routinely tested serum markers, such as alkaline phosphatase (ALP) and lactate dehydrogenase (LDH), have been demonstrated to have prognostic value in various malignancies. The elevation of ALP was shown to predict worse treatment tolerance, treatment response, progress free survival (PFS), and overall survival (OS) in patients with colorectal cancer receiving palliative chemotherapy of FOLFOX4 [4]. It was also found to be associated with worse prognosis in other cancers, including prostate cancer [5, 6] and nasopharyngeal carcinoma [7]. The prognostic value of LDH in malignancies has been more widely demonstrated. The level of LDH was found to be a prognostic factor in small cell lung cancer [8], metastatic renal cell carcinoma [9], breast cancer [10], nasopharyngeal carcinoma [11], prostate cancer [12], and lymphoma [13]. These serum markers are routinely tested, and they have the superiority of rapid, inexpensive, and convenient application in clinical practice. Thus, their prognostic value is worthy of more investigations and broader applications.
Existing studies about the prognostic value of ALP in ESCC are limited. Chau I et al. found that ALP ≥ 100 U/L was a risk factor for poor prognosis in locally advanced and metastatic esophagogastric cancer [14]. However, most of the cases included in their study were diagnosed with EAC, and only 50 cases were confirmed to be with ESCC. Another study by Kogo M et al. suggested that ALP level could be a predictor for response of ESCC to chemoradiotherapy, but they did not evaluate its prognostic value. Several studies also explored the prognostic value of LDH in ESCC [15–17]. However, they were all small-scaled and the conclusions were contradictory. Thus, we aimed to explore the prognostic value of ALP and LDH in patients with ESCC in this study.
Materials and methods
Ethics statement
All patients provided written informed consent for the information to be used in our hospital database. Study approval was obtained from independent ethics committees at Sun Yat-sen University Cancer Center. This study was conducted in accordance with the ethical standards of the World Medical Association Declaration of Helsinki.
Study population
We retrospectively reviewed the medical records of 1295 patients potentially diagnosed with EC from March 1, 1999 to December 31, 2010 in Sun Yat-sen University Cancer Center in Guangzhou, China. Patients with pathological diagnosis of EAC, esophageal small cell carcinoma, esophageal carcinosarcoma, esophageal leiomyoma, and other non-ESCC tumors were excluded. Only those with ESCC were included in this study. Then, patients missing information for important clinicopathological characteristics, such as the TNM stage and survival status, were further excluded. Finally, there were 906 patients with pathologically confirmed ESCC included in this study.
Data collection
Clinicopathological information and prognostic indexes were retrospectively collected. All the pathological diagnoses were confirmed by pathologists in our department. Morphologically indistinguishable tumors were further distinguished with immunohistochemical indicators. The pathological information was collected from the pathological reports. Some previously confirmed prognostic factors were included in our study to adjust the prognostic effect of ALP and LDH, such as the prognostic nutritional index (PNI; calculated by the formula of 10 × albumin (g/dL) + 0.005 × lymphocyte count/uL), the neutrophil–lymphocyte ratio (NLR), and the platelet–lymphocyte ratio (PLR). The pretreatment information of ALP, LDH, PNI, NLR, and PLR were collected from the test reports. Other information such as age, sex, diagnostic date, the body mass index (BMI; calculated by weight (kg) / height (m)2), and treatment were collected from the medical records.
Treatment and follow-up
The treatment strategies were made according to the National Comprehensive Cancer Network (NCCN) Clinical Practice guidelines. Patients included in this study were at diverse TNM stages from I to IV, along with a long diagnosis time span; therefore, there was a great diversity of treatment modalities in this study. To simplistically analyze the impact of treatment on survival of patients, we categorized all the patients into curative treatment group and palliative treatment group.
Follow-up schedules were also established and applied referring to the NCCN Clinical Practice Guidelines. For those who received curative treatment, the follow-up was scheduled every 3 months for the first 2 years, then every 6 months for another 3 years, and every year thereafter. For those who received palliative treatment, regular treatment and follow-up was conducted at the outpatient department and/or inpatient department. In addition, for those who did not follow the schedule to come back to our hospital, we had a special follow-up department to conduct telephone interviews.
Statistical analysis
We used SPSS 13.0 (SPSS Inc., Chicago, IL, USA) to perform all the statistical analysis. A two tailed P value <0.05 was considered statistically significant. Differences of clinicopathological parameters between groups were evaluated by chi-square test, Mann–Whitney U test or Kruskal–Wallis H test based on the type of data and comparisons. The definition of the OS interval was the duration between the date of diagnosis and the date of death or last contact. The optimal cutoff points for continuous prognostic indexes were determined by the method proposed by Jan Budczies et al. They developed cutoff finder, which was a freely available web application that could translate a continuous variable into a clinical decision by determining an optimal cutoff point. It was implemented based on the R statistical language, and the web application was straightforward to use [18]. The Kaplan–Meier method was used to estimate the survival differences in univariate analysis. Multivariate Cox regression analysis was performed to evaluate the prognostic value of the variables with significant prognostic value identified by univariate analysis.
Results
Patient characteristics
The median age was 58 years old, with a range of 30–88 years old. There were 710 (78.4 %) male patients and 196 (21.6 %) female patients. The majority (804, 88.7 %) of patients were diagnosed with non-metastatic ESCC. The number of patients from stage I to III was 93 (10.3 %), 357 (39.4 %), and 354 (39.1 %), respectively. Only 102 (11.3 %) cases were at stage IV. One hundred one (11.2 %) patients had tumors located in the upper esophagus, while 544 (60.0 %) and 261 (28.8 %) in the middle and lower esophagus, respectively. There were 699 (77.2 %) patients receiving curative treatment, while 207 (22.8 %) patients received treatment for palliative purpose.
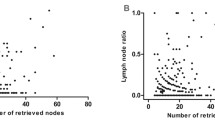
The association between ALP, LDH, and clinicopathological characteristics
The value of ALP ranged from 27.0 to 259.0 U/L, with a median of 69.0 U/L. The value of LDH ranged from 11.0 to 851.0 U/L, with a median of 156.0 U/L. The suggested normal ranges of ALP and LDH were 30–110 and 109–245 U/L, respectively, according to the reagent used to detect the levels of ALP and LDH in our hospital. The optimal cutoff points to distinguish the differences of OS were determined to be 90.7 and 361.5 U/L for ALP and LDH, respectively, by cutoff finder. Using the optimal cutoff points, we categorized all the patients into subgroups to analyze the correlation of the levels of ALP and LDH with the clinicopathological characteristics of patients with ESCC (Table 1). There were 781 (86.2 %) patients with a lower level of ALP (≤90.7 U/L) and 125 (13.8 %) patients with a higher level of ALP (>90.7 U/L). There were 895 (98.8 %) patients with a lower level of LDH (≤361.5 U/L) and 11 (1.2 %) patients with a higher level of ALP (>361.5 U/L). We found that higher levels of both ALP and LDH were related with more advanced TNM stage (P = 0.003 and 0.002, respectively) and more distant metastasis (P = 0.001 and P < 0.00,1 respectively). In addition, a higher level of LDH was also associated with poorer tumor differentiation (P = 0.02). We found no association of the levels of ALP and LDH with other clinicopathological characteristics.
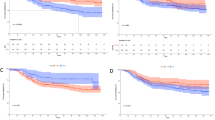
The association between ALP, LDH, and overall survival
The median follow-up time was 29.6 months, with a range of 0.2–167.0 months. The median OS was 39.6 months. By univariate analysis, we identified the following characteristics to be significantly associated with OS: the TNM stage (P < 0.001), distant metastasis (P < 0.001), surgery (P < 0.001), treatment purpose (P < 0.001), BMI (P < 0.001), PNI (P < 0.001), NLR (P = 0.003), PLR (P < 0.001), ALP (P < 0.001), and LDH (P < 0.001). In contrast, the following factors were not associated with OS: sex (P = 0.10), age (P = 0.15), tumor location (P = 0.87), and tumor differentiation (P = 0.21). In multivariate analysis, the TNM stage (P < 0.001), surgery (P < 0.001), PNI (P < 0.001), ALP (P = 0.004), and LDH (P < 0.001) remained as independent prognostic factors (Table 2). The survival curves of ALP (≤90.7/>90.7 U/L) and LDH (≤361.5/>361.5 U/L) for OS by Kaplan–Meier method were shown in Figs. 1 and 2, respectively.
We further classified the patients into three subgroups according to both levels of ALP (≤90.7/>90.7 U/L) and LDH (≤361.5/>361.5 U/L): group I: patients with a lower level of both ALP (≤90.7 U/L) and LDH (≤361.5 U/L), group III: patients with a higher level of both ALP (>90.7 U/L) and LDH (>361.5 U/L), and group II: all the rest of the patients. As a result, there were respectively 774 (85.4 %), 128 (14.1 %), and 4 (0.4 %) patients classified into group I, II, and III. The median OS of patients in group I, II, and III were 45.4, 23.7, and 4.2 months, respectively. The univariate analysis suggested that the ALP and LDH classification was significantly prognostic for OS of patients with ESCC. After adjustment by TNM stage, surgery, and PNI, which had been demonstrated to be independent prognostic factors, the ALP and LDH classification remained an independent prognostic factor. Compared with patients in group I, patients in both groups II and III showed significant worse OS (HR 95 % CI 1.56 (1.23–1.97), P < 0.001 and HR 95 % CI 5.06 (1.83–14.02), P = 0.002, respectively), and patients in group III had the worst OS among the three groups (Table 3). The prognostic value of the ALP and LDH classification for OS was presented in Fig. 3.
The prognostic value of the ALP and LDH classification for overall survival in patients with esophageal squamous cell carcinoma. Full legend: the ALP and LDH classification stratified patients into three subgroups with distinct overall survival. Patients in group III had the worst prognosis with a median overall survival of 4.2 months
The prognostic value of the ALP and LDH classification in subgroups
To further test the prognostic value of the ALP and LDH classification in patients with ESCC, we repeated the univariate and multivariate analysis in subgroups of patients stratified by the following clinicopathological and treatment characteristics: sex (male/female), age (≤58/>58 years), tumor location (upper/middle/lower esophagus), degree of differentiation (poorly or not/moderate/well differentiated), tumor stage (I + II + III/IV), surgery (no/yes), and treatment purpose (curative/palliative treatment). The detailed results were shown in Table 3.
In univariate analysis, the ALP and LDH classification was found to be a significant prognostic factor in all subgroups of patients except for females. The multivariate analysis was performed adjusted by all possible prognostic factors as listed in Table 2 except for the one used for patient stratification. It was demonstrated that the ALP and LDH classification remained significantly and independently prognostic in most subgroups. Its prognostic value for OS in ESCC was not influenced by the degree of tumor differentiation and tumor stage. However, the analysis in subgroups also allowed us to identify some features of patients in which the ALP and LDH classification could be more appropriately used for OS prediction. Those subgroups included male patients, patients at a younger age (≤58 years), patients with tumor located in the upper and middle esophagus, patients without resection of primary esophageal tumor, and patients receiving palliative treatment (Table 3).
Discussion
There have been ongoing interests in identifying prognostic factors besides the TNM stage in ESCC. Previous studies have demonstrated the prognostic value of some easily available indicators, such as the BMI [19] and some inflammation-based prognostic factors like PNI [20], NLR, and PLR [21]. To further categorize patients with different prognosis, more prognostic factors are warranted.
ALP and LDH are both routinely tested serum enzymes in clinical practice, which makes them easily available. Their prognostic value has been proved in some other cancers such as prostate cancer and nasopharyngeal carcinoma [6, 7, 11, 22]. Investigations about the prognostic value of ALP and LDH in ESCC were limited owing to small-sized studies and inconsistent conclusions. To the best of our knowledge, our study was not only the first one to specifically explore the prognostic value of ALP in ESCC but also the largest one to test the prognostic value of LDH in ESCC. What’s more, for the first time, we found that the ALP and LDH classification by the combination of ALP and LDH could categorize patients into three subgroups with distinct prognosis.
Special attention should be paid to group III of the ALP and LDH classification. Although there were only four patients in this group, the OS of this group of patients was particularly poor, with a median OS of only 4.2 months. All the four patients were males, at stage IV, and had a poor tumor differentiation. The ALP and LDH classification might be a simple and convenient method to distinguish a small part of patients with extremely poor prognosis.
The mechanism of how ALP and LDH influence or reflect prognosis in cancer is not completely understood. ALP is a hydrolase enzyme presenting in all tissues and is concentrated in certain organs, such as the liver, kidney, bone, and placenta [23]. The elevation of ALP is related with some bone and hepatobiliary diseases [24]. A hepatocellular carcinoma staging system includes ALP > 200 IU/L as a score indicator for poor outcome [25]. However, the elevation of ALP is not only associated with bone and hepatobiliary diseases but also has some roles in malignancies. Certain subtypes of ALP have been found to be expressed in several malignant cell lines [26–28]. Thus, the elevation of ALP could possibly reflect a heavy tumor burden. Due to heterogeneity of tumor cells, tumors with heavier load contain tumor cells with greater diversities, which possibly endow the inclination for treatment resistance [29]. This is consistent with the findings of a previous study by Kogo M et al. They found that the elevation of ALP predicted worse response to chemoradiotherapy in EC [30]. Similar discoveries have also been made in metastatic colorectal cancer [4]. Our study found that a higher level of ALP was related with more advanced TNM stage and more distant metastasis, but not associated with T stage or N stage, suggesting that instead of promoting tumor progression, the elevation of ALP was more likely to reflect a heavier tumor burden in ESCC.
LDH is an important enzyme in energy production in many cell types, which catalyzes the conversion of pyruvate to lactate in hypoxic conditions. It is demonstrated that various malignancies express a higher level of LDH isoforms than normal cells. Lactate, a product of glycolysis, has been demonstrated to have critical roles in regulating carcinogenesis, tumor metabolic reprogramming, and tumor angiogenesis [31]. Thus, except for reflecting a heavier tumor burden, the elevation of LDH may also promote tumor progression by influencing the tumor metabolism and microenvironment. This is consistent with our finding that the level of LDH is associated with tumor differentiation. What is noteworthy is that there have already been much interests in developing therapeutic targets to inhibit isoforms of LDH, the LDHA and LDHB [32–34].
In the subgroup analysis, we identified some subgroups of patients in which the ALP and LDH classification was not prognostic. These subgroups contained female patients, patients with an older age (>58 years), patients with tumors located in the lower esophagus, patients receiving resection of esophageal tumors, and patients receiving curative treatment. It was explicable that the ALP and LDH classification had little prognostic value in patients who received curative treatment and resection of esophageal tumors because those patients might have very low tumor load after receiving resection of esophageal tumors. In this case, some other factors, such as the TNM stage, would be much more valuable than ALP and LDH in the prognosis of ESCC. However, there were no convincing explanations for the other three subgroups. More investigations were warranted to reveal the mechanism behind the appearance.
Although our study provided some meaningful findings about the prognostic value of ALP and LDH in ESCC, there are still some inevitable limitations. The most important one was that the implication of ALP and LDH in prognosis prediction was actually limited. It was because there were some other factors influencing the levels of ALP and LDH excepting for the tumors, especially some hepatobiliary and bone diseases. ALP and LDH might not be predictive in these patients. In our study, there were no patients with bone metastasis or bone diseases. There were 110 (12.1 %) patients with chronic hepatitis B virus infection. However, no patients had active chronic hepatitis B virus infection. In addition, our study was conducted retrospectively; the conclusions were not as convincing as those from the prospective ones. Last but not least, both ALP and LDH were continuous variables, it might cause some inconvenience to be used in clinical practice. However, we determined an optimal cutoff point for each factor, which made it easier for application. In conclusion, we made a good supplement for previous investigations about the prognostic value of ALP and LDH in ESCC and proposed the ALP and LDH classification to help predict OS in ESCC for the first time in this study.
References
Lin Y, Totsuka Y, He Y, Kikuchi S, Qiao Y, Ueda J, Wei W, Inoue M, Tanaka H. Epidemiology of esophageal cancer in Japan and China, vol. 23, 2013:233–42.
Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut 2014.
Rice TW, Rusch VW, Ishwaran H, Blackstone EH. Cancer of the esophagus and esophagogastric junction: data-driven staging for the seventh edition of the American Joint Committee on Cancer/International Union Against Cancer Cancer Staging Manuals. Cancer. 2010;116:3763–73.
Maisano R, Azzarello D, Del MP, Maisano M, Bottari M, Egitto G, et al. Alkaline phosphatase levels as a prognostic factor in metastatic colorectal cancer treated with the FOLFOX 4 regimen: a monoinstitutional retrospective study. Tumori. 2011;97:39–42.
Sonpavde G, Pond GR, Berry WR, de Wit R, Armstrong AJ, Eisenberger MA, et al. Serum alkaline phosphatase changes predict survival independent of PSA changes in men with castration-resistant prostate cancer and bone metastasis receiving chemotherapy. Urol Oncol. 2012;30:607–13.
Xie W, Nakabayashi M, Regan MM, Oh WK. Higher prostate-specific antigen levels predict improved survival in patients with hormone-refractory prostate cancer who have skeletal metastases and normal serum alkaline phosphatase. Cancer. 2007;110:2709–15.
Xie Y, Wei ZB, Duan XW. Prognostic value of pretreatment serum alkaline phosphatase in nasopharyngeal carcinoma. Asian Pac J Cancer Prev. 2014;15:3547–53.
Sagman U, Feld R, Evans WK, Warr D, Shepherd FA, Payne D, et al. The prognostic significance of pretreatment serum lactate dehydrogenase in patients with small-cell lung cancer. J Clin Oncol. 1991;9:954–61.
Armstrong AJ, George DJ, Halabi S. Serum lactate dehydrogenase predicts for overall survival benefit in patients with metastatic renal cell carcinoma treated with inhibition of mammalian target of rapamycin. J Clin Oncol. 2012;30:3402–7.
Brown JE, Cook RJ, Lipton A, Coleman RE. Serum lactate dehydrogenase is prognostic for survival in patients with bone metastases from breast cancer: a retrospective analysis in bisphosphonate-treated patients. Clin Cancer Res. 2012;18:6348–55.
Wei Z, Zeng X, Xu J, Duan X, Xie Y. Prognostic value of pretreatment serum levels of lactate dehydrogenase in nonmetastatic nasopharyngeal carcinoma: single-site analysis of 601 patients in a highly endemic area. Onco Targets Ther. 2014;7:739–49.
Yamada Y, Nakamura K, Aoki S, Tobiume M, Zennami K, Kato Y, et al. Lactate dehydrogenase, Gleason score and HER-2 overexpression are significant prognostic factors for M1b prostate cancer. Oncol Rep. 2011;25:937–44.
Huang JJ, Cai MY, Ye S, Li ZM, Huang HQ, Lin TY. Clinical analysis of 19 cases of subcutaneous panniculitis T-cell lymphoma with literature review. Ai Zheng. 2009;28:1093–9.
Chau I, Norman AR, Cunningham D, Waters JS, Oates J, Ross PJ. Multivariate prognostic factor analysis in locally advanced and metastatic esophago-gastric cancer—pooled analysis from three multicenter, randomized, controlled trials using individual patient data. J Clin Oncol. 2004;22:2395–403.
Polee MB, Hop WC, Kok TC, Eskens FA, van der Burg ME, Splinter TA, et al. Prognostic factors for survival in patients with advanced oesophageal cancer treated with cisplatin-based combination chemotherapy. Br J Cancer. 2003;89:2045–50.
Alici S, Ugras S, Bayram I, Izmirli M. Prognostic factors and COX-2 expression in advanced stage esophageal squamous cell carcinoma. Adv Ther. 2006;23:672–9.
Zhang P, Xi M, Li QQ, He LR, Liu SL, Zhao L, et al. The modified Glasgow prognostic score is an independent prognostic factor in patients with inoperable thoracic esophageal squamous cell carcinoma undergoing chemoradiotherapy. J Cancer Educ. 2014;5:689–95.
Budczies J, Klauschen F, Sinn BV, Gyorffy B, Schmitt WD, Darb-Esfahani S, et al. Cutoff finder: a comprehensive and straightforward Web application enabling rapid biomarker cutoff optimization. PLoS One. 2012;7, e51862.
Zhang SS, Yang H, Luo KJ, Huang QY, Chen JY, Yang F, et al. The impact of body mass index on complication and survival in resected oesophageal cancer: a clinical-based cohort and meta-analysis. Br J Cancer. 2013;109:2894–903.
Feng JF, Chen QX. Significance of the prognostic nutritional index in patients with esophageal squamous cell carcinoma. Ther Clin Risk Manag. 2014;10:1–7.
Feng JF, Huang Y, Liu JS. Combination of neutrophil lymphocyte ratio and platelet lymphocyte ratio is a useful predictor of postoperative survival in patients with esophageal squamous cell carcinoma. Onco Targets Ther. 2013;6:1605–12.
Turen S, Ozyar E, Altundag K, Gullu I, Atahan IL. Serum lactate dehydrogenase level is a prognostic factor in patients with locoregionally advanced nasopharyngeal carcinoma treated with chemoradiotherapy. Cancer Investig. 2007;25:315–21.
Weiss MJ, Ray K, Henthorn PS, Lamb B, Kadesch T, Harris H. Structure of the human liver/bone/kidney alkaline phosphatase gene. J Biol Chem. 1988;263:12002–10.
Xu XS, Wan Y, Song SD, Chen W, Miao RC, Zhou YY, et al. Model based on gamma-glutamyltransferase and alkaline phosphatase for hepatocellular carcinoma prognosis. World J Gastroenterol. 2014;20:10944–52.
Leung TW, Tang AM, Zee B, Lau WY, Lai PB, Leung KL, et al. Construction of the Chinese University Prognostic Index for hepatocellular carcinoma and comparison with the TNM staging system, the Okuda staging system, and the Cancer of the Liver Italian Program staging system: a study based on 926 patients. Cancer. 2002;94:1760–9.
Zhang M, Yan X, Zhang F. Expression of placental alkaline phosphatase in esophageal cancer cell line Eca109. Zhonghua Zhong Liu Za Zhi. 1996;18:186–8.
Ali NN, Rowe J, Teich NM. Constitutive expression of non-bone/liver/kidney alkaline phosphatase in human osteosarcoma cell lines. J Bone Miner Res. 1996;11:512–20.
Tokumitsu SI, Tokumitsu K, Kohnoe K, Takeuchi T. Characterization of liver-type alkaline phosphatase from human gastric carcinoma cells (KMK-2) in vitro. Cancer Res. 1979;39:4732–8.
Burrell RA, Swanton C. Tumour heterogeneity and the evolution of polyclonal drug resistance. Mol Oncol. 2014;8:1095–111.
Kogo M, Suzuki A, Kaneko K, Yoneyama K, Imawari M, Kiuchi Y. Scoring system for predicting response to chemoradiotherapy, including 5-fluorouracil and platinum, for patients with esophageal cancer. Dig Dis Sci. 2008;53:2415–21.
Doherty JR, Cleveland JL. Targeting lactate metabolism for cancer therapeutics. J Clin Invest. 2013;123:3685–92.
Baggstrom MQ, Qi Y, Koczywas M, Argiris A, Johnson EA, Millward MJ, et al. A phase II study of AT-101 (Gossypol) in chemotherapy-sensitive recurrent extensive-stage small cell lung cancer. J Thorac Oncol. 2011;6:1757–60.
Liu G, Kelly WK, Wilding G, Leopold L, Brill K, Somer B. An open-label, multicenter, phase I/II study of single-agent AT-101 in men with castrate-resistant prostate cancer. Clin Cancer Res. 2009;15:3172–6.
Han X, Sheng X, Jones HM, Jackson AL, Kilgore J, Stine JE, et al. Evaluation of the anti-tumor effects of lactate dehydrogenase inhibitor galloflavin in endometrial cancer cells. J Hematol Oncol. 2015;8:2.
Acknowledgments
This work was supported by The National Natural Science Foundation of China (No. 81372570), The Science and Technology Department of Guangdong Province, China (No. 2012B031800088), and The Science and Technology Department of Guangdong Province, China (No. C2011019). We gratefully thank all the staff members in our department for their support and suggestion in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xiao-li Wei and Dong-sheng Zhang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wei, Xl., Zhang, Ds., He, Mm. et al. The predictive value of alkaline phosphatase and lactate dehydrogenase for overall survival in patients with esophageal squamous cell carcinoma. Tumor Biol. 37, 1879–1887 (2016). https://doi.org/10.1007/s13277-015-3851-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3851-y