Abstract
Forkhead box P3 (FoxP3) expression in papillary thyroid carcinoma (PTC) is associated with resistance to radioiodine treatment. The sodium iodine symporter (NIS) is a plasma membrane glycoprotein, the repression of which may render the tumor refractive to radioiodine therapy. In this study, samples from 90 PTCs as well as 40 normal thyroid tissues were examined for FoxP3 and NIS by immunohistochemistry and real-time PCR. We found that FoxP3 was associated with decreased NIS expression. Lentiviral-mediated FoxP3-overexpressing cells were constructed and real-time PCR and western blotting were performed to evaluate the expression of NIS. Meanwhile, key members of the transforming growth factor-β1 (TGF-β1) pathway were explored by ELISA and immunofluorescence and a neutralizing TGF-β1 antibody was used to block activity. In vitro, FoxP3 overexpression significantly reduced NIS transcript and protein levels and the TGF-β1 pathway was activated. However, treatment with neutralizing TGF-β1 antibody partially abrogated FoxP3-induced NIS repression. These findings suggest that FoxP3 could compromise NIS expression by inducing TGF-β1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) accounts for the majority of thyroid cancers (85–90 %) and generally carries an excellent prognosis, with a 10-year survival rate of 90 % [1, 2]. Following thyroidectomy, radioiodine ablation is the primary treatment for PTC; however, some patients may fail to respond when the cancer has lost radioiodine avidity. Multiple lines of evidence suggest decreased expression of sodium iodine symporter (NIS) is associated with this loss of radioiodine responsiveness [3, 4].
NIS is an intrinsic plasma membrane protein that mediates active transport of iodine in thyroid cells, where it is concentrated and organified. It is mainly regulated by TSH, which increases transcript and protein levels of NIS, but is also required for targeting of NIS to the thyrocyte plasma membrane [5]. In addition to TSH, transforming growth factor-β1 (TGF-β1), estrogen, and iodine also play an indispensable role in NIS modulation [6–10]. TGF-β1, which inhibits thyroid function by antagonizing the biological effect of TSH, is also a potent immunosuppressor and its upregulation is associated with autoimmunity, inflammation, and cancer [11, 12]. The Smads are a family of intracellular signaling transducers that function downstream of the TGF-β1 signaling pathway. They are the only TGF-β1 receptor substrates with the ability to amplify signals. TGF-β1 binds to a specific kinase (TβR-II) on the cell surface, leading to the activation of TβR-I, which then phosphorylates members of the Smad family (R-Smad2 and R-Smad3). The phosphorylated R-Smads form oligomers with Smad4 and immediately translocate to the nucleus, where the Smad compounds regulate the transcription of its target gene [13, 14].
Forkhead box P3 (FoxP3), which belongs to the forkhead box family, is a key regulator of CD4+CD25+ regulatory T cells (Tregs) and is considered the only definitive marker of Tregs [15, 16]. FoxP3 was considered to be specific to Tregs until Hanz et al. identified it in pancreatic carcinoma. Since then, many studies have confirmed that it is also expressed in a variety of tumor cells [17–24] and tumors that are FoxP3 positive usually have increased malignance which may be due to the suppression of immune function [21–24]. Studies have shown that FoxP3 in cancer cells mimics its function in the Tregs, which inhibit the proliferation and function of tumor-specific T cells through the secretion of immunosuppressive cytokines such as TGF-β1 and IL-10 [21, 22], thus leading to resistance of the tumors to immune destruction. More importantly, FoxP3 expression is significantly associated with resistance to radioiodine treatment [25].
In light of these findings, we supposed there might be a relationship between FoxP3 and NIS. TGF-β1 is a potent inhibitor of NIS transcription in normal thyroid epithelial cells and FoxP3 in cancer cells induces the secretion of TGF-β1; thus, we hypothesized that FoxP3 may inhibit the expression and membrane targeting of NIS by inducing TGF-β1 secretion and subsequent activation of the Smad signaling pathway. In this study, 90 papillary thyroid carcinomas and 40 normal thyroid tissues were examined by immunohistochemistry and real-time PCR. A significant decrease of NIS expression was observed in the FoxP3-positive group when compared with the FoxP3-negative group. Importantly, lentivirus-mediated FoxP3 overexpression demonstrated that FoxP3 inhibited NIS expression by inducing TGF-β1 secretion.
Materials and methods
Patients and tissues
First, a representative cohort of 90 nonconsecutive sporadic patients with PTC undergoing surgical resection from September 2013 to March 2014 was selected from the First Affiliated Hospital of Zhengzhou University (Henan, China). Forty normal thyroid tissues from the opposite lobe were taken as controls. Patients with a history of chemotherapy or radiation therapy before surgery were excluded from the study. The tissues were snap frozen and stored at −80 °C until use. Mean patient age was 44.3 ± 13.6 years and the female-to-male ratio was about 3:1. Tumors were staged according to the American Joint Committee on Cancer (AJCC) criteria. The study protocol was approved by the local medical ethics committee. Before surgery, each patient provided written, informed consent to the collection of fresh thyroid tissue for research.
Cell culture
The human PTC-derived TPC-1 cell line was a gift from Professor Zheng from the First Affiliated Hospital of Zhengzhou University. The cells were cultured in RP-1640 medium (Solarbio Biotech, Beijing, China) supplemented with 10 % donor calf serum (Gibio, USA) in an atmosphere containing 5 % CO2 at 37 °C. Meanwhile, a six-hormone mixture, including insulin (10 mg/mL; BioVision, USA), human transferrin (5 mg/mL; Sigma, Saint Louis, MO, USA), somatostatin (1 mg/mL; ProSpec, Israel), glycyl-l histidyl-l-lysine acetate (2 ng/mL; Sigma, Saint Louis, MO, USA), hydrocortisone (0.36 ng/mL; Sigma, Saint Louis, MO, USA), and TSH (10 mU/mL; ProSpec), was added to the culture to maintain the functional characteristics of iodine uptake and thyroid-specific protein synthesis over prolonged periods of culture [26]. Briefly, the effect on NIS expression was studied by starving near-confluent cells for TSH and insulin in the presence of 0.2 % serum (starvation medium) for 5 days, given the long half-life of NIS. Then, TSH and TGF-β1 (10 ng/mL; PeproTech) were added to the culture medium.
Construction of lentiviral vectors and the detection of infection efficiency
Lentiviral vectors of FoxP3 (LV-FoxP3) were constructed. The LV-FoxP3 gene was synthesized by GenePharma (Shanghai, China) as described previously [27]. To exclude the interference effect of the empty lentiviral vectors, we used them to infect TPC-1 and the infected cells were taken as the negative control group (LVNC). TPC-1 cells (1 × 104/well) were seeded in a 24-well plate and cultured in serum-free RP-1640 medium for 24 h. Then, lentiviral vectors infected the cells at an optimized multiplicity of infection. After 72 h, transfection efficiency was observed by inverted fluorescence microscopy and detected by flow cytometry (Becton Dickinson Biosciences).
RNA extraction, reverse transcription, and real-time PCR
Total RNA was extracted by TRIzol (TaKaRa Bio, Shiga, Japan); cDNA was synthesized according to the manufacturer’s instructions (TOYOBO, Japan) and quantified by real-time PCR on an ABI 7500 FAST system (Applied Biosystems), using the KOD SYBR Green qPCR Mix kit (TOYOBO, Japan) with appropriate primers: FoxP3, 5′-CACAACATGCGACCCCCTTTCACC-3′ (F) and 5′-AGGTTGTGGCGGATGGCGTTCTTC-3′ (R); TGF-β1, 5′-CAACAATTCCTGGCGATACA-3′ (F) and 5′-GGTAGTGAACCCGTTGATGTCC-3′ (R); and NIS, 5′-GCGTGGCTCTCTCAGTCAA-3′ (F) and 5′-GCGTCCATTCCTGAGCTG-3′ (R); primers were obtained from Sangon Biotech (Shanghai, China). Cycling conditions were as follows: 98 °C for 2 min, followed by 40 cycles of 98 °C for 10 s, 60 °C for 10 s, and 68 °C for 30 s. Relative expression was measured in triplicate and normalized to that of GAPDH. Analyses were performed by the 2−ΔΔCT method [28].
Antibodies and western blotting analysis
Anti-NIS and anti-FoxP3 antibodies were obtained from Abcam (Cambridge, UK). Antibodies against TGF-β1, TβR-I, pSmad3, and Smad3 were purchased from Sangon Biotech (Shanghai, China). The neutralizing TGF-β1 monoclonal antibody (BioLegend) was used to neutralize the TGF-β1 secreted in the medium. Total and plasma membrane proteins were extracted according to the manufacturer’s instructions (BestBio, China). Western blotting was performed according to standard methods, using anti-FoxP3 (1:100), anti-NIS (1:100), anti-TGF-β1 (1:500), anti-TβR-I (1:500), anti-pSmad3 (1:500), and anti-Smad3 antibodies (1:500). After incubation with the secondary antibody, immune complexes were detected by eECL western blot kit (Thermo Scientific).
Immunohistochemistry
Paraffin-embedded sections were obtained from the Department of Pathology of the First Affiliated Hospital of Zhengzhou University. The slides included samples from 90 papillary thyroid carcinomas and 40 normal thyroid tissues. Sections were studied by a PV-9000 two-step protocol (Zhongshan Golden Bridge Biotechnology, Beijing, China) according to manufacturer’s instructions. The working concentrations of human anti-FoxP3 and anti-hNIS were 1:100 and 1:50, respectively. The main criterion for NIS positivity was the presence of plasma membrane immunoreactivity, as it is essential for NIS to be functional. After the initial review and selection, all slides were reexamined by two independent pathologists.
Immunofluorescence analysis
TPC-1 cells were seeded onto chamber slides and incubated for 24 h. The cells were then fixed in 4 % paraformaldehyde for 20 min, permeabilized with 0.25 % Triton X-100 for 15 min, and blocked with 1 % BSA for 30 min at room temperature. After incubation with anti-TβR-I (1:50), anti-pSmad3 (1:50), and anti-FoxP3 (1:100) overnight at 4 °C, TPC-1 cells were exposed to Cy3-tagged secondary antibody diluted at 1:500 for 1 h at room temperature and DAPI (Vectashield, Vector Laboratories) for 2 min. The distribution and localization of target proteins were examined with a Leica confocal TCS SP2 microscope.
ELISA assay
TPC-1 cells were cultivated at a density of 5 × 105 cells/well in six-well plates. When the cell confluence was about 70 %, the supernatants were abandoned and fresh medium was added. Forty-eight hours later, the medium was collected and TGF-β1 secreted into the medium was determined by ELISA kit (Dakewe Biotech, Shenzhen, China), according to manufacturer’s instructions.
Statistical analysis
Data were analyzed with SPSS 20.0 software (IBM, Endicott, NY). Correlations between FoxP3 and clinicopathological parameters were determined and results are presented as mean ± SE or as percentages, as appropriate. We used the t test to compare continuous variables, and the Fisher exact test and Pearson chi-square test were also performed to compare clinical and pathological data between FoxP3-positive patients and FoxP3-negative patients. Comparisons between more than two groups were assessed by one-way ANOVA, followed by a Bonferroni test, and P < 0.05 was considered statistically significant.
Result
FoxP3 was expressed in tumor cells of papillary thyroid carcinoma and was associated with decreased NIS expression
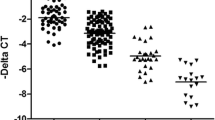
Among the tumor specimens that were immunostained for FoxP3, 66 of 90 (74 %) scored positive. In contrast, all normal cases were negative for FoxP3 staining (Fig. 1a). FoxP3 subcellular staining was usually observed in the nucleus and cytoplasm of the epithelial cells of the classical type (Fig. 1b) or the follicular variant (Fig. 1c). In all tumor specimens, we detected sporadic FoxP3-positive tumor-infiltrating lymphocytes (Fig. 1d), which presumably represented Tregs. As shown in Table 1, correlation of FoxP3 expression with clinicopathological features was significant only for the presence of extrathyroid invasion (P = 0.04). The results also revealed that NIS staining was located almost exclusively at the plasma membrane in normal thyroid tissues (Fig. 1e); however, staining was less intense in tumor tissues, particularly in those that were FoxP3 positive (Fig. 1f). Moreover, the limited amounts of NIS protein were confined almost exclusively to the cytoplasm rather than being targeted to the plasma membrane. We analyzed NIS staining in the FoxP3-positive and FoxP3-negative groups. As shown in Table 2, the FoxP3-positive group had a lower rate of NIS-positive staining (31.8 vs. 66.7 %) (P < 0.01). NIS transcript levels were also significantly reduced in tumor samples vs. normal tissue and in the FoxP3-positive group vs. the FoxP3-negative group (P < 0.001) (Table 3).
Expression of NIS and FoxP3 in papillary thyroid carcinomas and normal thyroid tissues. a Normal thyroid epithelial cells were FoxP3 negative. b Negative controls for FoxP3 in normal thyroid tissues. c Expression of FoxP3 in the nucleus and cytoplasm of epithelial cells of the classical type. d Negative controls for FoxP3 in papillary thyroid carcinomas. e FoxP3-positive staining in epithelial cells of the follicular variant. f Infiltrating lymphocytes, known as Tregs. g Expression of NIS in the epithelial cells of normal thyroid tissues and h papillary thyroid carcinomas. Magnification ×400
TGF-β1 inhibited NIS expression in TPC-1 cells
TPC-1 cells were pre-treated with human recombinant TGF-β1 for 24 h; transcript levels of NIS decreased and got a minimum at the concentration of 10 ng/mL, about a sixfold decrease compared to those in the control group (P < 0.01) when the cells were treated with increasing concentrations of recombinant TGF-β1 (1, 5, or 10 ng/mL) (Fig. 2a). NIS protein levels were also strongly suppressed by TGF-β1, and there was a roughly twofold decrease relative to the control group (P < 0.01) when the TPC-1 cells were incubated with 10 ng/mL TGF-β1 (Fig. 2b).
Effect of TGF-β1 on NIS expression in TPC-1 cells. a After incubation with TGF-β1 (1, 5, or 10 ng/mL) for 24 h, NIS mRNA levels were determined by real-time PCR. GAPDH was used as the reaction control. b After incubation with TGF-β1 (1, 5, or 10 ng/mL) for 48 h, NIS expression was detected by western blotting and normalized to Na+–K+–ATPase expression: top representative immunoblots, bottom densitometric analysis. Bars represent the mean ± SE of three independent experiments. *P<0.05 vs. the control; **P < 0.01 to 0.001 vs. the control; ***P < 0.001 vs. the control
Infection efficiency of lentiviral vectors
Infection efficiency of lentiviral vectors in TPC-1 cells was assessed by analyzing green fluorescent protein (GFP) expression by inverted fluorescence microscopy. TPC-1 cells generated abundant GFP in the LV-FoxP3 and LVNC group, but no GFP was present in the non-infected group (Fig. 3a). In addition, GFP positivity was detected by flow cytometry. GFP positivity, equivalent to the infection efficiency, was 0.2 % (non-infected group), 99.3 % (LV-FoxP3 group), and 99.6 % (LVNC group) (Fig. 3b). The results indicated that the lentiviral vectors efficiently infected TPC-1 cells and regulated FoxP3 expression.
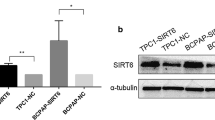
FoxP3 overexpression in TPC-1 cells induced activation of TGF-β1 signaling
After infection, FoxP3 messenger RNA (mRNA) and protein levels increased significantly in the LV-FoxP3 group vs. the control (P < 0.001). Meanwhile, there was a noticeable increase of TGF-β1 mRNA and protein expression in LV-FoxP3 cells vs. the control (P < 0.01) (Fig. 4a, b). To validate the induction of TGF-β1 secretion by FoxP3, cell culture supernatants were analyzed by ELISA (Fig. 4c); the results showed that FoxP3 overexpression led to >5-fold upregulation of TGF-β1 protein levels in the medium (P < 0.001). We analyzed the expression of other key members of the TGF-β1/Smad signaling pathway to determine whether the secreted TGF-β1 was biologically active. Western blotting revealed a noticeable increase in TβR-I and pSmad3 protein levels (P < 0.01), but no difference in total Smad3 protein levels (Fig. 4b). Similarly, there was no significant difference between the control group and the LVNC group for the whole targets. Immunofluorescence assays also confirmed that plasma membrane localization of TβR-I and phosphorylation of Smad3 were notably induced in the transfected TPC-1 cells (Fig. 5).
Effect of FoxP3 overexpression on key members of the TGF-β1 signaling pathway in TPC-1 cells. a Total RNA was extracted from cultured TPC-1 cells and analyzed by real-time PCR for FoxP3 and TGF-β1. b Total protein was extracted and analyzed by western blotting for FoxP3, TGF-β1, TβR-I, pSmad3, and Smad3. Left representative immunoblots. Right densitometry analysis of FoxP3, TGF-β1, TβR-I, pSmad3, and Smad3. Each bar represents the mean ± SE of three independent experiments. *P < 0.05 vs. the control group; **P < 0.01 to 0.001 vs. the control; ***P < 0.001 vs. the control. c ELISA of TGF-β1 secreted in the medium
NIS repression by FoxP3 is based on an autocrine TGF-β1 loop and neutralizing TGF-β1 antibody rescued FoxP3-induced repression of NIS
FoxP3 overexpression not only inhibited NIS transcript expression but also impaired NIS protein targeting to the plasma membrane (Fig. 6a, b). To verify whether the TGF-β1 pathway mediates this inhibition, we incubated the cells in LV-FoxP3 group with a neutralizing TGF-β1 antibody of indicated concentrations (1, 5, or 10 μg/mL); 24 h later, total RNA was extracted and real-time PCR showed that the decreased expression levels of NIS mRNA were rescued by neutralizing TGF-β1 antibody, about 70.6 % of the inhibitory effect of FoxP3 on NIS was abrogated (Fig. 6a). Forty-eight hours later, membrane protein was extracted and we observed that FoxP3-induced repression of NIS targeting to the plasma membrane was partially abrogated (up to 71.2 %) when cells were incubated with increasing amounts of TGF-β1 neutralizing antibody (Fig. 6b).
Effect of neutralizing TGF-β1 antibody on NIS expression in TPC-1 cells. Cells were cultured with increasing concentrations of neutralizing TGF-β1 antibody (1, 5, or 10 μg/mL). a After 24 h, total RNA was extracted and NIS was analyzed by real-time PCR. b After 48 h, membrane proteins were extracted and analyzed by western blotting: top representative immunoblots, bottom densitometry analysis. Results are presented as mean ± SE. *P < 0.05 vs. the control; **P < 0.01 to 0.001 vs. the control; ***P < 0.001 vs. the control. # P < 0.05 vs. the LVCA-FoxP3 group; ## P < 0.01 to 0.001 vs. the LVCA-FoxP3 group; ### P < 0.001 vs. the LVCA-FoxP3 group
Discussion
Radioiodine ablation has become an important auxiliary treatment for differentiated thyroid cancer. It is mainly used to remove the residual tissues after thyroidectomy; moreover, the metastatic lesions which cannot be cut off by surgery can also be cleaned up by it. Generally, patients with PTC always have a good prognosis by combined surgical and radioiodine treatment [1, 2], but a few cases become resistant to radioiodine therapy. Patients who have reduced expression of NIS are more disposed to an iodine-refractory metastatic disease, leading to a worse prognosis [3–5]. We demonstrated in our study that NIS transcript levels were noticeably reduced in all of the papillary thyroid carcinomas in comparison to normal tissues. IHC also revealed that NIS staining was less intense in tumor tissues; moreover, the limited amounts of NIS protein were confined exclusively to the cytoplasm rather than being targeted to the plasma membrane. The results indicated that the expression levels of NIS as well as its localization in tumor tissues altered greatly when compared with the normal thyroid tissues.
NIS is an intrinsic plasma membrane protein, which offers thyroid cells the unique function to uptake, concentrate, and organify iodine. It is mainly regulated by TSH, the stimulation of which results, at least in part, from the cAMP-mediated increase in NIS biosynthesis. RET/PTC, RAS, or BRAF appears frequently in PTC and can induce tumor dedifferentiation in part by inhibiting thyroid-specific gene expression, including NIS expression [29–31]. In addition, TGF-β1 is also an effector that can inhibit NIS expression through the TGF-β1/Smad pathway in normal and tumor thyroid cells [6, 10, 29]. Studies have demonstrated that the inhibitory effect of TGF-β1 on NIS expression is associated with functional interaction between transcription factor Pax8 and Smad3 [9]. However, the effect and revolved mechanism of TGF-β1 on NIS expression in thyroid cancer cells is still controversial. It has been confirmed that TGF-β1 can inhibit normal epithelial thyroid cells including their proliferation and differentiation. TGF-β1 has also been demonstrated to be overexpressed in thyroid tumors; however, the thyroid cancer cell lines are frequently resistant to its growth inhibitory effect instead. Some scholars believed that loss of TGF-β responsiveness could be due to a reduced expression of TGF-β receptors or to alterations of other members of TGF-β signaling pathway [7–10]; therefore, the inhibitory effect of TGF-β on the synthesis of thyroid-specific proteins such as NIS would also disappear in tumor cells. However, in this study, a significant decrease of NIS was observed when the TPC-1 cells were incubated with indicated concentrations of TGF-β1, which was consistent with that observed in previous studies [7–10]. We believe that this peculiar pleiotropic behavior of TGF-β1 on growth was background dependent and may result from cross-talk with signaling pathways mediated by other growth factors, among which EGF-like ligands play an important role [6]. In tumor cases, the growth inhibitory effect of TGF-β1 may be blocked by the EGF; however, the expression levels of Smad4 remained normal or increased. It is possible that factors like EGF inhibit Smad4 combining to the target genes which regulate growth, but the TGF-β1 signaling pathway could still play its inhibitory functions on thyroid-specific protein synthesis through the common partner Smad4 combining to other target genes.
FoxP3, which was previously considered to be strictly expressed within the Tregs, has been detected in multiple kinds of cancer cells [20–25]. FoxP3-positive tumors are more likely to invade and metastasize, perhaps by inducing the secretion of immunosuppressive cytokines such as TGF-β1 and IL-10 [21, 22]. This may represent a model of molecular mimicry and could reveal a hidden mechanism of immune evasion by cancer cells [21]. Here, we demonstrated in a small representative patient population that FoxP3 expression in PTC was associated with extrathyroid invasion. Because we wanted to analyze the relationship between FoxP3 expression and distant disease, we tended to choose the patients who already had the invasion and metastasis when collecting the cases; therefore, the distant disease rate was high when compared with that in previous literatures. Considering that FoxP3 is involved in autoimmune thyroid disease, we also divided the patients into different groups according to their status of Hashimoto and Grave’s diseases in Table 1; however, we found no significance between the FoxP3-positive and FoxP3-negative patients in the incidence of autoimmune thyroid disease. Furthermore, by analyzing the relationship between FoxP3 and NIS, we discovered that FoxP3 expression was associated with decreased NIS expression. These observations strongly suggest that FoxP3 may inhibit NIS expression and provide a clinical context for the subsequent in vitro research, but the relationship between FoxP3, TGF-β1, and NIS remains unclear.
The main aim of the second part of the study was to test the hypothesis that FoxP3 overexpression suppresses NIS through the TGF-β1/Smad pathway. First, we established the lentiviral-mediated FoxP3 overexpression model and observed that FoxP3 sharply inhibited NIS expression, which coincided with the previous finding that FoxP3 expression was associated with resistance to radioiodine treatment [25]. Then, wide activation of the TGF-β1/Smad pathway was detected by immunofluorescence and western blotting, indicating that FoxP3 overexpression indeed promotes TGF-β1 secretion in TPC-1 cells. Lastly and most importantly, we discovered that the neutralizing TGF-β1 monoclonal antibody rescued FoxP3-induced repression of NIS. It is clear that TGF-β induces FoxP3 expression; here, we propose that FoxP3 promotes TGF-β1 secretion, which in return induces FoxP3 expression in a positive feedback loop.
Our findings support the hypothesis that FoxP3 promotes TGF-β1 secretion, leading to NIS repression, which is associated with radioiodine therapy resistance. The study does have some limitations. Above all, we only analyzed NIS at the transcript and protein levels; we did not detect iodine transport in the TPC-1 cells. Moreover, considering that the transcript and protein levels of FoxP3 in TPC-1 cells were very low, we did not suppress expression with small interfering RNA targeting FoxP3. Therefore, the FoxP3-downregulated cells were not constructed to further illustrate the problem. Last but not least, there is no assessment of BRAF mutational status in the clinical specimens, which is a highly prevalence mutation (up to 70 % of samples in some studies), and is associated with decreased NIS expression, radioiodine refractory status, and increased tumor aggressiveness. In this study, NIS expression did not return to normal levels after treatment with the neutralizing TGF-β1 antibody, indicating that factors other than TGF-β1 could mediate FoxP3 inhibition of NIS and BRAF mutation may contribute a lot to it. We also hypothesize that FoxP3 can directly act on the transcript regulation regions of NIS as FoxP3 itself is a transcription factor. We will focus on the relationship between BRAF mutation status, FoxP3, and NIS expression in our next work. Moreover, we will use the BRAF-positive K-1 PTC cell line at the same time in vitro to test whether the conclusions we summarized from the BRAF-negative TPC-1 can be of the same assessment in the K-1.
Although the precise role of FoxP3 in promoting malignancy and resistance to radioiodine treatment requires further investigation, we believe the activation of TGF-β1 signaling may explain it to a large degree. This study may provide new insights into the understanding of thyroid carcinogenesis. More importantly, we suggest that FoxP3 is expected to become a new diagnostic hallmark and therapeutic target for PTC. Developing drugs that simultaneously target FoxP3 and TGF-β1 will be of great importance because they can abrogate the repression of NIS and provide relief to patients with cancers that are refractory to radioiodine therapy. They may also weaken the suppression of immune function, thereby leading to a reduced presence of extrathyroid invasion and lymph node metastasis.
References
Xing MZ. Molecular pathogenesis and mechanisms of thyroid cancer. Nat Rev Cancer. 2013;13:184–99.
Lopes JP, Fonseca E. BRAF gene mutation in the natural history of papillary thyroid carcinoma: diagnostic and prognostic implications. Acta Med Port. 2011;4:855–68.
Lakshmanan A, Scarberry D, Shen DH, Jhiang SM. Mutation of sodium iodine symporter in thyroid cancer. Horm Cancer. 2014;5:363–73.
Chung JK, Cheon GJ. Radioiodine therapy in differentiated thyroid cancer: the first targeted therapy in oncology. Endocrinol Metab. 2014;29:233–9.
Kogai T, Brent GA. The sodium iodide symporter (NIS): regulation and approaches to targeting for cancer therapeutics. Pharmacol Ther. 2014;135:355–70.
Mincione G, Di Marcantonio MC, Tarantelli C, D’Inzeo S, Nicolussi A, Nardi F, Donini CF, Coppa A. EGF and TGF-β1 effects on thyroid function. J Thyroid Res. 2011; 431718.
Serrano-Nascimento C, da Silva Teixeira S, Nicola JP, Nachbar RT, Masini-Repiso AM, Nunes MT. The acute inhibitory effect of iodide excess on sodium/iodide symporter expression and activity involves the PI3K/Akt signaling pathway. Endocrinology. 2014;155:1145–56.
Xu S, Chen G, Peng W, Renko K, Derwahl M. Oestrogen action on thyroid progenitor cells: relevant for the pathogenesis of thyroid nodules? J Endocrinol. 2013;218:125–33.
Costamagna E, Garıa B, Santisteban P. The functional interaction between the paired domain transcription factor Pax8 and Smad3 is involved in transforming growth factor-beta repression of the sodium/iodide symporter gene. Biol Chem. 2004;5:3439–46.
Eloy C, Santos J, Cameselle-Teijeiro J, Soares P, Sobrinho-Simões M. TGF-beta/Smad pathway and BRAF mutation play different roles in circumscribed and infiltrative papillary thyroid carcinoma. Virchows Arch. 2012;460:587–600.
Zhang J, Wang Y, Li D, Jing S. Notch and TGF-β1/Smad3 pathways are involved in the interaction between cancer cells and cancer-associated fibroblasts in papillary thyroid. Tumour Biol. 2014;35:379–85.
Poveda KT, Román MB, González C, García AB, Morales VHB, Zaragoza OP, et al. Role of IL-10 and TGF-β1 in local immunosuppression in HPV associated cervical neoplasia. World J Clin Oncol. 2014;5:753–63.
D'Inzeo S, Nicolussi A, Donini CF, Zani M, Mancini P, Nardi F, et al. A novel human Smad4 mutation is involved in papillary thyroid carcinoma. Endocr Relat Cancer. 2012;19:39–55.
Brown KA, Pietenpol JA, Moses HL. A tale of two proteins: differential roles and regulation of Smad2 and Smad3 in TGF-β signaling. J Cell Biochem. 2007;101:9–33.
Hori S. Stability of regulatory T-cell lineage. Adv Immunol. 2011;112:1–24.
Haque R, Lei F, Xiong X, Song J. The regulation of FoxP3-expressing regulatory T cells. Endocr Metab Immune Disord Drug Targets. 2011;11:334–46.
Ebert LM, Tan BS, Browning J, Svobodova S, Russell SE, Kirkpatrick N, et al. The regulatory T cell-associated transcription factor FoxP3 is expressed by tumor cells. Cancer Res. 2008;68:3001–9.
Ma GF, Chen SY, Sun ZR, Miao Q, Liu YM, Zeng XQ, et al. FoxP3 inhibits proliferation and induces apoptosis of gastric cancer cells by activating the apoptotic signaling pathway. Biochem Biophys Res Commun. 2013;430:804–9.
Chu R, Vlantis AC, van Hasselt CA, Ng SK. Inhibition of FoxP3 induced apoptosis of thyroid cancer cells. Mol Cell Endocrinol. 2015;399:228–34.
Liang YJ, Liu HC, Su YX, Zhang TH, Chu M, Liang LZ, et al. FoxP3 expressed by tongue squamous cell carcinoma cells correlates with clinicopathologic features and overall survival in tongue squamous cell carcinoma patients. Oral Oncol. 2011;47:566–70.
Hinz S, Pagerols-Raluy L, Oberg HH, Ammerpohl O, Grussel S, Sipos B, et al. FoxP3 expression in pancreatic carcinoma cells as a novel mechanism of immune evasion in cancer. Cancer Res. 2007;67:8344–50.
Niu J, Jiang C, Li C, Liu L, Li K, Jian Z, et al. Foxp3 expression in melanoma cells as a possible mechanism of resistance to immune destruction. Cancer Immunol Immunother. 2011;60:1109–18.
Liang YJ, Lao XM, Liang LZ. Genome-wide analysis of cancer cell-derived FoxP3 target genes in human tongue squamous cell carcinoma cells. Int J Oncol. 2015;46:1935–43.
Schipmann S, Wermker K, Schulze HJ, Kleinheinz J, Brunner G. Cutaneous and oral squamous cell carcinoma-dual immunosuppression via recruitment of FoxP3(+) regulatory T cells and endogenous tumour FoxP3 expression? J Craniomaxillofac Surg. 2014;42:1827–33.
Clara U, Rossella E, Agnese P, Serena P, Cristiana L, Nicla B, et al. FoxP3 expression in papillary thyroid carcinoma: a possible resistance biomarker to iodine 131 treatment. Thyroid. 2014;24:339–46.
Dohan O, De La Vieja A, Paroder V, Riedel C, Artani M, Reed M, et al. Endocr Rev. 2003;24:48–77.
Liu F, Ma XJ, Zhao YY, Wu LN, Zhao YY, Qin GJ. The effect of FoxO1 on the proliferation of rat mesangial cells under high glucose conditions. DNT. 2014;29:1879–87.
Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T). Nat Protoc. 2008;3:1101–8.
Riesco-Eizaguirre G, Rodríguez I, De la Vieja A, Costamagna E, Carrasco N, Nistal M, et al. The BRAFV600E oncogene induces transforming growth factor β secretion leading to sodium iodide symporter repression and increased malignancy in thyroid cancer. Cancer Res. 2009;69:8317–25.
David A, Daniel B, Michael J, Toni B, Alexander J, Veach P, et al. Thyroid stimulating hormone increases iodine uptake by thyroid cancer cells during BRAF silencing. J Surg Res. 2013;182:85–93.
Morari EC, Marcello MA, Guilhen AC, Cunha LL, Latuff P, Soares FA, et al. Use of sodium iodine symporter expression in differentiated thyroid carcinomas. Clin Endocrinol. 2011;75:247–54.
Acknowledgments
This work was supported by grants from the Innovation Scientists and Technicians Troop Construction Projects of Henan Province (No. 134200510021). The authors appreciate the generous help of the Institute of Clinical Medicine (The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China) in providing the necessary facilities, and Jun Ouyang and Jinfa Li from the endocrinology laboratory of The First Affiliated Hospital of Zhengzhou University.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ma, S., Wang, Q., Ma, X. et al. FoxP3 in papillary thyroid carcinoma induces NIS repression through activation of the TGF-β1/Smad signaling pathway. Tumor Biol. 37, 989–998 (2016). https://doi.org/10.1007/s13277-015-3848-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3848-6