Abstract
Pancreatic ductal adenocarcinoma (PDAC) is extremely malignant. Efficient control of cancer growth may substantially improve the survival of PDAC patients. However, no efficient treatments are so far available. Here, we inhibited transforming growth factor β (TGFβ) receptor signaling by overexpression of a key inhibitor of this pathway, SMAD7, in the mouse pancreas, using a recently developed intraductal infusion method. Overexpression of SMAD7 significantly increased growth of both implanted PDAC and PDAC by K-ras modification. Our data thus suggest that TGFβ receptor signaling restrains growth of PDAC, and modulation of TGFβ receptor signaling may be an effective treatment for PDAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is one of the leading lethal cancers worldwide and less than 6 % of the patients survive 5 years after diagnosis [1–3]. Pancreatic ductal adenocarcinoma (PDAC) is the most common type of pancreatic cancer [1–3]. A gene called K-ras has been shown to be the genetic driver of pancreatic cancer initiation and progression, although no therapy directing K-ras mutations has so far been developed [1–3]. Thus, further understanding of the molecular regulation of the tumorigenesis of PDAC appears to be very critical for developing effective therapeutic treatments for PDAC.
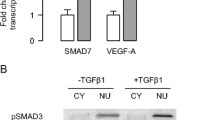
Transforming growth factor β (TGFβ) receptor signaling pathway plays an essential role during various biological processes, including cell proliferation, apoptosis, phenotype modification, and formation of neoplasms [4–6]. When a TGFβ ligand binds to a type II receptor, it catalyzes the phosphorylation of a type I receptor to trigger phosphorylation of intracellular proteins SMAD2 and SMAD3 to form heteromeric complexes with SMAD4. The activated SMAD complexes then translocate to the nucleus, where they regulate the transcription of target genes [4–8]. However, nuclear translocation of phosphorylated SMAD2 and SMAD3 does not require SMAD4, although the proper function of nuclear SMADs depends on the presence of SMAD4 in the SMAD complexes [4–8]. Previous studies have demonstrated a critical role of TGFβ receptor signaling in regulating pancreas organogenesis [9] and pathogenesis of pancreatitis and PDAC [1–3, 10, 11]. However, an analysis of in vivo inhibition of activated TGFβ receptor signaling in PDAC has not been reported.
Here, we show that inhibition of TGFβ receptor signaling by viral-induced expression of a key inhibitor of this pathway, SMAD7, in either implanted PDAC or PDAC developed from genetically modification, significantly enhanced the growth of PDAC in vivo, suggesting that modulation of TGFβ receptor signaling may be an effective treatment for PDAC.
Materials and methods
Cell line culture
PANC-1 has been generated from a human carcinoma of the exocrine pancreas in 1975 [12] and was purchased from American Type Culture Collection (ATCC; Rockville, MD, USA). PANC-1 was cultured in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 20 % fetal bovine serum (Invitrogen, Carlsbad, CA, USA).
Preparation of adeno-associated viruses
The adeno-associated virus (AAV) carrying a recombinant SMAD7 and a GFP reporter under a CAG promoter, AAV carrying a GFP reporter only (AAV-Null), and AAV carrying luciferase and RFP reporter (AAV-luc) were performed as has been previously described [13–15].
Transduction of PANC-1 cells
PANC-1 cells were transduced with AAV-luc to allow in vivo tracing and purification of the transduced cells based on RFP by flow cytometry, respectively.
Animals
All mouse experiments were approved by the Animal Research and Care Committee at Chinese PLA General Hospital. K-ras (G12D) mice [16, 17] and Ptf1a promoter Cre reporter (Ptf1a-Cre) mice [7, 18] were both purchased from the Jackson Labs (Bar Harbor, ME, USA). Ptf1a-Cre mice were bred with K-ras G12D mice to generate Ptf1a-Cre; K-ras G12D mice. NOD/SCID mice were purchased from the Jackson Lab to receive implantation of cancer cells.
In vivo quantification of tumor growth by bioluminescence
Luciferase-carrying PANC-1 cells (PANC-1-Luc, 106) were directly injected into the parenchyma of the pancreas in NOD/SCID mice, as has been described before [19]. The tumor growth was monitored and quantified by luminescence levels after 2 and 6 weeks of the injection. Bioluminescence was measured with the IVIS imaging system (Xenogen Corp., Alameda, CA, USA). All of the images were taken 10 min after intraperitoneal injection of luciferin (Sigma-Aldrich, St. Louis, MO, USA) of 150 mg/kg body weight, as a 60-s acquisition and 10 of binning. During image acquisition, mice were sedated continuously via inhalation of 3 % isoflurane. Image analysis and bioluminescent quantification was performed using Living Image software (Xenogen Corp.). Ten mice were analyzed in each group.
Intraductal infusion
Intraductal infusion was performed as has been previously described [20–22]. Briefly, the duodenum was isolated to expose the common bile duct, after which a microclamp was placed on the common bile duct above the branching of the pancreatic duct. A 31-gauge catheter was then put into the common bile duct through the sphincter of Oddi in the duodenum, which was then clamped with another microclamp to prevent backflow. The other end of the catheter is connected to a micro-infusion apparatus, which delivers 100 μl of AAV-SMAD7 or control AAV-Null via the catheter at a rate of 5 μl/min. Both viruses have GFP reporters. After viral infusion, the hole created by the catheter in the duodenum was closed with 6-gauge suture.
Immunohistochemistry and quantification
All the mice were perfused through the heart with PBS to remove blood cells from the circulation, after which pancreata were isolated and fixed in 4 % formalin for 6 h, followed by cryoprotection in 30 % sucrose overnight before freezing in a longitudinal orientation (from tail to head of the pancreas) and sectioned at 6 μm. HE staining was then performed. The regions for normal pancreas and PDAC were independently decided by two experienced pathologists. The area of PDAC was then divided by the total area of the examined pancreas. In each animal, at least five slides that were 100 μm in distance were analyzed. Quantification was done in ten mice in each condition.
Statistical analysis
All statistical analyses were carried out using the SPSS 17.0 statistical software package. All values are depicted as mean ± standard deviation and are considered significant if p < 0.05. All data were statistically analyzed using one-way ANOVA with a Bonferoni correction, followed by Fisher’s exact text to compare two groups.
Results
Experimental model
For inhibition of TGFβ receptor signaling, we prepared a SMAD7 expressing AAV (Fig. 1a). The virus also contained a GFP reporter (Fig. 1a).
A human PDAC cell line, PANC-1, was used in our study. To trace these cells in vivo, we transduced them with an AAV carrying a luciferase and a RFP reporter, reaching about 65 % of infection efficiency (Fig. 1b). The purification of transduced cells was performed by flow cytometry based on RFP (Fig. 1c, d). Then, these cells were directly injected into the pancreas of NOD/SCID mice. The establishment of the implanted tumor was confirmed by bioluminescence analyses after 2 weeks. Then, we performed an intraductal infusion of AAV-SMAD7, or control AAV-Null viruses, into the pancreas of the tumor-transplanted mice (Fig. 2a). Both viruses contained GFP reporter to allow visualization of the infection by gross imaging at the time of sacrifice (Fig. 2b). We examined the changes in bioluminescence in these mice 4 weeks after viral infusion (Fig. 2a).
Experimental model. a, b Schematic of the model. Luciferase-carrying PANC-1-Luc cells were directly injected into the pancreas of NOD/SCID mice. The establishment of the implanted tumor was confirmed by bioluminescence analyses after 2 weeks. An intraductal infusion of AAV-SMAD7, or control AAV-Null viruses, into the pancreas of the mice was performed (a). Infection can be confirmed by visualization of GFP (b)
Inhibition of TGFβ receptor signaling enhanced growth of the implanted PDAC cells
We found that infusion with AAV-SMAD7 significantly increased the growth of implanted PANC-1 cells in mice, by representative images (Fig. 3b) and by quantification (Fig. 3c), compared to infusion with AAV-Null. These data suggest that inhibition of TGFβ receptor signaling enhanced PDAC cell growth in vivo.
Inhibition of TGFβ receptor signaling enhanced growth of the primary PDAC cells in genetically modified mice
Then, we aimed to examine the effects of inhibition of TGFβ receptor signaling on the growth of primary PDAC cells in vivo. We used an established mouse PDAC model (Ptf1a-Cre; K-ras G12D) (Fig. 4a) [23]. For inhibition of TGFβ receptor signaling in these mice, we also gave the mice at 12 weeks of age an intraductal infusion of AAV-SMAD7, or control AAV-Null viruses, and examined the development of PDAC in these mice by histology after 1 month (Fig. 4b, c). The percentage of the PDAC in these mice was evaluated, showing that the mice that had received AAV-SMAD7 had a significantly higher PDAC area, compared to the mice that had received control AAV-Null virus (Fig. 4d). These data suggest that inhibition of TGFβ receptor signaling enhanced growth of primary PDAC cells from genetically modified mice in vivo.
Inhibition of TGFβ receptor signaling enhanced growth of the primary PDAC cells in genetically modified mice. a Schematic of mouse PDAC model (Ptf1a-Cre; K-ras G12D). b Schematic of the model: at 12 weeks of age, the Ptf1a-Cre; K-ras G12D mice received an intraductal infusion of AAV-SMAD7 or control AAV-Null viruses. The development of PDAC in these mice was examined by histology after 1 month. c Representative HE staining images for normal pancreas and PDAC. d The percentage of the PDAC area in these mice by histology. *p < 0.05. Scale bar is 50 μm
Discussion
PDAC is a highly lethal cancer that affects many humans worldwide. So far, no really effective therapy is available for PDAC. Thus, further elucidation of the molecular regulation of the tumorigenesis of PDAC is substantially important for development of novel strategies for an optimized treatment. Among all the signaling pathways that have been suggested to be involved in the pathogenesis of PDAC, transforming growth factor β (TGFβ) receptor signaling pathway is an important one [10, 11]. Although many studies have demonstrated a role of TGFβ receptor signaling in the progression of PDAC, compelling data to show its direct regulation of tumor growth in vivo are still lacking.
PANC-1 is the most commonly used human PDAC cell line. To trace these cells in vivo, we transduced them with a luciferase reporter, which may allow visualization of the living tumor cells in the living animals by provision of the substrate luciferin. These labeled cells were directly injected into the pancreas of immunodeficient NOD/SCID mice, where they could growth without being rejected as mice of normal immunity. For inhibition of TGFβ receptor signaling, we prepared a SMAD7 expressing AAV. SMAD7 is a specific inhibitor for TGFβ receptor signaling in that it inhibits the activation of the signaling at all levels, like receptor activation, SMAD complex formation, and their nuclear targeting. Then, we used an intraductal infusion method to specifically deliver AAV-SMAD7, or control AAV-Null viruses, into the pancreas of the mice and examined the changes in bioluminescence in these mice after 4 weeks, compared to the bioluminescence level before viral infusion. We found that infusion with AAV-SMAD7 significantly increased the growth of implanted PANC-1 cells in mice, suggesting that inhibition of TGFβ receptor signaling enhanced PDAC cell growth in vivo. Moreover, we found that inhibition of TGFβ receptor signaling enhanced growth of the primary PDAC cells in genetically modified Ptf1a-Cre; K-ras G12D mouse model. Hence, the inhibitory effect of an activated TGFβ receptor signaling exists in both primary PDAC cells and cell line. Also, since the mice with a wild-type background were used in the second study, our data suggest that it is unlikely that inhibitory effect of TGFβ receptor signaling on PDAC growth may require the involvement of leukocytes since NOD/SCID mice had nearly absence of lymphocytes and granulocytes and significantly reduced monocytes/macrophages.
Taken together, our data suggest that TGFβ receptor signaling restrains growth of PDAC, and modulation of TGFβ receptor signaling may be an effective treatment for PDAC.
References
Song W, Li Q, Wang L, Wang L. Modulation of FoxO1 expression by miR-21 to promote growth of pancreatic ductal adenocarcinoma. Cell Physiol Biochem. 2015;35:184–90.
Shi W, Yin J, Chen Z, Chen H, Liu L, Meng Z. Cyr61 promotes growth of pancreatic carcinoma via nuclear exclusion of p27. Tumour Biol. 2014;35:11147–51.
Zhang H, Liu C, Kong Y, Huang H, Wang C, Zhang H. TGFbeta signaling in pancreatic ductal adenocarcinoma. Tumour Biol. 2015;36:1613–8.
Massague J. TGFbeta in cancer. Cell. 2008;134:215–30.
Yi JJ, Barnes AP, Hand R, Polleux F, Ehlers MD. TGF-beta signaling specifies axons during brain development. Cell. 2010;142:144–57.
Naka K, Hoshii T, Muraguchi T, Tadokoro Y, Ooshio T, Kondo Y, et al. TGF-beta-FOXO signalling maintains leukaemia-initiating cells in chronic myeloid leukaemia. Nature. 2010;463:676–80.
Xiao X, Wiersch J, El-Gohary Y, Guo P, Prasadan K, Paredes J, et al. TGFbeta receptor signaling is essential for inflammation-induced but not beta-cell workload-induced beta-cell proliferation. Diabetes. 2013;62:1217–26.
Xiao X, Gaffar I, Guo P, Wiersch J, Fischbach S, Peirish L, et al. M2 macrophages promote beta-cell proliferation by up-regulation of SMAD7. Proc Natl Acad Sci U S A. 2014;111:E1211–20.
El-Gohary Y, Tulachan S, Guo P, Welsh C, Wiersch J, Prasadan K, et al. Smad signaling pathways regulate pancreatic endocrine development. Dev Biol. 2013;378:83–93.
Truty MJ, Urrutia R. Basics of TGF-beta and pancreatic cancer. Pancreatology. 2007;7:423–35.
Muller-Pillasch F, Menke A, Yamaguchi H, Elsasser HP, Bachem M, Adler G, et al. TGFbeta and the extracellular matrix in pancreatitis. Hepatogastroenterology. 1999;46:2751–6.
Lieber M, Mazzetta J, Nelson-Rees W, Kaplan M, Todaro G. Establishment of a continuous tumor-cell line (panc-1) from a human carcinoma of the exocrine pancreas. Int J Cancer. 1975;15:741–7.
Khan IF, Hirata RK, Russell DW. AAV-mediated gene targeting methods for human cells. Nat Protoc. 2011;6:482–501.
Grieger JC, Choi VW, Samulski RJ. Production and characterization of adeno-associated viral vectors. Nat Protoc. 2006;1:1412–28.
Koerber JT, Maheshri N, Kaspar BK, Schaffer DV. Construction of diverse adeno-associated viral libraries for directed evolution of enhanced gene delivery vehicles. Nat Protoc. 2006;1:701–6.
Jackson EL, Willis N, Mercer K, Bronson RT, Crowley D, Montoya R, et al. Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes Dev. 2001;15:3243–8.
Gidekel Friedlander SY, Chu GC, Snyder EL, Girnius N, Dibelius G, Crowley D, et al. Context-dependent transformation of adult pancreatic cells by oncogenic K-Ras. Cancer Cell. 2009;16:379–89.
Kawaguchi Y, Cooper B, Gannon M, Ray M, MacDonald RJ, Wright CV. The role of the transcriptional regulator Ptf1a in converting intestinal to pancreatic progenitors. Nat Genet. 2002;32:128–34.
Cao X, Han ZB, Zhao H, Liu Q. Transplantation of mesenchymal stem cells recruits trophic macrophages to induce pancreatic beta cell regeneration in diabetic mice. Int J Biochem Cell Biol. 2014;53:372–9.
Perides G, van Acker GJ, Laukkarinen JM, Steer ML. Experimental acute biliary pancreatitis induced by retrograde infusion of bile acids into the mouse pancreatic duct. Nat Protoc. 2010;5:335–41.
Jimenez V, Ayuso E, Mallol C, Agudo J, Casellas A, Obach M, et al. In vivo genetic engineering of murine pancreatic beta cells mediated by single-stranded adeno-associated viral vectors of serotypes 6, 8 and 9. Diabetologia. 2011;54:1075–86.
Xiao X, Guo P, Prasadan K, Shiota C, Peirish L, Fischbach S, et al. Pancreatic cell tracing, lineage tagging and targeted genetic manipulations in multiple cell types using pancreatic ductal infusion of adeno-associated viral vectors and/or cell-tagging dyes. Nat Protoc. 2014;9:2719–24.
di Magliano MP, Logsdon CD. Roles for KRAS in pancreatic tumor development and progression. Gastroenterology. 2013;144:1220–9.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
The Publisher and Editor retract this article in accordance with the recommendations of the Committee on Publication Ethics (COPE). After a thorough investigation we have strong reason to believe that the peer review process was compromised.
An erratum to this article is available at http://dx.doi.org/10.1007/s13277-017-5487-6.
About this article
Cite this article
Zhao, Z., Xi, H., Xu, D. et al. RETRACTED ARTICLE: Transforming growth factor β receptor signaling restrains growth of pancreatic carcinoma cells. Tumor Biol. 36, 7711–7716 (2015). https://doi.org/10.1007/s13277-015-3466-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3466-3