Abstract
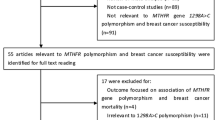
Breast cancer is the most common cancer affecting women in China and the world. Folate supplementation is proven to be effective in reducing the risk of breast cancer or improving its prognosis. Methylenetetrahydrofolate reductase (MTHFR) is an important enzyme involved in folate metabolism and DNA synthesis. This study aims to examine whether single nucleotide polymorphisms (SNP) in the MTHFR gene are associated with risk and survival of breast cancer and serum folate levels in healthy controls. We genotyped nine tagging SNPs in the MTHFR gene in a case–control study, including 560 breast cancer cases and 560 healthy controls in China. We found that TT genotype of rs1801133 had significant increased risk of breast cancer [adjusted odds ratio (OR) = 1.60, 95 % confidence interval (CI) 1.12–2.28] compared with CC genotype, and CC genotype of rs9651118 conferred significant reduced risk of breast cancer (adjusted OR = 0.65, 95 % CI 0.45–0.95) compared to TT genotype. Haplotype analysis also showed that MTHFR CACCAA and AGTCAC haplotypes (rs12121543-rs13306553-rs9651118-rs1801133-rs4846048-rs1801131) had significant reduced risk of breast cancer (adjusted OR = 0.70, 95 % CI 0.58–0.86; adjusted OR = 0.57, 95 % CI 0.40–0.80) compared with CATTAA haplotype. Besides, MTHFR rs9651118 CC genotype was significantly associated with survival in breast cancer cases (adjusted hazard ratio (HR) = 0.63, 95 % CI 0.40–0.99). But none of the SNPs in the MTHFR gene was associated with serum folate level in healthy controls. These findings suggest that variants in the MTHFR gene may influence the risk and prognosis of breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most prevalent cancer affecting women in the world. In China, breast cancer is the most common type of cancer and the sixth leading cause of cancer-related death in women. Based on the estimation of IARC (International Agency for Research on Cancer, GLOBOCAN 2012), about 187,000 new cases of breast cancer were diagnosed annually in women in China, and approximately 48,000 Chinese women died of breast cancer per year [1].
Although the etiological factors of breast cancer are complicated and have not been fully understood yet, there are potential risk factors that may affect the development of breast cancer, including obesity, lack of physical exercise, alcohol consumption, hormone replacement therapy, using oral contraceptives, ever-breastfeeding, and genetic factors [2–4]. It is estimated that approximately 20–25 % of breast cancer cases have a positive family history [5]. High-risk predisposition alleles conferring a 40–85 % lifetime risk of developing breast cancer, including mutations in BRCA1, BRCA2, TP53, PTEN, STK11, etc. [6].
Methylenetetrahydrofolate reductase (MTHFR) is a folate-dependent enzyme that plays an important role in the conversion of homocysteine to methionine by converting 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate. It is a key enzyme in the folate metabolism pathway that can regulate the intracellular folate level, and it is also important for synthesis and methylation of DNA [7]. Studies have proven that specific genetic mutations in the MTHFR gene could lead to change of MTHFR enzyme activity [8]. Molecular epidemiologic studies have also shown that genetic mutations in MTHFR gene may be related to cancers, including breast [9–11]. But most of the studies were focused on the hot spots (C677T and A1298C), and little is known of other mutations in the MTHFR gene and susceptibility to breast cancer in Chinese population.
To help clarify whether the MTHFR variants are associated with susceptibility and prognosis of breast cancer and serum folate levels in healthy controls, we examined nine tagging single nucleotide polymorphisms (SNP) in the MTHFR gene (rs12121543, rs13306561, rs13306553, rs9651118, rs1801133, rs2274976, rs4846048, rs1801131, and rs17037396) in a case–control study in China.
Methods
Study participants
In this study, 560 breast cancer patients were consecutively enrolled in Yueyang Hospital of Integrated Chinese and Western Medicine, Shanghai, China, aged from 35 to 66 years. All patients were pathologically confirmed between June 2009 and June 2014. A total of 560 healthy control subjects were randomly selected from Yueyang Hospital of Integrated Chinese and Western Medicine during the same period and were frequency-matched to the cases by age (5-year age groups). In this study, the response rates of the cases and controls were 90.5 and 88.6 %, respectively. At enrollment, written informed consent and structured questionnaire, including demographic and medical histories, were obtained from each subject by a trained interviewer. Fasting venous blood samples were also collected and then separated into serum, red blood cells, and buffy coat. This study was approved by the Ethics Committee of Yueyang Hospital of Integrated Chinese and Western Medicine.
SNP selection
Tagging SNPs were selected from the HapMap project (www.hapmap.org) by searching Han Chinese data using the following criteria: (a) SNPs located in the gene or within the 2-kb region flanking the gene, (b) with minor allele frequency ≥0.1, and (c) with a linkage disequilibrium of r 2 ≥ 0.90. As a result, a total of nine tag SNPs were identified.
Laboratory tests
Serum levels of folate in healthy controls were determined by chemiluminescent immunoassay using a Beckman Coulter ACCESS Immunoassay System (Beckman Coulter, Krefeld, Germany). The intra-assay and inter-assay coefficients of variation were 3.8 and 6.2 %, respectively.
Genomic DNA was extracted from buffy coat of each subjects using DNA Extraction Kit (Qiagen, Hilden, Germany). Genotyping was performed on the ABI PRISM 7900HT Sequence Detection System (Applied Biosystems, Foster City, CA, USA), using the TaqMan SNP Genotyping Assays. The genotyping call rate was >95 %, and the completion rate was >99 %. For quality control, 5 % of duplicate samples were randomly selected from the whole population and re-genotyped. The concordance rate for the quality control samples was 100 %.
Statistical analysis
We used SAS software (version 9.3; SAS Institute, Inc.) for the statistical analyses. Chi-square statistics and t test were used to evaluate case–control differences in the distribution of risk factors. Hardy–Weinberg equilibrium for genotypic distribution in controls was tested against departure from the Hardy–Weinberg equilibrium (HWE) using a goodness-of-fit chi-square test before analysis. The associations between the SNPs and breast cancer risk were accessed by odds ratios (ORs) and 95 % confidence intervals (CIs) using unconditional logistic regression model. Linkage disequilibrium between loci was assessed by HaploView version 4.0 (Daly Lab at the Broad Institute, Cambridge, MA, USA) [12]. Associations between haplotypes (>1 % frequency) and the risk of breast cancer were evaluated by HAPSTAT [13]. Overall survival time was calculated from the date of cancer diagnosis to the date of death. Univariate and multivariate Cox regression analyses were used to evaluate the effects of the different genotypes on cancer survival. Both univariate ANOVA and multivariate ANCOVA analyses adjusting for age, age at menarche, BMI, and family history of breast cancer were performed to determine the effects of the MTHFR polymorphisms on serum folate levels in healthy controls. P values of less than 0.05 (two-sided probability) were considered as statistically significant.
Results
Characteristics of the cases and controls are shown in Table 1. Cases and controls were evenly matched by age. Cases were more probably to have an earlier age at menarche, higher BMI levels, and more likely to have family history of breast cancer than healthy controls.
The associations between MTHFR variants and risk of breast cancer are presented in Table 2. The genotype distributions of the SNPs among controls showed no deviation from the expected Hardy–Weinberg equilibrium (p > 0.05). TT genotype of rs1801133 conferred significantly elevated risk of breast cancer (OR = 1.62, 95 % CI 1.14–2.30, P = 0.007) compared with CC genotype, and rs9651118 CC genotype conferred significantly reduced cancer risk (OR = 0.68, 95 % CI 0.47–0.99, P = 0.04) compared to TT genotype. These associations remained significant after adjustment for other risk factors (age, age at menarche, BMI, and family history of breast cancer). None of the other SNPs examined was associated with the risk of breast cancer.
Six SNPs in the MTHFR gene (rs12121543, rs13306553, rs9651118, rs1801133, rs4846048, and rs1801131) were in linkage disequilibrium with D′ ranging from 0.89 to 0.99 and r 2 ranging from 0.01 to 0.89 (Fig. 1). Subjects carrying the MTHFR CACCAA and AGTCAC haplotypes had significant reduced risks of breast cancer (OR = 0.71, 95 % CI 0.59–0.87; OR = 0.58, 95 % CI 0.41–0.82) compared with those carrying the CATTAA haplotype (Table 3). This association remained significant after adjustment for other risk factors.
Till June 2014, a total of 105 patients died. When the Cox regression analysis was used, there was one genetic marker significantly associated with breast cancer survival (Table 4). Specifically, cases with the rs9651118 CC genotype had significant decreased risk of death compared with the TT carriers (crude HR = 0.60, 95 % CI 0.38–0.92). To identify independent prognostic factor for breast cancer, we further adjusted for age, age at menarche, BMI, family history of breast cancer, histological grade, ER, RR, and tumor size using multivariate models. The result showed that rs9651118 was an independent prognostic factor for breast cancer survival with adjusted HR of 0.63 (95 % CI 0.40–0.99). None of the other SNPs were associated with survival time.
Finally, we investigated the associations between the MTHFR SNPs and serum folate levels in healthy controls but failed to find any significance (Supplementary Table 1).
Discussion
In this molecular epidemiologic study, mutations in the MTHFR gene were fully studied for their associations with breast cancer risk and prognosis and serum folate levels in healthy controls. We demonstrated that two genetic mutations (rs1801133 and rs9651118) in MTHFR gene were significantly associated with risk of breast cancer, and rs9651118 was significantly associated with prognosis of breast cancer in cases.
MTHFR gene is located on chromosome 1 location p36.3 in humans, and over 40 point genetic mutations in this gene have been identified. Mutations in this gene are associated with methylenetetrahydrofolate reductase deficiency, among which A1298C (rs1801131) and C677T (rs1801133) are the most studied [9]. MTHFR is a key enzyme in folate metabolism and it mainly involves in two important pathways of folate metabolism: one leads to numerous methylation processes that are dependent on S-adenosylmethionine (SAM), and the other, via thymidylate synthesis that contributes to DNA replication and cell division [14]. Reduced MTHFR activity may result in DNA hypomethylation, and a reduced level of MTHFR substrate could lead to uracil misincorporation into DNA, diminished DNA repair and increased frequency of chromosomal breaks and damage. Thus, our finding that genetic variations in MTHFR can influence the susceptibility and prognosis of breast cancer is biologically plausible.
Rs1801133 is a missense mutation (Ala to Val) that locates in exon 8 of MTHFR gene. This genetic change results in approximately 70 and 35 % reduction of normal MTHFR enzyme activity in TT and CT genotype carriers, respectively [15]. Although many studies focused on the association of rs1801133 and breast cancer risk, the results varied. Gao et al. [16] previously investigated MTHFR C677T and A1298C genotypes and breast cancer risk among 669 cases and 682 controls in a Chinese population and found that 667TT genotype conferred increased risk breast cancer (OR = 1.62, 95 % CI = 1.14–2.30). The Shanghai Breast Cancer Study, a population-based case–control study of 1144 breast cancer cases and 1236 controls, failed to find any association between MTHFR C677T and breast cancer risk (TT vs. CC: age-adjusted OR = 0.97, 95 % CI 0.76–1.24), but a significant inverse relationship was observed between folate intake and breast cancer risk [17]. Recently, a meta-analysis, consisted of 22 case–control studies in Chinese population, revealed that MTHFR C677T had a positive relationship with breast cancer (TT vs. CC: OR = 1.18, 95 % CI 1.07–1.29), which was consist with our study results [18]. Besides, our results revealed that breast cancer patients who were carrying 677TT allele had a relatively shorter median survival time than 677CC carriers (10.65 vs. 12.01 months), although it was not statistically significant.
Rs9651118, a mutation in the intron region of MTHFR gene with unknown genetic function, gets less attention than MTHFR C677T and A1298C. To our knowledge, no study has investigated the association between rs9651118 and breast cancer risk or prognosis. It was once reported that C allele of rs9651118 was associated with reduced lung cancer risk in never smokers non-Hispanic white population [19]. Another case–control study of esophageal cancer in Xinjiang (China) also found a decreased cancer risk among C allele carriers than those T allele carriers [20]. In our study, we first found that the mutant allele of this SNP was related to decreased risk of breast cancer and longer survival time among cases. In addition, the haplotype analysis also suggested that six SNPs in MTHFR gene, including rs9651118 and rs1801133, were highly correlated in our study population. The combined effect of these SNPs was in consistent with individual SNPs results.
In conclusion, the present study suggests that MTHFR rs1801133 and rs9651118 were associated with breast cancer risk and MTHFR rs9651118 may affect the prognosis of breast cancer cases.
References
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr, accessed on 09/10/2014
Shah R, Rosso K, Nathanson SD. Pathogenesis, prevention, diagnosis and treatment of breast cancer. World J Clin Oncol. 2014;5:283–98.
Brody JG, Rudel RA, Michels KB, Moysich KB, Bernstein L, Attfield KR, et al. Environmental pollutants, diet, physical activity, body size, and breast cancer: where do we stand in research to identify opportunities for prevention? Cancer. 2007;109:2627–34.
Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J, et al. Risk factors of breast cancer: a systematic review and meta-analysis. Asia Pac J Public Health. 2013;25:368–87.
Rawal R, Bertelsen L, Olsen JH. Cancer incidence in first-degree relatives of a population-based set of cases of early-onset breast cancer. Eur J Cancer. 2006;42:3034–40.
Sharif S, Moran A, Huson SM, Iddenden R, Shenton A, Howard E, et al. Women with neurofibromatosis 1 are at a moderately increased risk of developing breast cancer and should be considered for early screening. J Med Genet. 2007;44:481–4.
Das PM, Singal R. DNA methylation and cancer. J Clin Oncol. 2004;22:4632–42.
Shahzad K, Hai A, Ahmed A, Kizilbash N, Alruwaili J. A structured-based model for the decreased activity of Ala222Val and Glu429Ala methylenetetrahydrofolate reductase (MTHFR) mutants. Bioinformation. 2013;9:929–36.
Izmirli M. A literature review of MTHFR (C677T and A1298C polymorphisms) and cancer risk. Mol Biol Rep. 2013;40:625–37.
Shujuan Y, Jianxing Z, Xin-Yue C. Methylenetetrahydrofolate reductase genetic polymorphisms and esophageal squamous cell carcinoma susceptibility: a meta-analysis of case-control studies. Pak J Med Sci. 2013;29:693–8.
Yu L, Chen J. Association of MTHFR Ala222Val (rs1801133) polymorphism and breast cancer susceptibility: an update meta-analysis based on 51 research studies. Diagn Pathol. 2012;7:171.
Barrett JC, Fry B, Maller J, Daly MJ. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005;21:263–5.
Lin DY, Zeng D, Millikan R. Maximum likelihood estimation of haplotype effects and haplotype-environment interactions in association studies. Genet Epidemiol. 2005;29:299–312.
Nazki FH, Sameer AS, Ganaie BA. Folate: metabolism, genes, polymorphisms and the associated diseases. Gene. 2014;533:11–20.
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995;10:111–3.
Gao CM, Tang JH, Cao HX, Ding JH, Wu JZ, Wang J, et al. MTHFR polymorphisms, dietary folate intake and breast cancer risk in Chinese women. J Hum Genet. 2009;4:414–8.
Shrubsole MJ, Gao YT, Cai Q, Shu XO, Dai Q, Hébert JR, et al. MTHFR polymorphisms, dietary folate intake, and breast cancer risk: results from the Shanghai breast cancer study. Cancer Epidemiol Biomarkers Prev. 2004;13:190–6.
Liang H, Yan Y, Li T, Li R, Li M, Li S, et al. Methylenetetrahydrofolate reductase polymorphisms and breast cancer risk in Chinese population: a meta-analysis of 22 case-control studies. Tumour Biol. 2014;35:1695–701.
Swartz MD, Peterson CB, Lupo PJ, Wu X, Forman MR, Spitz MR, et al. Investigating multiple candidate genes and nutrients in the folate metabolism pathway to detect genetic and nutritional risk factors for lung cancer. PLoS One. 2013;8:e53475.
Chen Y, Ying D, Deng YC AHL, Wang HJ, Ma YQ, et al. Relationship between MTHFR gene polymorphisms and susceptibility of esophageal cancer of Han nationality in Xinjiang. J Toxicol. 2009;23:429–32.
Acknowledgments
This study was supported by the third specialist construction Program of Shanghai Clinical Chinese Medicine (ZYSNXD-YL-YSZK009).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Lu, Q., Jiang, K., Li, Q. et al. Polymorphisms in the MTHFR gene are associated with breast cancer risk and prognosis in a Chinese population. Tumor Biol. 36, 3757–3762 (2015). https://doi.org/10.1007/s13277-014-3016-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-3016-4