Abstract
Activation of the epithelial-to-mesenchymal transition (EMT) endows extraordinary invasive capability of cancer cells and causes of treatment failure and metastasis in gastrointestinal stromal tumor (GIST); however, the molecular mechanisms governing GIST invasion remain largely unknown. MicroRNAs (miRNAs) have been shown to play critical roles in cell motility and invasion, which promotes us to study the biological functions of miR-137 in the EMT of GIST. We have found that miR-137 was dramatically downregulated in clinical specimen of GIST. Using an in silico analysis approach, Twist1, a key regulator gene of EMT, has been identified as the target of miR-137. Quantitative RT-PCT and western blot were used to confirm that miR-137 directly targeted on Twist1 and repressed Twist1 expression in GIST-H1 human gastrointestinal stromal tumor cell line. Further, miR-137 was found to increase expression of E-cadherin and cytokeratin, but suppress expression of N-cadherin and vimentin. In vitro experiments have shown that miR-137 enhanced the epithelial cell morphology, decreased GIST cell migration, activated G1 cell cycle arrest, and induced cell apoptosis. These results suggest a novel mechanism that miR-137 regulates EMT and inhibits cell migration via Twist1 downregulation. Therefore, miR-137 may function as anti-migration and anti-metastasis in GIST and our study provides a potential approach for developing miR-137-based therapeutic strategy for GIST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastrointestinal stromal tumor (GIST) is one of the most common mesenchymal tumors in human gastrointestinal tract and accounts for 1~3 % gastrointestinal malignancies [1, 2]. Recent investigations on the molecular pathogenesis of GIST showed that mutations on two oncogenes of the receptor tyrosine kinase family, KIT, and PDGFRA may contribute to the initiation and progression of GIST [3, 4]. The sustained activation of KIT and PDGFRA in the intestinal cell of Cajal can promote cell proliferation through PI3K-AKT, Src family kinase, Ras-ERK, and JAK-STAT signaling pathways [5, 6]. Although progress in diagnosis and therapies helped to improve the cure of GIST at early stage, the prognosis for patients with advanced GIST and metastasis remains very poor. Up to 30 % of patients still obtained GIST metastasis after the surgical resection [7].
Recently, microRNAs (miRNAs) have been reported to play important roles in tumorigenesis, tumor progression, metastasis, and drug resistance [8–11]. miRNAs are a class of small noncoding RNAs that regulate gene expression by targeting 3′UTR of messenger RNA (mRNA), leading to mRNA degradation and inhibition of protein synthesis [12]. Recently, several groups reported that microRNAs can modulate the expression level of genes which are critical in GIST initiation and progression [13–17]. For example, Kim et al. reported miR-494 downregulates KIT and inhibits proliferation of GIST882 cell line [16]. Fan et al. showed miR-218 also targeted KIT and inhibited the invasion of GIST-T1 cells [4]. These accumulative evidences indicate that miRNAs may serve as a critical layer in modulating GIST progression and metastasis.
Our recent study indicated that epithelial-mesenchymal transition program may play an important role in GIST progression and metastasis [18]. EMT program is an evolutionarily conserved program of gene expression during which epithelial cells obtained characteristics of mesenchymal cells [19]. Activation of EMT endows invasive and metastatic properties upon cancer cells that favor successful colonization of distal target organs [20]. EMT has been shown to play a pivotal role in promoting metastasis in epithelium-derived tumors [21]. Recently, a series of microRNA have been found to be associated with EMT of many other cancers. However, the mechanism of miRNA involvement in the EMT program of GIST remains largely unknown. In the present study, we first identified miR-137 as a critical regulator of EMT in GIST. miR-137 was downregulated in GIST comparing to the normal tissues. By bioinformatics analysis, we validated Twist1 as a bona fide target of miR-137. miR-137 can inhibit GIST metastasis by regulating Twist1 and overexpression of miR-137 in GISTs may be a promising approach to GIST treatment.
Materials and methods
Tissue samples and cell line
The tissue samples were obtained from the GISTs patients who received surgery from 2005 to 2012 at Xiangya Hospital, Central South University. None of the patients had received neoadjuvant chemotherapy before resection [18]. The samples were immediately stored in liquid nitrogen for further analysis. The GIST-H1 cell line was established in our laboratory as previously described [22]. The GIST-H1 cells were cultured in RPMI 1640 media supplemented with 10 % fetal bovine serum and incubated at 37 °C, 5 % CO2, and saturated humidity.
Ethics statement
All tissues were handled and made anonymous according to the ethical and legal standards. This study was conducted with the approval of the Ethics Committee of Xiangya Hospital, China (equivalent to an institutional review board).
RNA isolation and quantitative real-time PCR
Total RNAs from tissue samples and GIST-H1 cells were extracted using TRIzol reagent (Invitrogen). The expression of miR-137 was detected using the TaqMan microRNA assay and the TaqMan Universal PCR Master Mix with U6 as an internal control gene. Reverse transcription PCR was performed with the RevertAid H Minus First Strand cDNA Synthesis Kit (Fermentas). Quantitative real-time PCR was performed with SYBR GreenPCR Master Mix (ABI) on the ABI-7500 platform (ABI), as described previously [23]. qPCR primers were shown as below:
Gene | Forward primer | Reverse primer |
Twist1 | GCCTAGAGTTGCCGACTTATG | TGCGTTTCCTGTTAAGGTAGC |
Slug | TGTGACAAGGAATATGTGAGCC | TGAGCCCTCAGATTTGACCTG |
ZEB1 | CAGCTTGATACCTGTGAATGGG | TATCTGTGGTCGTGTGGGACT |
E-cadherin | CGAGAGCTACACGTTCACGG | CGAGAGCTACACGTTCACGG |
Cytokeratin | TATGGCAACTACTACGGAGGAC | TCCAGGATTCTAAAGGCACCAA |
N-cadherin | TTTGATGGAGGTCTCCTAACACC | ACGTTTAACACGTTGGAAATGTG |
Vimentin | GACGCCATCAACACCGAGTT | CTTTGTCGTTGGTTAGCTGGT |
β-actin | CATTAAGGAGAAGCTGTGCT | GTTGAAGGTAGTTTCGTGGA |
Gene knockdown assay
The cells were infected with shRNA lentiviral pool purchased from GenePharma (Shanghai, China), including TWIST1-homo-782: GCAAGATTCAGACCCTCAAGC; TWIST1-homo-812: GGTACATCGACTTCCTCTACC, and TWIST1-homo-864: GATGGCAAGCTGCAGCTATGT.
Western blot analysis
Western blot analyses were performed by standard methods. Anti-Twist (ab49254) and anti-cytokeratin (ab8068) antibodies were purchased from Abcam. Anti-E-cadherin (sc7870), anti-N-cadherin (sc53488), anti-vimentin (sc53464), and anti-GAPDH (sc365062) antibodies were purchased from Santa Cruz Biotechnology.
Cell cycle and apoptosis
The GIST-H1 cells were transfected with miR-137 mimic and nonspecific control. The blank control group was also established. After transfection for 48 h, the cells were washed with PBS two times and digested with trypsin. After collected, washed, and fixed, the cells were stained with PI dye. Cell cycles of the cells were analyzed using flow cytometry (Beckman-Coulter). In apoptosis assay, Annexin V-FITC was used to detect apoptotic cells according to the manufacturer’s instruction (Millipore). In brief, trypsinized cells were washed two times with PBS and resuspended in binding buffer containing Annexin V-FITC. The cells were incubated at room temperature for 15 min in the dark. Apoptosis of the cells were analyzed using flow cytometry (Beckman-Coulter).
Fluorescent immunohistochemistry
The anti-E-cadherin (#3195) antibody was purchased from Cell Signaling Technology. The anti-vimentin (#m0725) antibody was purchased from Doko. The anti-cytokeratin (#ab82612) and anti-N-cadherin (#ab12221) antibodies were purchased from Abcam. Cells were fixed with 4 % of formaldehyde and permeabilized with 0.3 % of Triton X-100 in PBS at room temperature for 20 min. Samples were blocked with 1 % of goat serum albumin and incubated with appropriate primary antibody at 37 °C for 1 h. After washing extensively, they were incubated with Alexa Fluor-488 anti-mouse IgG (#4408) or Alexa Fluor-488 anti-Rabbit IgG (#4412) or Alexa Fluor-488 anti-Rat IgG (#4416) antibodies (Invitrogen) at 37 °C for 1 h. Counterstaining of nuclei with DAPI (Invitrogen) was also performed. Cells were then washed and mounted for observation under fluorescent microscope.
Wound-healing migration assay
GIST cells were cultured in 6-well plates until confluent and a line in the middle area of the well was scratched using a micropipette tip. The cells were incubated in growth medium for 72 h. At the end, the wounds were photographed using an inverted phase-contrast microscope.
Statistical analysis
All statistical analysis was performed using SPSS version 17.0 software (SPSS Inc.). Comparisons between two groups were performed using the t test, whereas comparisons among three or more groups were performed using one-way ANOVA. Difference was considered significant for a p value <0.05.
Result
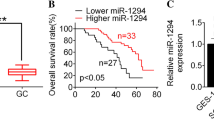
miR-137 was downregulated in primary GIST tissues and cell line
We compared the miRNA expression profiles of the GIST tissues and adjacent tissues by using miRNA microarray chip analysis with ~1,200 mature human miRNAs. Of note, the miR-137 was significantly reduced in GIST tissues by comparing to the adjacent tissues (data not shown). We verified the expression level of miR-137 in 10 GIST tissues and adjacent tissues by quantitative real-time PCR. Consistently, miR-137 was significantly downregulated in GIST tissues by comparing to the adjacent tissues (Fig. 1a). We also examined the expression level of miR-137 in GIST-H1 cell line, a well-established GIST cell line in our laboratory and found miR-137 was significantly reduced in GIST-H1 cell line (Fig. 1b).
miR-137 is downregulated in GIST tissues and cell line. a RNA expression level of miR-137 in GIST tissues and adjacent tissues (Ctrl). ***p < 0.01 between control group and GIST group. b RNA expression level of miR-137 in adjacent tissue and GIST-H1 cell line. The miR-137 level is measured by quantitative RT-PCT and normalized to U6
miR-137 targets Twist1
Since our recent study indicated that EMT is significantly associated with metastasis in GISTs [18], we determined whether miR-137 plays a role in the EMT of GISTs. Using in silico prediction software, we identified a number of potential miR-137 targets. Among the predicted miR-137 targets, one of which is in the 3′UTR region of Twist1, a central regulator of the EMT (Fig. 2a). We confirmed the target element of miR-137 in Twist1 by using luciferase assay (data not shown). The expression level of miR-137 in GIST-T1 cell line was restored by overexpressing miR-137 mimic (Fig. 2b). Overexpression of miR-137 in GIST downregulated the mRNA level of Twist, but unchanged the mRNA level of other EMT regulators, Slug and ZEB1 (Fig. 2c). It indicates that Twist is the only target for miR-137 in regulating the EMT.
miR-137 suppresses Twist1 expression by targeting the 3′UTR. a Illustration of the in silico predicted miR-137 targeting site in the Twist1 3′UTR region. b Establishment of overexpressed miR-137 cell line by transfecting with miR-137 mimic vectors in GIST-H1 cells. c RNA expression level of EMT regulators (Twist, Slug, and ZEB1) in miR-137-overexpressed GIST-H1 cells. The RNA levels of target genes are measured by quantitative RT-PCT
miR-137 regulates EMT by targeting Twist1
By further analysis of the downstream effectors of EMT, we found that both the mRNA level and the protein level of EMT effector genes were regulated by miR-137 in GIST-H1 cells. Overexpression of miR-137 significantly increased the mRNA and protein level of epithelial markers, E-cadherin, and cytokeratin; however, the mRNA and protein level of mesenchymal markers, N-cadherin, and vimentin, were downregulated in miR-137 mimic cells compare to the control (Fig. 3).
miR-137 regulates the EMT effector genes by targeting Twist1. a RNA expression level of EMT effectors (E-cadherin, cytokeratin, N-cadherin, and vimentin) in miR-137-overexpressed GIST-H1 cells. The RNA levels of target genes are measured by quantitative RT-PCT. b Protein expression level of EMT regulator and effectors in miR-137-overexpressed GIST-H1 cells. The protein levels of target genes are measured by western blot. c Quantification of protein levels in the EMT
Overexpressed miR-137 regulates EMT and inhibits the cell motility
EMT genes are known to change the morphology of cancer cells including cell shape, motility, and adhesion [24, 25]. We first examined the roles of miR-137 in cell morphology by fluorescent microscopy. Consistently, overexpression of miR-137 enhanced the expression of E-cadherin and cytokeratin while inhibiting the expression of N-cadherin and vimentin in GIST cells (Fig. 4a). The migration ability of the overexpressed miR-137 was further tested using the wound-healing assay. The wound-healing process was monitored after 72 h after scrape for GIST-H1 cells. Our results clearly showed that the cells with miR-137 mimic vector have a retarded mobility in comparison with other two controls (Fig. 4b, c). These results indicated the anti-migration effect of miR-137 in GIST cells.
miR-137 regulates cell morphology and cell motility in GIST-H1 cells. a GIST-H1 cells were immunostained for EMT effectors (E-cadherin, cytokeratin, N-cadherin, and vimentin) and visualized by fluorescent microscopy. b Wound-healing assay of GIST-H1 cells transfected with either control or the miR-137 mimic overexpression vector. c Quantitative analysis of migration ability by wound-healing assay
Overexpressed miR-137 regulates cell cycle progression and apoptosis
To assess the effect of miR-137 in cell growth in GIST cells, we performed cell cycle assay and apoptosis assay. Cell cycle analyses demonstrated a stronger G1 checkpoint (45.54 vs 34.58 and 35.23 %) when miR-137 was overexpressed in GIST-H1 cells (Fig. 5a). We next examined the effect of miR-137 in GIST cells. Apoptotic cells were quantified and analyzed by Annexin V staining and flow cytometry. miR-137 overexpressed GIST-H1 cells demonstrated much increased apoptosis (10.09 vs 3.23 and 3.27 %) in comparison to the controls (Fig. 5b). These results suggested that miR-137 inhibits cell cycle progression and promotes cell apoptosis in GIST cells.
Discussion
Emerging evidence has shown that miRNAs are able to regulate multiple genes involving in all aspects of cancer biology [26]. Study of these miRNAs would allow us to better understand tumorigenesis by analyzing their targets associated and mediated signaling pathways. Several groups have reported the roles of some specific miRNAs in various pathways in GIST [13, 15, 16, 27, 28]. In the present study, we found miR-137 was one of the differential expressed miRNAs in GIST. miR-137 has shown to be a putative tumor suppressor in several human cancers including breast cancer, lung cancer, ovarian cancer, colorectal cancer, gastric cancer, melanoma, neuroblastoma, and glioblastoma [29–37]. Recently, miR-137 was found to inhibit the stemness of gliomas stem cells by targeting RTVP-1, which promotes the neural differentiation of neural stem cells and cancer stem cells [38]. In our study, we found miR-137 was significantly downregulated in GIST tissues by comparing to the adjacent tissues. The overexpression of miR-137 significantly inhibited GIST cell proliferation and invasion as well as induced G1 cell cycle arrest and apoptosis. Therefore, miR-137 is possible to be developed into a negative biomarker for diagnosis.
Our recent study has shown that the expression levels of EMT genes were significantly associated with metastasis in GISTs [18]. EMT is key developmental program to transdifferentiate of polarized epithelial cells to mesenchymal cells, which is evoked during tumor invasion and metastasis [39, 40]. EMT can also lead to the generation of cancer cells with stem cell-like characteristics, including increased self-renewal and tumor-initiating capabilities and increased resistance to apoptosis and chemotherapy [19, 41]. To determine whether miR-137 played roles in the EMT during GIST metastasis, we used online in silico prediction software to identify target genes of miR-137, interestingly, one of which are included in the critical regulators of EMT. We identified miR-137 directly targets Twist1 by the 3′UTR in the mRNA sequence and further verified the inhibitory effect of miR-137 on Twist gene by quantitative RT-PCR and western blot. Twist genes are the basic helix-loop-helix (bHLH) family of transcription factors, which can induce EMT alone or cooperatively with other regulators [24, 42]. Recent studied have found that Twist1 can not only repress E-cadherin through induction of Snail transcription factor, but also activate programs associated with tumor invasion, thus coordinating two major aspects of the EMT program [24, 43–45]. By targeting Twist, miR-137 regulates several EMT effector genes, including E-cadherin, cytokeratin, N-cadherin, and vimentin. Overexpressed miR-137 in GIST-H1 cells significantly upregulated E-cadherin and cytokeratin, while downregulated N-cadherin and vimentin, promoting GIST cells remain in the epithelial status. These results are consistent with our previous study that low E-cadherin expression was significantly associated with metastasis in GISTs, where miR-137 is significantly downregulated in GIST tissues.
In summary, in this study, we have demonstrated that the endogenous expression of miR-137 was significantly downregulated in the GIST tissues by comparison with adjacent tissues. And bioinformatics analyses have identified Twist1 as the direct target gene of miR-137. MiR-137 regulates the expression level of EMT genes including E-cadherin, cytokeratin, N-cadherin, and vimentin by targeting Twist1. Further in vitro experiments have shown that miR-137 modulated the epithelial cell morphology, reduced GIST migration, initiated G1 cell cycle arrest, and induced apoptosis. Based on these observations and results, treatment with enhanced expression of miR-137 may serve as a promising strategy for GIST.
References
Datar M, Khanna R. Inpatient burden of gastrointestinal stromal tumors in the United States. J Gastroint Oncol. 2012;3:335–41.
Patel S. Exploring novel therapeutic targets in gist: focus on the pi3k/akt/mtor pathway. Curr Oncol Rep. 2013;15:386–95.
Miettinen M, Lasota J. Gastrointestinal stromal tumors—definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch Int J Pathol. 2001;438:1–12.
Rubin BP, Heinrich MC, Corless CL. Gastrointestinal stromal tumour. Lancet. 2007;369:1731–41.
Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med. 2006;130:1466–78.
Lennartsson J, Ronnstrand L. The stem cell factor receptor/c-Kit as a drug target in cancer. Curr Cancer Drug Targets. 2006;6:65–75.
Krajinovic K, Germer CT, Agaimy A, Wunsch PH, Isbert C. Outcome after resection of one hundred gastrointestinal stromal tumors. Dig Surg. 2010;27:313–9.
Calin GA, Sevignani C, Dumitru CD, Hyslop T, Noch E, Yendamuri S, et al. Human microRNA genes are frequently located at fragile sites and genomic regions involved in cancers. Proc Natl Acad Sci U S A. 2004;101:2999–3004.
Volinia S, Calin GA, Liu CG, Ambs S, Cimmino A, Petrocca F, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci U S A. 2006;103:2257–61.
Zhou Y, Wan G, Spizzo R, Ivan C, Mathur R, Hu X, et al. miR-203 induces oxaliplatin resistance in colorectal cancer cells by negatively regulating ATM kinase. Mol Oncol. 2014;8:83–92.
Wan G, Zhang X, Langley RR, Liu Y, Hu X, Han C, et al. DNA-damage-induced nuclear export of precursor microRNAs is regulated by the ATM-AKT pathway. Cell Rep. 2013;3:2100–12.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136:215–33.
Gits CM, van Kuijk PF, Jonkers MB, Boersma AW, van Ijcken WF, Wozniak A, et al. Mir-17-92 and miR-221/222 cluster members target KIT and ETV1 in human gastrointestinal stromal tumours. Br J Cancer. 2013;109:1625–35.
Yamamoto H, Kohashi K, Fujita A, Oda Y. Fascin-1 overexpression and miR-133b downregulation in the progression of gastrointestinal stromal tumor. Mod Pathol Off J U S Can Acad Pathol Inc. 2013;26:563–71.
Niinuma T, Suzuki H, Nojima M, Nosho K, Yamamoto H, Takamaru H, et al. Upregulation of miR-196a and HOTAIR drive malignant character in gastrointestinal stromal tumors. Cancer Res. 2012;72:1126–36.
Kim WK, Park M, Kim YK, Tae YK, Yang HK, Lee JM, et al. MicroRNA-494 downregulates KIT and inhibits gastrointestinal stromal tumor cell proliferation. Clin Cancer Res Off J Am Assoc Cancer Res. 2011;17:7584–94.
Fan R, Zhong J, Zheng S, Wang Z, Xu Y, Li S, et al. MicroRNA-218 inhibits gastrointestinal stromal tumor cell and invasion by targeting KIT. Tumour Biol J Int Soc Oncodevelopmental Biol Med. 2013.
Liu S, Liao G, Ding J, Ye K, Zhang Y, Zeng L, et al. Dysregulated expression of Snail and E-cadherin correlates with gastrointestinal stromal tumor metastasis. Eur J Cancer Prev. 2014.
Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–90.
Tsai JH, Yang J. Epithelial-mesenchymal plasticity in carcinoma metastasis. Genes Dev. 2013;27:2192–206.
Gao D, Vahdat LT, Wong S, Chang JC, Mittal V. Microenvironmental regulation of epithelial-mesenchymal transitions in cancer. Cancer Res. 2012;72:4883–9.
Zhu B, Liao G, Liu S, Huang B, Wu S, Zhou J, et al. Characteristics and establishment of cell lines from human gastrointestinal stromal tumors. Zhong nan da xue xue bao Yi xue ban J Cent South Univ Med Sci. 2010;35:1138–44.
Wan G, Cheuk WK, Chan KM. Differential regulation of zebrafish metallothionein-II (zMT-II) gene transcription in ZFL and SJD cell lines by metal ions. Aquat Toxicol. 2009;91:33–43.
Yang J, Mani SA, Donaher JL, Ramaswamy S, Itzykson RA, Come C, et al. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell. 2004;117:927–39.
Scheel C, Weinberg RA. Phenotypic plasticity and epithelial-mesenchymal transitions in cancer and normal stem cells? Int J Cancer J Int Cancer. 2011;129:2310–4.
Garzon R, Calin GA, Croce CM. MicroRNAs in cancer. Annu Rev Med. 2009;60:167–79.
Song DW, Ryu JY, Kim JO, Kwon EJ, Kim do H. The miR-19a/b family positively regulates cardiomyocyte hypertrophy by targeting atrogin-1 and MuRF-1. Biochem J. 2014;457:151–62.
Kelly L, Bryan K, Kim SY, Janeway KA, Killian JK, Schildhaus HU, et al. Post-transcriptional dysregulation by miRNAs is implicated in the pathogenesis of gastrointestinal stromal tumor [GIST]. PLoS One. 2013;8:e64102.
Bemis LT, Chen R, Amato CM, Classen EH, Robinson SE, Coffey DG, et al. MicroRNA-137 targets microphthalmia-associated transcription factor in melanoma cell lines. Cancer Res. 2008;68:1362–8.
Silber J, Lim DA, Petritsch C, Persson AI, Maunakea AK, Yu M, et al. miR-124 and miR-137 inhibit proliferation of glioblastoma multiforme cells and induce differentiation of brain tumor stem cells. BMC Med. 2008;6:14.
Balaguer F, Link A, Lozano JJ, Cuatrecasas M, Nagasaka T, Boland CR, et al. Epigenetic silencing of miR-137 is an early event in colorectal carcinogenesis. Cancer Res. 2010;70:6609–18.
Chen Q, Chen X, Zhang M, Fan Q, Luo S, Cao X. miR-137 is frequently down-regulated in gastric cancer and is a negative regulator of Cdc42. Dig Dis Sci. 2011;56:2009–16.
Chen L, Wang X, Wang H, Li Y, Yan W, Han L, et al. miR-137 is frequently down-regulated in glioblastoma and is a negative regulator of Cox-2. Eur J Cancer. 2012;48:3104–11.
Zhao Y, Li Y, Lou G, Zhao L, Xu Z, Zhang Y, et al. MiR-137 targets estrogen-related receptor alpha and impairs the proliferative and migratory capacity of breast cancer cells. PLoS One. 2012;7:e39102.
Althoff K, Beckers A, Odersky A, Mestdagh P, Koster J, Bray IM, et al. MiR-137 functions as a tumor suppressor in neuroblastoma by downregulating KDM1A. Int J Cancer J Int Cancer. 2013;133:1064–73.
Guo J, Xia B, Meng F, Lou G. miR-137 suppresses cell growth in ovarian cancer by targeting AEG-1. Biochem Biophys Res Commun. 2013;441:357–63.
Tamim S, Vo DT, Uren PJ, Qiao M, Bindewald E, Kasprzak WK, et al. Genomic analyses reveal broad impact of miR-137 on genes associated with malignant transformation and neuronal differentiation in glioblastoma cells. PLoS One. 2014;9:e85591.
Bier A, Giladi N, Kronfeld N, Lee HK, Cazacu S, Finniss S, et al. MicroRNA-137 is downregulated in glioblastoma and inhibits the stemness of glioma stem cells by targeting RTVP-1. Oncotarget. 2013;4:665–76.
Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119:1420–8.
Polyak K, Weinberg RA. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009;9:265–73.
Dave B, Mittal V, Tan NM, Chang JC. Epithelial-mesenchymal transition, cancer stem cells and treatment resistance. Breast Cancer Res BCR. 2012;14:202.
Fang X, Cai Y, Liu J, Wang Z, Wu Q, Zhang Z, et al. Twist2 contributes to breast cancer progression by promoting an epithelial-mesenchymal transition and cancer stem-like cell self-renewal. Oncogene. 2011;30:4707–20.
Li L, Cserjesi P, Olson EN. Dermo-1: a novel twist-related bHLH protein expressed in the developing dermis. Dev Biol. 1995;172:280–92.
Casas E, Kim J, Bendesky A, Ohno-Machado L, Wolfe CJ, Yang J. Snail2 is an essential mediator of twist1-induced epithelial mesenchymal transition and metastasis. Cancer Res. 2011;71:245–54.
Eckert MA, Lwin TM, Chang AT, Kim J, Danis E, Ohno-Machado L, et al. Twist1-induced invadopodia formation promotes tumor metastasis. Cancer Cell. 2011;19:372–86.
Acknowledgments
This study was supported by Hunan Social Development Support Program (Grant No. 2012SK3190) and Hunan Graduate student research innovation project (Grant No. CX2012B090).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, S., Cui, J., Liao, G. et al. miR-137 regulates epithelial-mesenchymal transition in gastrointestinal stromal tumor. Tumor Biol. 35, 9131–9138 (2014). https://doi.org/10.1007/s13277-014-2177-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2177-5