Abstract
Tumor necrosis factor alpha (TNF-α) is a multifunctional cytokine which plays an important role in the human immune response against various pathogens, and there may be a relationship between TNF-α 308 G/A polymorphism and cervical cancer risk. We performed a meta-analysis to get a systemic assessment of the association between TNF-α 308 G/A polymorphism and cervical cancer risk. Electronic searches of PubMed, Embase, and Web of Science were performed for all publications on the association between TNF-α 308 G/A polymorphism and cervical cancer risk through October 26, 2012. The pooled odds ratios (ORs) with their 95 % confidence interval (95 % CIs) were calculated to assess the association. Fifteen studies with a total of 3,743 cervical cancer cases and 4,096 controls were finally included into the meta-analysis. Overall, TNF-α 308 G/A polymorphism was significantly associated with increased risk of cervical cancer under three main genetic comparison models (A vs. G, OR 1.20, 95 % CI 1.02–1.42, P = 0.03; AA vs. GG, OR 1.31, 95 % CI 1.00–1.72, P = 0.048; AA vs. GG/GA, OR 1.30, 95 % CI 1.00–1.71, P = 0.05). Subgroup analysis by ethnicity further showed that there was a significant association between TNF-α 308 G/A polymorphism and increased risk of cervical cancer in Asians (AA vs. GG, OR 1.83, 95 % CI 1.05–3.20, P = 0.034; AA vs. GG/GA, OR 1.84, 95 % CI 1.05–3.22, P = 0.032). The meta-analysis suggests that TNF-α 308 G/A polymorphism is associated with increased risk of cervical cancer, and TNF-α 308 G/A mutant allele A is a risk factor of cervical cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
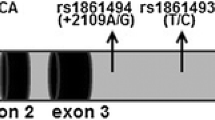
Cervical cancer is third most common cancer in both incidence and mortality in females, accounting for 9 % (529,800) of the total new cancer cases and 8 % (275,100) of the total cancer deaths among females [1]. More than 85 % of these cases and deaths occur in developing countries, which is a major public health threat and heavy burden to the society [1, 2]. It has been well established that human papillomavirus (HPV) infection plays a critical role in the cervical carcinogenesis [3]. However, there are a large number of females who are with HPV infection but never develop cervical cancer, which suggests that genetic factors are also involved in the progression of cervical precancerous lesions to invasive cervical cancer [4–6]. Infection-associated chronic inflammation plays an important role in tumorigenesis of cervical cancer, and tumor necrosis factor alpha (TNF-α) is a key player in both inflammation and tumorigenesis [7–9]. TNF-α is a multifunctional cytokine which plays an important role in the human immune response against various pathogens [10, 11]. There are several common single-nucleotide polymorphisms in the TNF-α gene which can regulate the transcription and production of TNF-α, such as including −238 G/A (rs361525) and −308 G/A (rs1800629) [10, 12]. TNF-α 308 G/A polymorphism is the most studied polymorphism, which is the G to A transition in the promoter at position −308 [13]. Previous studies reported that there was a possible association of the TNF-α 308 G/A polymorphism with cervical cancer, but the findings were conflicting, and it was still unknown whether there was a genetic association between TNF-α 308 G/A polymorphism and cervical cancer risk [14–23]. Therefore, we performed a meta-analysis to get a systemic assessment of the association between TNF-α 308 G/A polymorphism and cervical cancer risk.
Methods
Search strategy
Electronic searches of PubMed, Embase, and Web of Science were performed for all possible publications on the association between TNF-α 308 G/A polymorphism and cervical cancer risk through October 26, 2012. We used the following keywords and subject terms: (“cervical carcinoma,” “cervical cancer,” “cervix carcinoma,” or “cervix cancer,” or cervical neoplasm, cervical lesions, cervical lesion, cervical intraepithelial lesion, cervical intraepithelial lesions, cervical dysplasia, and cervical intraepithelial neoplasia) and (“polymorphism” or “variant” or “genotype” or “mutation”) and (“tumor necrosis factor” or “TNF” or “308 G/A” or “TNF-α” or “rs1800629”). There was no language limitation in the literature search. All eligible studies were retrieved, and their bibliographies were checked for other relevant publications.
Eligible criteria
The following eligible criteria were used to select the included studies: (1) case–control studies, (2) assessing the association between TNF-α 308 G/A polymorphism and cervical cancer risk, and (3) reporting genotype frequencies of TNF-α 308 G/A polymorphism in both cases and controls or providing the odds ratios (ORs) with their 95 % confidence intervals (95 % CIs). If two or more studies reported the same patients populations, only the most recent or complete study was included into this meta-analysis.
Data extraction
The final eligible articles selected for meta-analysis were carefully evaluated independently by two reviewers. Data retrieved from the reports included first author’s name, year of publication, ethnicity of study population (categorized as Caucasians, Asians, and Africans), genotyping method, number of cases and controls, genotype frequencies of TNF-α 308 G/A polymorphism in cases and controls, and the ORs with their 95 % CIs.
Statistical methods
The individual and summary estimates were obtained by calculating the crude ORs with their 95 % CIs and the corresponding P value (the P value being significant if <0.05). The pooled ORs were estimated for the allele model (A vs. G), the codominant model (AA vs. GG), the dominant model (AA+AG vs. GG), and the recessive model (AA vs. AG+GG). Heterogeneity between studies was assessed by calculating the Q-statistic method [24]. The fixed-effects model (Mantel–Haenszel method) was used to calculate the pooled ORs when the P value for Q-statistic was more than 0.10 [25]. Otherwise, the random-effects model (DerSimonian–Laird method) was used to calculate the pooled ORs [26]. Subgroup analysis was also performed by the ethnicity of study population (categorized as Caucasians, Asians, and Africans). Moreover, the funnel plot was employed to assess the possible publication bias. All analyses were conducted using STATA (version 11, StataCorp, College Station, TX), and P values were two sided.
Results
Characteristics of included studies
According to eligibility criteria and exclusion criteria, 15 studies with a total of 3,743 cervical cancer cases and 4,096 controls were finally included into the meta-analysis [14–23, 27–31]. All those 15 studies were all reported in English. The majority of those 15 studies were conducted in Caucasian (eight ones) [15–18, 21, 23, 28, 29] and Asian populations (five ones) [14, 19, 27, 30, 31]. Two of those studies were from African population [20, 22]. Controls in most of those 15 studies were derived from hospital-based participants, and the DNA source for genotype determination of TNF-α 308 G/A polymorphism was mainly from blood samples. The method for testing genotype frequencies of TNF-α 308 G/A polymorphism in both cases and controls was mainly the polymerase chain reaction-restriction fragment length polymorphism method.
Overall analysis
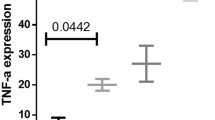
Overall, TNF-α 308 G/A polymorphism was significantly associated with increased risk of cervical cancer under three main genetic comparison models (A vs. G, OR 1.20, 95 % CI 1.02–1.42, P = 0.03; AA vs. GG, OR 1.31, 95 % CI 1.00–1.72, P = 0.048; AA vs. GG/GA, OR 1.30, 95 % CI 1.00–1.71, P = 0.05) (Figs. 1, 2 and 3). However, there was no significant association between TNF-α 308 G/A polymorphism and cervical cancer risk under the dominant model (AA/GA vs. GG, OR 1.16, 95 % CI 0.97–1.39, P = 0.105) (Fig. 4).
Subgroup analysis
In the subgroup analysis of Caucasians, TNF-α 308 G/A polymorphism was not significantly associated with risk of cervical cancer under all four genetic comparison models in Caucasian population (A vs. G, OR 1.12, 95 % CI 0.95–1.33, P = 0.187; AA vs. GG, OR 1.26, 95 % CI 0.91–1.76, P = 0.168; AA vs. GG/GA, OR 1.26, 95 % CI 0.91–1.75, P = 0.17; AA/GA vs. GG, OR 1.09, 95 % CI 0.89–1.32, P = 0.411) when those eight studies from Caucasians were pooled into the meta-analysis.
In the subgroup analysis of Asians, TNF-α 308 G/A polymorphism was also not significantly associated with risk of cervical cancer in Asians under the allele model (A vs. G) and the dominant model (AA + AG vs. GG) (A vs. G, OR 1.47, 95 % CI 0.84–2.57, P = 0.173; AA/GA vs. GG, OR 1.33, 95 % CI 0.75–2.38, P = 0.331) when those five studies from Asians were pooled into the meta-analysis. But, TNF-α 308 G/A polymorphism was significantly associated with increased risk of cervical cancer in Asians under the codominant model (AA vs. GG) and the recessive model (AA vs. AG+GG) (AA vs. GG, OR 1.83, 95 % CI 1.05–3.20, P = 0.034; AA vs. GG/GA, OR 1.84, 95 % CI 1.05–3.22, P = 0.032).
In the subgroup analysis of Africans, TNF-α 308 G/A polymorphism was also not significantly associated with risk of cervical cancer under all four genetic comparison models in Africans (A vs. G, OR 1.19, 95 % CI 0.88–1.62, P = 0.259; AA vs. GG, OR 0.75, 95 % CI 0.31–1.82, P = 0.526; AA vs. GG/GA, OR 0.70, 95 % CI 0.29–1.68, P = 0.421; AA/GA vs. GG, OR 1.33, 95 % CI 0.94–1.88, P = 0.109) when those two studies from Africans were pooled into the meta-analysis.
Publication bias
Funnel plot was conducted to assess the publication bias of the meta-analysis, and the shape of the funnel plots of all genetic comparison models seemed symmetrical. As was shown in the Fig. 5, the funnel plot of the allele comparison model (A vs. G) was symmetrical, which indicated low risk of publication bias in this meta-analysis (Fig. 5).
Discussion
There is no doubt that HPV infection plays a critical role in the cervical carcinogenesis, but previous studies suggest that genetic factors are also involved in the development of invasive cervical cancer [4–6]. TNF-α not only has important roles in the infection-associated chronic inflammation but also has some vital roles in the cell apoptosis, proliferation, invasion, and angiogenesis [10]. Therefore, TNF-α may play important roles in the development of various diseases, such as immunologic, cardiovascular, and metabolic diseases [10, 13]. TNF-α has initially been discovered as an antitumor factor, but it is now considered as a universal effecter of innate signaling implicating its key role in host defense and inflammation. Since accumulating evidence suggests that inflammatory pathways play an essential role in all stages in the tumorigenesis, and it is easy to accept that the TNF-α plays important roles in the in the cervical carcinogenesis [9].
TNF-α 308 G/A polymorphism is one of the most common polymorphisms in the TNF-α gene, and TNF-α 308 G/A polymorphism is associated with the functions of TNF-α in human bodies. This transition has been shown to influence the expression of TNF-α, and a position −308 allele A is associated with an about sixfold increased transcriptional activity and higher levels of TNF-α. Previous studies reported that there was a possible association of the TNF-α 308 G/A polymorphism with cervical cancer, but the findings were conflicting, and it was still unknown whether there was a genetic association between TNF-α 308 G/A polymorphism and cervical cancer risk [14–23]. Therefore, we performed a meta-analysis of 15 studies with a total of 3,743 cervical cancer cases and 4,096 controls. By pooling data from those studies, we found that TNF-α 308 G/A polymorphism was significantly associated with increased risk of cervical cancer under three main genetic comparison models (Figs. 1, 2 and 3). Subgroup analysis by ethnicity further showed that there was a significant association between TNF-α 308 G/A polymorphism and increased risk of cervical cancer in Asians. Therefore, the meta-analysis suggests that TNF-α 308 G/A polymorphism is associated with increased risk of cervical cancer, and TNF-α 308 G/A mutant allele A is a risk factor of cervical cancer.
There is increasing interests in the investigations regarding associations of the TNF-α 308 G/A polymorphism and susceptibility to various kinds of cancers. There are a large number of studies performed to assess those possible associations, but the findings from those studies are inconclusive, which impel the researchers to get a systemic assessment of the associations at a meta-analytical level. Currently, TNF-α 308 G/A polymorphism has been proven to be associated with increased risk of colorectal cancer, gastric cancer, and hepatocellular carcinoma [32–34]. On the contrary, other available studies suggest that there are no obvious associations between TNF-α 308 G/A polymorphism and risk of lung cancer or breast cancer [35, 36]. The finding from current meta-analysis suggests that TNF-α 308 G/A polymorphism is associated with increased risk of cervical cancer, and this finding further suggests the important role of TNF-α in the cervical carcinogenesis.
However, certain limitations in this study had to be acknowledged. First of all, large inter-study heterogeneity was observed, which meant that interpretations of our findings should be undertaken carefully. The obvious heterogeneity may be due to the differences such as ethnicity variations, and different selection criteria of controls. Secondly, there were only two case–control studies published to investigate the association between TNF-α 308 G/A polymorphism and cervical cancer risk in Africans. The limited numbers of eligible studies could cause the relatively small sample size and further resulted in poor validation and increased the risk of random error in the subgroup analysis of Africans. Therefore, more well-designed studies with large sample sizes are needed to further identify the association among Africans. Finally, gene–HPV interactions were not fully addressed in the meta-analysis for the lack of relevant data. Both HPV infection and genetic factors play critical roles in the cervical carcinogenesis, and there is a high possibility of gene–HPV interactions in the association between TNF-α 308 G/A polymorphism and cervical cancer risk. Further studies with large sample size and well designed are needed to assess the possible gene–HPV interactions in the association.
In summary, this meta-analysis suggests that TNF-α 308 G/A polymorphism is associated with increased risk of cervical cancer, and TNF-α 308 G/A mutant allele A is a risk factor of cervical cancer. Besides, further studies with large sample size and well designed are needed to assess the possible gene–HPV interactions in the association.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJ, et al. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378:1461–84.
Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907.
Thomas M, Narayan N, Pim D, Tomaic V, Massimi P, Nagasaka K, et al. Human papillomaviruses, cervical cancer and cell polarity. Oncogene. 2008;27:7018–30.
Ibeanu OA. Molecular pathogenesis of cervical cancer. Cancer Biol Ther. 2011;11:295–306.
de Freitas AC, Gurgel AP, Chagas BS, Coimbra EC, do Amaral CM. Susceptibility to cervical cancer: an overview. Gynecol Oncol. 2012;126:304–11.
Drutskaya MS, Efimov GA, Kruglov AA, Kuprash DV, Nedospasov SA. Tumor necrosis factor, lymphotoxin and cancer. IUBMB Life. 2010;62:283–9.
Aggarwal BB, Gupta SC, Kim JH. Historical perspectives on tumor necrosis factor and its superfamily: 25 years later, a golden journey. Blood. 2012;119:651–65.
Mocellin S, Nitti D. TNF and cancer: the two sides of the coin. Front Biosci. 2008;13:2774–83.
Aukrust P, Sandberg WJ, Otterdal K, Vinge LE, Gullestad L, Yndestad A, et al. Tumor necrosis factor superfamily molecules in acute coronary syndromes. Ann Med. 2011;43:90–103.
Patel R, Cafardi JM, Patel N, Sami N, Cafardi JA. Tumor necrosis factor biologics beyond psoriasis in dermatology. Expert Opin Biol Ther. 2011;11:1341–59.
Mekinian A, Tamouza R, Pavy S, Gestermann N, Ittah M, Mariette X, et al. Functional study of TNF-alpha promoter polymorphisms: literature review and meta-analysis. Eur Cytokine Netw. 2011;22:88–102.
Qidwai T, Khan F. Tumour necrosis factor gene polymorphism and disease prevalence. Scand J Immunol. 2011;74:522–47.
Wang N, Yin D, Zhang S, Wei H, Wang S, Zhang Y, et al. TNF-alpha rs1800629 polymorphism is not associated with HPV infection or cervical cancer in the Chinese population. PLoS One. 2012;7:e45246.
Barbisan G, Perez LO, Contreras A, Golijow CD. TNF-alpha and IL-10 promoter polymorphisms, HPV infection, and cervical cancer risk. Tumour Biol. 2012;33:1549–56.
Badano I, Stietz SM, Schurr TG, Picconi AM, Fekete D, Quintero IM, et al. Analysis of TNFalpha promoter SNPs and the risk of cervical cancer in urban populations of Posadas (Misiones, Argentina). J Clin Virol. 2012;53:54–9.
Ivansson EL, Juko-Pecirep I, Gyllensten UB. Interaction of immunological genes on chromosome 2q33 and IFNG in susceptibility to cervical cancer. Gynecol Oncol. 2010;116:544–8.
Wang SS, Bratti MC, Rodriguez AC, Herrero R, Burk RD, Porras C, et al. Common variants in immune and DNA repair genes and risk for human papillomavirus persistence and progression to cervical cancer. J Infect Dis. 2009;199:20–30.
Kohaar I, Thakur N, Salhan S, Batra S, Singh V, Sharma A, et al. TNFalpha-308 G/A polymorphism as a risk factor for HPV associated cervical cancer in Indian population. Cell Oncol. 2007;29:249–56.
Govan VA, Constant D, Hoffman M, Williamson AL. The allelic distribution of -308 tumor necrosis factor-alpha gene polymorphism in south African women with cervical cancer and control women. BMC Cancer. 2006;6:24.
Duarte I, Santos A, Sousa H, Catarino R, Pinto D, Matos A, et al. G-308A TNF-alpha polymorphism is associated with an increased risk of invasive cervical cancer. Biochem Biophys Res Commun. 2005;334:588–92.
Stanczuk GA, Sibanda EN, Tswana SA, Bergstrom S. Polymorphism at the -308-promoter position of the tumor necrosis factor-alpha (TNF-alpha) gene and cervical cancer. Int J Gynecol Cancer. 2003;13:148–53.
Gostout BS, Poland GA, Calhoun ES, Sohni YR, Giuntoli 2nd RL, McGovern RM, et al. TAP1, TAP2, and HLA-DR2 alleles are predictors of cervical cancer risk. Gynecol Oncol. 2003;88:326–32.
Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:101–29.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Jang WH, Yang YI, Yea SS, Lee YJ, Chun JH, Kim HI, et al. The -238 tumor necrosis factor-alpha promoter polymorphism is associated with decreased susceptibility to cancers. Cancer Lett. 2001;166:41–6.
Calhoun ES, McGovern RM, Janney CA, Cerhan JR, Iturria SJ, Smith DI, et al. Host genetic polymorphism analysis in cervical cancer. Clin Chem. 2002;48:1218–24.
Deshpande A, Nolan JP, White PS, Valdez YE, Hunt WC, Peyton CL, et al. TNF-alpha promoter polymorphisms and susceptibility to human papillomavirus 16-associated cervical cancer. J Infect Dis. 2005;191:969–76.
Singh H, Jain M, Sachan R, Mittal B. Association of TNFα (-308 G > A) and IL-10 (-819C > T) promoter polymorphisms with risk of cervical cancer. Int J Gynecol Cancer. 2009;19:1190–4.
Wang Q, Zhang C, Walayat S, Chen HW, Wang Y. Association between cytokine gene polymorphisms and cervical cancer in a Chinese population. Eur J Obstet Gynecol Reprod Biol. 2011;158:330–3.
Gorouhi F, Islami F, Bahrami H, Kamangar F. Tumour-necrosis factor-α polymorphisms and gastric cancer risk: a meta-analysis. Br J Cancer. 2008;98:1443–51.
Fan W, Maoqing W, Wangyang C, Fulan H, Dandan L, Jiaojiao R, et al. Relationship between the polymorphism of tumor necrosis factor-alpha-308 G > A and susceptibility to inflammatory bowel diseases and colorectal cancer: a meta-analysis. Eur J Hum Genet. 2011;19:432–7.
Yang Y, Luo C, Feng R, Bi S. The TNF-alpha, IL-1B and IL-10 polymorphisms and risk for hepatocellular carcinoma: a meta-analysis. J Cancer Res Clin Oncol. 2011;137:947–52.
Wang J, Cao C, Luo H, Xiong S, Xu Y, Xiong W. Tumour necrosis factor alpha -308 G/A polymorphism and risk of the four most frequent cancers: a meta-analysis. Int J Immunogenet. 2011;38:311–20.
Peng WJ, He Q, Yang JX, Wang BX, Lu MM, Wang S, et al. Meta-analysis of association between cytokine gene polymorphisms and lung cancer risk. Mol Biol Rep. 2012;39:5187–94.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, HL., Zhang, YJ. A systemic assessment of the association between tumor necrosis factor alpha 308 G/A polymorphism and risk of cervical cancer. Tumor Biol. 34, 1659–1665 (2013). https://doi.org/10.1007/s13277-013-0699-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-013-0699-x