Abstract
Although the implication of genetic factors in cervical cancer development remains to be elucidated, accumulative epidemiological evidence suggests that polymorphisms of cytokine genes may be involved in the etiology of cervical carcinoma. Tumor necrosis factor alpha (TNF-α) and interleukin-10 (IL-10) are two multifunctional cytokines implicated in inflammation, immunity, and cellular organization, and were proposed to play important roles in cancer biology. In order to determine whether IL-10 -1082 (G/A) and TNF-α -238 (G/A) and -308 (G/A) polymorphisms are associated with susceptibility to cervical cancer, a case–control study of 122 cancer patients and 176 healthy controls was conducted. Cervical samples were genotyped for both TNF-α polymorphisms by PCR-RFLP assay. SNP-1082 from IL-10 gene was genotyped using pyrosequencing technology. The association between cervical cancer risk and the studied SNPs was evaluated by logistic regression. Under univariate analysis, none of these polymorphisms appeared associated with susceptibility of cervical cancer development or HPV infection. However, individuals carrying heterozygous genotype for TNF-α -238 polymorphism seem to be at lower risk for cervical cancer development, with borderline significance (OR = 0.42, P = 0.069), as well as those carrying heterozygous genotypes for IL-10 and TNF-α -238 (OR = 0.40, P = 0.08). In conclusion, these results suggest a potential effect of TNF-α -238 G/A in the reduction of cervical cancer risk in Argentine women, but not TNF-α -308 or IL-10. Larger studies are needed to fully understand the genetic predisposition for the development of cervical cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is the second most common cancer among women, with about 500,000 new cases and 250,000 deaths each year worldwide [1]. Moreover, in developing countries cervical cancer is the main cancer affecting women, representing 80 % of total cervical cancer cases worldwide [2].
Invasive cervical cancer arises as the result of a combination between host and environmental factors, where persistent infection with high-risk human papilloma virus (HPV) plays a key role in the development and progression of cervical intraepithelial neoplasia and squamous cell carcinoma of the cervix [3]. Most genital HPV infections regress within 2 years, and only a minority of women develop persistent HPV infection that could eventually cause cervical intraepithelial neoplasia (CIN). Consequently, it is expectable that host genetic differences influencing the host response against viral infection may determine those people who are at highest risk for developing cervical lesions and progressing to invasive carcinoma. In this way, genetic polymorphisms present in genes related to viral infection, immune response, DNA repair systems, and tumor suppressor genes may influence and determine the excessive risk to develop cervical cancer [4, 5].
Chronic inflammation has been shown to be an important risk factor for a variety of epithelial cancers. In cervical cancer, a number of previous reports suggested that chronic inflammation is associated with precancerous and cancerous lesions. Cytokines, as the products of host response to inflammation, play an important role in the defense against viral infections, modulating viral replication and polarizing the immune response to a Th1 (cellular) or Th2 (humoral) pattern [6]. Th1 cells are immuno-stimulatory and are associated with the clearance of HPV infection and regression of CIN; Th2 cells are immuno-inhibitory and are capable of stimulating tumor growth [7, 8]. It has been observed that a pronounced shift from a Th1 (proinflammatory) cytokine production to Th2 (anti-inflammatory) cytokine production has occurred in CIN patients with extensive HPV infection [8], suggesting that the cytokine response to HPV infection may be influential in determining disease outcome. In addition, there is evidence that reduced Th1 [9] and increased Th2 [10] cytokine levels are associated with poor prognosis in cervical cancer.
Tumor necrosis factor alpha (TNF-α) and interleukin-10 (IL-10) are two multifunctional cytokines. TNF-α is a Th1 proinflammatory cytokine, predominantly secreted by monocytes/macrophages, involved in inflammation, immunity, and cellular organization. It has effects on several functions, including endothelial function, coagulation, lipids, and insulin [11, 12].The specific role of TNF-α in cancer progression remains to be solved, given that different results with several tumor types have shown that this proinflammatory cytokine may present both tumor necrotic [13] and tumor-promoting behavior [14].
Single base polymorphisms occur within the promoter region of TNF-α gene, appearing to be biologically important. The G to A transition at position -308 of the TNF-α gene increases in vitro transcription [15, 16] and may affect disease susceptibility. A second G to A transition at position -238 is associated with various diseases, including endometrial carcinoma [17, 18] but has not been directly linked with in vitro protein expression. Although the regulated release of TNF may exert normal physiologic effects, the uncontrolled production of TNF may lead to organ dysfunction and death [19]. It was also demonstrated that blood level of TNF-α is increased in solid tumors [20].
As a Th2-cytokine with both immunosuppressive and antiangiogenic functions, IL-10 may have both tumor-promoting and tumor-inhibiting properties. It has been reported that several important polymorphic sites in the IL-10 gene, including three in the promoter region (-1082 A/G, -819 T/C, and -592 A/C) may influence the transcription levels of IL-10 messenger RNA and the expression of IL-10 protein in vitro [21] and consequently play a role in susceptibility to cancer [22]. In particular, the association of IL-10 -1082 alleles G and A with low (AA), high (GG), and medium (GA) cytokine production were shown in vitro and in vivo [21].
In the present study, a genetic analysis of SNPs located in the promoter regions of TNF-α (-308 G/A and -238 G/A) and IL-10 (-1082 G/A) genes was undertaken in a series of cervical carcinoma and normal cervical samples obtained from Argentine women in order to assess the effect of these polymorphisms in the development of squamous cervical cancer.
Materials and methods
A total of 298 cervical samples obtained from an anonymous cervical specimen data bank in La Plata, Argentina were used in this study. Samples were obtained considering all bioethical issues, and the study design was evaluated and approved by the committee from the Faculty of Medicine, National University of La Plata, Argentina, as part of a thesis plan. The normal cytologies (obtained from women attending screening) comprised 176 samples; meanwhile 122 samples corresponded to histologically diagnosed squamous cervical carcinomas. The mean age for the control group was 37 years old (SD ± 11) and 44 years old (SD ± 11) for the case group. Cervical specimens include exfoliated cells from the ecto-endocervix, freshly frozen tissue biopsies, and formalin-fixed and paraffin-embedded tissue biopsies.
DNA extraction
Paraffin-embedded samples were washed twice with xylol and finally with 100 % ethanol, resuspended in 250 μl of digestion buffer (50 mM Tris–ClH pH 8.5; 1 mM EDTA; 1 % Triton X100; and 0.5 % Tween 20) with 250 mg/ml proteinase K (Genbiotech, Buenos Aires, Argentina) and incubated for 24 h at 56 °C. Cervical exfoliated cell pellets and freshly frozen biopsies were suspended and washed twice with 1 ml of PBS and incubated for 24 h at 56 °C in 400 of digestion buffer (50 mM Tris–ClH pH 8.5; 1 mM EDTA; 1 % Triton X100; and 0.5 % Tween 20) containing 250 mg/ml of proteinase K (Genbiotech, Buenos Aires, Argentina). After protease digestion, all samples were kept for 10 min at 100 °C for enzyme inactivation. DNA purification was done by the salting-out procedure as described by Miller [23]. Finally, the DNA was suspended in distillate water at a final concentration of 1 ng/μl and stored at 20 °C until used.
Human papillomavirus DNA detection and genotyping
Human papillomavirus DNA was detected in cervical tissues using a nested PCR approach with MY09/11 as external primers and GP5+/6+ as internal ones according to the methods previously described by Ting and Manos [24] and Evander et al. [25]. These two primer pairs are the most widely used for the detection of genital HPVs. A negative control containing only digestion buffer was included every five samples in order to prevent and detect carry-over between samples. After an initial amplification with the primers My9 and My11, 5 μl of the amplicon was subjected to a second nested PCR reaction. This nested PCR was performed using the Gp5+ primer and a 5′ biotynilated Gp6+ oligonucleotide. The biotynilated amplicons were analyzed in 2 % agarose gels stained with Safer Green™ and visualized using a blue light transilluminator (450 nm).
For HPV genotyping, an enzyme immuno assay (EIA) procedure was performed using the biotynilated PCR product. The PCR–EIA assay was done according to the method described by Söderlund-Strand et al. [26], with some modifications. Briefly, 5 μl of the amplicons was captured on streptavidin-coated Maxi Sorp wells (Nunc, Thermo Fisher Scientific, Rochester, NY, USA). The biotynilated Gp was denatured with OHNa, washed three times with wash solution (SSC 0.25X, 20 % Tween-20) and hybridized with 5′fluorescein-labeled oligoprobes corresponding to HPV-6, -11, -16, -18, -31, -33, -35, -39, -45, -51, -52, -56, -58, and -66. Hybridization was carried out at 60 °C for 20 min, using 5 pmol of each probe in a final volume of 100 μl of hybridization solution (5X SSC, 20 % Tween 20). After hybridization, the wells were washed three times with 300 μl of wash solution at room temperature. After the washing steps, samples were incubated for 30 min with an antifluorescein monoclonal antibody (Millipore, MA, USA). After two additional washings, the reactions were revealed using 1-Step™ Turbo TMB-ELISA (Pierce Biotechnology, Rockford, IL, USA). The color reaction was stopped after 10 min of development with 100 μl of 1 M sulfuric acid and read in a microplate reader using a 404-nm filter.
TNF-α and IL-10 fragment amplification
PCR oligonucleotides for polymorphisms amplification were designed according to the human TNF-α and IL-10 genes sequences rs1800629 (TNF-308), rs361525 (TNF-238), and rs1800896 (IL-10 1082) using the software FastPCR™ version 5.4.6. (University of Helsinsky, Finland).
The PCR oligonucleotides for the TNF-α -238 polymorphism were 5′-GAA GAC CCC CCT CGG AAC C-3′ and 5′-GTA GTG GGC CCT GCA CCT TCT G-3′ for forward and reverse primers, respectively. There were two mismatched positions on the forward primer. The first one corresponded to the -244 SNP, and the second one created a cutting site for MspI enzyme (Genbiotech, Argentina). Primers defined a region of 137 base pairs. The reaction mixture was performed in a final volume of 25 μl: 5 μl of genomic DNA; 0.5 pmol/μl of each primer; 0.2 mM of each deoxynucleoside triphosphate; PCR buffer 1X (50 mM KCl and 10 mM Tris–HCl at pH 8.3) and 0.1 % Triton X-100; 1.5 mM of MgCl2; and 0.75 u of Taq DNA polymerase. The amplification reaction was carried out under the following conditions: an initial melting step of 92 °C for 3 min followed by 35 cycles of 30 min at 92 °C, 40 min at 62 °C, and 40 min at 72 °C, with a final elongation step of 72 °C for 5 min.
The primers for TNF-α -308 amplification were 5′-AAA AGA AAT GGA GGC AAT AGG TTT TGA GGG GCC TG-3′ and 5′-CTT CTG GGC CAC TGA CTG ATT TGT GTG TAG GAC AC -3′ for forward and reverse primers, respectively. The mismatched position on the forward primer created a cutting site for BstNI enzyme (Genbiotech, Argentina).This pair of primers defined a 90-base pairs fragment. The PCR reaction mixture (25 μl) consisted of 5 μl of genomic DNA, 0.75 pmol/μl of each primer, 0.2 mM of deoxynucleotide triphosphate, 1X PCR buffer (50 mM KCl and 10 mM Tris-HCl, pH 8.3), 1.35 mM MgCl2, and 0.75 u of Taq polymerase . The conditions for the amplification reaction included an initial melting step of 92 °C for 3 min followed by 35 cycles of 30 min at 92 °C, 40 min at 65 °C, and 30 min at 72 °C, and a final extension step of 72 °C for 5 min.
The forward and reverse oligonucleotides for IL-10 amplification were 5′-GAG CAA CAC TCC TCG CCG CAA-3′ (IL-10 PiroFBiotin) and 5′-TGG AGG CTG GAT AGG AGG TCC CTT AC-3′ (IL-10 PiroR), respectively. This pair of primers defined a fragment of 176 bp. The reaction mixture was performed in a final volume of 50 μl containing 5 μl of genomic DNA; 0.31 pmol/μl of each primer; 0.14 mM of each deoxynucleoside triphosphate; PCR buffer 1X (50 mM KCl and 10 mM Tris–HCl, pH 8.3) and 0.1 % Triton X-100; 1 mM of MgCl2; and 1 u of Taq DNA polymerase. The amplification reaction for IL-10 was carried out using an initial denaturing step of 92 °C for 3 min followed by 35 cycles of 30 min at 92 °C, 15 min at 64 °C, and 15 min at 72 °C with a final elongation step of 72 °C for 5 min. The PCR products for both genes were verified on 2 % agarose gels, stained with Safer Green™, and visualized using the Safe Imager ™ (Invitrogen, USA).
SNPs genotyping
Genotyping of both polymorphisms of TNF-α gene was assessed by restriction enzyme digestion. PCR products were digested overnight at 37 °C with 5 u per sample of MspI and BstNI for TNF-α -238 and -308 polymorphims, respectively. The obtained fragments were resolved on 10 % poliacrylamide gels, stained with Sybr Safe ™, and visualized with blue light. The homozygous TNF-α -238 A allele yields a unique 137-bp band while the homozygous for the G allele yields two bands of 118 and 19 bp. The heterozygous AG genotype is determined by the presence of 137, 118, and 19 bp bands although 19 bp is too small to be clearly appreciated in the gel. On the other hand, TNF-α -308 digestion yields 55 and 35 bp bands for the homozygous GG genotype, while the homozygous A allele generates a unique 90-bp band. The heterozygous AG genotype is determined by the presence of three bands at 90, 55, and 35 bp. In order to avoid misclassification, a randomly selected subset of 20 % of the samples was redigested for genotype confirmation.
SNP-1082 from IL-10 gene was genotyped using Pyrosequencing TM technology on a Biotage PSQ 96MA Pyrosequencer. The relative levels of each allele for the analyzed SNP were evaluated with the PSQ96MA SNP analysis software (Biotage AB, Uppsala, Sweden).
Briefly, pyrosequencing was performed in a volume of 50 μl, at 25 °C. Twenty microliters of biotinylated PCR products was resuspended in binding buffer, captured on streptavidin-coated beads, denaturated, and prepared for pyrosequencing using the recommended protocol for the vacuum prep tool (Biotage AB, Uppsala, Sweden). For each reaction, purified PCR products were incorporated in 45 μl of annealing buffer containing 0.3 μM of sequencing primer (5′-TATCCCTACTTCCCC-3′). Single-stranded DNA with annealed sequencing primer was added to the pyrosequencing reaction mixture containing 10 u of exonuclease-deficient (exo-) Klenow DNA polymerase (Amersham Pharmacia Biotech, Uppsala, Sweden), 40 mU of apyrase (Sigma Chemical Co., St. Louis, MO), 4 μg of purified luciferase/ml (BioThema, Dalaro, Sweden), 15 mU of recombinant ATP sulfurylase, 0.1 M Tris–acetate (pH 7.75), 0.5 mM EDTA, 5 mM Mg–acetate, 0.1 % (w/v) bovine serum albumin (BioThema), 1 mM dithiothreitol, 10 μM adenosine 5′-phosphosulfate, 0.4 mg of poly(vinylpyrrolidone)/ml, and 100 μg of d-luciferin/ml (BioThema). The sequencing procedure was carried out by stepwise elongation of the primer strand upon sequential addition of the different deoxynucleoside triphosphates. Degradation of excess nucleotides by apyrase was carried out simultaneously.
Statistical analysis
Descriptive statistics were analyzed using the SPSS™ software version 15.0. Pearson's chi-square test was conducted to examine the Hardy–Weinberg equilibrium and the independence of genotype frequencies between cases and controls. In order to determine the polymorphisms risk estimation, unconditional logistic regression was used to calculate crude and age adjusted odd ratios (ORs) and their relative 95 % confidence intervals. Finally, potential interaction between polymorphisms was also examined using logistic regression considering two variables (polymorphisms) at a time. Significant associations were defined by a P value below 0.05 in all cases.
Results
In this study, IL-10 -1082 and TNF-α -238 and -308 polymorphisms were successfully genotyped in all samples. The specimens were also tested for the presence of human papillomavirus (HPV) infection. In the control group, the prevalence of HPV infection was 39 %. Among the cervical carcinomas specimens, 80. 3 % appeared as HPV-DNA positive. Whereas high-risk HPV-DNA was found in 73 % of the control group infected samples and 84.3 % of the case group infected samples, the remaining infected samples were positive for low-risk HPV genotypes. The HPV-16 was found more frequently than other viral genotype, comprising 50.7 and 71.8 % of the analyzed infected samples in the control and case groups, respectively. Multiple infections were less frequent than single infection. Table 1 shows details on HPV type-specific frequencies.
Allele frequencies of TNF-α -308 G > A, TNF-α -238 G > A, and IL-10 -1082 G > A polymorphisms were uniformly distributed among cases and controls, showing no statistically significant differences (P > 0.05). Table 2 shows allele distributions of these three SNPs.
The observed genotype distributions did not deviate from those predicted by the Hardy–Weinberg equilibrium. Table 3 shows the genotype frequencies of IL-10 and both TNF-α polymorphisms in women with cervical carcinoma and control subjects. No significant differences were found between cases patients and control subjects (P > 0.05). In addition, when grouping the population considering individuals as being carriers or not carriers of a specific allele, no differences were found between patients and control subjects (P > 0.05).
Moreover, TNF-α and IL-10 genotypes were uniformly distributed among HPV-positive and HPV-negative women in the control group (P > 0.05). In addition, no significant association was found between these polymorphisms and high-risk HPV infection in the control group. In this sense, none of the studied polymorphisms was found to provide a higher risk of virus infection.
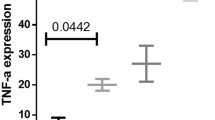
Conversely, TNF-α -238 showed a higher prevalence of women carrying heterozygous AG genotype in controls (15.3 %) than in cases (7.4 %), resulting in an odds ratio of 0.42 when compared to homozygous GG genotype. However, this result did not reach statistical significance (P = 0.069).
Polymorphisms interaction
All potential combinations of polymorphisms were assessed for cervical cancer risk. A codominant model (three-level variable) was hypothesized for a two factor analysis of interaction (TNF-α -238/TNF-α -308; TNF-α -238/IL-10; and TNF-α -308/IL-10). The odds ratios for cervical cancer in a specific polymorphism did not differ significantly within genotypes of other markers (P > 0.05), indicating that no interaction between genes was detected. However, individuals carrying both heterozygous genotypes for IL-10 -1082 and TNF-α -238 showed a trend toward protective effect for cervical cancer (OR = 0.40, IC = 0.14–1.13, and P = 0.08) when compared to those carrying IL-10-1082 AA/TNF-α -238 GG genotypes.
Discussion
A number of genetic polymorphisms have been associated with increased risk for cervical cancer. In this study, the impact of IL-10 and TNF-α polymorphisms was evaluated in 298 samples corresponding to 122 cervical cancer cases and 176 healthy tissues obtained from white Argentine women. Under univariate analysis, none of these polymorphisms appeared associated with susceptibility of cervical cancer development or HPV infection. However, individuals heterozygous for TNF-α -238 polymorphism seem to be at lower risk for cervical cancer development, with borderline significance, as well as those carrying heterozygous genotypes for IL-10 and TNF-α -238. Moreover, this is the first study performed in the Argentine population of La Plata analyzing the association between polymorphisms within the promoter region of TNF-α (-308 G/A, -238 G/A) and IL-10 (-1082 G/A) genes and the development of cervical carcinoma.
Experimental studies have shown the importance of functional polymorphisms occurring in cytokine genes [27, 28]. In this sense, Wilson et al. [16] indicated that the rare allele TNF-α -308 A (TNF2) carries a sevenfold increased risk of death from malaria, and it is a much stronger transcriptional activator than TNF1 (TNF-α -308 G). In addition, Kroeger et al. [15] found that TNF-α -308 A allele binds differently to a nuclear transcription protein giving rise to a twofold increase in the level of transcription of the TNF-α gene in PMA-induced immortalized T cells. Since then, several studies have explored the relationship between this polymorphism and cancer susceptibility. Regarding cervical disease, Kirkpatrick et al. [29] reported that the frequency of the TNF-α -308 low-secretor genotype was significantly increased among all categories of SIL patients, particularly in those presenting LG-SIL.
In a recent meta-analysis, Liu et al. [30] pooled data from 12 case–control studies and observed that TNF-α -308 AA genotype caused a slightly increased overall susceptibility to cervical cancer (OR = 1.39). After stratified by ethnicity, the association between TNF-α -308 AA genotype and risk of cervical cancer was higher in Asians. On the other hand, subjects with African ethnicity carrying TNF-α -308 AA genotype showed some protection against cervical cancer development, while no significant association was observed among Caucasian women. The authors concluded that discordant effects of homozygous AA genotype among different populations may arise from different genetic backgrounds, as indicated by the difference of A allele frequency in controls [30]. In a recent study, Badano et al. [31] evaluated the potential role of TNF-α promoter SNPs in cervical cancer in a population from Posadas, Argentina. They reported that the frequency of the TNF-α -308 high-secretor A allele was significantly associated with an increased risk for cervical cancer development. In our study, allele frequencies for TNF-α -308 polymorphism differed from that reported by Badano et al. [31], and the lack of association between TNF-α -308 G/A polymorphism and cervical cancer was in accordance with previous reports from African [32, 33] and Caucasian ethnicity [34, 35].
Another TNF-α polymorphism that has drawn researchers' attention is a G to A change inside the promoter region at position -238. This polymorphism is frequently associated with genetic susceptibility for psoriasis vulgaris and other autoimmune diseases [36, 37], although it has not been directly associated with change of gene expression level. It is worth noting that there have been a set of case–control studies in which TNF-α -238 showed an underrepresentation of heterozygous genotypes in cervical cancer subjects [18, 28, 35, 38]. The present study gave similar results than those obtained in those studies: the GA genotype was more frequent in controls than cases, although the difference was not statistical significant (P = 0.08). In the meta-analysis performed by Liu et al. [30], six case–control studies on TNF-α-238 were examined. The authors found that both GA and GA + AA genotypes gave significantly protective effect compared to GG genotype. Besides, Badano et al. [31] detected a haplotype defined by the TNF-α -375A and TNF-α -237A SNPs that was restricted to controls and hypothesized that this haplotype may confer a protective effect to individuals having it. These results raise an intriguing question about the role of TNF-α -238 and whether this SNP somehow has a role or not in affecting transcription levels. However, there exists evidence that this sequence location may be placed within a putative repressor recognition sequence, the transcription repression site [39] that spans a 25-bp stretch between positions -230 and -250 in the promoter region. Further evidence of a potential site was given by Kaluza et al. [40] who found that peripheral blood mononuclear cells from psoriasis patients and controls, who were heterozygous for the TNF-α -238 polymorphism, showed a decrease in TNF alpha production after stimulation with different mitogens and antigens. To the best of our knowledge, there have not been more reports about a transcriptional regulator in this sequence.
The results of previous studies on the effects of the IL-10 -1082 polymorphism and the risk of cervical cancer are controversial. This polymorphism has been found to be associated with the risk of cervical cancer development in populations from Zimbabwe and Japan [27, 41], while studies in The Netherlands [42], South Africa [43], and Hungary [44] did not find any association. In Japanese population, IL-10 -1082 genotypes corresponding to high production of interleukin (GA and GG) were significantly associated with cervical disease severity [41]. As pointed out by the authors, the discrepancy of reported results among studies may be explained by the frequency of the G allele in healthy controls: 0.09 in Japan [41], 0.16 in Zimbabwe [27], 0.75 in Hungary [44], and 0.78 in The Netherlands [42]. Evidently, the allele frequencies of this polymorphism appeared to differ widely according to ethnicity. In the UK, the frequency of G allele was 0.52 in South East England [45] and 0.49 in Manchester [46]. In contrast, Chinese populations have the lowest frequencies for this allele [47], with a frequency as low as 0.06. As expected, the G alelle frequency obtained in this study (0.32) was similar to that reported for Italy (0.37) [48], showing no relation with cervical cancer risk.
Finally, although we found that the effect of TNF-α -238 heterozygous genotype was different among the groups of IL-10, suggesting a potential interaction, this difference was not statistically significant (P = 0.08). In conclusion, the present evidence supports the consideration of a potential effect of TNF-α -238 A/G in the reduction of cervical cancer risk in Argentine women, but not TNF-α -308 or IL-10. Larger studies are needed to fully understand the genetic predisposition for the development of cervical cancer.
References
Cogliano V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F. WHO International Agency for Research on Cancer (2005). Carcinogenicity of human papillomaviruses. Lancet Oncol. 2005;6:204.
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Muñoz N, Bosch FX, de Sanjose S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518–27.
Hemminki K, Dong C, Vaittinen P. Familial risks in cervical cancer: is there a hereditary component? Int J Cancer. 1999;82:775–81.
Horng JT, Hu KC, Wu LC, et al. Identifying the combination of genetic factors that determine susceptibility to cervical cancer. IEEE Trans Inf Technol Biomed. 2004;8:59–66.
zur Hausen H. Papillomaviruses and cancer: from basic studies to clinical application. Nat Rev Cancer. 2002;2:342–50.
Kadish AS, Ho GY, Burk RD, et al. Lymphoproliferative responses to human papillomavirus (HPV) type 16 proteins E6 and E7: outcome of HPV infection and associated neoplasia. J Natl Cancer Inst. 1997;89:1285–93.
Clerici M, Merola M, Ferrario E, et al. Cytokine production patterns in cervical intraepithelial neoplasia: association with human papillomavirus infection. J Natl Cancer Inst. 1997;89:245–50.
Tartour E, Gey A, Sastsre-Garou X, Lombard Surin I, Mosseri V, Fridman WH. Prognostic value of intratumoral interferon gamma messenger RNA expression in invasive cervical carcinomas. J Natl Cancer Inst. 1998;90:287–94.
Tartour E, Pannetier C, Mathiot C, et al. Prognostic value of cytokine and Fc gamma receptor assays in oncology. Immunol Lett. 1995;44:145–8.
Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med. 1998;38:423–8.
Li H, Groop L, Nilsson A, Weng J, Tuomi T. A combination of human leukocyte antigen DQB1*02 and the tumor necrosis factor alpha promoter G308A polymorphism predisposes to an insulin-deficient phenotype in patients with type 2 diabetes. J Clin Endocr Metab. 2003;88:2767–74.
Pillai S, Bikle DD, Eessalu TE, Aggarwal BB, Elias PM. Binding and biological effects of tumor necrosis factor alpha on cultured human neonatal foreskin keratinocytes. J Clin Invest. 1989;83:816–21.
Eksteen JA, Scott PA, Perry I, Jankowski JA. Inflammation promotes Barretts metaplasia and cancer: a unique role for TNF alpha. Eur J Cancer Prev. 2001;10:163–6.
Kroeger KM, Carville KS, Abraham LJ. The -308 tumor necrosis factor-alpha promoter polymorphism effects transcription. Mol Immunol. 1997;34:391–9.
Wilson AG, Symons JA, McDowell TL, McDevitt HQ, Duff GW. Effects of a polymorphism in the human tumor necrosis factor alpha promoter on transcriptional activation. Proc Natl Acad Sci USA. 1997;94:3195–9.
Höhler T, Kruger A, Gerken G, Schneider PM, Meyer zum Büschenfelde KH, Rittner C. Tumor necrosis factor alpha promoter polymorphism at position -238 is associated with chronic active hepatitis C infection. J Med Virol. 1998;54:173–7.
Jang WH, Yang YI, Yea SS, et al. The -238 tumor necrosis factor-alpha promoter polymorphism is associated with decreased susceptibility to cancers. Cancer Lett. 2001;166:41–6.
Strieter RM, Kunkel SL, Bone RC. Role of tumor necrosis factor-alpha in disease states and inflammation. Crit Care Med. 1993;21:S447–63.
Ardizzoia A, Lissoni P, Brivio F, et al. Tumor necrosis factor in solid tumors: increased blood levels in the metastasic disease. J Biol Regul Homeost Agents. 1992;6:103–7.
Turner DM, Williams DM, Sankaran D, Lazarus M, Sinnott PJ, Hutchinson IV. An investigation of polymorphism in the interleukin-10 gene promoter. Eur J Immunogenet. 1997;24:1–8.
Alamartine E, Berthoux P, Mariat C, Cambazard F, Berthoux F. Interleukin-10 promoter polymorphisms and susceptibility to skin squamous cell carcinoma after renal transplantation. J Invest Derm. 2003;120:99–103.
Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16:1215.
Ting Y, Manos MM. Detection and typing of genital human Papillomavirus. In: Innis MA, Gelfand DH, Sninsky JJ, White TJ, editors. PCR protocols. San Diego: Academic Pres; 1990. p. 356.
Evander M, Edlund K, Bodun E, et al. Comparison of a one-step and two-step polimerase chain reaction with degenerate general primers in a population-based study of human papillomavirus infection in young Swedish women. J Clin Microbiol. 1992;30:987–92.
Söderlund-Strand A, Rymark P, Andersson P, Dillner J, Dillner L. Comparison between the Hybrid Capture II Test and a PCR-Based Human Papillomavirus detection method for diagnosis and posttreatment follow-up of cervical intraepithelial neoplasia. J Clin Microbiol. 2005;43:3260–6.
Stanczuk GA, Sibanda EN, Perrey C, et al. Cancer of the uterine cervix may be significantly associated with a gene polymorphism coding for increased IL-10 production. Int J Cancer. 2001;94:792–4.
Deshpande A, Nolan JP, White PS, et al. TNF-alpha promoter polymorphisms and susceptibility to human papillomavirus 16-associated cervical cancer. J Infect Dis. 2005;191:969–76.
Kirkpatrick A, Bidwell J, van den Brule AJ, Meijer CJ, Pawade J, Glew S. TNF alpha polymorphism frequencies in HPV-associated cervical dysplasia. Gynecol Oncol. 2004;92:675–9.
Liu L, Yang X, Chen X, et al. Association between TNF-α polymorphisms and cervical cancer risk: a meta-analysis. Mol Biol Rep. 2012;39:2683–8.
Badano I, Stietz SM, Schurr TG, et al. Analysis of TNF-α promoter SNPs and the risk of cervical cancer in urban populations of Posadas (Misiones, Argentina). J Clin Virol. 2012;53:54–9.
Govan VA, Constant D, Hoffman M, Williamson AL. The allelic distribution of -308 tumor necrosis factor-alpha gene polymorphism in South African women with cervical cancer and control women. BMC Cancer. 2006;6:24.
Stanczuk GA, Sibanda EN, Tswana SA, Bergstrom S. Polymorphism at the -308-promoter position of the tumor necrosis factor-alpha (TNF-alpha) gene and cervical cancer. Int J Gynecol Cancer. 2003;13:148–53.
Ivansson EL, Juko-Pecirep I, Gyllensten UB. Interaction of immunological genes on chromosome 2q33 and IFNG in susceptibility to cervical cancer. Gynecol Oncol. 2010;116:544–8.
Calhoun ES, McGovern RM, Janney CA, et al. Host genetic polymorphism analysis in cervical cancer. Clin Chem. 2002;48:1218–24.
Magalhães RF, Biral AC, Pancoto JA, et al. Human leukocyte antigen (HLA) and single nucleotide polymorphisms (SNPs) tumor necrosis factor (TNF)-alpha -238 and -308 as genetic markers of susceptibility to psoriasis and severity of the disease in a long-term follow-up Brazilian study. Int J Dermatol. 2010;49:1133–40.
Nedoszytko B, Szczerkowska-Dobosz A, Zabłotna M, Gleń J, Rebała K, Roszkiewicz J. Associations of promoter region polymorphisms in the tumour necrosis factor-alpha gene and early-onset psoriasis vulgaris in a northern Polish population. Br J Dermatol. 2007;157:165–7.
Gostout BS, Poland GA, Calhoun ES, et al. TAP1, TAP2, and HLA-DR2 alleles are predictors of cervical cancer risk. Gynecol Oncol. 2003;88:326–32.
Fong CL, Siddiqui AH, Mark DF. Identification and characterization of a novel repressor site in the human tumor necrosis factor alpha gene. Nucleic Acids Res. 1994;22:1108–14.
kaluza W, Reuss E, Grossmann S, et al. Different transcriptional activity and in vitro TNF-alpha production in psoriasis patients carrying the TNF-alpha 238A promoter polymorphism. J Invest Dermatol. 2000;114:1180–3.
Matsumoto K, Oki A, Satoh T, et al. Interleukin-10–1082 gene polymorphism and susceptibility to cervical cancer among Japanese women. Jpn J Clin Oncol. 2010;40:1113–6.
Zoodsma M, Nolte IM, Schipper M, et al. Interleukin-10 and Fas polymorphisms and susceptibility for (pre)neoplastic cervical disease. Int J Gynecol Cancer. 2005;15:282–90.
Govan VA, Carrara HR, Sachs JA, Hoffman M, Stanczuk GA, Williamson AL. Ethnic differences in allelic distribution of IFN-g in South African women but no link with cervical cancer. J Carcinog. 2003;2:3.
Szöke K, Szalmás A, Szládek G, et al. IL-10 promoter nt -1082A/G polymorphism and human papillomavirus infection in cytologic abnormalities of the uterine cervix. J Interferon Cytokine Res. 2004;24:245–51.
Reynard MP, Turner D, Navarrete CV. Allele frequencies of polymorphisms of the tumour necrosis factor-alpha, interleukin-10, interferon-gamma and interleukin-2 genes in a North European Caucasoid group from the UK. Eur J Immunogenet. 2000;27:241–9.
Perrey C, Pravica V, Sinnott PJ, Hutchinson IV. Genotyping for polymorphisms in interferon-gamma, interleukin-10, transforming growth factor-beta 1 and tumour necrosis factor-alpha genes: a technical report. Transpl Immunol. 1998;6:193–7.
Mok CC, Lanchbury JS, Chan DW, Lau CS. Interleukin-10 promoter polymorphisms in Southern Chinese patients with systemic lupus erythematosus. Arthritis Rheum. 1998;41:1090–5.
Poli F, Nocco A, Berra S, et al. Allele frequencies of polymorphisms of TNFA, IL-6, IL-10 and IFNG in an Italian Caucasian population. Eur J Immunogenet. 2002;29:237–40.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barbisan, G., Pérez, L.O., Contreras, A. et al. TNF-α and IL-10 promoter polymorphisms, HPV infection, and cervical cancer risk. Tumor Biol. 33, 1549–1556 (2012). https://doi.org/10.1007/s13277-012-0408-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-012-0408-1